Abstract
Background
People living with dementia (PWD) and their informal caregivers often report difficulties in maintaining their usual activities. Several dyadic, psychosocial, activating interventions were developed to create insight into how to cope with limitations in a practical way and to increase skills for maintaining personal activities. Effects of these interventions varied so far. More knowledge on the working mechanisms of activating interventions might help to increase their impact. This study will provide more insights into the working mechanisms of three dyadic, psychosocial, activating interventions as the participating PWD, caregivers, and coaches perceived them during the interventions.
Participants and methods
We used a qualitative design with semi-structured interviews of 34 dyads that included 27 PWD, 34 caregivers, and 19 coaches. The data were analyzed with the constant comparative method.
Results
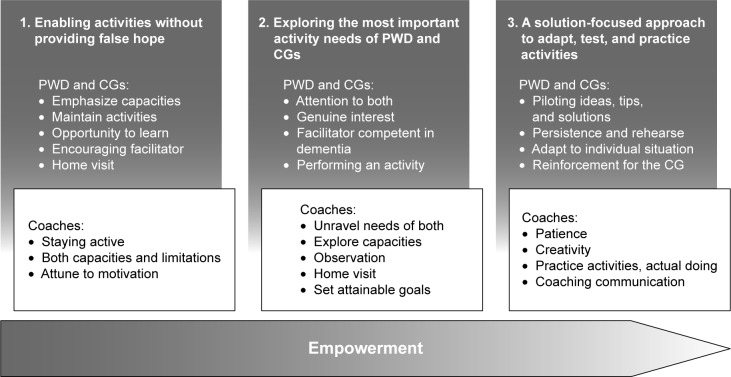
Many PWD and caregivers found capacity-building approaches beneficial. We identified “empowerment” as the core theme. Three working mechanisms explained why the interventions were perceived as having a beneficial impact: 1) enabling activities without providing false hope; 2) exploring the most important personal activity needs of the PWD and caregivers; and 3) a solution-focused approach to adapt, test, and practice activities. An individualized approach contributed to positive change.
Conclusion
For the overarching working mechanism empowerment, expertise in the field of dementia and psychological skills of coaches seem to be important. Assessing the needs, capacities, and limitations of both the PWD and the caregivers to take part in activities seems to be key, as well as the communication about it and the skills to teach a solution-focused approach. Studies on the impact of psychosocial and activating interventions might benefit from considering outcome measures directed at empowerment, along with aspects such as hope and belief in one’s own capacities versus traditional outcome measures as mood, burden, or quality of life.
Keywords: occupational therapy, exercise, pleasant events, psychosocial interventions, working mechanisms, components
Introduction
Worldwide, 50 million persons with dementia have to cope with the daily consequences.1 There is currently no cure for dementia. Dyadic psychosocial interventions aim at supporting both people living with dementia (PWD) and their informal caregivers (usually spouses or children).2,3 PWD often report difficulties in performing their usual activities.4,5 Daily activities are important because they can create structure, satisfaction, and continuity in life, and they contribute to well-being and health.6–8 It is difficult for caregivers to engage in joint social activities with PWD.9 Furthermore, due to their caregiving tasks, they have difficulty maintaining their own activities as well.10,11 Some psychosocial interventions take these challenges as a starting point and are focused on engaging both PWD and caregivers in activities.12–20 They aim at increasing skills for maintaining participation in activities and how to cope with declines in capacities in a practical way and to increase self-management.21,22 These multicomponent interventions comprise performing activities, psychoeducation, and emotional support. In this study, we label these interventions “activating interventions.”
Studies show benefits of activating interventions, but the effects vary widely, from no effects at all to large effects on PWD outcomes, such as outcomes for mood, behavior, activities of daily living (ADL) dependency, and quality of life. This is also true for caregiver outcomes such as mood, burden, competency, and quality of life.12–15,18,19,23–29 Some authors address the issue that knowledge on the impact of different components in multicomponent interventions is lacking.3,30–32 A few studies provide information about the relation between treatment components and effects. Pinquart and Sorensen showed positive effects of counseling and psychoeducation for the caregiver’s active engagement.33 Van’t Leven et al showed a relation between skills training of PWD and their ADL independence and a relation between training of caregivers’ communication skills and their competence.3 Furthermore, Brodaty and Asaratnam reported indications for delivery characteristics of successful multicomponent interventions. These indications are: the interventions that are multicomponent, tailored to the needs of PWD and caregivers, include 9–12 sessions, and are delivered at home. They are interspersed with telephone sessions and individual or group follow-ups.30 Olazaran et al, however, could not conclude that any relation existed between the effects of either treatment components or delivery characteristics in their review.32
More knowledge on working mechanisms of the interventions may add to more effective support for PWD and caregivers. In this study, we concentrate on dyadic, psychosocial, activating interventions because of the PWD’ and caregivers’ activity losses that are consequences of dementia in daily life. We used data from studies about three activating interventions: the Pleasant Events Program, the Exercise and Support Intervention for People with Dementia and their Caregivers, and the Community Occupational Therapy in Dementia guideline.12,16,17,19,20 These interventions aim at increasing skills to cope with the consequences of dementia. They are all dyadic, training activities, and they are delivered at home. Table 1 provides a detailed description of the treatment components, the evidence found in effect studies, and the organizational structure in which the interventions were offered to PWD–caregiver dyads.
Table 1.
Interventions: treatment components, evidence, and provision of the interventions
| Pleasant events program12,19,20 | Exercise and support intervention for people with dementia and their caregivers17,18 | Community occupational therapy in dementia16,24,29 | |
|---|---|---|---|
| Primary goal | Maintaining activity, having pleasant activities, and preventing depression of PWD and CGs | Improving mood and physical health of PWD and CGs and decreasing burden of CGs | Improving the performance of daily activities of PWD and mitigating the care burden of CGs |
| Components | – Choosing and planning pleasant activities for PWD and CGs or both, – Practicing these activities, – Adjusting activities to the capabilities of PWD, – Psychoeducation, and – Homework: pleasant activities |
– Exercises for flexibility, balance, power, and stamina of PWD and the CGs, supervised by a coach at home, – Identifying pleasant activities for both, – Psychoeducation and communication training, and – Homework: repeating mobility exercises and pleasant activities (preferred at least three times a week) |
– Needs assessment and observation, – Practicing meaningful, daily activities (self-sufficiency) with compensation strategies and adjustments for PWD, – Psychoeducation, – Practicing different ways with CGs of approaching PWD, and – Homework: individual appointments for practicing activities and approach |
| Duration | A maximum of six home visits of 1.5 hours each, weekly, and biweekly | A maximum of 8 home visits of 1 hour each, four times weekly, four times biweekly | A maximum of 10 home visits of 1 hour each, two times a week, weekly, and biweekly |
| Original interventions | This program is based on the behavioral treatment of depression in dementia program.19 The Dutch manual for the program was published by Dutch Institute for Primary Health Care20 and is supplemented by examples from Gitlin et al’s program12 | This intervention is based on reducing disability in Alzheimer’s disease.18 After a pilot study with the original program, this program was adapted. Attributes such as a ball, weights, and elastic equipment made the exercises more attractive for people with dementia. The number of sessions was limited to eight. This program emphasized the pleasant events component and the training for activating events, beliefs, and consequences was included in the psychoeducation for CGs17 | This therapy is described in Graff et al.16,24,45 Four sessions of diagnostics and goal defining to priorities meaningful activities. Next compensatory strategies to adapt activities for PWD and the use of environmental modifications are trained, and the CG is trained in supervision skills |
| Evidence | Significant effects (posttreatment) for PWD on – Depression (CDS: p<0.01; ES: 1.7) and for CG – Depression (HDRS: p<0.01) n (I/C): 23 of 2019 Significant effects (4 months) for PWD on – Activity engagement (p=0.029; 95% CI =0.02–0.41) – Frequency of agitated behavior (p=0.009; 95% CI =−0.55 to −0.09) and for CG on – Mastery (p=0.013; 95% CI =0.08–0.60) – Confidence using activities (p=0.011; 95% CI =0.41–2.94) n (I/C): 27 of 2912 |
Significant effects (3 months) for PWD on – Depression (CDS: p=0.02; MED =−1.03 (95% CI =−0.17 to 1.19) – General health (SP-36: p<0.001; MED 19.29 (95% CI =8.75 to 29.83) n (I/C): 76 of 7718 Significant effect (3 and 6 months for PWD on – Attention span of PWD (p=0.04; ES: 0.25) n (I/C): 57 of 5426 Effects were not demonstrated in a RCT with the adjusted program25,27 |
Significant effects (3 months) for PWD on – Daily functioning (AMPS process: p<0.0001; ES 2.7) – Depression (CDS: p<0.0001; ES: 0.7) – General health (GHQ: p<0.0001; ES: 0.7) – Quality of life (DQoL: p<0.0001; ES: 1.1) and for CGs – Competence (SCQ: p<0.0001; ES: 0.8) – Depression (CES-D: p<0.0001; ES: 1.3) – General health (GHQ: p=0.001; ES: 1.1) – Quality of life (DQoL: p<0.0001; ES: 1.5) n (I/C): 68 of 6724,29 These effects were not demonstrated in other studies23,28 |
| Organizational structure | The program was offered as part of the Academic Collaborative Centre for Dementia, which entails the collaboration of Rotterdam Uni versity, the Home Care Organization De Zellingen and the Van Kleef Institute (for generating and disseminating knowledge for home care professionals). The coaches were students graduating in health care studies and home-care workers from De Zellingen. They were supervised during the intervention. The project leader and case manager in the region recruited participants | The program was offered within an RCT from the Department of Clinical Psychology, VU University, Amsterdam.17 The coaches were master students from the Department of Clinical Psychology, VU University, who completed a special training program for geropsychology. They were supervised during the project. The project leader recruited participants for the program with the help of caregiver organizations, local Alzheimer cafes (public meetings for people with dementia, their caregivers, and others), and case managers throughout the Netherlands | Occupational therapy was regularly offered and delivered by certified occupational therapists who followed an additional training for this program. The participants were referred by general practitioners and geriatricians as well as case managers throughout the Netherlands |
Notes: Adapted from Van’t Leven et al.46
Abbreviations: AMPS, Assessment of Motor and Process Skills; CDS, Cornell Depression Scale; CES-D, Centre of Epidemic Studies – Depression; CG, informal caregiver; DQoL, Dementia Quality of Life Instrument; ES, effect size; GHQ, General Health Questionnaire; HDRS, Hamilton Depression Rating Scale; MED, mean estimated difference; n (I/C), study population intervention/control group; PWD, people living with dementia; RCT, randomized controlled trial; SCQ, Sense of Competence Questionnaire; SP-36, Sickness Profile-36.
The aim of our study was to provide more insights into the working mechanisms of three dyadic, psychosocial, activating interventions as the participating PWD, caregivers, and guiding coaches perceived them during the intervention. We define “working mechanisms” as “specific processes within psychosocial interventions which appear to contribute to positive changes,” according to Dugmore et al.31
Participants and methods
Design
We used a qualitative design with semi-structured interviews to gather in-depth information about intervention processes that contributed to positive change for the participating dyads.34,35 We wanted to explore the perspectives of participating PWD and caregivers, as well as the perspectives of the coaches who guided them during the intervention.
Ethical considerations
Ethical approval for interviews with the participating dyads was obtained as part of the approving process of the ethics committees for the Pleasant Events Program and the Exercise and Support Intervention (Medical Ethics Review Committee of the Erasmus Medical Center, Rotterdam, the Netherlands [number 2009-117] and the Medical Ethics Review Committee of the VU University Medical Center, Amsterdam, the Netherlands [number 2008/320]). Ethical approval was obtained separately for the interviews with participants in the Occupational Therapy Intervention (Medical–Ethical Review Committee for Mental Health Care, Rotterdam, the Netherlands [number 11.123]). The dyads consented to the study procedures, including participation in evaluative interviews. The approval for the Pleasant Events Program and Occupational Therapy Intervention included written informed consent from the caregiver who signed for the dyad. The approval for the Exercise and Support Intervention included written informed consent from both the PWD and the caregivers.
Recruitment and participants
For the Pleasant Events Program and the Exercise and Support Intervention, the project managers asked the participants (a total of 23 dyads) and the coaches if they were willing to participate in an interview. All but one dyad agreed to be interviewed. For the Occupational Therapy Intervention, which was reimbursed under the Dutch Health Insurance Act, we contacted occupational therapists and asked them to identify clients willing to participate in an interview. We contacted 51 occupational therapists. Nine of them identified 16 dyads who were willing to participate in an interview. Thus, a convenience sample was composed of 38 cases, consisting of a person with dementia, a caregiver, and a coach in each. The other occupational therapists had no referrals for these activating interventions for PWD (26); some indicated that they were too busy to take part (3), and others thought it is too burdening for the dyad(s) they coached (2), or the dyad(s) had quit early (1), and the reason is unknown (10).
Upon receiving names and contact details, the interviewer (NL or Anna-Eva Prick [AEP]) phoned the dyad, explaining again the goal of the interview and the study. If both the person with dementia and the caregiver were still willing to be interviewed, an appointment was made. Four dyads cancelled their interviews because of the burden or illness. Eventually 34 dyads (9 for the Pleasant Events Program, 11 for the Exercise and Support Intervention, and 14 for the Occupational Therapy Intervention) were interviewed. We interviewed 19 coaches, who guided 28 dyads. The coaches consisted of professional occupational therapists, master students of geropsychology, fourth-year health care students, and homecare workers, all with the supervision of an experienced psychologist or occupational therapist. Table 2 provides more information about the participants.
Table 2.
Participants
| 34 Cases | Mean age/(range) years | Male/female | Relation | Onset of dementia: (mean) | Care services used by dyads | Interviewed cases |
|---|---|---|---|---|---|---|
| People living with dementia | 78 (62–93) | 22/12 (65%/35%) | 1–5 years (2.6) | Geriatrician/general physician 24 × case manager |
27a | |
| Informal caregivers | Partners: 75 (61–88) Children: 53 (45–65) |
9 of 25 (27%/73%) | 28 partners 6 children |
17 × meeting center or day care 8 × home care 3 × speech therapy 1 × pastoral worker 9 × informal care support/volunteer/Alzheimer café |
34 | |
| Professional experience: | ||||||
| Coaches | 0–30 Years | 28b |
Notes:
Not all persons with dementia were able to participate in an interview.
Some coaches were involved in more than one case.
Data collection
We aimed at interviewing both members of the dyad, either together or separately, whichever they preferred. Seven caregivers said that the partner or parent with dementia could no longer reflect on their experiences, and a joint interview would be too burdensome for them. Only the caregivers in these dyads were interviewed. In two interviews, a daughter was present in addition to the person with dementia and caregiver. All interviews started with an open question about their experiences with the intervention. The follow-up questions for the PWD addressed the main topics or activities in the intervention and what they had learned from participating. Nonverbal signs such as frowning were interpreted as prompts to pose a question in another way or to investigate the answer further. Follow-up questions for the caregivers addressed the topics, activities, what had been learned, what had been changed, and how or why. The interviews with the dyads lasted from 50 to 120 minutes, with a mean of 75 minutes. The interviews took place at the homes of the dyads, except for one caregiver who was interviewed by phone. AEP conducted seven interviews with dyads in the Exercise and Support Intervention. NL conducted all the other interviews.
The interviews with the coaches took place after the interview with the dyad, and they also began with an open question about the coach’s experience with the intervention with that particular dyad. Follow-up questions addressed the achieved results, how the coach tailored the intervention to the needs and preferences of the dyad, and what was not achieved. The interviews with the coaches lasted 20–30 minutes. These interviews took place at their workplaces (12), at their homes (4), at a public place (2), or by phone (1).
Field notes were taken during all interviews. All face-to-face interviews were digital audio-recorded and transcribed verbatim. Notes were taken during the two interviews by phone and transcribed extensively immediately afterward. All transcripts and field notes were imported into Atlas-ti-6/7.1 to facilitate qualitative analysis.36
Data analysis
We performed a conventional content analysis, following an iterative and reflexive process based on the constant comparative method.37,38
Stage 1
Three researchers (NL, JL, and AEP) coded the interviews for the first four cases independently. There was an agreement about the selection of significant sections. The codes used for the treatment components were given in the intervention manuals, such as those for the chosen activities or exercises, instructions for PWD, homework, needs inventory, adaptations, and open codes for PWD, such as telling their story and being heard and staying active; for caregivers, practical advice and reinforcement; for coaches, communication, revealing needs, and memory aids. We also coded the effects as the PWD–caregiver dyad perceived them; there were effects such as self-confidence, pleasure, new ideas, and more knowledge. Differences were discussed, and a preliminary code tree was composed. NL used this code tree to analyze seven cases again. After 11 cases had been done, each case was summarized, and the working mechanisms of each case and the effects as perceived by the interviewees were described.
Stage 2
The research team discussed the results based on the 11 cases. The codes were grouped into more abstract categories that covered what contributed to positive change for the dyads, such as the importance of activities, attention for both capacities and limitations, confidence in the coach, hope, and individualized adaptations. The code tree was changed as necessary. Next, 10 new cases were coded, and the 11 cases that had been coded were recoded in accordance with the new code tree. After recoding the 21 interviews, more categories were formulated, such as actually doing things together with PWD, emphasis on potential possibilities, the coach’s expertise in dementia, and the coach’s creativity. We recognized three themes in these categories.
Stage 3
These themes and categories were deepened with the experiences of the last 13 cases.
Stage 4
Then, we identified one encompassing theme with three subthemes.
Results
We identified “empowerment” as the core theme in the stories of our participants, eg, focusing on remaining capacities, searching for strengths that could compensate for limitations, and increasing self-confidence without denying limitations. Thus, a dyad was enabled to get a grip on their situation and find out what works for them by themselves. The PWD and caregivers appreciated the positive approach of focusing on capabilities instead of failures. Some dyads saw the intervention as a training course to learn how to cope with their situation by improving their capacities instead of a therapy focusing on problems. The emphasis was on “getting a grip on their situation” rather than on “being in need of help.” Some coaches noticed that the dyads had already discussed their daily problems with other care professionals. Often these professionals acknowledged that their problems were a consequence of dementia, but they had not proposed ways of dealing with the problems and compensating for limitations. Three working mechanisms emerged within the core theme of empowerment, which were present in all three interventions: 1) enabling activities without providing false hope; 2) exploring the most important personal activity needs of the PWD and the caregiver; and 3) a solution-focused approach to adapt, test, and practice activities. An individualized combination (rather than single components) of these working mechanisms, tailored to the needs and capacities of the dyad, contributed to positive change. Figure 1 shows working mechanisms and components.
Figure 1.
Working mechanisms.
Abbreviations: CG, informal caregiver; PWD, people living with Dementia.
Working mechanism 1: enabling activities without providing false hope
This mechanism involves emphasizing capacities instead of limitations in a realistic way. This made the PWD and caregivers more aware of qualities that were still intact. The participants said they focused on maintaining activities, while acknowledging difficulties in the performance.
The therapist insisted that I should keep doing what I used to do. I felt inclined to pull back, but now I say to myself, if I stop, there will be nothing left. [A person with dementia]
Some participants reflected on the intervention as “an opportunity to learn,” as if it was a training course to get better equipped for the situation.
Both PWD and caregivers often spoke of the coach’s encouragement and positive approach. As a result, the dyads were more accepting of the intervention and wanted to “give it a try.” All coaches emphasized the subtle and difficult balance between a focus on possibilities and staying active, but also recognized the reality of the dyad’s situation, including limitations. They found it challenging to explain that maintaining daily and recreational activities may help to cope with the dementia process, although the activities could not relieve grief and feelings of loss. They needed to show enthusiasm and optimism, but had to avoid creating false hope. Especially the first contact was important for exploring the participants’ interest in the intervention and attuning to their motivation. The dyads were more comfortable if the first contact took place in a home visit because they felt more at ease in their own homes.
Several respondents told us that the immediate aftermath of receiving the diagnosis was still affecting them at the time of the interview. In their perception, the physician had told them there was no therapy for them: “nothing can be done about it.” For some participants, this message confirmed their own premises of dementia that “it is all over.” They had lost their belief in their own capacities and had become apathetic.
After the diagnosis, my father [with dementia] slept the whole day, while he used to be busy all the time. The geriatrician suggested day care on a farm, but my father felt “too good for this.” To gain insight into his activities, the occupational therapist asked him to write down what he did during the day.
The result was that in the morning he wrote down all kinds of activities to do, and the rest of the day he actually performed them. [Daughter]
When she (the occupational therapist) visited me again, I could show her my notes. [Father]
So, this approach, directed at what he was still able to do, did help him. [Daughter]
Working mechanism 2: exploring the most important personal activity needs of PWD and caregivers
This mechanism is about accurate, detailed exploration of needs of both PWD and caregivers and assessing physical and cognitive limitations of PWD as well as identifying the remaining capacities and usable coping strategies of both. The dyads thought it is important that their personal needs formed the core of the interventions, rather than being offered a predefined intervention program. The PWD recognized the genuine interest in themselves as individuals; they did not merely represent instances of a disease. The caregivers, too, said that attention for them as individuals was more helpful than being regarded only as caregivers.
I could show people who I am in a way. Well, I liked that very much. [A person with dementia]
In fact, it was the first time I told the story of your dementia from my perspective. [His caregiver]
Feeling that the coach understood them was extremely important. Feeling understood meant that the coach listened well, was familiar with the diagnosis, understood the perceived difficulties, and maintained a positive attitude. Common was that the coaches inquired not only about the daily pattern of activities, but also about previous activities and important events in the lives of the dyad. This helped them uncover the dyad’s perspective and gain the dyad’s confidence.
The coach explored their needs and challenges with regard to activities. It was often difficult to puzzle out the dyad’s real needs. Although some caregivers asked concrete questions such as “Can he or she (person with dementia) learn to use a mobile phone?”, others asked general, sometimes unrealistic questions. The PWD said that they wanted “to cope with memory problems” or wished “to be as the way they used to be before.” Several caregivers wanted to know how to support the person with dementia, how to keep him or her active, or how to cope with feelings of burden. Often needs were formulated as wishes. The coaches explored those wishes and activities in detail with them and tried to uncover what a dyad really missed.
It took some effort finding out the needs of this caregiver and the right way to approach him. I had to make him find out for himself instead of telling him. [Coach]
Nearly, all the participants found actually doing activities or exercises with the coach helpful. Several PWD could still reflect on this and had perceived it as collaboration with the coach which made them feel more involved. However, one other person with dementia had experienced it negatively, as a way of being tested. Most of the caregivers were confident that the coach had a realistic picture of the capacities of the person with dementia. The coaches needed insight into capacities, including declines in cognitive and physical functioning, of both PWD and caregivers. This could be obtained by observation and performing activities together. Furthermore, this allowed insight into the communication between the person with dementia and the caregiver. Visiting a dyad at home helped the coaches build confidence and gave them insight into their individual daily routines. This information, together with the clarified needs, enabled the coach and the dyad to set attainable goals that matched in the intervention.
Working mechanism 3: a solution-focused approach to adapt, test, and practice activities
This mechanism is about the practical adjustment of meaningful activities to personal capacities and experimenting with new ways of overcoming problems. Adapted ways of performing activities were established through repetition as a new routine. We recognized a solution-focused approach by piloting adaptations in collaboration with the coach, the person with dementia, and the caregiver. Patience and persistence were needed to find an individual, tailored approach. The coaches needed creativity when searching for appropriate activities, tailored exercises, and adaptations to the individual needs of the PWD and caregivers. The actual doing often created ideas for possible adaptations of activities or exercises, which sometimes had not been foreseen. The coaches used expressions such as “it turned out that…” or after some attempts “then suddenly we found out that….”
Her daughter wanted to encourage her because she was just sitting there the whole day. As a pianist, she had given concerts in earlier days. After a few visits, she was willing to sit with me at the piano, and fortunately she started to play (because I couldn’t…). I asked her to write down in her diary: play a few times a week, and she wrote: “Mind the piano!” Her neighbors told the daughter that they heard her playing. [Coach of a woman with dementia, living on her own with help from her daughter]
The coaches encouraged the dyad and involved them actively; they took on a coaching attitude. The dyads mentioned a variety of actions that had been helpful to them: simplifying activities, using memory aids, changing routines, experimenting with an adapted attitude and adapted instruction, validation of providing good care for the caregivers, and enhancing informal or professional support. Some received adaptations for physical limitations.
Most caregivers felt insecure about their way of providing care, and they were worried that it might be improper or suboptimal. They felt that being empowered to try out several options to manage daily problems was important.
It provided me with the mindset just to try; if it doesn’t work today, maybe I can try again tomorrow. [A caregiver]
Several caregivers mentioned that they already had made some changes themselves and that the intervention had not changed much, but it increased their self-confidence.
Discussion
We identified “empowerment” as the core theme that explained why the interventions were perceived as working according to PWD, caregivers, and their assisting coaches. More specifically, we found three working mechanisms for the beneficial impact of the interventions in the interviews: 1) enabling activities without providing false hope; 2) a detailed exploration of the most important activity needs; and 3) a solution-focused approach to adapt, test, and practice activities.
The first working mechanism enabling activities without providing false hope taught PWD and caregivers to cope with their situation by improving their capacities instead of emphasizing problems. Several dyads reflected very positively on the intervention as a training course instead of needing support. The term “support” was associated with helplessness, whereas the term “training” was associated with maintaining skills.39 Although people living with early dementia and their caregivers experience all kinds of difficulties, they often do not want to be seen as being in need of professional help, which they may perceive as negative and stigmatizing.40 Emphasizing possibilities without providing false hope also means an opening to the future. Realistic beliefs help both PWD and caregivers to cope in a positive manner and to maintain better health and social relationships.41 Especially in the case of progressive diseases such as dementia, there is a thin line between realistic hope and false hope. It is always uncertain whether the benefits of an intervention aiming at maintaining capacities will surpass the decline. Coaches with positive experiences with the interventions can express a certain convincing attitude and enthusiasm.42 The second working mechanism is essential for professionals to provide realistic expectations.
The second working mechanism to empower PWD and caregivers is a detailed exploration of their most important needs for activities and their capacities and limitations. Knowledge about dementia, understanding its consequences in daily life, and knowing how to communicate with PWD and caregivers are necessary to make dyads feel understood and, hopefully, to share their actual needs. Accurate needs assessment, including revealing latent needs, will clarify if and how PWD–caregiver dyads need support to maintain daily activities. In addition, a coach should display a positive attitude and be able to assess mental and physical capacities and limitations related to the performance of activities.43
The third working mechanism is a solution-focused approach to adapt, test, and practice activities, and it is directed at the activity needs of both the person with dementia and the caregiver. To enable activities, it is important to find creative, but also realistic and pragmatic solutions for PWD and caregivers to continue to do activities they value but need adaptation as a result of the disease. Actually doing things and the performance of activities can elicit creative, realistic, and pragmatic solutions that fit both the PWD and their caregivers.44
The respondents always mentioned more than one mechanism, rather than single components, that had been important for beneficial results and emphasized the process. An individualized approach, tailored to the needs and capacities of the dyad, contributed to positive change. Many of the PWD and caregivers shared in the interviews that they felt more self-confident and that some PWD maintained meaningful activities. The dyads found solutions, which they could use for a longer time.
Strengths and limitations
The strength of this study is that we succeeded in interviewing 27 PWD. Many of them could still talk about the intervention or the coach 6 or even 9 months later. It also helped that the caregiver was present at nearly all the interviews and often provided examples of activities that prompted the PWD to tell us about his or her experiences. Some PWD were no longer able to reflect on the intervention, but they could still indicate what activities were important to them and why. Since we had a convenience sample of dyads and coaches who were willing to participate in an interview, this sample may not be the representative of the total group of PWD, caregivers, and professionals. Both dyads and coaches wanted to share their experiences to contribute to improving care for PWD. The intervention gave most dyads satisfactory benefits. For those dyads, the interventions appeared to fit their needs and preferences rather well. We interviewed some dyads who stopped early in the intervention, too. They mainly needed information, were not ready at that moment for a practical approach, and did not have activity needs, or the needs assessment had been to general. Those dyads afforded us information about preconditions for these interventions and what was not working. Furthermore, the heterogeneity in terms of age, education, relationship, work experience, duration of the dementia, and both positive and negative experiences may be representative for PWD and caregivers in general. The coaches had various background characteristics as well.
Recommendations for practice
Our findings can provide guidance for competences professionals need when they would like to provide activating intervention to PWD and their caregivers. It is important to enable PWD and caregivers to continue to do activities taking into account any declines in capacities. Professionals have to be skilled in assessing the needs of PWD and caregivers and their capacities and limitations and in training how to adapt activities and practice. Good communication skills are needed to engage both PWD and caregivers in the intervention. Starting from individual needs with a focus on possibilities requires the coaches to have an open and creative attitude in a collaborative process with the dyad.
Creativity and innovative thinking may need more attention in training and education. Professionals may consider offering these interventions to PWD and caregivers in a training session to get a grip on the situation, rather than just giving care service, aligned with what PWD and caregivers perceive as the valuable mechanisms of these interventions.
Recommendations for research
Further study is needed to find out how the professionals guiding these interventions can achieve empowerment for PWD and caregivers and how they can learn to develop these competencies.
Studies on the impact of dyadic, psychosocial, activating interventions should focus on enabling activities despite declines in capacities and reinforcing self-efficacy. Therefore, outcome measures should also include self-efficacy, with aspects such as hope and belief in one’s own capacities, along with outcome measures for mood, burden, and quality of life.
Acknowledgments
We thank all the participants with dementia, their family caregivers, the coaches, and the project managers Connie Klingeman and AEP. AEP conducted seven interviews with participants in the Exercise and Support Intervention and assisted in coding the first four cases in the analysis. The Rotterdam University of Applied Sciences financially supported the study.
Footnotes
Author contributions
NL, JL, and AMP developed the study design. NL analyzed all data in detail. NL, JL, and AMP discussed preliminary coding outcomes. NL, JL, and EP frequently discussed results during all phases for plausibility and consistency. All authors discussed the methods, summaries, analyses, and results in the study and were involved in the writing of this paper. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Livingston G, Sommerlad A, Orgeta V, et al. Dementia prevention, intervention, and care. Lancet. 2017;390(10113):2673–2734. doi: 10.1016/S0140-6736(17)31363-6. [DOI] [PubMed] [Google Scholar]
- 2.Smits CH, de Lange J, Dröes RM, Meiland F, Vernooij-Dassen M, Pot AM. Effects of combined intervention programmes for people with dementia living at home and their caregivers: a systematic review. Int J Geriatr Psychiatry. 2007;22(12):1181–1193. doi: 10.1002/gps.1805. [DOI] [PubMed] [Google Scholar]
- 3.Van’t Leven N, Prick AE, Groenewoud JG, Roelofs PD, de Lange J, Pot AM. Dyadic interventions for community-dwelling people with dementia and their family caregivers: a systematic review. Int Psychogeriatr. 2013;25(10):1581–1603. doi: 10.1017/S1041610213000860. [DOI] [PubMed] [Google Scholar]
- 4.Nygard L. Responses of persons with dementia to challenges in daily activities: a synthesis of findings from empirical studies. Am J Occup Ther. 2004;58(4):435–445. doi: 10.5014/ajot.58.4.435. [DOI] [PubMed] [Google Scholar]
- 5.van der Roest HG, Meiland FJ, Maroccini R, Comijs HC, Jonker C, Droes RM. Subjective needs of people with dementia: a review of the literature. Int Psychogeriatr. 2007;19(3):559–592. doi: 10.1017/S1041610206004716. [DOI] [PubMed] [Google Scholar]
- 6.Öhman A, Nygard L. Meanings and motives for engagement in self-chosen daily life occupations among individuals with Alzheimer’s disease. OTJR (Thorofare N J) 2005;25(3):89–97. [Google Scholar]
- 7.Stav WB, Hallenen T, Lane J, Arbesman M. Systematic review of occupational engagement and health outcomes among community-dwelling older adults. Am J Occup Ther. 2012;66(3):301–310. doi: 10.5014/ajot.2012.003707. [DOI] [PubMed] [Google Scholar]
- 8.Vikstrom S, Josephsson S, Stigsdotter-Neely A, Nygard L. Engagement in activities: experiences of persons with dementia and their caregiving spouses. Dementia. 2008;7(2):251–270. [Google Scholar]
- 9.Van Bruggen S, Gussekloo J, Bode C, Touwen DP, Engberts DP, Blom JW. Problems experienced by informal caregivers with older care recipients with and without cognitive impairment. Home Health Care Serv Q. 2016;35(1):11–24. doi: 10.1080/01621424.2016.1145166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peeters JM, Van Beek AP, Meerveld JH, Spreeuwenberg PM, Francke AL. Informal caregivers of persons with dementia, their use of and needs for specific professional support: a survey of the National Dementia Programme. BMC Nurs. 2010;9:9. doi: 10.1186/1472-6955-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vikström S, Borell L, Stigsdotter-Neely A, Josephsson S. Caregivers’ Self-Initiated Support Toward Their Partners With Dementia When Performing an Everyday Occupation Together at Home. OTJR (Thoro-fare N J) 2005;25(34):149–159. [Google Scholar]
- 12.Gitlin LN, Winter L, Burke J, Chemett N, Dennis MP, Hauck WW. Tailored activities to manage neuropsychiatric behaviors in persons with dementia and reduce caregiver burden: a randomized pilot study. Am J Geriatr Psychiatry. 2008;16(3):229–239. doi: 10.1097/JGP.0b013e318160da72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gitlin LN, Winter L, Corcoran M, Dennis MP, Schinfeld S, Hauck WW. Effects of the home environmental skill-building program on the caregiver-care recipient dyad: 6-month outcomes from the Philadelphia REACH Initiative. Gerontologist. 2003;43(4):532–546. doi: 10.1093/geront/43.4.532. [DOI] [PubMed] [Google Scholar]
- 14.Gitlin LN, Winter L, Dennis MP, Hodgson N, Hauck WW. A biobehavioral home-based intervention and the well-being of patients with dementia and their caregivers: the COPE randomized trial. JAMA. 2010;304(9):983–991. doi: 10.1001/jama.2010.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gitlin LN, Winter L, Dennis MP, Hodgson N, Hauck WW. Targeting and managing behavioral symptoms in individuals with dementia: a randomized trial of a nonpharmacological intervention. J Am Geriatr Soc. 2010;58(8):1465–1474. doi: 10.1111/j.1532-5415.2010.02971.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Graff M, van Melick M, Thijssen M, Verstraten P. Ergotherapie bij ouderen met dementie en hun mantelzorgers: Het EDOMAH-programma [Occupational Therapy for Older Persons with Dementia and Their Informal Caregivers: COTiD-Programme] Houten: Bohn Stafleu van Loghum; 2010. [Google Scholar]
- 17.Prick AE, de Lange J, Scherder E, Pot AM. Home-based exercise and support programme for people with dementia and their caregivers: study protocol of a randomised controlled trial. BMC Public Health. 2011;11:894. doi: 10.1186/1471-2458-11-894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Teri L, Gibbons LE, McCurry SM, et al. Exercise plus behavioral management in patients with Alzheimer disease: a randomized controlled trial. JAMA. 2003;290(15):2015–2022. doi: 10.1001/jama.290.15.2015. [DOI] [PubMed] [Google Scholar]
- 19.Teri L, Logsdon RG, Uomoto J, McCurry SM. Behavioral treatment of depression in dementia patients: a controlled clinical trial. J Gerontol B Psychol Sci Soc Sci. 1997;52(4):P159–P166. doi: 10.1093/geronb/52b.4.p159. [DOI] [PubMed] [Google Scholar]
- 20.Verkaik R, Francke A, Lahr M, Zuidervaart M. Huisbezoeken; Voorkom Somberheid bij Geheugenproblemen, Handboek voor de hulpverlener (Plezierige Activiteitenmethode) [Home Visits: Preventing Depressive Mood in Memory Problems, Manual for the Professional: Pleasant Activities] Utrecht: NIVEL; 2005. [Accessed July 5, 2018]. Available from: https://www.nivel.nl/en/node/891. Dutch. [Google Scholar]
- 21.Mountain GA, Craig CL. What should be in a self-management programme for people with early dementia? Aging Ment Health. 2012;16(5):576–583. doi: 10.1080/13607863.2011.651430. [DOI] [PubMed] [Google Scholar]
- 22.O’Sullivan G, Hocking C. Translating action research into practice: seeking occupational justice for people with dementia. OTJR (Thorofare N J) 2013;33(3):168–176. doi: 10.3928/15394492-20130614-05. [DOI] [PubMed] [Google Scholar]
- 23.Dopp CM, Graff MJ, Teerenstra S, Olde Rikkert MG, Nijhuisvan der Sanden MW, Vernooij-Dassen MJ. Effectiveness of a training package for implementing a community-based occupational therapy program in dementia: a cluster randomized controlled trial. Clin Rehabil. 2015;29(10):974–986. doi: 10.1177/0269215514564699. [DOI] [PubMed] [Google Scholar]
- 24.Graff MJ, Vernooij-Dassen MJ, Thijssen M, Dekker J, Hoefnagels WH, Rikkert MG. Community based occupational therapy for patients with dementia and their care givers: randomised controlled trial. BMJ. 2006;333(7580):1196. doi: 10.1136/bmj.39001.688843.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prick AE, de Lange J, Scherder E, Twisk J, Pot AM. The effects of a multicomponent dyadic intervention on the mood, behavior, and physical health of people with dementia: a randomized controlled trial. Clin Interv Aging. 2016;11:383–395. doi: 10.2147/CIA.S95789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prick AE, de Lange J, Scherder E, Twisk J, Pot AM. The effects of a multicomponent dyadic intervention with physical exercise on the cognitive functioning of people with dementia: a randomized controlled trial. J Aging Phys Act. 2017;25(4):539–552. doi: 10.1123/japa.2016-0038. [DOI] [PubMed] [Google Scholar]
- 27.Prick AE, de Lange J, Twisk J, Pot AM. The effects of a multi-component dyadic intervention on the psychological distress of family caregivers providing care to people with dementia: a randomized controlled trial. Int Psychogeriatr. 2015;27(12):2031–2044. doi: 10.1017/S104161021500071X. [DOI] [PubMed] [Google Scholar]
- 28.Voigt-Radloff S, Graff M, Leonhart R, et al. A multicentre RCT on community occupational therapy in Alzheimer’s disease: 10 sessions are not better than one consultation. BMJ Open. 2011;1(1):e000096. doi: 10.1136/bmjopen-2011-000096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Graff MJ, Vernooij-Dassen MJ, Thijssen M, Dekker J, Hoefnagels WH, Olderikkert MG. Effects of community occupational therapy on quality of life, mood, and health status in dementia patients and their caregivers: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2007;62(9):1002–1009. doi: 10.1093/gerona/62.9.1002. [DOI] [PubMed] [Google Scholar]
- 30.Brodaty H, Arasaratnam C. Meta-analysis of nonpharmacological interventions for neuropsychiatric symptoms of dementia. Am J Psychiatry. 2012;169(9):946–953. doi: 10.1176/appi.ajp.2012.11101529. [DOI] [PubMed] [Google Scholar]
- 31.Dugmore O, Orrell M, Spector A. Qualitative studies of psychosocial interventions for dementia: a systematic review. Aging Ment Health. 2015;19(11):955–967. doi: 10.1080/13607863.2015.1011079. [DOI] [PubMed] [Google Scholar]
- 32.Olazaran J, Reisberg B, Clare L, et al. Nonpharmacological therapies in Alzheimer’s disease: a systematic review of efficacy. Dement Geriatr Cogn Disord. 2010;30(2):161–178. doi: 10.1159/000316119. [DOI] [PubMed] [Google Scholar]
- 33.Pinquart M, Sorensen S. Helping caregivers of persons with dementia: which interventions work and how large are their effects? Int Psychogeriatr. 2006;18(4):577–595. doi: 10.1017/S1041610206003462. [DOI] [PubMed] [Google Scholar]
- 34.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 35.Kvale S, Brinkmann S. InterViews: Learning the Craft of Qualitative Research Interviewing. 2nd ed. Thousand Oaks, CA: Sage Publications, Inc; 2009. [Google Scholar]
- 36.Friese S. Qualitative Data Analysis with ATLASti. London: Sage Publications Ltd.; 2012. [Google Scholar]
- 37.Boeije H. Analysis in Qualitative Research. London: Sage Publications Ltd.; 2010. [Google Scholar]
- 38.Bogdan RC, Biklen SK. Qualitative Research for Education: An Introduction to Theory and Methods. Boston: Allyn & Bacon; 1997. [Google Scholar]
- 39.Haberstroh J, Neumeyer K, Krause K, Franzmann J, Pantel J. TANDEM: communication training for informal caregivers of people with dementia. Aging Ment Health. 2011;15(3):405–413. doi: 10.1080/13607863.2010.536135. [DOI] [PubMed] [Google Scholar]
- 40.Boots LM, Wolfs CA, Verhey FR, Kempen GI, de Vugt ME. Qualitative study on needs and wishes of early-stage dementia caregivers: the paradox between needing and accepting help. Int Psychogeriatr. 2015;27(6):927–936. doi: 10.1017/S1041610214002804. [DOI] [PubMed] [Google Scholar]
- 41.Wolverson Radbourne EL, Clarke C, Moniz-Cook E. Remaining hopeful in early-stage dementia: a qualitative study. Aging Ment Health. 2010;14(4):450–460. doi: 10.1080/13607860903483110. [DOI] [PubMed] [Google Scholar]
- 42.Clemson L, Donaldson A, Hill K, Day L. Implementing person- environment approaches to prevent falls: a qualitative inquiry in applying the Westmead approach to occupational therapy home visits. Aust Occup Ther J. 2014;61(5):325–334. doi: 10.1111/1440-1630.12132. [DOI] [PubMed] [Google Scholar]
- 43.Zwijsen SA, van der Ploeg E, Hertogh CM. Understanding the world of dementia. How do people with dementia experience the world? Int Psychogeriatr. 2016;28(7):1067–1077. doi: 10.1017/S1041610216000351. [DOI] [PubMed] [Google Scholar]
- 44.Kuiper C. The Eventmaker, the hybrid Art of Performing Professionals, Work-setting Rehabilitation. Den Haag: Lemma; 2007. [Google Scholar]
- 45.Graff MJL, Vernooij-Dassen MJM, Zajec J, Rikkert MGM, Hoefnagels WHL, Dekker J. How can occupational therapy improve the daily performance and communication of an older patient with dementia and his primary caregiver? A case study. Dementia. 2006;5(4):503–532. [Google Scholar]
- 46.Van’t Leven N, de Lange J, Prick AE, Pot AM. How do activating interventions fit the personal needs, characteristics and preferences of people with dementia living in the community and their informal caregivers? Dementia. 2016;0(0):1–21. doi: 10.1177/1471301216662378. [DOI] [PubMed] [Google Scholar]