Abstract
Diabetes is a chronic metabolic disorder that impacts physical, social and mental including psychological well-being of people living with it. Additionally, psychosocial problems that are most common in diabetes patients often result in serious negative impact on patient's well-being and social life, if left un-addressed. Addressing such psychosocial aspects including cognitive, emotional, behavioral and social factors in the treatment interventions would help overcome the psychological barriers, associated with adherence and self-care for diabetes; the latter being the ultimate goal of management of patients with diabetes. While ample literature on self-management and psychological interventions for diabetes is available, there is limited information on the impact of psychological response and unmanaged emotional distresses on overall health. The current review therefore examines the emotional, psychological needs of the patients with diabetes and emphasizes the role of diabetologist, mental health professionals including clinical psychologists to mitigate the problems faced by these patients. Search was performed using a combination of keywords that cover all relevant terminology for diabetes and associated emotional distress. The psychological reactions experienced by the patient upon diagnosis of diabetes have been reviewed in this article with a focus on typical emotional distress at different levels. Identifying and supporting patients with psychosocial problems early in the course of diabetes may promote psychosocial well-being and improve their ability to adjust or take adequate responsibility in diabetes self-management – the utopian state dreamt of by all diabetologists !.
Keywords: Anxiety, depression, diabetes mellitus, psychological factors, psychosocial support
INTRODUCTION
Diabetes is a serious and complex metabolic disorder with the prevalence reaching endemic proportions over the past few decades. According to the International Diabetes Federation, there are 382 million people worldwide affected by diabetes, and it is expected to reach 592 million by 2035.[1] Among them, India alone has 65.1 million people with diabetes in the age group of 20–79 years.[1] With India approaching numbers predicted to be attained by 2030, in 2020 itself, India is sitting on a diabetic volcano!
Majority of the guidelines on diabetes care focus on the medical aspects of initial management without addressing the psychological needs of the patient.[2] Although many people with diabetes cope well and live healthy lives, several studies, including The Diabetes Attitudes, Wishes, and Needs study, emphasized that psychological support in this group of patients is under-resourced and inadequate, resulting in poor quality of life (QoL) and reduced general well-being.[3,4,5,6,7,8,9] It is often difficult for many to accept that they have to take drugs invariably throughout their life, resulting in poor treatment adherence and diabetes self-management.[2] These psychosocial problems can eventually develop into depressive or other psychological disorders that are associated with poor self-care behavior, poor metabolic outcomes, increased mortality, functional limitations, increased health-care cost, loss of productivity, and reduced QoL.[10,11,12,13,14,15,16,17] Emotional and psychological needs of the patients with diabetes are compromised, when personal efforts to meet these challenges fail to succeed as anticipated, or when the complications of diabetes take their toll on physical and mental (psychological) health.[18]
Evidence indicates that diabetes[11,19] and its complications are strongly associated with psychological and psychiatric problems. These include depression,[20,21,22] poor-eating habits,[23] and fear of hypoglycemia.[24,25] Moreover, patients with type 2 diabetes mellitus (T2DM) also have a two-fold greater risk for comorbid depression compared to healthy controls, hampering the QoL of patients.[26,27] Research also indicates that patients with diabetes suffer from high levels of diabetes-specific emotional stress.[28,29] This is associated with functional impairment, poor adherence to exercise, diet and medications, and inadequate glycemic control.[11,30,31,32]
In view of this, it is important to identify and support patients with psychosocial problems early in the course of diabetes as it may affect their ability to adjust or take adequate responsibility for self-care.[33] Addressing the psychological needs results in improvement on diabetes outcomes in terms of better glycemic control[34,35] and reduced comorbid psychiatric disorders such as depressed mood.[36]
Effective self-management of diabetes is a critical step in achieving healthy and satisfying life. However, it requires a great deal of personal motivation and change in behavior. The importance of psychological interventions in diabetes management has been identified by organizations such as Scottish Intercollegiate Guidelines Network,[37] The National Institute of Health and Clinical Excellence,[38] and Institute for Clinical Systems Improvement.[39] These organizations have incorporated evidence-based guidelines for psychosocial care in adults with diabetes.
The aim of this review is to:
Provide an overview on the psychological needs among people with diabetes
Address the psychological reactions in patients with diabetes by focusing on different levels of emotional distress.
An attempt has been made to understand the physiological role of stress in the development of diabetes and to establish a relationship between psychiatric disorders including depression and anxiety to the clinical presentation with diabetes. Finally, a brief overview on different psychological interventions for improved self-care behavior has been discussed.
METHODOLOGY
An extensive search was performed in databases of medical and scientific literature including, but not limited to, “PubMed,” “CrossRef,” “EMBASE,” and “Cochrane Library” with search terms “diabetes mellitus,” “psychosocial support,” “psychological,” “psychiatric,” “anxiety,” “depression,” and other terms related to the current topic of research. Our search criteria identified previous randomized control trials, prospective observational studies, and retrospective case series, reflecting a balance between designed coordinated studies and real-world clinical data. Studies with significance for the current research question were qualitatively graded for inclusion in the current review. Studies conducted in recent years and published in the last 15 years are primarily included in the current review. The review aimed at presenting a wide-ranging discussion on the current topic, and hence, no specific data synthesis was carried out.
Pyramid model
Given that emotional and psychological needs of people living with diabetes are complex, it is important to understand the range of psychological problems in any patient population or individual. The NHS Diabetes and Diabetes UK's summary of psychological needs in diabetes group advocated a tiered model of emotional and psychological support known as the “pyramid of psychological need.”[40] This “pyramid model” illustrates the diversity of need and the broadly inverse relationship between prevalence and severity of need which can have a profound effect on QoL and psychological well-being of a patient. From a population perspective, this model can be used to describe differences in need against differences in variables such as type of diabetes, duration of the condition, lifespan, and sociodemographic characteristics. Boundaries between the levels of the pyramid are not absolute as any person may move up or down these levels at any point in his/her life.
Based on the severity of psychological needs of the patient, the model has five levels (i.e., Level 1 to Level 5) [Table 1] as described below:[18]
Table 1.
Role of diabetologist and mental health professionals based on severity level of difficulties faced by persons with diabetes mellitus
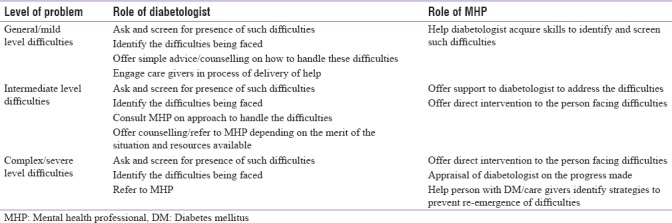
Level 1 is associated with general difficulties coping with diabetes and its perceived consequences
Level 2 is associated with more severe difficulties with coping, causing significant anxiety, or lowered mood with impaired ability to self-care as a result. General and diabetes-related chronic stress at Level 1 can lead to symptoms of anxiety and depression at Level 2[28,41,42,43]
Level 3 is associated with psychological problems that are diagnosable and can be treated through psychological interventions alone, for example, mild and moderate cases of depression, anxiety states, and obsessive/compulsive disorders[18]
Level 4 covers more severe psychological problems that are diagnosable and require biological treatments, medications, and psychologist consultation and interventions[18]
Level 5 is associated with severe and complex mental illness/disorder requiring psychiatric intervention.[18]
Concept of stress in diabetes
Psychological stress has been implicated as a chief causative factor for psychosomatic disorders. Stress is defined as “the consequence of the failure of an organism – human or animal – to respond appropriately to emotional or physical threats, whether actual or imagined.”[44] Stress response can be defined as a cognitive, emotional, physical, or behavioral level that can have serious, negative consequences on the body upon long-term activation.[44] Interestingly, stress has long been suspected as having important effects on the development of diabetes through different pathways via behavioral and physiological mechanisms. Behavior-induced emotional stress was associated with unhealthy lifestyle behaviors, such as inadequate-eating behaviors in terms of quality and quantity of food, low exercise levels, smoking, and alcohol abuse.[45,46] On the other hand, physiological, emotional stress is associated with long-term activation of the hypothalamic–pituitary–adrenal axis and the sympathetic nervous system, resulting in chronic stress reactions, including depression, anxiety, mood disorders, and sleep disturbances.[47,48]
Gonzalez in diabetes care, 2011 defined diabetes distress (DD) as the unique, often hidden, emotional burdens and worries that a patient experiences when they are managing a severe chronic disease such as diabetes. High levels of DD are common and distinct from clinical depression. DD screening tool is a unique 17-question survey used for assessing emotional burden, physical-related distress, regimen-related distress, and interpersonal distress. Such tool is quite handy in understanding patient's emotional need in the overall management of diabetes.
Relationship of psychological stress factors to the clinical presentation of diabetes
The biopsychosocial model, which describes psychological stress as a state of normal tension, preoccupation, and agitation, defines it as a relationship between environmental parameters and individual processes of perception and coping with stressors.[49] Under stress, numerous metabolic changes including vasoconstriction in the peripheral vascular system, increased heart rate, increased muscle activity, and increased production of stress hormones serve to elevate blood glucose levels for extra energy required to combat stress.[50] Besides, they have also been associated with increased feeling of vulnerability and activate body to the “fight–flight” response.
The response of a diabetic patient to stress is not uniform across all patients.[50] In patient with type 1 diabetes mellitus, the effects of stress are influenced by aberrant regulation of stress hormones and relative presence of insulin at the time of stress.[51] This can also be attributed to the presence of autonomic nervous system abnormalities associated with diabetic neuropathy, as well as individual psychological differences.[51]
The association between psychological stress and diabetes outcomes is evident in several cross-sectional and longitudinal studies. Several studies have demonstrated that emotional distress in patients with diabetes is associated with poor glycemic control,[11,52] deficit in self-care behavior,[53] and adverse diabetes outcomes.[54] Studies have suggested that nonadherence to treatment may represent an important pathway between emotional distress and poor diabetes outcomes.[55] A longitudinal study by Gonzalez et al. (2008b) demonstrated positive correlation between depressive symptoms and poor medication adherence and diabetes self-care after 9 months.[56] Similarly, another study has shown that persistent depressive symptoms were associated with poor self-management in terms of diet and exercise over the subsequent 5 years.[57] On the contrary, reduction in depressive symptoms was associated with improved glycemic control.[11]
In some reports, psychological factors such as self-efficacy,[58] self-esteem,[59] diabetes coping,[60] and social support[61] were found to be associated with good treatment adherence and glycemic control; whereas factors such as stressful life events,[62] daily environmental stressors,[63] and diabetes-related distress[10] were associated with poor glycemic control and nonadherence to treatment. Depression and anxiety have also been shown to be associated with increased hyperglycemia.[11,64] Furthermore, other studies have also demonstrated that psychological factors may contribute to metabolic,[65] gastrointestinal,[66] and sexual dysfunction[67] along with neuropathic[68] symptoms in patients with diabetes. A study by Lustman et al. evaluated the relationship between depression and diabetes symptoms and concluded that diabetes symptoms are more likely to be associated with depression than to conventional markers of glucose control.[65] Another study revealed that each group of gastrointestinal symptoms was significantly associated with psychiatric illness (P < 0.01 for each) than with peripheral neuropathy (P > 0.2 for each).[66] Furthermore, Lustman and Clouse demonstrated that psychiatric illness (generalized anxiety disorder and depression) was significantly (P < 0.01) associated with sexual dysfunction, irrespective of the effects of neuropathy.[67] Overall, these findings suggest that psychological factors have a great impact on diabetes outcomes and hence should be considered in casual speculations.
Psychological reaction in patients with diabetes
The patient's perception about the seriousness of diabetes will affect the way they cope with the disease.[69] Several psychological factors as discussed earlier contribute to affect the emotional and psychological well-being of a person with diabetes. These include degree to which an individual accepts his/her diagnosis, how the individual adjusts to the demands of self-care routine, and finally how he/she copes with progression of the condition, which potentially includes the development of diabetes-related complications.[70] However, considering that living with diabetes is a lifelong stress and requires dealing with psychological issues, the psychological reactions of patients towards diabetes can be categorized under four basic levels of emotional distress. The psychological factors and reactions with negative outcomes in patients with diabetes have been summarized in Figure 1.
Figure 1.
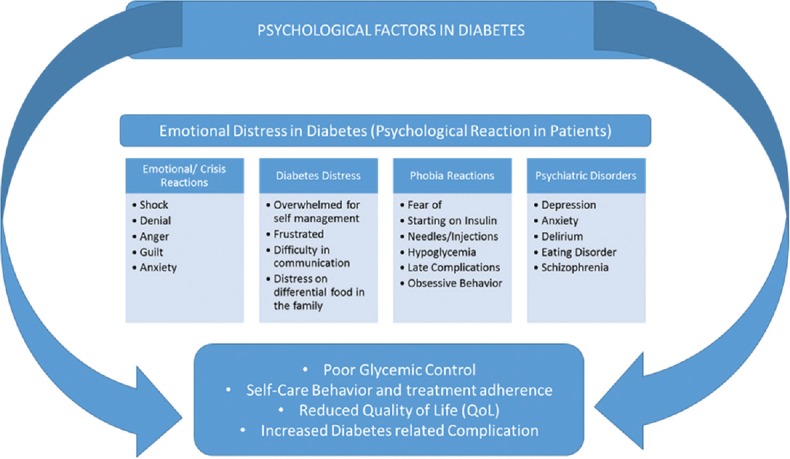
Psychological factors and reactions with negative outcomes in patients with diabetes
Emotional reactions at the time of diagnosis
Beeney et al. found that patients were distressed at the time of diagnosis with emotions ranging from anxiety, shock, anger, or denial.[71] Similar results were observed in other studies.[10,72,73,74,75,76]
Denial
It is a common response against some restrictive or uncomfortable situation and appears when diagnosed with diabetes. As a defense measure, patient may refuse to believe in diagnostic method or the report and try to avoid the long-term complications. In particular, denial interferes with the patients’ ability to monitor their condition, take initiative in seeking treatment, and manage their illness. A crucial aspect regarding denial in T2DM patients as a first reaction may also be explained in the absence of significant physical symptoms or complications in the early stages of T2DM.
Anger
It is a strong feeling of resentment, displeasure, and hostility that often arises in response to a perceived wrongdoing. Once diagnosed with diabetes, the patient may express his/her anguish on the development of such unexpected clinical condition. In addition, the person may get frustrated as to why he/she has developed diabetes. Such emotional state could interfere with the natural coping mechanism of the body which may further deteriorate the condition.
Guilt
It is a natural emotion to a wrong work and often arises after being diagnosed with diabetes. Feeling of guilt may be realistic or unrealistic. These could be managed by answering questions such as ‘”Why am I feeling guilty?,” “Is my guilt realistic?,” “What should I do when I am feeling guilty?,” “Do I have to worry too much,” or “should I try to make positive changes?”
Sorrow/depression
It is a normal response to diabetes which may result from sadness and feeling of loss. Depression is often characterized by sustained changes such as sleep, fatigue, appetite disruption, and disinterest in daily activities over a period of weeks. It may interfere with diabetes self-care and can be managed by counseling with the patient and engaging him/her in fun activities.
Acceptance
This may take time up to a year, but finally, the person accepts his/her situation and prepares himself/herself for living with diabetes. However, this step requires patience, assistance from others, full understanding of diabetes, and its management approaches to manage diabetes into his lifestyle.
Diabetes distress
The National Diabetes Service Scheme Australia defines DD as the emotional burden of living with and managing diabetes. It is a unique, often hidden, emotional burdens and worries that a patient experiences when he/she is managing a severe chronic disease such as diabetes. The needs of the patient during the DD have to be assessed and managed at self, family and friends, and the care provider. The DD learning center of St Johns River Rural Health Network identified the critical information for different stakeholders.
Patients
Feel overwhelmed with the demands of self-management
Feel frustrated, fatigue, anger, burn out, and poor mood
Difficult to keep up with complicated routine
Make it difficult for self-management the control of blood sugar.
Family and friends
Inability for the family members to understand the feelings of the patient makes the patient further burdensome
Food differentiation and restriction of food by family members may lead to further distress
Absence of conducive discussion with family and friends would make the situation worse
The communication by the patient with the family member may be difficult as the patient does not want to make the family members uncomfortable.
Caregivers/physician
Health-care providers (HCPs) are driven by fear of diabetes complications and not maintaining right hemoglobin A1c (HbA1c)
The fear produces behavior in HCPs may interface with diabetes self-management
The common reaction of the HCP is to label the patient as noncompliant to treatment.
Phobia reactions
Although insulin therapy remains the mainstay for the management of diabetes, often nonadherence to insulin therapy is observed among patients with diabetes. The problem of treatment adherence can be linked to psychological barrier associated with fear of needles/injections, insulin initiation, hypoglycemia late complications, and obsessive behavior or overdosing.[77,78] Anxiety related to fear of insulin injection is common among people with diabetes and is reported high among insulin-naïve patients.[79] It has been observed that an extreme level of fear of self-injection is associated with high diabetes-related distress, poor general well-being, and psychological comorbidity, as well as poor adherence to the diabetes treatment regimen.[79,80] Moreover, individuals with diabetes may experience unpleasant symptoms and negative consequences associated with hypoglycemia. This may result in anxiety or even a fear of hypoglycemia that can have significant clinical implications for diabetes management.[81] Patients with these conditions may miss monitoring of blood glucose levels or administration of insulin dose in severe cases.
Depression and anxiety
Diabetes and psychiatric disorders share a bidirectional association influencing one another in multiple ways and different patterns.[2,82] They can present as independent conditions with parallel pathogenic pathways, or one may manifest during the course of the other and contribute to the pathogenesis of the earlier. In another case, psychiatric disorders may represent as an independent risk factor for the development of diabetes or could be an overlap of the clinical presentations or emerge as a side effect of the medication used to treat psychiatric disorder or vice versa. Psychiatric disorders represent a pattern of behavioral or psychological symptoms that impact the life of an individual. Although psychiatric disorders create suffering for the person experiencing these symptoms, depression is one of the most studied disorders and has been shown to be associated with significant negative impact on patients with diabetes.[83]
Depression is the most common psychiatric disorder in people with diabetes, with an estimated 41% of patients suffer from poor psychological well-being and elevated rates of depression and anxiety disorders.[18] People with type 2 diabetes have 24% of higher risk of developing depression[84] and therefore the co-morbid conditions of depression and diabetes needs a careful attention.[85] Data also indicate that 13% of all newly diagnosed T2DM cases in the US are associated with clinical depression.[86] A systematic review by Ali et al. (2006) reported that the prevalence of depression was significantly higher among patients with T2DM than those without diabetes (17.6% vs. 9.8% odds ratio = 1.6, 95% confidence interval 1.2–2.0).[87] The bidirectional relationship between depression and diabetes was evidenced from a meta-analysis by Mezuk et al., who reported that patients with depression have ~ 60% increased risk of developing T2DM.[88,89] Physicians caring for individuals with type 2 diabetes must be aware of possible coexisting depression, which must be identified and managed appropriately by a combination of lifestyle advice, antidepressant medicines, and psychotherapy.[114]
Anxiety is another common psychological disorder in patients with diabetes.[90] Evidence from a systematic review reported higher prevalence of anxiety in diabetes patients with 14% of patients suffering from generalized anxiety disorder, 27% with sub-syndromal anxiety disorder, and 40% with elevated anxiety symptoms than those without diabetes.[91] In another study, patients assessed for the clinical features of anxiety using Hamilton Rating Scale for Anxiety (HRSA) and reported higher HRSA scores in the depressed group compared to those in nondepressed group (21.07 ± 5.44 vs. 6.88 ± 3.43).[92]
Other psychiatric disorders in diabetes
Delirium is another psychiatric disorder associated with diabetes and characterized by expression of hypoglycemic episodes or diabetic ketoacidosis.[93] It is associated with increased hospital stay, increased cognitive and functional deterioration, and morbidity and mortality.[82,94,95] In addition, outcomes such as disorientation, confusion, and altered sensorium are often seen in these patients. Early identification is crucial for the outcome of the disease. Close supervision and supportive care remain the main stay of treatment[82]
Eating disorders are another set of psychiatric disorders commonly observed among people with diabetes.[96,97] These disorders can have significant impact on glycemic control and increase the chances of diabetes complications.[23] In a study of 714 patients with diabetes, it was reported that 9.7% of the patients had night eating syndrome (NES).[98] Moreover, these patients were likely to be obese and depressed with poor glycemic control and higher incidence of diabetes complications[98]
Depression, obesity, and type 2 diabetes occur together more often than by chance. Epidemiological and metabolic evidence suggests common pathogenic pathways among the three conditions. However, the cause–effect relationship is less clearly established: depression could lead to obesity and diabetes through lifestyle factors such as sedentary habits, overeating and poor self-care; diabetes, on the other hand, could be associated with depression due to the major emotional, social, medical, and financial burdens placed for its management. In addition, use of antidepressant medicines, particularly the newer generation agents, increases body weight and induces insulin resistance and thereby T2DM[114]
There is a close association between schizophrenia (SZ) and diabetes.[99] Evidence from a large metabolic monitoring database from urban mental health facility reported that depending on demographic variables, such as ethnicity and cigarette smoking, 20%–30% of patients with SZ will diabetes or prediabetes during the course of psychiatric treatment.[100] The prevalence of impaired glucose tolerance in these people may be as high as 30%, depending upon the age[101]
There is evidence showing that insulin resistance may be the link between affective disorders and Alzheimer's disease.[115] Insulin is vital for glucose utilization and neuronal survival in the central nervous system. Fluctuating glucose levels as a result of dysglycemia can result in neuronal apoptosis and formation of neurofibrillary tangles, the hallmark of Alzheimer's disease.
PSYCHOLOGICAL THERAPIES/STRATEGIES IN THE TREATMENT OF DIABETES
Effective management of diabetes requires complex, continual, and demanding self-care behavior. Considering that psychosocial impact is a strong predictor of mortality and morbidity in diabetes patients, integrating psychosocial aspects at all levels of diabetes management is important for better treatment adherence to achieve good glycemic control.[102,103] It is well known that psychosocial stress is common in subjects with diabetes mellitus.[116] Keeping in mind the importance of psychosocial factors in the management and growing burden of diabetes, there is a need for development and implementation of effective, well-evaluated psychosocial interventions/therapies to assist people in dealing with the daily demands of diabetes.[103]
It has been observed that addressing psychological needs improves HbA1c by 0.5%–1% in adults with T2DM.[34,35] Moreover, most physicians believe that psychological problems are associated with worse outcomes and have prompted the establishment of guidelines to ensure that proper psychological support is provided to the patients and negative emotions that arise in living with diabetes are adequately managed.[2,3] Psychosocial interventions such as cognitive behavioral therapy,[104,105] motivational therapy,[106] problem-solving therapy,[2,107] coping skills training,[108,109] and family behavior therapy[110,111] have all shown to improve the treatment adherence and achieve good glycemic control. Considering these facts, psychosocial interventions have been recognized as an integral part of diabetes care.[112,113] Such interventions are very useful to improve glycemic control and self-care behavior, thus reducing the risk of complications and improving the QoL of the patient with diabetes.
Again, to bring the psychological intervention into the existing treatment regimen, few changes are important at the health-care delivery points;
It is important to incorporate psychological screening and management at every level of diabetes care
It is important to sensitize health-care professionals, persons with diabetes, and their family members about the importance of psychological screening and intervention along with other advised treatment
There must be an advocacy program at the community level to improve the awareness level of psychological well-being of persons with diabetes.
CONCLUSION
The relation between diabetes and psychosocial disorders is multifactorial. Their coexistence can impact glycemic control, self-care behavior, and QoL. The emotional and psychological needs of the patients with diabetes are often compromised when personal efforts to meet these challenges fail to succeed, resulting in increased risk of diabetes-related complications. Such complications lead to reduced QoL, increased mortality, increased health-care costs, and lost productivity. Addressing the psychosocial needs of the patient would overcome the psychological barrier associated with adherence and self-care, while achieving long-term benefits in terms of better health outcomes and glycemic control. Thus, increased understanding of the psychological aspects of the patient with diabetes would allow clinicians to formulate strategies focusing on the improvement in diabetes outcomes and reduction of disease burden.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.International Diabetes Federation. Diabetes Atlas. 6th ed. Brussels: International Diabetes Federation; 2013. [Google Scholar]
- 2.Kalra S, Sridhar GR, Balhara YP, Sahay RK, Bantwal G, Baruah MP, et al. National recommendations: Psychosocial management of diabetes in India. Indian J Endocrinol Metab. 2013a;17:376–95. doi: 10.4103/2230-8210.111608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peyrot M, Rubin RR, Lauritzen T, Snoek FJ, Matthews DR, Skovlund SE, et al. Psychosocial problems and barriers to improved diabetes management: Results of the cross-national diabetes attitudes, wishes and needs (DAWN) study. Diabet Med. 2005;22:1379–85. doi: 10.1111/j.1464-5491.2005.01644.x. [DOI] [PubMed] [Google Scholar]
- 4.Koopmanschap M CODE-2 Advisory Board. Coping with type II diabetes: The patient's perspective. Diabetologia. 2002;45:S18–22. doi: 10.1007/s00125-002-0861-2. [DOI] [PubMed] [Google Scholar]
- 5.Quality of life in type 2 diabetic patients is affected by complications but not by intensive policies to improve blood glucose or blood pressure control (UKPDS 37). U.K. Prospective Diabetes Study Group. Diabetes Care. 1999;22:1125–36. doi: 10.2337/diacare.22.7.1125. [DOI] [PubMed] [Google Scholar]
- 6.Vileikyte L. Diabetic foot ulcers: A quality of life issue. Diabetes Metab Res Rev. 2001;17:246–9. doi: 10.1002/dmrr.216. [DOI] [PubMed] [Google Scholar]
- 7.Holt RI, Kalra S. A new DAWN: Improving the psychosocial management of diabetes. Indian J Endocrinol Metab. 2013;17:S95–9. doi: 10.4103/2230-8210.119515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kalra B, Kalra S, Balhara YP. Psychological assessment and management in diabetes. J Pak Med Assoc. 2013;63:1555–7. [PubMed] [Google Scholar]
- 9.Nicolucci A, Kovacs Burns K, Holt RI, Comaschi M, Hermanns N, Ishii H, et al. Diabetes attitudes, wishes and needs second study (DAWN2™): Cross-national benchmarking of diabetes-related psychosocial outcomes for people with diabetes. Diabet Med. 2013;30:767–77. doi: 10.1111/dme.12245. [DOI] [PubMed] [Google Scholar]
- 10.Polonsky WH, Anderson BJ, Lohrer PA, Welch G, Jacobson AM, Aponte JE, et al. Assessment of diabetes-related distress. Diabetes Care. 1995;18:754–60. doi: 10.2337/diacare.18.6.754. [DOI] [PubMed] [Google Scholar]
- 11.Lustman PJ, Anderson RJ, Freedland KE, de Groot M, Carney RM, Clouse RE, et al. Depression and poor glycemic control: A meta-analytic review of the literature. Diabetes Care. 2000;23:934–42. doi: 10.2337/diacare.23.7.934. [DOI] [PubMed] [Google Scholar]
- 12.Ciechanowski PS, Katon WJ, Russo JE, Walker EA. The patient-provider relationship: Attachment theory and adherence to treatment in diabetes. Am J Psychiatry. 2001;158:29–35. doi: 10.1176/appi.ajp.158.1.29. [DOI] [PubMed] [Google Scholar]
- 13.Rosenthal MJ, Fajardo M, Gilmore S, Morley JE, Naliboff BD. Hospitalization and mortality of diabetes in older adults. A 3-year prospective study. Diabetes Care. 1998;21:231–5. doi: 10.2337/diacare.21.2.231. [DOI] [PubMed] [Google Scholar]
- 14.Katon WJ, Rutter C, Simon G, Lin EH, Ludman E, Ciechanowski P, et al. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care. 2005;28:2668–72. doi: 10.2337/diacare.28.11.2668. [DOI] [PubMed] [Google Scholar]
- 15.Goldney RD, Phillips PJ, Fisher LJ, Wilson DH. Diabetes, depression, and quality of life: A population study. Diabetes Care. 2004;27:1066–70. doi: 10.2337/diacare.27.5.1066. [DOI] [PubMed] [Google Scholar]
- 16.Egede LE. Effects of depression on work loss and disability bed days in individuals with diabetes. Diabetes Care. 2004;27:1751–3. doi: 10.2337/diacare.27.7.1751. [DOI] [PubMed] [Google Scholar]
- 17.Kumar A, Nagpal J, Bhartia A. Direct cost of ambulatory care of type 2 diabetes in the middle and high income group populace of Delhi: The DEDICOM survey. J Assoc Physicians India. 2008;56:667–74. [PubMed] [Google Scholar]
- 18.NHS Diabetes, Diabetes UK. Emotional and Psychological Support and Care in Diabetes. [Last accessed on 2014 Jun 09]. Available from: http://www.diabetes.org.uk/Documents/Reports/Emotional_and_Psychological_Support_and_Care_in_Diabetes_2010.pdf .
- 19.Snoek FJ, Skinner TC. Psychological counselling in problematic diabetes: Does it help? Diabet Med. 2002;19:265–73. doi: 10.1046/j.1464-5491.2002.00678.x. [DOI] [PubMed] [Google Scholar]
- 20.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care. 2001;24:1069–78. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 21.Sridhar GR. Psychiatric co-morbidity & diabetes. Indian J Med Res. 2007;125:311–20. [PubMed] [Google Scholar]
- 22.Ghosh S, Chatterjee S. Should depressive patients undergo a regular diabetes screening test? Indian J Endocrinol Metab. 2013;17:537–8. doi: 10.4103/2230-8210.111692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peveler RC, Bryden KS, Neil HA, Fairburn CG, Mayou RA, Dunger DB, et al. The relationship of disordered eating habits and attitudes to clinical outcomes in young adult females with type 1 diabetes. Diabetes Care. 2005;28:84–8. doi: 10.2337/diacare.28.1.84. [DOI] [PubMed] [Google Scholar]
- 24.Cox DJ, Irvine A, Gonder-Frederick L, Nowacek G, Butterfield J. Fear of hypoglycemia: Quantification, validation, and utilization. Diabetes Care. 1987;10:617–21. doi: 10.2337/diacare.10.5.617. [DOI] [PubMed] [Google Scholar]
- 25.Gold AE, Deary IJ, Frier BM. Hypoglycaemia and non-cognitive aspects of psychological function in insulin-dependent (type 1) diabetes mellitus (IDDM) Diabet Med. 1997;14:111–8. doi: 10.1002/(SICI)1096-9136(199702)14:2<111::AID-DIA309>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 26.Pouwer F, Beekman AT, Nijpels G, Dekker JM, Snoek FJ, Kostense PJ, et al. Rates and risks for co-morbid depression in patients with type 2 diabetes mellitus: Results from a community-based study. Diabetologia. 2003;46:892–8. doi: 10.1007/s00125-003-1124-6. [DOI] [PubMed] [Google Scholar]
- 27.Schram MT, Baan CA, Pouwer F. Depression and quality of life in patients with diabetes: A systematic review from the European depression in diabetes (EDID) research consortium. Curr Diabetes Rev. 2009;5:112–9. doi: 10.2174/157339909788166828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pouwer F, Skinner TC, Pibernik-Okanovic M, Beekman AT, Cradock S, Szabo S, et al. Serious diabetes-specific emotional problems and depression in a Croatian-Dutch-English Survey from the European depression in diabetes [EDID] research consortium. Diabetes Res Clin Pract. 2005;70:166–73. doi: 10.1016/j.diabres.2005.03.031. [DOI] [PubMed] [Google Scholar]
- 29.Kokoszka A, Pouwer F, Jodko A, Radzio R, Mućko P, Bieńkowska J, et al. Serious diabetes-specific emotional problems in patients with type 2 diabetes who have different levels of comorbid depression: A Polish study from the European depression in diabetes (EDID) research consortium. Eur Psychiatry. 2009;24:425–30. doi: 10.1016/j.eurpsy.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 30.Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: Impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160:3278–85. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- 31.Ciechanowski PS, Katon WJ, Russo JE, Hirsch IB. The relationship of depressive symptoms to symptom reporting, self-care and glucose control in diabetes. Gen Hosp Psychiatry. 2003;25:246–52. doi: 10.1016/s0163-8343(03)00055-0. [DOI] [PubMed] [Google Scholar]
- 32.Bhutani G, Kalra S, Verma P, Kaushal J. Bibliometric analysis of Journal of Social Health and Diabetes (JOSH Diabetes) J Soc Health Diabetes. 2014;2:37–9. [Google Scholar]
- 33.Peyrot M, Rubin RR. Behavioral and psychosocial interventions in diabetes: A conceptual review. Diabetes Care. 2007;30:2433–40. doi: 10.2337/dc07-1222. [DOI] [PubMed] [Google Scholar]
- 34.Ismail K, Winkley K, Rabe-Hesketh S. Systematic review and meta-analysis of randomised controlled trials of psychological interventions to improve glycaemic control in patients with type 2 diabetes. Lancet. 2004;363:1589–97. doi: 10.1016/S0140-6736(04)16202-8. [DOI] [PubMed] [Google Scholar]
- 35.Alam R, Sturt J, Lall R, Winkley K. An updated meta-analysis to assess the effectiveness of psychological interventions delivered by psychological specialists and generalist clinicians on glycaemic control and on psychological status. Patient Educ Couns. 2009;75:25–36. doi: 10.1016/j.pec.2008.08.026. [DOI] [PubMed] [Google Scholar]
- 36.Katon WJ, Lin EH, Von Korff M, Ciechanowski P, Ludman EJ, Young B, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363:2611–20. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Scottish Intercollegiate Guidelines Network. SIGN 55. Management of Diabetes. 2001. [Last accessed on 2017 Aug 09]. Available from: http://www.sign.ac.uk; http://www.algadam.net/images2/Management_Diabetes.pdf .
- 38.London: Royal College of Physicians (UK); 2004. The National Collaborating Centre for Chronic Conditions (UK). Type 1 Diabetes in Adults. National Clinical Guideline for Diagnosis and Management in Primary and Secondary Care. [PubMed] [Google Scholar]
- 39.Bloomington, MN, USA: Institute for Clinical Systems Improvement; 2004. [Last accessed on 2014 Jun 09]. Institute for Clinical Systems Improvement. Management of Type 2 Diabetes Mellitus. Available from: http://www.icsi.org/knowledge . [Google Scholar]
- 40.Trigwell P, Taylor JP, Ismail K, Nicholson T, Alibhai M, Gosden C. Minding the Gap. The Provision of Psychological Support and Care for People with Diabetes in the UK. Diabetes UK. 2008. [Last accessed on 2014 Jun 09]. Available from: http://www.diabetes.org.uk/Documents/Reports/Minding_the_Gap_psychological_report.pdf .
- 41.Peyrot M, Rubin RR. Levels and risks of depression and anxiety symptomatology among diabetic adults. Diabetes Care. 1997;20:585–90. doi: 10.2337/diacare.20.4.585. [DOI] [PubMed] [Google Scholar]
- 42.Fisher L, Chesla CA, Mullan JT, Skaff MM, Kanter RA. Contributors to depression in Latino and European-American patients with type 2 diabetes. Diabetes Care. 2001;24:1751–7. doi: 10.2337/diacare.24.10.1751. [DOI] [PubMed] [Google Scholar]
- 43.Hermanns N, Kulzer B, Krichbaum M, Kubiak T, Haak T. How to screen for depression and emotional problems in patients with diabetes: Comparison of screening characteristics of depression questionnaires, measurement of diabetes-specific emotional problems and standard clinical assessment. Diabetologia. 2006;49:469–77. doi: 10.1007/s00125-005-0094-2. [DOI] [PubMed] [Google Scholar]
- 44.Bao AM, Meynen G, Swaab DF. The stress system in depression and neurodegeneration: Focus on the human hypothalamus. Brain Res Rev. 2008;57:531–53. doi: 10.1016/j.brainresrev.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 45.Bonnet F, Irving K, Terra JL, Nony P, Berthezène F, Moulin P, et al. Anxiety and depression are associated with unhealthy lifestyle in patients at risk of cardiovascular disease. Atherosclerosis. 2005;178:339–44. doi: 10.1016/j.atherosclerosis.2004.08.035. [DOI] [PubMed] [Google Scholar]
- 46.Rod NH, Grønbaek M, Schnohr P, Prescott E, Kristensen TS. Perceived stress as a risk factor for changes in health behaviour and cardiac risk profile: A longitudinal study. J Intern Med. 2009;266:467–75. doi: 10.1111/j.1365-2796.2009.02124.x. [DOI] [PubMed] [Google Scholar]
- 47.Björntorp P. Do stress reactions cause abdominal obesity and comorbidities? Obes Rev. 2001;2:73–86. doi: 10.1046/j.1467-789x.2001.00027.x. [DOI] [PubMed] [Google Scholar]
- 48.Vogelzangs N, Kritchevsky SB, Beekman AT, Newman AB, Satterfield S, Simonsick EM, et al. Depressive symptoms and change in abdominal obesity in older persons. Arch Gen Psychiatry. 2008;65:1386–93. doi: 10.1001/archpsyc.65.12.1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Commodari E. Children staying in hospital: A research on psychological stress of caregivers. Ital J Pediatr. 2010;36:40. doi: 10.1186/1824-7288-36-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lustman PJ, Gavard JA. Psychosocial aspects of diabetes adult populations. In: Harris MI, Cowie CC, Stem MP, Boyko EJ, Reiber GE, Bennett PH, editors. Diabetes in America. NIH Publication no. 95-1468. 2nd ed. Washington, DC, U.S: Govt. Printing Office; 1995. pp. 507–17. [Google Scholar]
- 51.Surwit RS, Schneider MS, Feinglos MN. Stress and diabetes mellitus. Diabetes Care. 1992;15:1413–22. doi: 10.2337/diacare.15.10.1413. [DOI] [PubMed] [Google Scholar]
- 52.Lustman PJ, Clouse RE. Depression in diabetic patients: The relationship between mood and glycemic control. J Diabetes Complications. 2005;19:113–22. doi: 10.1016/j.jdiacomp.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 53.Gonzalez JS, Safren SA, Cagliero E, Wexler DJ, Delahanty L, Wittenberg E, et al. Depression, self-care, and medication adherence in type 2 diabetes: Relationships across the full range of symptom severity. Diabetes Care. 2007;30:2222–7. doi: 10.2337/dc07-0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lin EH, Rutter CM, Katon W, Heckbert SR, Ciechanowski P, Oliver MM, et al. Depression and advanced complications of diabetes: A prospective cohort study. Diabetes Care. 2010;33:264–9. doi: 10.2337/dc09-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gonzalez JS, Peyrot M, McCarl LA, Collins EM, Serpa L, Mimiaga MJ, et al. Depression and diabetes treatment nonadherence: A meta-analysis. Diabetes Care. 2008;31:2398–403. doi: 10.2337/dc08-1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gonzalez JS, Safren SA, Delahanty LM, Cagliero E, Wexler DJ, Meigs JB, et al. Symptoms of depression prospectively predict poorer self-care in patients with type 2 diabetes. Diabet Med. 2008a;25:1102–7. doi: 10.1111/j.1464-5491.2008.02535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Katon WJ, Russo JE, Heckbert SR, Lin EH, Ciechanowski P, Ludman E, et al. The relationship between changes in depression symptoms and changes in health risk behaviors in patients with diabetes. Int J Geriatr Psychiatry. 2010b;25:466–75. doi: 10.1002/gps.2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ikeda K, Aoki H, Saito K, Muramatsu Y, Suzuki T. Associations of blood glucose control with self-efficacy and rated anxiety/depression in type II diabetes mellitus patients. Psychol Rep. 2003;92:540–4. doi: 10.2466/pr0.2003.92.2.540. [DOI] [PubMed] [Google Scholar]
- 59.Kneckt MC, Keinänen-Kiukaanniemi SM, Knuuttila ML, Syrjälä AM. Self-esteem as a characteristic of adherence to diabetes and dental self-care regimens. J Clin Periodontol. 2001;28:175–80. doi: 10.1034/j.1600-051x.2001.028002175.x. [DOI] [PubMed] [Google Scholar]
- 60.Mooy JM, de Vries H, Grootenhuis PA, Bouter LM, Heine RJ. Major stressful life events in relation to prevalence of undetected type 2 diabetes: The Hoorn study. Diabetes Care. 2000;23:197–201. doi: 10.2337/diacare.23.2.197. [DOI] [PubMed] [Google Scholar]
- 61.Glasgow RE, Toobert DJ, Riddle M, Donnelly J, Mitchell DL, Calder D, et al. Diabetes-specific social learning variables and self-care behaviors among persons with type II diabetes. Health Psychol. 1989;8:285–303. doi: 10.1037//0278-6133.8.3.285. [DOI] [PubMed] [Google Scholar]
- 62.Aikens JE, Mayes R. Elevated glycosylated albumin in NIDDM is a function of recent everyday environmental stress. Diabetes Care. 1997;20:1111–3. doi: 10.2337/diacare.20.7.1111. [DOI] [PubMed] [Google Scholar]
- 63.Toobert DJ, Glasgow RE. Problem solving and diabetes self-care. J Behav Med. 1991;14:71–86. doi: 10.1007/BF00844769. [DOI] [PubMed] [Google Scholar]
- 64.Anderson RJ, Grigsby AB, Freedland KE, de Groot M, McGill JB, Clouse RE, et al. Anxiety and poor glycemic control: A meta-analytic review of the literature. Int J Psychiatry Med. 2002;32:235–47. doi: 10.2190/KLGD-4H8D-4RYL-TWQ8. [DOI] [PubMed] [Google Scholar]
- 65.Lustman PJ, Clouse RE, Carney RM. Depression and the reporting of diabetes symptoms. Int J Psychiatry Med. 1988;18:295–303. doi: 10.2190/lw52-jfkm-jchv-j67x. [DOI] [PubMed] [Google Scholar]
- 66.Clouse RE, Lustman PJ. Gastrointestinal symptoms in diabetic patients: Lack of association with neuropathy. Am J Gastroenterol. 1989;84:868–72. [PubMed] [Google Scholar]
- 67.Lustman PJ, Clouse RE. Relationship of psychiatric illness to impotence in men with diabetes. Diabetes Care. 1990;13:893–5. doi: 10.2337/diacare.13.8.893. [DOI] [PubMed] [Google Scholar]
- 68.Turkington RW. Depression masquerading as diabetic neuropathy. JAMA. 1980;243:1147–50. [PubMed] [Google Scholar]
- 69.MacLean D, Lo R. The non-insulin-dependent diabetic: Success and failure in compliance. Aust J Adv Nurs. 1998;15:33–42. [PubMed] [Google Scholar]
- 70.Garratt AM, Schmidt L, Fitzpatrick R. Patient-assessed health outcome measures for diabetes: A structured review. Diabet Med. 2002;19:1–1. doi: 10.1046/j.1464-5491.2002.00650.x. [DOI] [PubMed] [Google Scholar]
- 71.Beeney LJ, Bakry AA, Dunn SM. Patient psychological and information needs when the diagnosis is diabetes. Patient Educ Couns. 1996;29:109–16. doi: 10.1016/0738-3991(96)00939-1. [DOI] [PubMed] [Google Scholar]
- 72.Chandra P. Psychological aspects of diabetes. Int J Diab Dev Ctries. 1997;17:111–2. [Google Scholar]
- 73.Piotrowski M, Sochalski JA. Learning to Live with Diabetes. Michigan Diabetes Research and Training Center. Univ of Michigan; 1980. [Google Scholar]
- 74.Sridhar GR, Madhu K. Psychosocial and cultural issues in diabetes mellitus. Curr Sci. 2002;83:1556–64. [Google Scholar]
- 75.Kübler-Ross E, Wessler S, Avioli LV. On death and dying. JAMA. 1972;221:174–9. doi: 10.1001/jama.1972.03200150040010. [DOI] [PubMed] [Google Scholar]
- 76.Bajaj S, Jawad F, Islam N, Mahtab H, Bhattarai J, Shrestha D, et al. South Asian women with diabetes: Psychosocial challenges and management: Consensus statement. Indian J Endocrinol Metab. 2013;17:548–62. doi: 10.4103/2230-8210.113720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fu AZ, Qiu Y, Radican L. Impact of fear of insulin or fear of injection on treatment outcomes of patients with diabetes. Curr Med Res Opin. 2009;25:1413–20. doi: 10.1185/03007990902905724. [DOI] [PubMed] [Google Scholar]
- 78.Patni P, Varghese D, Balekar N, Jain DK. Needle-free insulin drug delivery. Indian J Pharm Sci. 2006;68:7–12. [Google Scholar]
- 79.Abu Hassan H, Tohid H, Mohd Amin R, Long Bidin MB, Muthupalaniappen L, Omar K, et al. Factors influencing insulin acceptance among type 2 diabetes mellitus patients in a primary care clinic: A qualitative exploration. BMC Fam Pract. 2013;14:164. doi: 10.1186/1471-2296-14-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mollema ED, Snoek FJ, Adèr HJ, Heine RJ, van der Ploeg HM. Insulin-treated diabetes patients with fear of self-injecting or fear of self-testing: Psychological comorbidity and general well-being. J Psychosom Res. 2001;51:665–72. doi: 10.1016/s0022-3999(01)00229-x. [DOI] [PubMed] [Google Scholar]
- 81.Wild D, von Maltzahn R, Brohan E, Christensen T, Clauson P, Gonder-Frederick L, et al. A critical review of the literature on fear of hypoglycemia in diabetes: Implications for diabetes management and patient education. Patient Educ Couns. 2007;68:10–5. doi: 10.1016/j.pec.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 82.Balhara YP. Diabetes and psychiatric disorders. Indian J Endocrinol Metab. 2011;15:274–83. doi: 10.4103/2230-8210.85579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nefs G. Diabetes and Emotional Distress: The Need for a Personalized Approach. 2013. [Last accessed on 2014 Jun 09]. Available from: http://www.arno.uvt.nl/show.cgi?fid=132249.https://pure.uvt.nl/portal/files/1515360/Nefs_diabetes_31-05-2013.pdf .
- 84.Nouwen A, Winkley K, Twisk J, Lloyd CE, Peyrot M, Ismail K, et al. Type 2 diabetes mellitus as a risk factor for the onset of depression: A systematic review and meta-analysis. Diabetologia. 2010;53:2480–6. doi: 10.1007/s00125-010-1874-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Campayo A, Gómez-Biel CH, Lobo A. Diabetes and depression. Curr Psychiatry Rep. 2011;13:26–30. doi: 10.1007/s11920-010-0165-z. [DOI] [PubMed] [Google Scholar]
- 86.Katon WJ, Von Korff M, Lin EH, Simon G, Ludman E, Russo J, et al. The pathways study: A randomized trial of collaborative care in patients with diabetes and depression. Arch Gen Psychiatry. 2004;61:1042–9. doi: 10.1001/archpsyc.61.10.1042. [DOI] [PubMed] [Google Scholar]
- 87.Ali S, Stone MA, Peters JL, Davies MJ, Khunti K. The prevalence of co-morbid depression in adults with type 2 diabetes: A systematic review and meta-analysis. Diabet Med. 2006;23:1165–73. doi: 10.1111/j.1464-5491.2006.01943.x. [DOI] [PubMed] [Google Scholar]
- 88.Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: A meta-analysis. Diabetes Care. 2008;31:2383–90. doi: 10.2337/dc08-0985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Golden SH, Lazo M, Carnethon M, Bertoni AG, Schreiner PJ, Diez Roux AV, et al. Examining a bidirectional association between depressive symptoms and diabetes. JAMA. 2008;299:2751–9. doi: 10.1001/jama.299.23.2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Huang CJ, Chiu HC, Lee MH, Wang SY. Prevalence and incidence of anxiety disorders in diabetic patients: A national population-based cohort study. Gen Hosp Psychiatry. 2011;33:8–15. doi: 10.1016/j.genhosppsych.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 91.Grigsby AB, Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. Prevalence of anxiety in adults with diabetes: A systematic review. J Psychosom Res. 2002;53:1053–60. doi: 10.1016/s0022-3999(02)00417-8. [DOI] [PubMed] [Google Scholar]
- 92.Eren I, Erdi O, Sahin M. The effect of depression on quality of life of patients with type II diabetes mellitus. Depress Anxiety. 2008;25:98–106. doi: 10.1002/da.20288. [DOI] [PubMed] [Google Scholar]
- 93.Lewis R. Diabetic emergencies: Part 1. Hypoglycaemia. Accid Emerg Nurs. 1999;7:190–6. doi: 10.1016/s0965-2302(99)80049-6. [DOI] [PubMed] [Google Scholar]
- 94.MacLullich AM, Beaglehole A, Hall RJ, Meagher DJ. Delirium and long-term cognitive impairment. Int Rev Psychiatry. 2009;21:30–42. doi: 10.1080/09540260802675031. [DOI] [PubMed] [Google Scholar]
- 95.Han JH, Shintani A, Eden S, Morandi A, Solberg LM, Schnelle J, et al. Delirium in the emergency department: An independent predictor of death within 6 months. Ann Emerg Med. 2010;56:244–520. doi: 10.1016/j.annemergmed.2010.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Crow S, Kendall D, Praus B, Thuras P. Binge eating and other psychopathology in patients with type II diabetes mellitus. Int J Eat Disord. 2001;30:222–6. doi: 10.1002/eat.1077. [DOI] [PubMed] [Google Scholar]
- 97.Jones JM, Lawson ML, Daneman D, Olmsted MP, Rodin G. Eating disorders in adolescent females with and without type 1 diabetes: Cross sectional study. BMJ. 2000;320:1563–6. [PMC free article] [PubMed] [Google Scholar]
- 98.Morse SA, Ciechanowski PS, Katon WJ, Hirsch IB. Isn’t this just bedtime snacking? The potential adverse effects of night-eating symptoms on treatment adherence and outcomes in patients with diabetes. Diabetes Care. 2006;29:1800–4. doi: 10.2337/dc06-0315. [DOI] [PubMed] [Google Scholar]
- 99.Kohen D. Diabetes mellitus and schizophrenia: Historical perspective. Br J Psychiatry Suppl. 2004;47:S64–6. doi: 10.1192/bjp.184.47.s64. [DOI] [PubMed] [Google Scholar]
- 100.Cohn T. The link between schizophrenia and diabetes. Curr Psychiatry. 2012;11:29–46. [Google Scholar]
- 101.Expert Group. ‘Schizophrenia and diabetes 2003’ expert consensus meeting, Dublin, 3-4 October 2003: Consensus summary. Br J Psychiatry Suppl. 2004;47:S112–4. [PubMed] [Google Scholar]
- 102.Davis WK, Hess GE, Hiss RG. Psychosocial correlates of survival in diabetes. Diabetes Care. 1988;11:538–45. doi: 10.2337/diacare.11.7.538. [DOI] [PubMed] [Google Scholar]
- 103.Delamater AM, Jacobson AM, Anderson B, Cox D, Fisher L, Lustman P, et al. Psychosocial therapies in diabetes: Report of the Psychosocial Therapies Working Group. Diabetes Care. 2001;24:1286–92. doi: 10.2337/diacare.24.7.1286. [DOI] [PubMed] [Google Scholar]
- 104.Fosbury JA, Bosley CM, Ryle A, Sönksen PH, Judd SL. A trial of cognitive analytic therapy in poorly controlled type I patients. Diabetes Care. 1997;20:959–64. doi: 10.2337/diacare.20.6.959. [DOI] [PubMed] [Google Scholar]
- 105.Ismail K, Maissi E, Thomas S, Chalder T, Schmidt U, Bartlett J, et al. A randomised controlled trial of cognitive behaviour therapy and motivational interviewing for people with type 1 diabetes mellitus with persistent sub-optimal glycaemic control: A Diabetes and psychological therapies (ADaPT) study. Health Technol Assess. 2010;14:1. doi: 10.3310/hta14220. [DOI] [PubMed] [Google Scholar]
- 106.Rubak S, Sandbæk A, Lauritzen T, Borch-Johnsen K, Christensen B. Effect of “motivational interviewing” on quality of care measures in screen detected type 2 diabetes patients: A one-year follow-up of an RCT, ADDITION Denmark. Scand J Prim Health Care. 2011;29:92–8. doi: 10.3109/02813432.2011.554271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hill-Briggs F, Gemmell L. Problem solving in diabetes self-management and control: A systematic review of the literature. Diabetes Educ. 2007;33:1032–50. doi: 10.1177/0145721707308412. [DOI] [PubMed] [Google Scholar]
- 108.Grey M, Boland EA, Davidson M, Yu C, Sullivan-Bolyai S, Tamborlane WV, et al. Short-term effects of coping skills training as adjunct to intensive therapy in adolescents. Diabetes Care. 1998;21:902–8. doi: 10.2337/diacare.21.6.902. [DOI] [PubMed] [Google Scholar]
- 109.Fisher EB, Thorpe CT, Devellis BM, Devellis RF. Healthy coping, negative emotions, and diabetes management: A systematic review and appraisal. Diabetes Educ. 2007;33:1080–103. doi: 10.1177/0145721707309808. [DOI] [PubMed] [Google Scholar]
- 110.Wysocki T, Harris MA, Greco P, Bubb J, Danda CE, Harvey LM, et al. Randomized, controlled trial of behavior therapy for families of adolescents with insulin-dependent diabetes mellitus. J Pediatr Psychol. 2000;25:23–33. doi: 10.1093/jpepsy/25.1.23. [DOI] [PubMed] [Google Scholar]
- 111.Anderson BJ, Brackett J, Ho J, Laffel LM. An office-based intervention to maintain parent-adolescent teamwork in diabetes management. Impact on parent involvement, family conflict, and subsequent glycemic control. Diabetes Care. 1999;22:713–21. doi: 10.2337/diacare.22.5.713. [DOI] [PubMed] [Google Scholar]
- 112.Betts P, Buckley M, Davies R, McEvilly E, Swift P. The care of young people with diabetes. Diabet Med. 1996;13:S54–9. [PubMed] [Google Scholar]
- 113.A desktop guide to type 1 (insulin-dependent) diabetes mellitus. European Diabetes Policy Group 1998. Diabet Med. 1999;16:253–66. [PubMed] [Google Scholar]
- 114.Sridhar GR. Depression and mental disorders in obese subjects with diabetes, chapter 11- Advances in diabetes novel insights, The Health Sciences Publisher. 2016;2:137–147. [Google Scholar]
- 115.Rasgon N, Jarvik L. Insulin resistance, affective disorders, and Alzheimer's disease: review and hypothesis. J Gerontology. 2004;59:178–83. doi: 10.1093/gerona/59.2.m178. [DOI] [PubMed] [Google Scholar]
- 116.Sridhar GR, Madhu K. Psychosocial and cultural issues in diabetes mellitus. Curr Sci. 2002;83:1556–64. [Google Scholar]


