Abstract
Indian health sector is a complex admixture of public and private providers, but several lacunae of public health service delivery system in terms of human resource, access, and quality have resulted in unprecedented growth of private sector. Although seamless delivery of services at rural and urban areas, timely approach, and improved information technology system are the strength of the private sector, this package comes at the cost of high out-of-pocket expenditure. Mobilization of private sector health workforce by their capacity building in terms of orientation toward public health services is one of the available solutions to move toward wider coverage of public health services. However, numerous challenges need to be addressed before realization of this vision.
Keywords: Capacity building, health workforce, out-of-pocket expenditure, private sector, public health service
INTRODUCTION
India has a complex health-care delivery system with an admixture of public and private providers which has evolved into a competitive, performance-driven industry demanding the best management skills related to workforce, technology, and finance.[1] In the past few decades, there has been an increasing demand for health care in our country which can be attributed to the increase in proportion of aging population, rising income levels, growing health awareness, and changing adaptive attitude toward preventive health care. However, several lacunae of public sector services in terms of human resource, access, and quality have resulted in unprecedented growth of the private health sector. Seamless delivery of services, both at rural and urban areas, timely approach, and improved information technology system are the strength of the private sector which concentrates more on patient convenience and comfort, thus making the services more attractive for the users, even though technical deficiencies in patient treatment are often reported.
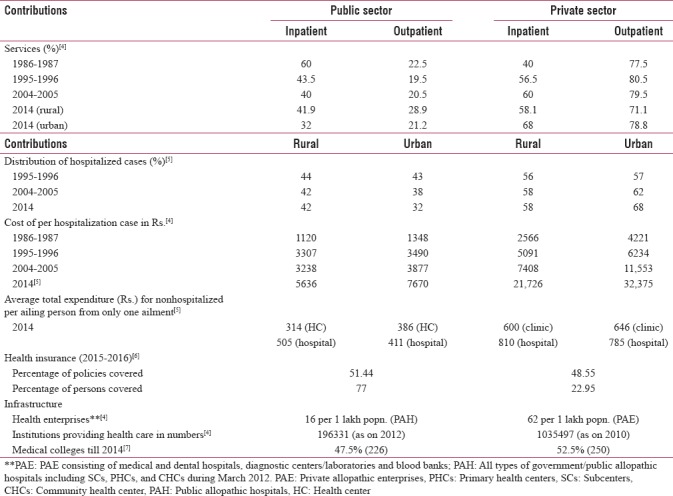
The public sector was the forefront provider of health at the time of independence when private health sector accounted for only 8% of total patient care (World Bank, 2004), but now, it is estimated that 93% of all hospitals, 64% of beds, 80%–85% of doctors, and 80% of outpatient and 57% of inpatient services are catered to by private sector.[2] The National Sample Survey (NSS) 2014 estimated that >70% (72% in rural and 79% in urban) spells of ailment were treated in the private sector (consisting of private doctors, nursing homes, private hospitals, charitable institutions, etc.). This inclination toward availing services from private sector is also corroborated from NFHS-4 report, which states that 56.1% and 49% of members of surveyed urban and rural households, respectively, sought private health care in times of sickness, while for public sector, it was only 42% and 46.4%, respectively.[3] The increasing trend of utilization of private sector services for both inpatient and outpatient care at the expense of high costs incurred is evident from Table 1.[4,5] In terms of health insurance, public sector provides wider coverage, but overall contributions of private sector as regards to infrastructure, i.e., health enterprises, doctors, and medical colleges are greater than that of government sector.[4,5,6,7]
Table 1.
Contributions of public and private health sector in terms of service utilization, expenditure, insurance coverage, and infrastructure
World Bank data, 2014, estimated that out-of-pocket expenditure (OOP) was about 62.4% of total health expenditure, one of highest in the world.[8] The primary reason for this huge OOP has been attributed to the fact that a high proportion of patients tend to seek the services of private for-profit providers, due to ease of access because of longer outpatient clinic opening hours, personalized and caring attitude of health personnel, and greater confidentiality in dealing with sensitive issues such as sexually transmitted diseases and tuberculosis (TB).[9]
Although the 2004–2014 decade had witnessed many significant policy changes in the health-care sector of India, comparison of percentage of the reasons for nonutilization of government health facility as available from the NSS data of the 60th (January–June 2004) and 71st (January–June 2014) rounds show that “poor quality” of available services was the key reason for avoiding public health care (26.8% and 28.8%, respectively).[10]
Assuming that government spends about 10 lakh rupees at the current prices on the education and training of each doctor and about 80% of the out-turns of government medical colleges either join the private sector or migrate abroad, the country loses large resources which could have been used for public benefit, i.e., Rs. 4000–5000 million as a result of out-migration of 4000–5000 doctors every year.[11] It is estimated that there is a shortage of 5 lakh doctors in the country today.[12] Scarcity of health workforce in the public sector is due to not only outmigration or “brain drain,” but also the fresh pass outs are less inclined to serve the public sector, blemished by the age-old predictable problems of poor pay package, compromised promotional avenues, frequent transfers, and unsatisfactory working environment. Therefore, mobilization of health workforce of private sector toward public service delivery remains one of the available solutions to move toward wider coverage of public health services. With this background, this paper intends to examine the avenues for capacity building of health workforce of private sector for delivery of public health services and identify the challenges that need to be addressed for their capacity building with the aspiration of achieving universal health coverage in India by 2020.
CAPACITY BUILDING OF HEALTH WORKFORCE OF PRIVATE SECTOR
For public health service delivery, one of the most important prerequisites is adherence to standard treatment guidelines of common diseases by the health providers. This would ensure uniformity of treatment protocols, thereby preventing unnecessary OOP, antimicrobial resistance, and unnecessary referrals causing delay in treatment initiation. Globally, there are evidences of breach of technical quality of care in the private sector like irrational use of antibiotics for treatment of diarrheal diseases and noncomplicated acute respiratory infections from Egypt and Pakistan, insufficient use of oral rehydration salts for treatment of dehydration from Bangladesh, Nigeria, Pakistan, Sri Lanka, and Yemen, underdosing of antimalarials from Vietnam, and nonadherence to treatment guidelines in TB care from India.[13] Nevertheless, adherence to standard treatment protocols by the Private Medical Practitioners (PMPs) can be enhanced by their competence building through continuing medical education (CME) to keep their knowledge updated. The Medical Council of India in 2002 had formulated that doctors should complete 30 hours of CME every 5 years in order to re-register, but only about 20% of the doctors in India have complied to this code.[14] Barriers such as lack of legislative binding, resistance to change, and lack of motivation are some of the reasons for not attending CMEs. However, exemplary action has been taken by Delhi Medical Council in 2002 which has given a mandate of attendance of 100 hours of CME every 5 years before they can re-register as doctors.[15]
Additional strategies such as use of financial incentives to ensure adherence to treatment protocols as per national programmatic guidelines can also be implemented. According to the National Strategic Plan for TB Elimination (2017–2025), plans of providing the private sector TB care providers' monetary incentives to promote TB case notification and completion have been outlined as a part of strategy to adhere to national guidelines for treatment of TB.[16] Nevertheless, emphasis on development of inclination and skill toward public health service delivery and a population perspective in undergraduate medical training should also form a part of long-term strategy to improve provider practices.
The scarcity of trained doctors in rural India has led to the emergence of untrained medical practitioners (quacks) who often serve as important first responders in rural health-care delivery system. It is estimated that these unlicensed practitioners in the country outnumber qualified medical doctors by at least 10:1. Although a large majority of them operate in rural areas, urban areas are witnessing their increasing numbers as well.[17] However, capacity building of the informal health professionals is possible though proper skill based training and thereby mainstream them as mid-level service providers. The concept of mid-level service providers as put forward by the National Health Policy (NHP) (2017) aims at developing a cadre of front-line health workers in the community who are not doctors but who can be trained through competency-based short courses and equip them with skills to provide services at the subcenter and other underserved areas where they are needed most.[18] In contrast to community or lay health workers, however, they must have a formal certificate and accreditation through appropriate licensing bodies.[19] Evidence from low-income countries, for example, Africa, Southeast Asia, and the Pacific regions show that a wide array of services by mid-level service providers have made significant contributions to improvement of public health-care delivery system.[20]
CHALLENGES AHEAD
In spite of its inherent trait of profit-making, the private sector has a significant potential for providing both preventive and curative public health services. However, failure of the public sector to assign practical public duties to the PMPs is also one of the major bottlenecks that have to be overcome in future.
Another major challenge lies in enforcing regulations in the private sector due to heterogeneity of the institutions, lack of standardized costs, variability in infrastructure, workforce, and gaps in legislative implementation of the existing regulations. Legislative support in terms of mandatory accreditation of the private institutions to the relevant accreditation bodies such as National Accreditation Board for Testing and Calibration Laboratories (NABL) and National Accreditation Board for Hospitals and Healthcare Providers (NABH) would also be a welcome move to ensure compliance with quality control standards.
One of the major hurdles in mobilizing private providers for public health services is the huge OOP that the patients will incur on availing the services; therefore, it is utmost essential to regulate user fees of this sector. Three different payment methods, i.e., (a) Flexible Fee Schedule (FLFS), (b) Fixed Fee Schedule, and (c) Fee Sharing System are prevalent in the urban private hospital sector.[21] These methods of which FLFS is the most widely prevalent involve fee-for-service payments, i.e., the patient pays the physician's fee directly, and there is no control over the physician's charges; thus, his OOP is left at the mercy of the physician's discretion. Hence, there is an urgent need for introduction of fee capping of services in all categories, i.e., diagnostics, inpatient, surgical, and outpatient services with a balancing attitude such that the huge profit-making business like turnover is stabilized to a decent surplus. Commendable steps have been put forward in this regard by the West Bengal Clinical Establishments (Registration, Regulation and Transparency) Bill and Karnataka Private Medical Establishments (Amendment) Bill in October 2017. The bills are in the process of fixing rates of private health-care services, for example, laboratory investigation, intensive care, and implants, and in the event of any complication requiring a change in course of treatment, hospitals will not be allowed to charge anything extra. Other regulations such as no demand for dues to hand over dead body would also be enforced and hefty penalty would be imposed for not following the regulations.[22] However, detailed mechanism as to how compliance is to be audited has not been spelled out clearly.
WAY FORWARD
The National Health Mission had envisaged participation and utilization of the private sector in public health services. Furthermore, NHP 2017 provides future directions to shape up the growth of private health-care industry currently valued at $40 billion and projected to grow to $280 billion by 2020.[23] Utilization of the potential of private sector would facilitate to bring in revenue, provide employment, and meet up the minimum Human Resource for Health norm of 23 workers/10,000 population which is presently 19/10,000.[24] The policy advocates contracting private sector for skill development programs of paramedical staff and medical skills in select areas. Utilization of Corporate Social Responsibility platform to play an active role for filling health infrastructure gaps in public health facilities across the country is another welcome move. Creation of unified emergency response system along with public sector during disasters by pooling up infrastructure, trained human resource to act as first responders, stewardship role in strategic purchasing, active role in immunization, disease notification and surveillance, health information system, and acceptance of referrals from public health system at subsidized rate are some of the services identified in the policy that can be provided by the private health sector which would, in turn, contribute to strengthen the health system.[18]
For streamlining the workforce of this sector for the visionary public service delivery in alignment with public health goals, the first step is to develop geographic information system enabled reliable database on private health-care providers starting from the district level building up to the state and national levels so that a definitive plan of services to be provided at each geographic area/specific population can be drawn up. Guidelines in agreement with protocols of national health programs need to be formulated to outline the services that the different categories of private health providers (qualified and informal) may and may not provide. Using the public–private partnership model of social franchising, wider service coverage can be ensured through dissemination of drugs, tests, devices, and vaccines provided through national health programs. On a final note, formulation of standards similar to Indian Public Health Standards (IPHS) for private health sector will help in maintaining the quality of care component and thus achieve the ultimate target of universal health coverage for the millions of citizens of India in near future.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mehra A. Private Sector in Health. Role of the Private Sector in Health Care in India - Present and Future. [Last accessed on 2017 Aug 10]. Available from: http://www.medind.nic.in/haa/t08/i1/haat08i1p2.pdf .
- 2.Tiwari VK, Nair KS. Private health care in India. Health Millions. 2006;32:36–45. [Google Scholar]
- 3.National Family Health Survey (NFHS-4), 2015-16: India. Mumbai: IIPS; 2017. [Last accessed on 2018 Mar 01]. International Institute for Population Sciences (IIPS) and ICF. Available from: http://www.rchiips.org/NFHS/NFHS-4Reports/India.pdf . [Google Scholar]
- 4.Kumar S. Private sector in healthcare delivery market in India: Structure, Growth and Implications. 2015. Dec, [Last accessed on 2018 Jan 10]. Available from: http://www.isid.org.in/pdf/WP185.pdf .
- 5.Health in India. NSS 71st Round. (January – June 2014) Ministry of Statistics and Programme Implementation, Government of India. Report No. 574 (71/25.0) [Last accessed on 2018 Jan 10]. p. 38. Available from: http://www.mospi.nic.in/sites/default/files/publication_reports/nss_rep574.pdf .
- 6.National Health Profile 2017. Central Bureau of Health Intelligence. Ministry of Health and Family Welfare, Government of India. 2017. [Last accessed on 2018 Mar 01]. Available from: http://www.indiaenvironmentportal.org.in/files/file/NHP_2017-1.pdf .
- 7.Medical Council of India. Information Desk (Homepage) [Last accessed on 2018 Mar 01]. Available from: https://www.mciindia.org/cms/information-desk/college-and-course-search .
- 8.Out-of-Pocket Health Expenditure (% of Total Expenditure on Health) World Health Organization Global Health Expenditure database. [Last accessed on 2017 Dec 08]. Available from: https://ww.data.worldbank.org/indicator/SH.XPD.OOPC.TO.ZS .
- 9.Brugha R, Zwi A. Improving the quality of private sector delivery of public health services: Challenges and strategies. Health Policy Plan. 1998;13:107–20. doi: 10.1093/heapol/13.2.107. [DOI] [PubMed] [Google Scholar]
- 10.Ravi S, Ahluwalia R, Bergkvist S. Health and Morbidity in India (2004-2014) Brookings India. Research Paper No. 092016. 2016. [Last accessed on 2018 Jan 18]. p. 16. Available from: https://www.brookings.edu/wp.content/uploads/2016/12/201612_health-and-morbidity.pdf .
- 11.The private Health Sector in India: Nature, Trends and Critique. [Last accessed on 2017 Dec 05]. Available from: http://www.cehat.org/researchareas/project/1489662497 .
- 12.Healthcare Crisis: Short of 5 Lakh Doctors, India has Just 1 for 1,674 People. [Last accessed on 2017 Dec 06]. Available from: http://www.hindustantimes.com/india-news/healthcarecrisis-short-of-5-lakh-doctors-india-has-just-1-for-1-674-people/story-SZepTyjJ78WgOVIo93tBVK.html .
- 13.(Draft) The Montreux challenge: Making health systems work. Glion sur Montreux, Switzerland: World Health Organization; 2005. Working with the Private Sector to Achieve Public Health Goals at the Country Level; pp. 4–6. [Google Scholar]
- 14.Rao PH. The private health sector in India: A framework for improving the quality of care. ASCI J Manage. 2012;41:14–39. [Google Scholar]
- 15.Sarkar Bd, Kumar S. Delays in legislation slow the progress of CME in India. Bull World Health Organ. 2004;82:154–5. [PMC free article] [PubMed] [Google Scholar]
- 16.Revised National Tuberculosis Control Programme. New Delhi: Central TB Division, Directorate General of Health Services, Ministry of Health with Family Welfare; 2017. National Strategic Plan for Tuberculosis Elimination 2017–2025. [Google Scholar]
- 17.National URBAN Health Mission. (May 2013) Ministry of Health and Family Welfare, Government of India. [Last accessed on 2017 Sep 15]. Available from: http://www.cghealth.nic.in/ehealth/2016/NUHMDOC/Implementation_Framework_NUHM.pdf .
- 18.National Health Policy. Ministry of Health and Family Welfare, Government of India. 2017. [Last accessed on 2017 Dec 01]. Available from: https://www.nhp.gov.in/NHPfiles/national_health_policy_2017pdf .
- 19.WHO/WPRO (2001:1) Mid-Level and Nurse Practitioners in the Pacific: models and issues. [Last accessed on 2017 Sep 15]. Available from: http://www.wpro.who.int/NR/rdonlyres/2B4C3B03-7F6F-47CF-A001-06305ABEA3DD/0/nursescoverall.pdf .
- 20.Lehmann U. A Literature Review. Geneva: World Health Organization Department of Human Resources for Health; 2008. [Last accessed on 2017 Dec 08]. Mid-Level Health Workers. The state of the Evidences on Programmes, Activities, Costs and Impact on Health Outcomes. Available from: http://www.who.int/hrh/MLHW_review_2008.pdf . [Google Scholar]
- 21.Muraleedharan VR. Small Applied Research Paper 5. Bethesda, MD: Partnerships for Health Reform Project, Abt Associates Inc.; 1999a. Characteristics and structure of the Private Hospital Sector in Urban India: A Study of Madras City. [Google Scholar]
- 22.West Bengal Assembly Passes Bill to Regulate Private Hospitals in State. [Last accessed on 2017 Oct 11]. Available from: http://www.livemint.com .
- 23.Situation Analyses. Backdrop to the National Health Policy 2017. Ministry of health and family Welfare, Government of India. 2017. [Last accessed on 2018 Mar 01]. Available from: https://www.mohfw.gov.in/sites/default/files/71275472221489753307.pdf .
- 24.Instituted by Planning Commission of India. Cha. 4. New Delhi: High Level Expert Group Report on Universal Health Coverage for India; 2011. [Last accessed on 2018 Mar 09]. High Level Expert Group Report on Universal Health Coverage for India; p. 144. Available from: http://www.planningcommission.nic.in/reports/genrep/rep_uhc0812.pdf . [Google Scholar]


