Abstract
Purpose
Previous studies have indicated that transcranial direct current stimulation (tDCS) with the anode over the motor cortex and the cathode over the contralateral supraorbital region is effective in reducing clinical pain in patients with chronic pain, but these studies have not focused on experimental pain sensitivity. Therefore, the aim of this study was to examine the effect of tDCS on experimental pain sensitivity in older adults with knee osteoarthritis (OA).
Patients and methods
Forty community-dwelling participants aged 50–70 years with knee OA pain were randomly assigned to receive five daily sessions of 2 mA tDCS for 20 minutes (n = 20) or sham tDCS (n = 20) using a parallel group design. A multimodal quantitative sensory testing battery was completed, including heat pain, pressure pain threshold (PPT), punctate mechanical pain, and conditioned pain modulation (CPM).
Results
The active tDCS group showed greater increases in heat pain thresholds and tolerances, PPTs, and CPM, and reductions in punctate pain. In addition, beneficial changes in experimental pain measures were associated with reductions in clinical pain. Future studies are needed to extend these findings to better understand the underlying mechanisms of tDCS as well as to optimize treatment parameters including number and duration of stimulation sessions.
Conclusion
Our findings demonstrate that tDCS reduces experimental pain sensitivity, and these beneficial changes in experimental pain measures were associated with reductions in clinical pain.
Keywords: transcranial direct current stimulation, knee osteoarthritis, quantitative sensory testing, Bayesian analysis
Introduction
Osteoarthritis (OA), which is the most common form of the arthritis, is a leading cause of pain, functional impairments, and disability in older adults.1,2 However, patients with knee OA pain often have inadequate pain relief.3 Also, recent literature suggests that knee OA pain is characterized by altered central pain processing,4–7 which may explain the limited success of existing peripherally based treatments that target the pain locally in the area of the knee. Moreover, neuroimaging studies have revealed increased blood-oxygen-level dependent activity in response to pain stimuli in people with knee OA.8–10 Therefore, interventions targeting central nervous system pain processing have received significant attention to manage knee OA pain.
Recently, there is a growing interest in the transcranial direct current stimulation (tDCS) for the treatment of pain in chronic conditions due to its neuromodulatory effect as it can change the brain activity in a noninvasive, painless, and safe way.11–14 tDCS with the anode electrode placed over the primary motor cortex (M1) of the hemisphere contralateral to the affected knee and with the cathode electrode placed over the supraorbital region (SO) ipsilateral to the affected knee (referred to hereafter as M1-SO tDCS) involves the application of weak direct electric current to the scalp in a noninvasive and painless manner, leading to the modulation of neuronal resting membrane potentials and alteration of the endogenous excitability of the targeted brain tissue.15–17
Persons with OA are reported to display higher experimental pain sensitivity, such as lower heat pain thresholds and tolerances, lower pressure pain threshold (PPT), and higher punctate mechanical pain.6,18,19 However, previous studies, including ours, examined clinical outcomes associated with tDCS,11,13,20,21 but few studies reported changes in experimental pain sensitivity after tDCS. The examination of the effect of tDCS on experimental pain sensitivity, which can be different based on the parameters of tDCS (eg, polarity, electric current intensity, and target site), could help clinicians and researchers to better understand the underlying mechanisms of action involved with tDCS and the role played by the cortex in the integration of nociceptive information. Unfortunately, the few studies that have assessed experimental pain sensitivity have not focused on M1-SO tDCS with an electrical current of 2 mA intensity in older adults.22 Therefore, the aim of this study was to examine the effect of tDCS on experimental pain sensitivity in older adults with knee OA and how these changes in experimental pain sensitivity are related to OA-related clinical pain and function changes.
Patients and methods
Study participants
Detailed selection criteria and enrollment procedures were published and described previously.21 Briefly, 40 participants aged 50–70 years with self-reported knee OA pain based on the American College of Rheumatology criteria23 from North Central Florida were recruited into the study. Participants were excluded if they have any concurrent medical conditions that could confound interpretation of outcome measures (eg, systemic lupus erythematosus, rheumatoid arthritis, or fibromyalgia), pose a safety risk for any of the assessment or tDCS procedures (eg, history of stroke, seizure, brain tumor, brain surgery, or intracranial metal implantation), or preclude successful completion of the protocol (eg, cognitive impairment, or alcohol/substance abuse).
This double-blinded, randomized, sham-controlled pilot study was approved by the institutional review board of University of Florida prior to commencement and is registered at clinicaltrials.gov (NCT02512393). All participants were provided with detailed information about the protocol and aware that they could receive either sham or active stimulation. Written informed consent was obtained from all participants before participation.
Experimental design
The study was conducted in a double-blind and sham-controlled design to ensure that neither participants nor experimenters were aware of the stimulation condition. All participants underwent five daily sessions of stimulation for 20 minutes. Participants were randomly assigned to either the active or the sham tDCS group in a 1:1 ratio, and allocation concealment was ensured. The stimulations were administered by a Soterix Clinical Trial direct current stimulator (Soterix Medical Inc., New York, NY, USA) to deliver experimenter- and participant-blinded tDCS. The experimenters entered a six-digit blinded code into the device to deliver noninvasive brain stimulation so that they were blind to the condition. The participants were blinded with regard to the type of tDCS, and they knew that they could receive either sham or active stimulation. Only the statistician who had no involvement in data collection de-identified the data at the completion of the study.
tDCS intervention
tDCS with a constant current of 2 mA intensity was applied for 20 minutes once a day for 5 consecutive days using a pair of saline-saturated rectangular sponge electrodes sized 5 × 7 cm (35 cm2). The anode electrode was placed over C3 or C4 (10–20 systems for electroencephalography electrode placement) contralateral to the affected knee, and the cathode electrode was placed over the SO contralateral to the anode (M1-SO montage). A panel of the experts at the European Chapter of the International Federation of Clinical Neurophysiology recommended M1-SO tDCS for possible efficacy among population with chronic pain.24 M1-SO tDCS is believed to modulate pain processing pathways25,26 and provide a broad pattern of stimulation to motor, somatosensory, and frontal cortices implicated in pain sensitivity.11,27,28
For sham tDCS, the electrodes were placed in the same positions but included only ramp-up and ramp-down periods (30 seconds each) at the beginning and end to mimic somatosensory perception of active tDCS. This sham stimulation method has been shown to be reliable.11,29
OA-related clinical pain and function measures
The Numeric Rating Scale (NRS) and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)30 were used to measure OA-related pain and function. The NRS assessing current knee pain ranges from 0 (no pain) to 100 (worst pain imaginable), and the WOMAC ranges from 0 to 96, with higher scores indicating worse OA symptoms. These scales have been widely used in clinical pain studies, and psychometric properties have been demonstrated.30–32
Quantitative sensory testing procedures
A multimodal quantitative sensory testing battery was completed, including heat pain (ie, threshold and tolerance), PPT, punctate mechanical pain, and conditioned pain modulation (CPM). The order of heat and mechanical testing was randomized and counterbalanced, while CPM always occurred last to avoid carryover effects. Standardized recorded instructions were played for all participants.
Thermal testing procedures
All thermal stimuli were delivered using a computer-controlled TSA-II NeuroSensory Analyzer (Medoc Ltd., Ramat Yishai, Israel) to measure heat pain thresholds and heat pain tolerances on the index knee as well as the ipsilateral ventral forearm using an ascending method of limits. At each body site, the thermode position was moved between trials to avoid sensitization and/or habituation of cutaneous receptors. From the baseline of 32°C, the thermode temperature increased at a rate of 0.5°C per second until the participants pressed a button to stop heat stimuli. Participants were asked to press the button when the sensation “first becomes painful” to assess the heat pain threshold and when they “no longer feel able to tolerate the pain” to assess their heat pain tolerance. Three trials of heat pain threshold were presented at the first test site, followed by three trials at the second test site, followed by a 5-minute rest period. Then, three trials of heat pain tolerance were conducted at each site. The average of the three individual trials was computed to determine heat pain threshold and heat pain tolerance at each site.
Mechanical testing procedures
We assessed two types of mechanical pain responses. First, we measured PPTs by applying blunt mechanical pressure to deep tissues (ie, muscle and joint) via a handheld digital pressure algometer (Wagner, Greenwich, CT, USA). Increasing pressure was applied at a constant rate of 0.3 kgf/cm2/s to measure the PPT at four sites: the medial and lateral aspect of the index knee, ipsilateral quadriceps, and trapezius. Participants were instructed to notify the experimenter when the sensation “first becomes painful” to assess the PPT. The results of the three trials at each body site were averaged for each site.
Following the assessment of the PPT, participants underwent a procedure to assess their cutaneous mechanical sensitivity to punctate stimuli on both the index patella and the back of the ipsilateral hand. We used calibrated nylon monofilament that delivered a target force of 300 g to obtain verbal ratings of the pain intensity on a scale of 0 (no pain sensation) to 100 (the most intense pain sensation imaginable) following 10 contacts at the rate of 1 contact per second. Pain ratings for the two trials were averaged to generate the punctate pain sensitivity at each site
CPM
Ten minutes following the assessment of thermal or mechanical pain, CPM was assessed as a measure of pain inhibition. CPM was assessed by determining the change in PPT on the trapezius immediately after the immersion of the contralateral hand up to the wrist in the cold water bath at the temperature of 12°C for 1 minute. Thirty seconds after hand immersion, participants were asked to rate the cold pain intensity (0–100) from the immersed hand and were instructed to keep their hand in the water bath for as long as tolerable up to 1 minute. We selected this temperature based on our previous experience in middle-aged and older adults with knee OA.33 We found that the 12°C cold pressor produced moderate pain but was tolerable for the majority of participants. The water was maintained at a constant temperature by a refrigeration unit (Neslab, Portsmouth, NH, USA), and the water was constantly circulated to prevent local warming around the submerged hand. Pain inhibition was reflected by an increase in PPT after cold water immersion.
Statistical analyses
Descriptive statistics (ie, frequency, central tendency) were performed to evaluate sample characteristics. Demographic variables (eg, sex, race) were screened as potential confounders of the relationship between treatment condition and experimental pain measures following recommendations in the literature.34 As none of the screened variables were related to the independent variable (and thus not confounding variables), none met the criteria for inclusion as a covariate in subsequent models.
Primary analyses used general linear models to examine each experimental pain outcome as a function of treatment group while covarying for measurement at baseline to assess the effect of treatment over time (residual change). Bayesian statistical inference was used to directly quantify the probability of the alternative hypothesis that an effect of treatment exists, given the data. Bayesian parameter estimates are taken from the posterior distribution that captures the uncertainty surrounding the magnitude of an effect.35 The posterior distribution describes the probability that a given effect exists. For these primary analyses, the visual inspection of histograms indicated that the experimental pain measures were normally distributed. Model fit indices obtained from intercept-only models confirmed the appropriateness of fitting these outcomes using the Gaussian distributions. Analyses were performed using Proc GENMOD in SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
Bayesian inference has demonstrated the utility for decision-making in the context of continuing investigation into treatment effects found in pilot trials.36 Vague, neutral priors (~Normal [µ = 0, σ2 = 1 × 106]) were used to maximize the influence of the present data on posterior probabilities. The focus of the present Bayesian analysis is to provide the probability that the alternative hypothesis is true. Disparate researchers might identify different posterior probabilities that constitute a meaningful likelihood of an effect existing. Such probabilities should be based on the specific research context and investigator domain knowledge, rather than using a monolithic cutoff value as in frequentist inference. In the present study, a posterior probability ≥75% that an effect of treatment exists was considered to merit further consideration. This value was chosen for its consistency with previous probability thresholds chosen a priori in the similar context of existing medication trials.37–40 In our scientific and clinical opinion, the current research would be worth pursuing if there was a 3/4 chance that our alternative hypothesis was correct. Higher or lower probabilities might serve as better cutoffs depending on the potential risks or benefits associated with a given intervention. For instance, we might argue that a posterior probability of 66% is warranted if the intervention provides some benefit for an otherwise fatal disorder for which no effective treatment exists. Each individual presented with the present alternative hypothesis must ascertain whether a 75% chance of benefit as defined here warrants further investigation.
While a comprehensive account of Bayesian vs frequentist inference is beyond the scope of the present article, additional details regarding the difference between the Bayesian posterior probability and the frequentist P-value merit further discussion. A null hypothesis test at the frequentist P ≤ 0.05 level evaluates the probability of observing the current data, or data more extreme, given that the null hypothesis is true. The Bayesian posterior probability is the probability that the alternative hypothesis is true, given the data. These describe qualitatively different issues: the first attempts to reject the null hypothesis, while the latter estimates the probability of the alternative hypothesis. This is important because it reveals that the P-value is not the complement of the posterior probability; that is, posterior probability is not equivalent to 1 – P-value (75% posterior probability ≠ 0.25 P-value).41
The present analytic scheme purposely deviates from the predominant null hypothesis significance testing (NHST) approach to research. As currently practiced, the NHST approach is problematic: estimates are often overstated, in the wrong direction, and complicated by exaggeration from so-called p-hacking.42 The present research adopts an alternative, incrementalist perspective. The results from all models are presented along with an explicitly stated, yet subjective, threshold of notable probability that the alternative hypothesis exists. The goal is to provide all the results with minimal bias to incrementally increase knowledge, while also allowing researchers to consider their own subjective threshold of notable probability that the alternative hypothesis exists (as well as the extent to which their subjective threshold agrees with that presently stated).
Additional exploratory analyses utilized Bayesian generalized linear mixed models (GLMMs) to model each of two clinical pain measures (NRS and WOMAC) as a function of each experimental pain measure, controlling for time. GLMM is a statistical technique that allows the investigation of non-normal outcomes and the explicit modeling of random effects to account for correlation between repeated observations.35 Clinical and experimental pain data were recast into longitudinal format, and all analyses included a random intercept for participant. For these secondary analyses, visual inspection of histograms suggested that the clinical pain measures were non-Gaussian. Posterior predictive checking indicated that the lognormal distribution (with identity link) was appropriate for both clinical pain measures (NRS and WOMAC). A small constant c = 1.0 was added to each NRS value to countenance zero values. Similar to the primary analyses, a posterior probability ≥75% of an effect of experimental pain existing in predicting clinical pain was considered sufficient evidence that a relationship exists. Bayesian GLMMs were fit using the brms package in the R statistical computing environment.43
Results
Sample characteristics
Forty participants were randomly assigned to receive either treatment (n = 20) or sham (n = 20). Participant characteristics were not significantly different between groups (Table 1). Mean and SD of all pain outcomes are included in Table 2.
Table 1.
Baseline demographic characteristics of the participants
| Sham (n = 20) | Treatment (n = 20) | Group differences, χ2 (P-value) | |
|---|---|---|---|
| Sex, N | 0.10 (0.75) | ||
| Male | 9 | 10 | |
| Female | 11 | 10 | |
| Race, N | 0.00 (1.00) | ||
| Asian | 10 | 10 | |
| White | 10 | 10 | |
| Education, N | 1.73 (0.79) | ||
| <High school | 0 | 0 | |
| High school | 3 | 3 | |
| 2 years college | 5 | 2 | |
| College | 5 | 7 | |
| Master’s | 3 | 3 | |
| Doctoral | 4 | 5 | |
| Employment, N | 3.13 (0.68) | ||
| Working | 11 | 10 | |
| Laid off | 0 | 1 | |
| Unemployed | 0 | 0 | |
| Retired | 5 | 0 | |
| Disabled | 0 | 0 | |
| Student | 0 | 1 | |
| Keeping house | 1 | 1 | |
| Marital status, N | 1.33 (0.86) | ||
| Married | 15 | 15 | |
| Widowed | 1 | 1 | |
| Divorced | 1 | 0 | |
| Separated | 0 | 2 | |
| Never married | 2 | 0 | |
| Living with partner | 1 | 2 | |
| M (SD) | M (SD) | F(1) (P-value) | |
| Age (years) | 59.3 (8.6) | 60.6 (9.8) | 0.18 (0.67) |
| BMI (kg/m2) | 26.0 (4.1) | 27.0 (3.3) | 0.85 (0.36) |
Abbreviations: BMI, body mass index; M, mean; N, number.
Table 2.
Mean and SD for primary outcomes
| Measures | Sham group (n = 20) | Active group (n = 20) | ||
|---|---|---|---|---|
| Baseline | Post-tDCS | Baseline | Post-tDCS | |
| HPTh, arm, °C | 39.97 (5.01) | 40.57 (4.04) | 40.89 (4.53) | 42.39 (3.64) |
| HPTh, knee, °C | 40.51 (4.69) | 40.18 (4.34) | 41.84 (4.38) | 42.62 (3.20) |
| HPTo, arm, °C | 45.24 (3.18) | 45.54 (3.22) | 45.46 (3.64) | 46.38 (3.24) |
| HPTo, knee, °C | 45.04 (3.59) | 45.42 (3.50) | 46.47 (3.01) | 47.07 (2.26) |
| Punctate pain, hand | 34.53 (26.20) | 43.80 (32.43) | 29.80 (26.18) | 31.58 (24.15) |
| Punctate pain, patella | 46.60 (25.99) | 50.73 (33.61) | 45.85 (31.94) | 42.23 (26.87) |
| PPT, lateral knee, kgf | 2.87 (1.29) | 3.22 (1.17) | 2.83 (1.33) | 3.36 (1.19) |
| PPT, medial knee, kgf | 2.63 (1.30) | 2.98 (1.10) | 2.61 (1.13) | 3.21 (1.08) |
| PPT, quadriceps, kgf | 2.95 (1.21) | 3.16 (1.15) | 3.25 (1.30) | 3.69 (1.28) |
| PPT, trapezius, kgf | 2.32 (1.01) | 2.81 (0.91) | 3.21 (1.50) | 3.43 (1.38) |
| CPM | 0.73 (0.48) | 0.70 (0.71) | 0.84 (0.69) | 0.94 (0.52) |
| Cold pain | 62.75 (27.36) | 62.05 (30.46) | 69.25 (24.56) | 65.40 (24.37) |
Notes: The scores of punctate pain ranged from 0 to 100, with higher scores indicating more intense pain. We assessed CPM by determining the change in PPT on the trapezius following immersion of the contralateral hand up to the wrist in the cold water bath at the temperature of 12°C for 1 minute, with higher CPM scores indicating better pain inhibition.
Abbreviations: CPM, conditioned pain modulation; HPTh, heat pain threshold, HPTo, heat pain tolerance, PPT, pressure pain tolerance; tDCS, transcranial direct current stimulation.
Bayesian general linear modeling – experimental pain as a function of treatment
Interpretation of results using Bayesian inference requires an understanding of how to interpret the posterior distribution. Figure 1 provides graphical depictions of the posterior distributions for the effect of treatment on one of the outcome measures in the present study: heat pain threshold (arm). The figure demonstrates several key concepts for interpreting the posterior distribution. First, the probability that an effect exists is depicted using an arrow pointing in the direction of benefit. The posterior distribution is a probability distribution integrating to one, and the area under the curve above 0 is an estimate of the probability that the effect exceeds 0: for heat pain threshold (arm), 94% of the posterior distribution is greater than 0, indicating a 0.94 probability that a positive effect exists (and a corresponding 0.06 probability that a negative effect exists). The 95% credible interval (CrI) is captured with a bracket along the x-axis, and a line is drawn at the median of the posterior distribution. The median of the posterior provides a point estimate of the effect of treatment that may be interpreted in the same fashion as a regression coefficient: in Figure 1, a median effect of 1.29 indicates that active tDCS treatment produces a heat pain threshold that is 1.29°C higher than sham tDCS treatment. Table 3 provides a summary of the Bayesian results for each of the dependent measures, including the median and CrI of the posterior distribution as well as the posterior probability that an effect of treatment exists.
Figure 1.
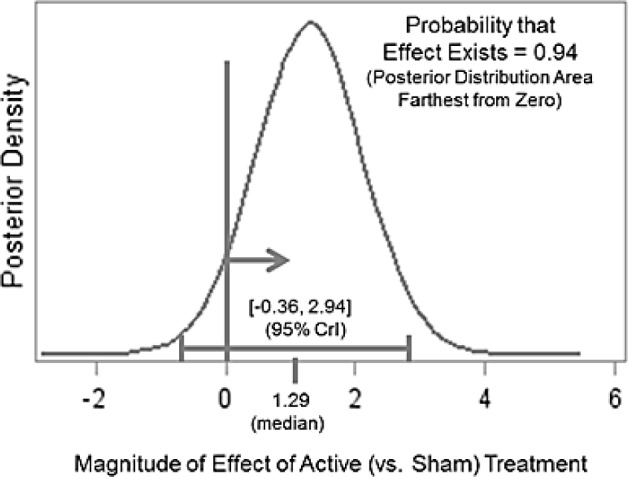
Interpretation of posterior distribution of the effect of tDCS group on heat pain threshold.
Abbreviations: CrI, credible interval; tDCS, transcranial direct current stimulation.
Table 3.
Bayesian general linear modeling results
| Measures | Posterior distribution, median [95% CrI] | Posterior probability |
|---|---|---|
| HPTh, arm, °C | 1.29 [−0.36, 2.94] | 0.94 |
| HPTh, knee, °C | 1.49 [0.23, 2.75] | 0.99 |
| HPTo, arm, °C | 0.66 [−0.32, 1.63] | 0.91 |
| HPTo, knee, °C | 0.51 [−0.31, 1.34] | 0.89 |
| Punctuate pain, hand | −8.66 [−21.43, 4.19] | 0.91 |
| Punctuate pain, patella | −8.01 [−22.47, 6.50] | 0.87 |
| PPT, lateral knee, kgf | 0.16 [−0.35, 0.67] | 0.74 |
| PPT, medial knee, kgf | 0.24 [−0.34, 0.81] | 0.79 |
| PPT, quadriceps, kgf | 0.32 [−0.20, 0.84] | 0.89 |
| PPT, trapezius, kgf | 0.03 [−0.48, 0.55] | 0.55 |
| CPM | 0.22 [−0.15, 0.59] | 0.88 |
| Cold pain | −2.31 [−12.00, 7.38] | 0.69 |
Notes: The scores of punctate pain ranged from 0 to 100, with higher scores indicating more intense pain. We assessed CPM by determining the change in PPT on the trapezius following immersion of the contralateral hand up to the wrist in the cold water bath at the temperature of 12°C for 1 minute, with higher CPM scores indicating better pain inhibition.
Abbreviations: CPM, conditioned pain modulation; CrI, credible interval; HPTh, heat pain threshold; HPTo, heat pain tolerance; PPT, pressure pain tolerance.
The point estimates and CrIs described in Table 3 provide a unique opportunity to address the possibility that the effect of active tDCS was greater in the region of chronic pain (the knee) relative to other regions. The point estimates and CrIs describe the effect of active tDCS on each given test. For example, active tDCS increased heat pain threshold by 1.29°C (95% CrI = [−0.36, 2.94]) in the arm and 1.49°C (95% CrI = [0.23, 2.75]) in the knee. The extent to which these CrIs overlap provides a qualitative assessment of the degree to which the effect of active tDCS is similar or dissimilar across regions. Such comparisons must take place on the same metric; that is, we can make these qualitative assessments for regions within each of four tests: heat pain threshold, heat pain tolerance, punctuate pain, and pressure pain tolerance. Examination of Table 3 suggests that the effect of active tDCS is not different in the region of chronic pain relative to comparable regions within each test.
Nine experimental pain measures demonstrated posterior probabilities greater than 0.75, favoring the active condition: heat threshold for the arm (0.94) and knee (0.99), heat tolerance for the arm (0.91) and knee (0.89), punctate pain on the hand (0.91) and patella (0.87), PPT for the medial knee (0.79) and quadriceps (0.89), and CPM (0.88). Controlling for baseline measures, heat pain threshold, heat pain tolerance, PPT, and CPM increased and punctate pain ratings decreased in those receiving treatment relative to sham. Three outcome measures did not exceed the 0.75 posterior probability threshold: PPT for the lateral knee (0.74) and trapezius (0.55) as well as cold pain (0.69).
Bayesian generalized linear mixed modeling – clinical pain as a function of experimental pain
Bayesian GLMM was used to examine the relationship between clinical and experimental pain measures. Detailed results of changes in clinical pain and function measures were published and described previously.21 We found a significant difference in only the NRS scores between groups (F [1,146] = 4.60, P = 0.03), after adjusting for the baseline scores and other covariates.
Evidence emerged to support a relationship (posterior probability ≥75%) between at least one of the two clinical measures and all the experimental pain measures except the PPT quadriceps measure and cold pain. These findings suggest that beneficial changes in experimental pain measures were associated with reductions in clinical pain. Table 4 summarizes posterior distribution point estimates and posterior probabilities for each of the 22 models exploring these relationships. We have also added a table of Spearman’s Rho correlation coefficients between difference scores of the measures in the active tDCS group in a supplementary document (Table S1).
Table 4.
Bayesian generalized linear mixed model results for clinical pain predicted by experimental pain
| NRS | Posterior distribution, median [95% CrI] | Posterior probability |
|---|---|---|
| HPTh, arm, °C | −0.06 [−0.11,−0.01] | 0.99 |
| HPTh, knee, °C | −0.06 [−0.12,−0.01] | 0.99 |
| HPTo, arm, °C | −0.07 [−0.14, 0.00] | 0.99 |
| HPTo, knee, °C | −0.06 [−0.13, 0.02] | 0.97 |
| Punctuate pain, hand | 0.01 [0.00, 0.02] | 0.94 |
| Punctuate pain, patella | 0.01 [0.01, 0.02] | 0.99 |
| PPT, lateral knee, kgf | −0.13 [−0.31, 0.06] | 1.00 |
| PPT, medial knee, kgf | −0.06 [−0.26, 0.15] | 0.91 |
| PPT, quadriceps, kgf | −0.03 [−0.21, 0.16] | 0.71 |
| PPT, trapezius, kgf | 0.02 [−0.16, 0.21] | 0.62 |
| CPM | −0.44 [−0.78,−0.10] | 0.60 |
| Cold pain | 0.00 [−0.01,0.01] | 0.66 |
| WOMAC | Posterior distribution, median [95% CrI] | Posterior probability |
| HPTh, arm, °C | 0.02 [−0.02, 0.05] | 0.60 |
| HPTh, knee, °C | 0.01 [−0.03, 0.05] | 0.83 |
| HPTo, arm, °C | 0.03 [−0.03, 0.08] | 0.69 |
| HPTo, knee, °C | 0.02 [−0.03, 0.08] | 0.84 |
| Punctuate pain, hand | 0.00 [−0.00, 0.01] | 0.81 |
| Punctuate pain, patella | 0.00 [−0.00, 0.01] | 0.82 |
| PPT, lateral knee, kgf | −0.02 [−0.14, 0.11] | 0.88 |
| PPT, medial knee, kgf | −0.01 [−0.12, 0.11] | 0.60 |
| PPT, quadriceps, kgf | 0.08 [−0.04, 0.20] | 0.55 |
| PPT, trapezius, kgf | 0.07 [−0.06, 0.19] | 0.90 |
| CPM | −0.02 [−0.21, 0.17] | 0.86 |
| Cold pain | −0.00 [−0.01, 0.01] | 0.62 |
Notes: The scores of punctate pain ranged from 0 to 100, with higher scores indicating more intense pain. We assessed CPM by determining the change in PPT on the trapezius following immersion of the contralateral hand up to the wrist in the cold water bath at the temperature of 12°C for 1 minute, with higher CPM scores indicating better pain inhibition.
Abbreviations: CrI, credible interval; CPM, conditioned pain modulation; HPTh, heat pain threshold; HPTo, heat pain tolerance; NRS, Numeric Rating Scale; PPT, pressure pain tolerance; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
Discussion
In this study, we demonstrated that tDCS with the anode over M1 and the cathode over the contralateral SO reduces experimental pain sensitivity and increases pain inhibition in older adults with knee OA. We observed greater increases in heat pain thresholds and tolerances, PPTs, and CPM, and reductions in punctate pain in the active tDCS group compared to that in the sham tDCS group. Most of the experimental pain measures demonstrated posterior probabilities greater than 0.75 in the Bayesian general linear modeling, suggesting that M1-SO tDCS merits further consideration as a promising therapeutic for OA pain. The posterior distribution obtained via Bayesian inference characterizes the entire distribution of the parameters of concern, conditional on the given data and statistical model. Thus, the interpretation of the Bayesian inference results does not have to center at the qualification of extremeness under the null hypothesis in the same manner as a P-value. In this study, we chose the probability of the alternative hypothesis as a measure of the effect’s existence. Since a cutoff of zero effect instead of the mean or median effect is used to calculate such a value (Figure 1), it will be greater than 50% and may unsurprisingly look strong.
The findings of our study are similar to those of previous studies in which tDCS was efficacious in reducing experimental pain intensity. For example, Chang et al44 reported that M1-SO tDCS plus exercise in older adults with knee OA yielded significantly greater improvement in PPTs than sham stimulation plus exercise. In addition, Moloney and Witney45 showed that cathodal tDCS of M1 before repetitive transcranial magnetic stimulation in healthy male participants increased PPTs. Moreover, Bachmann et al46 demonstrated that cathodal tDCS of M1 in healthy adults increased cold detection thresholds, mechanical detection thresholds, and mechanical pain thresholds. Some studies found that tDCS did not improve experimental pain sensitivity measures.47
While Moloney and Witney45 and Bachman et al46 delivered 1 mA tDCS with the cathode over M1 and the anode over the contralateral SO, we delivered 2 mA tDCS with the anode over M1 and the cathode over SO. Prior research demonstrated that 1 mA tDCS results in increased excitability under the anode and decreased excitability under the cathode electrode.1 In contrast, other prior research demonstrated that 2 mA tDCS results in a net increase in excitability under both the anode and cathode electrodes.2 Thus, the mechanisms underlying the efficacy of tDCS for altering pain thresholds and inhibition between these studies may differ. However, a common element across these studies may lie in the increased excitability of brain tissue underlying the SO electrode. In contrast to many theories arguing that the effects of tDCS on pain result from the stimulation of the motor and somatosensory cortices, these data appear to support an important role for increasing excitability in the frontal and other intervening cortices stimulated under and around the SO electrode.48 As both anode and cathode electrodes are active contributors to current flow in the brain, the impact of the entire montage must be carefully considered. As such, it is important to note that the efficacy of tDCS depends on a number of factors, including the target brain area, the duration and number of stimulation sessions, the electrical current intensity, the polarity of the electrode, and the target population.17 Collectively, the findings from these studies indicate the effect of tDCS on experimental pain measures, and our study extends these findings to older adults with knee OA.
While the exact mechanisms underlying the analgesic effects of M1-SO tDCS are not fully understood, our findings support the idea that M1-SO stimulation produces analgesic effects by modulating pain processing pathways.25,26 Moreover, our results extend the previous literature by providing preliminary evidence suggesting that analgesic effects of tDCS are systemic rather than localized, since the magnitude of effect was similar for the knee and non-knee test sites. Prior research has suggested that tDCS interacts with a variety of neurotransmitters implicated in pain processing, such as γ-aminobutyric acid, dopamine, serotonin, and acetylcholine.49–53 Previous studies have also demonstrated that tDCS can alter functional connectivity within brain networks, such as those that are important for cognitive, motor, and pain processing.54 Peyron et al55 reported that noxious heat stimuli activate multiple brain areas associated with pain modulation, including the thalamus, contralateral anterior cingulate cortex, and M1, and tDCS of M1 may alter intracortical motor circuitry and influence thalamic activity.45,56 Taken together, these data suggest that the effects of tDCS are not limited to the area immediately under the electrodes, providing evidence of activity alterations in distant interconnected cortical and subcortical areas.57,58
In addition, Garcia-Larrea and Peyron59 reported that motor cortex stimulation might facilitate descending pain inhibitory mechanisms. DosSantos et al60 found evidence suggesting that the effects of tDCS on pain may be related to µ-opioid receptor non-displaceable binding potential in subcortical regions implicated in pain processing. Yet, others have suggested that the effects of tDCS on pain are related to the reversal of maladaptive plasticity in pain syndromes.61,62 In contrast to theories predominantly focused on the effects of stimulation under the anode electrode placed over the motor and somatosensory cortices, other work suggests that the effects in the frontal cortices under the cathode electrode placed over SO may play an active role in altering the emotional experience of pain and contribute to analgesic effects of tDCS.48 Therefore, the effects of tDCS on pain-related neurotransmitters and functional brain systems support the use of tDCS as a promising tool for neuromodulation of pain. Furthermore, the higher CPM in the active tDCS group in this study suggests that M1-SO tDCS may boost pain inhibitory function in people with knee OA.
Our study also makes an important contribution to the feasibility of treating chronic pain using tDCS in older adults. Prior research demonstrated that the intensity and spread of tDCS current is affected by cerebrospinal fluid (CSF) space, atrophy, skull thickness, and other neuroanatomical features that change across the lifespan.3–5 These data suggest that while younger brains (eg, 11 years of age) receive higher intensity stimulation to the cortical and subcortical regions than adults, older adults (eg, 50+ years) receive less current. In addition, the pathway of current flow can be altered by different neuroanatomical features (eg, CSF pockets affiliated with significant atrophy in later life).5 Thus, prior to this study, it remained possible that tDCS in older adults would not achieve effective alteration in pain thresholds and pain inhibition. However, our data demonstrate that tDCS is both feasible and effective for impacting pain thresholds and pain inhibition in older adults.
The present study also provides an introduction to Bayesian inference to a diverse readership. The strength of this approach is in its interpretation: the posterior probability that the alternative hypothesis exists is often the true value/ quantity that researchers are trying to address when they use P-values from frequentist inference. Researchers in this field in particular may benefit from the dissemination of Bayesian methods because such methods may be better equipped to investigate questions with small sample sizes, as in the present study.63,64 Further, the Bayesian paradigm promotes incremental knowledge gain by updating prior distributions with new data – for example, the results of the present study may provide informative priors for future research.
Our findings should be interpreted in light of the study’s limitations. We included a small sample of middle-aged to young older adults with knee OA, which limits the generalizability of the study findings. The findings in this small sample of relatively young older adults may not translate to older adults with multiple chronic conditions. Future studies would benefit from extending this work to include larger samples of older adults. Moreover, the magnitude of the observed effects was relatively small, perhaps owing to the brief duration of our tDCS intervention. Additional research with greater doses of tDCS is needed to evaluate this possibility.
Conclusion
The results of this study suggest that M1-SO tDCS with a constant direct current of 2 mA intensity for 20 minutes once a day for 5 consecutive days can reduce experimental pain sensitivity and facilitate pain inhibition. Our study also contributes important knowledge regarding feasibility and efficacy of tDCS in older adults with chronic pain and adds to a growing body of literature supporting the importance of stimulation delivered through the SO electrode. These data collectively serve as a strong foundation for future clinical trials assessing population-based efficacy of tDCS as a treatment for chronic knee OA pain in older adults. Future studies with larger samples and sophisticated neuroimaging techniques are needed to extend these findings and better understand the underlying mechanisms of tDCS. Additional stimulation sessions or stimulation durations are needed to refine this novel approach for pain treatment and determine the optimal dose of tDCS.
Supplementary material
Table S1.
Correlation between difference scores of clinical and experimental pain measures
| NRS | WOMAC | HPTh, arm | HPTh, knee | HPTo, arm | HPTo, knee | Punctate pain, hand | Punctate pain, patella | PPT, lateral. knee | PPT, medial knee | PPT, quadriceps | PPT, trapezius | CPM | Cold pain | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NRS | 1 | |||||||||||||
| WOMAC | 0.301 | 1 | ||||||||||||
| HPTh, arm | −0.343 | 0.258 | 1 | |||||||||||
| HPTh, knee | −0.438 | 0.063 | 0.301 | 1 | ||||||||||
| HPTo, arm | −0.419 | 0.15 | 0.585** | 0.35 | 1 | |||||||||
| HPTo, knee | −0.522* | 0.042 | 0.233 | 0.522* | 0.511* | 1 | ||||||||
| Punctuate pain, hand | 0.479* | 0.138 | −0.129 | −0.263 | −0.566** | −0.328 | 1 | |||||||
| Punctuate pain, patella | 0.188 | −0.305 | −0.366 | −0.184 | −0.635** | −0.450* | 0.726*** | 1 | ||||||
| PPT, lateral knee | −0.187 | 0.035 | 0.356 | −0.141 | 0.048 | −0.199 | −0.217 | −0.167 | 1 | |||||
| PPT, medial knee | −0.026 | −0.111 | 0.008 | −0.011 | −0.036 | −0.237 | −0.056 | 0.057 | 0.577** | 1 | ||||
| PPT, quadriceps | 0.044 | 0.050 | 0.229 | −0.188 | 0.202 | −0.075 | −0.173 | −0.295 | 0.654** | 0.702*** | 1 | |||
| PPT, trapezius | −0.052 | 0.130 | 0.362 | −0.087 | 0.200 | −0.028 | 0.075 | −0.146 | 0.630** | 0.717*** | 0.785*** | 1 | ||
| CPM | −0.192 | −0.102 | −0.186 | 0.162 | −0.035 | 0.380 | 0.053 | −0.007 | −0.364 | −0.086 | −0.059 | −0.137 | 1 | |
| Cold pain | 0.130 | −0.363 | −0.599** | −0.321 | −0.136 | −0.203 | 0.038 | 0.349 | −0.441 | −0.180 | −0.249 | −0.423 | 0.049 | 1 |
Notes:
P < 0.05,
P < 0.01,
P < 0.001.
Acknowledgments
This research was supported in part by the Claude D. Pepper Older Americans Independence Center (P30 AG028740), the University of Florida Center for Cognitive Aging and Memory, and NIA Grants K07AG04637, K01AG050707, and R01AG05477. The funding agencies had no role in the study design, methods, data collection and analysis, or preparation of the manuscript.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Hunter DJ, Mcdougall JJ, Keefe FJ. The symptoms of osteoarthritis and the genesis of pain. Rheum Dis Clin North Am. 2008;34(3):623–643. doi: 10.1016/j.rdc.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58(1):26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Institute of Medicine . Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 4.Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. 2009;10(9):895–926. doi: 10.1016/j.jpain.2009.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finan PH, Buenaver LF, Bounds SC, et al. Discordance between pain and radiographic severity in knee osteoarthritis: findings from quantitative sensory testing of central sensitization. Arthritis Rheum. 2013;65(2):363–372. doi: 10.1002/art.34646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rakel B, Vance C, Zimmerman MB, Petsas-Blodgett N, Amendola A, Sluka KA. Mechanical hyperalgesia and reduced quality of life occur in people with mild knee osteoarthritis pain. Clin J Pain. 2015;31(4):315–322. doi: 10.1097/AJP.0000000000000116. [DOI] [PubMed] [Google Scholar]
- 7.Neogi T, Guermazi A, Roemer F, et al. Association of Joint Inflammation With Pain Sensitization in Knee Osteoarthritis: The Multicenter Osteoarthritis Study. Arthritis Rheumatol. 2016;68(3):654–661. doi: 10.1002/art.39488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gwilym SE, Keltner JR, Warnaby CE, et al. Psychophysical and functional imaging evidence supporting the presence of central sensitization in a cohort of osteoarthritis patients. Arthritis Rheum. 2009;61(9):1226–1234. doi: 10.1002/art.24837. [DOI] [PubMed] [Google Scholar]
- 9.Hiramatsu T, Nakanishi K, Yoshimura S, et al. The dorsolateral prefrontal network is involved in pain perception in knee osteoarthritis patients. Neurosci Lett. 2014;581:109–114. doi: 10.1016/j.neulet.2014.08.027. [DOI] [PubMed] [Google Scholar]
- 10.Sofat N, Smee C, Hermansson M, et al. Functional MRI demonstrates pain perception in hand osteoarthritis has features of central pain processing. J Biomed Graph Comput. 2013;3(4) doi: 10.5430/jbgc.v3n4p20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fregni F, Gimenes R, Valle AC, et al. A randomized, sham-controlled, proof of principle study of transcranial direct current stimulation for the treatment of pain in fibromyalgia. Arthritis Rheum. 2006;54(12):3988–3998. doi: 10.1002/art.22195. [DOI] [PubMed] [Google Scholar]
- 12.Simis M, Reidler JS, Duarte Macea D, et al. Investigation of central nervous system dysfunction in chronic pelvic pain using magnetic resonance spectroscopy and noninvasive brain stimulation. Pain Pract. 2015;15(5):423–432. doi: 10.1111/papr.12202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mori F, Codecà C, Kusayanagi H, et al. Effects of anodal transcranial direct current stimulation on chronic neuropathic pain in patients with multiple sclerosis. J Pain. 2010;11(5):436–442. doi: 10.1016/j.jpain.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 14.Antal A, Terney D, Kühnl S, Paulus W. Anodal transcranial direct current stimulation of the motor cortex ameliorates chronic pain and reduces short intracortical inhibition. J Pain Symptom Manage. 2010;39(5):890–903. doi: 10.1016/j.jpainsymman.2009.09.023. [DOI] [PubMed] [Google Scholar]
- 15.Nitsche MA, Cohen LG, Wassermann EM, et al. Transcranial direct current stimulation: State of the art 2008. Brain Stimul. 2008;1(3):206–223. doi: 10.1016/j.brs.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 16.Bikson M, Grossman P, Thomas C, et al. Safety of Transcranial Direct Current Stimulation: Evidence Based Update 2016. Brain Stimul. 2016;9(5):641–661. doi: 10.1016/j.brs.2016.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Woods AJ, Antal A, Bikson M, et al. A technical guide to tDCS, and related non-invasive brain stimulation tools. Clin Neurophysiol. 2016;127(2):1031–1048. doi: 10.1016/j.clinph.2015.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suokas AK, Walsh DA, Mcwilliams DF, et al. Quantitative sensory testing in painful osteoarthritis: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2012;20(10):1075–1085. doi: 10.1016/j.joca.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 19.Arendt-Nielsen L, Skou ST, Nielsen TA, Petersen KK. Altered Central Sensitization and Pain Modulation in the CNS in Chronic Joint Pain. Curr Osteoporos Rep. 2015;13(4):225–234. doi: 10.1007/s11914-015-0276-x. [DOI] [PubMed] [Google Scholar]
- 20.Fregni F, Boggio PS, Lima MC, et al. A sham-controlled, phase II trial of transcranial direct current stimulation for the treatment of central pain in traumatic spinal cord injury. Pain. 2006;122(1–2):197–209. doi: 10.1016/j.pain.2006.02.023. [DOI] [PubMed] [Google Scholar]
- 21.Ahn H, Woods AJ, Kunik ME, et al. Efficacy of transcranial direct current stimulation over primary motor cortex (anode) and contralateral supraorbital area (cathode) on clinical pain severity and mobility performance in persons with knee osteoarthritis: An experimenter- and participant-blinded, randomized, sham-controlled pilot clinical study. Brain Stimul. 2017;10(5):902–909. doi: 10.1016/j.brs.2017.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mylius V, Borckardt JJ, Lefaucheur JP. Noninvasive cortical modulation of experimental pain. Pain. 2012;153(7):1350–1363. doi: 10.1016/j.pain.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 23.Altman R, Alarcón G, Appelrouth D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34(5):505–514. doi: 10.1002/art.1780340502. [DOI] [PubMed] [Google Scholar]
- 24.Lefaucheur JP, Antal A, Ayache SS, et al. Evidence-based guidelines on the therapeutic use of transcranial direct current stimulation (tDCS) Clin Neurophysiol. 2017;128(1):56–92. doi: 10.1016/j.clinph.2016.10.087. [DOI] [PubMed] [Google Scholar]
- 25.Fregni F, Pascual-Leone A. Technology insight: noninvasive brain stimulation in neurology-perspectives on the therapeutic potential of rTMS and tDCS. Nat Clin Pract Neurol. 2007;3(7):383–393. doi: 10.1038/ncpneuro0530. [DOI] [PubMed] [Google Scholar]
- 26.Valle A, Roizenblatt S, Botte S, et al. Efficacy of anodal transcranial direct current stimulation (tDCS) for the treatment of fibromyalgia: results of a randomized, sham-controlled longitudinal clinical trial. J Pain Manag. 2009;2(3):353–361. [PMC free article] [PubMed] [Google Scholar]
- 27.Luedtke K, Rushton A, Wright C, Geiss B, Juergens TP, May A. Transcranial direct current stimulation for the reduction of clinical and experimentally induced pain: a systematic review and meta-analysis. Clin J Pain. 2012;28(5):452–461. doi: 10.1097/AJP.0b013e31823853e3. [DOI] [PubMed] [Google Scholar]
- 28.O’Connell NE, Wand BM, Marston L, Spencer S, Desouza LH. Noninvasive brain stimulation techniques for chronic pain. Cochrane Database Syst Rev. 2014;4:CD008208. doi: 10.1002/14651858.CD008208.pub3. [DOI] [PubMed] [Google Scholar]
- 29.Gandiga PC, Hummel FC, Cohen LG. Stimulation TDC. Transcranial DC stimulation (tDCS): A tool for double-blind sham-controlled clinical studies in brain stimulation. Clin Neurophysiol. 2006;117(4):845–850. doi: 10.1016/j.clinph.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 30.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–1840. [PubMed] [Google Scholar]
- 31.Seror R, Tubach F, Baron G, et al. Individualising the Western Ontario and McMaster Universities osteoarthritis index (WOMAC) function subscale: incorporating patient priorities for improvement to measure functional impairment in hip or knee osteoarthritis. Ann Rheum Dis. 2008;67(4):494–499. doi: 10.1136/ard.2007.074591. [DOI] [PubMed] [Google Scholar]
- 32.Yang KG, Raijmakers NJ, Verbout AJ, Dhert WJ, Saris DB. Validation of the short-form WOMAC function scale for the evaluation of osteoarthritis of the knee. J Bone Joint Surg Br. 2007;89(1):50–56. doi: 10.1302/0301-620X.89B1.17790. [DOI] [PubMed] [Google Scholar]
- 33.King CD, Sibille KT, Goodin BR, et al. Experimental pain sensitivity differs as a function of clinical pain severity in symptomatic knee osteoarthritis. Osteoarthritis Cartilage. 2013;21(9):1243–1252. doi: 10.1016/j.joca.2013.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pocock SJ, Assmann SE, Enos LE, Kasten LE. Subgroup analysis, covariate adjustment and baseline comparisons in clinical trial reporting: current practice and problems. Stat Med. 2002;21(19):2917–2930. doi: 10.1002/sim.1296. [DOI] [PubMed] [Google Scholar]
- 35.Gelman A, Hill J. Data Analysis Using Regression and Multilevel/ hierarchical Models. New York: Cambridge University Press; 2007. [Google Scholar]
- 36.Schmitz JM, Green CE, Hasan KM, et al. PPAR-gamma agonist pioglitazone modifies craving intensity and brain white matter integrity in patients with primary cocaine use disorder: a double-blind randomized controlled pilot trial. Addiction. 2017;112(10):1861–1868. doi: 10.1111/add.13868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. NCT02271919 [homepage on the Internet] Varenicline and Combined Nicotine Replacement Therapy (NRT) for Smoking Cessation. [Accessed September 14, 2017]. Available from: https://clinicaltrials.gov/ct2/show/NCT02271919.
- 38. NCT02556606 [homepage on the Internet] Ketamine for Treatment Resistant Late-Life Depression. [Accessed September 14, 2017]. Available from: https://clinicaltrials.gov/ct2/show/NCT02556606.
- 39. NCT01535573 [homepage on the Internet] Citalopram for Cocaine Dependence. [Accessed September 14, 2017]. Available from: https://clinicaltrials.gov/ct2/show/NCT01535573.
- 40. NCT02162849 [homepage on the Internet] Reward Sensitivity and Pharmacotherapy for Smoking Cessation. [Accessed September 14, 2017]. Available from: https://clini-caltrials.gov/ct2/show/NCT02162849.
- 41.Johnson VE. Revised standards for statistical evidence. Proc Natl Acad Sci USA. 2013;110(48):19313–19317. doi: 10.1073/pnas.1313476110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gelman A. The Failure of Null Hypothesis Significance Testing When Studying Incremental Changes, and What to Do About It. Pers Soc Psychol Bull. 2018;44(1):16–23. doi: 10.1177/0146167217729162. [DOI] [PubMed] [Google Scholar]
- 43.Bürkner P-C. An R Package for Bayesian Multilevel Models Using Stan. J Stat Softw. 2017;80(1):1–28. [Google Scholar]
- 44.Chang WJ, Bennell KL, Hodges PW, et al. Addition of transcranial direct current stimulation to quadriceps strengthening exercise in knee osteoarthritis: A pilot randomised controlled trial. PLoS One. 2017;12(6):e0180328. doi: 10.1371/journal.pone.0180328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moloney TM, Witney AG. Pressure pain thresholds increase after preconditioning 1 Hz repetitive transcranial magnetic stimulation with transcranial direct current stimulation. PLoS One. 2014;9(3):e92540. doi: 10.1371/journal.pone.0092540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bachmann CG, Muschinsky S, Nitsche MA, et al. Transcranial direct current stimulation of the motor cortex induces distinct changes in thermal and mechanical sensory percepts. Clin Neurophysiol. 2010;121(12):2083–2089. doi: 10.1016/j.clinph.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 47.Ihle K, Rodriguez-Raecke R, Luedtke K, May A. tDCS modulates cortical nociceptive processing but has little to no impact on pain perception. Pain. 2014;155(10):2080–2087. doi: 10.1016/j.pain.2014.07.018. [DOI] [PubMed] [Google Scholar]
- 48.Knotkova H, Woods AJ, Bikson M, Nitsche M. Transcranial direct current stimulation (tDCS): What pain practitioners need to know. Prac Pain Manag. 2015;15:58–66. [Google Scholar]
- 49.Nitsche MA, Grundey J, Liebetanz D, Lang N, Tergau F, Paulus W. Catecholaminergic consolidation of motor cortical neuroplasticity in humans. Cereb Cortex. 2004;14(11):1240–1245. doi: 10.1093/cercor/bhh085. [DOI] [PubMed] [Google Scholar]
- 50.Nitsche MA, Jaussi W, Liebetanz D, Lang N, Tergau F, Paulus W. Consolidation of human motor cortical neuroplasticity by D-cycloserine. Neuropsychopharmacology. 2004;29(8):1573–1578. doi: 10.1038/sj.npp.1300517. [DOI] [PubMed] [Google Scholar]
- 51.Nitsche MA, Liebetanz D, Schlitterlau A, et al. GABAergic modulation of DC stimulation-induced motor cortex excitability shifts in humans. Eur J Neurosci. 2004;19(10):2720–2726. doi: 10.1111/j.0953-816X.2004.03398.x. [DOI] [PubMed] [Google Scholar]
- 52.Nitsche MA, Lampe C, Antal A, et al. Dopaminergic modulation of long-lasting direct current-induced cortical excitability changes in the human motor cortex. Eur J Neurosci. 2006;23(6):1651–1657. doi: 10.1111/j.1460-9568.2006.04676.x. [DOI] [PubMed] [Google Scholar]
- 53.Nitsche MA, Kuo MF, Karrasch R, Wächter B, Liebetanz D, Paulus W. Serotonin affects transcranial direct current-induced neuroplasticity in humans. Biol Psychiatry. 2009;66(5):503–508. doi: 10.1016/j.biopsych.2009.03.022. [DOI] [PubMed] [Google Scholar]
- 54.Stagg CJ, Lin RL, Mezue M, et al. Widespread modulation of cerebral perfusion induced during and after transcranial direct current stimulation applied to the left dorsolateral prefrontal cortex. J Neurosci. 2013;33(28):11425–11431. doi: 10.1523/JNEUROSCI.3887-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Peyron R, Laurent B, García-Larrea L. Functional imaging of brain responses to pain. A review and meta-analysis (2000) Neurophysiol Clin. 2000;30(5):263–288. doi: 10.1016/s0987-7053(00)00227-6. [DOI] [PubMed] [Google Scholar]
- 56.Peyron R, Faillenot I, Mertens P, Laurent B, Garcia-Larrea L. Motor cortex stimulation in neuropathic pain. Correlations between analgesic effect and hemodynamic changes in the brain. A PET study. Neuroimage. 2007;34(1):310–321. doi: 10.1016/j.neuroimage.2006.08.037. [DOI] [PubMed] [Google Scholar]
- 57.Polanía R, Paulus W, Nitsche MA. Modulating cortico-striatal and thalamo-cortical functional connectivity with transcranial direct current stimulation. Hum Brain Mapp. 2012;33(10):2499–2508. doi: 10.1002/hbm.21380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dasilva AF, Mendonca ME, Zaghi S, et al. tDCS-induced analgesia and electrical fields in pain-related neural networks in chronic migraine. Headache. 2012;52(8):1283–1295. doi: 10.1111/j.1526-4610.2012.02141.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Garcia-Larrea L, Peyron R. Motor cortex stimulation for neuropathic pain: From phenomenology to mechanisms. Neuroimage. 2007;37(Suppl 1):S71–S79. doi: 10.1016/j.neuroimage.2007.05.062. [DOI] [PubMed] [Google Scholar]
- 60.DosSantos MF, Love TM, Martikainen IK, et al. Immediate effects of tDCS on the µ-opioid system of a chronic pain patient. Front Psychiatry. 2012;3:93. doi: 10.3389/fpsyt.2012.00093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Maihöfner C, Handwerker HO, Neundörfer B, Birklein F. Cortical reorganization during recovery from complex regional pain syndrome. Neurology. 2004;63(4):693–701. doi: 10.1212/01.wnl.0000134661.46658.b0. [DOI] [PubMed] [Google Scholar]
- 62.Pleger B, Tegenthoff M, Ragert P, et al. Sensorimotor retuning [corrected] in complex regional pain syndrome parallels pain reduction. Ann Neurol. 2005;57(3):425–429. doi: 10.1002/ana.20394. [DOI] [PubMed] [Google Scholar]
- 63.Gelman A. Prior distributions for variance parameters in hierarchical models. Bayesian Analysis. 2006;1(3):515–533. [Google Scholar]
- 64.Mcneish D. On Using Bayesian Methods to Address Small Sample Problems. Structural Equation Modeling: A Multidisciplinary Journal. 2016;23(5):750–773. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Correlation between difference scores of clinical and experimental pain measures
| NRS | WOMAC | HPTh, arm | HPTh, knee | HPTo, arm | HPTo, knee | Punctate pain, hand | Punctate pain, patella | PPT, lateral. knee | PPT, medial knee | PPT, quadriceps | PPT, trapezius | CPM | Cold pain | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NRS | 1 | |||||||||||||
| WOMAC | 0.301 | 1 | ||||||||||||
| HPTh, arm | −0.343 | 0.258 | 1 | |||||||||||
| HPTh, knee | −0.438 | 0.063 | 0.301 | 1 | ||||||||||
| HPTo, arm | −0.419 | 0.15 | 0.585** | 0.35 | 1 | |||||||||
| HPTo, knee | −0.522* | 0.042 | 0.233 | 0.522* | 0.511* | 1 | ||||||||
| Punctuate pain, hand | 0.479* | 0.138 | −0.129 | −0.263 | −0.566** | −0.328 | 1 | |||||||
| Punctuate pain, patella | 0.188 | −0.305 | −0.366 | −0.184 | −0.635** | −0.450* | 0.726*** | 1 | ||||||
| PPT, lateral knee | −0.187 | 0.035 | 0.356 | −0.141 | 0.048 | −0.199 | −0.217 | −0.167 | 1 | |||||
| PPT, medial knee | −0.026 | −0.111 | 0.008 | −0.011 | −0.036 | −0.237 | −0.056 | 0.057 | 0.577** | 1 | ||||
| PPT, quadriceps | 0.044 | 0.050 | 0.229 | −0.188 | 0.202 | −0.075 | −0.173 | −0.295 | 0.654** | 0.702*** | 1 | |||
| PPT, trapezius | −0.052 | 0.130 | 0.362 | −0.087 | 0.200 | −0.028 | 0.075 | −0.146 | 0.630** | 0.717*** | 0.785*** | 1 | ||
| CPM | −0.192 | −0.102 | −0.186 | 0.162 | −0.035 | 0.380 | 0.053 | −0.007 | −0.364 | −0.086 | −0.059 | −0.137 | 1 | |
| Cold pain | 0.130 | −0.363 | −0.599** | −0.321 | −0.136 | −0.203 | 0.038 | 0.349 | −0.441 | −0.180 | −0.249 | −0.423 | 0.049 | 1 |
Notes:
P < 0.05,
P < 0.01,
P < 0.001.


