Abstract
Purpose
We investigate the measurable range of subfoveal choroidal thickness (SFCT) with conventional spectral domain optical coherence tomography (SD-OCT) in normal healthy eyes.
Methods
All subjects underwent an SD-OCT horizontal line scan centered at the fovea with standard and enhanced depth imaging (EDI) techniques. Two independent observers manually measured SFCT on standard and EDI-OCT images, if two choroidal borders were identified. The rate of successful measurement with standard OCT was evaluated. Inter- and intraclass correlation coefficients and Bland-Altman plots were used for analysis.
Results
OCT images of 724 normal healthy eyes from 374 subjects were evaluated. Although the inner choroidal border was identified on all OCT images, the outer choroidal border was identified on 378 of 724 (52.2%) conventional OCT images. Mean SFCT of all study eyes measured by EDI-OCT images was 292.6 ± 94.0. The number of successful measurements with conventional OCT was 100%, 87.5%, 48.1%, 33.0%, and 0%, in the SFCT ranges of <241, 241–280, 281–320, 321–360, and >360 μm, respectively. The accumulated rate of successful measurement with conventional OCT was 100%, 96.4%, and 82.2% in the SFCT ranges of ≤240, ≤280, and ≤320 μm, respectively. Two protocols showed good inter-correlation of SFCT, when SFCT were measurable in both scans.
Conclusions
SFCT can be measured by conventional OCT in eyes with thin choroid, and the measured value shows high agreement with those measured by EDI-OCT. In such eyes, conventional OCT can be used potentially to evaluate the retina and choroid.
Translational Relevance
In eyes with a thin choroid, conventional OCT can be used potentially to evaluate the retina and choroid with high agreement with EDI-OCT.
Keywords: choroidal thickness, conventional, enhanced depth imaging, optical coherence tomography
Introduction
Spectral domain optical coherence tomography (SD-OCT) is a noninvasive imaging modality that is used commonly to assess retinal thickness, volume, and morphology in pathologic eyes.1,2 However, evaluating the choroid using standard conventional SD-OCT often is difficult due to the limited signal transmission of the choroidal layer. Recently, the enhanced depth imaging (EDI) technique of SD-OCT and swept source (SS) OCT having longer wavelength were developed to evaluate the choroid.3–6 Choroidal thickness can be measured using these OCT techniques, and abnormal changes of choroidal thickness were reported in many retinochoroidal disorders.7–10
Although SS-OCT can provide retinal and choroidal imaging in one imaging process, it still is not available in many retina clinics, and SD-OCT devices are more popularly used. If an SD-OCT device is available, the standard technique is used for retinal evaluation, and the EDI technique is used for choroidal evaluation in general. Thus, two consecutive OCT imaging processes might be required for evaluation of eyes with a retinochoroidal disorder, which is more time-consuming and inconvenient than one imaging process. Recently, it was reported that EDI-OCT can be used in some retinochoroidal disorders to evaluate the retina and choroid.11 However, the software algorithm in commercially available OCT devices is generally optimized for conventional OCT scan images to reduce automated retinal segmentation error. Furthermore, in some conditions, such as vitreoretinal disorders, conventional OCT still is required for the evaluation, in addition to EDI-OCT.
Interestingly, we observed that the whole choroidal layer can be visualized on conventional OCT images acquired from eyes having a thin choroid, such as those with high myopia and age-related choroidal atrophy. In such eyes, the choroidal thickness, in addition to the retinal thickness, might be measured with conventional OCT, and it will be more desirable to use conventional OCT to evaluate the retina and choroid, if possible. However, most previous studies on eyes with a thin choroid used the EDI technique for the choroidal thickness measurement,7,12–16 probably because little is known about choroidal thickness measurement with conventional OCT. Thus, clarifying the capability and limitations of the standard technique for choroidal thickness measurement could help avoid unnecessary OCT scans and use OCT scan techniques more flexibly. In addition, we can use conventional OCT images for the subfoveal choroidal thickness (SFCT) measurement with confidence.
We investigated the measurable choroidal thickness range for standard conventional SD-OCT, using EDI SD-OCT measurements as control.
Methods
Subjects
We used data from 410 participants (184 males and 226 females) in the Healthy Twin study conducted from May 2013 to December 2013 at the Samsung Medical Center, Seoul, Korea. A more detailed description of the recruitment and protocols of the study has been reported previously.17,18 In brief, the Healthy Twin study has been conducted as a nationwide community-based cohort study since 2005, and has recruited Korean adult twins and their family members to investigate genetic and environmental determinants of a wide range of traits. This study was approved by the institutional review board of Samsung Medical Center, and informed consent was obtained from all participants, adhering to the tenets of the Declaration of Helsinki.
Analysis of Clinical Records, Ocular Measurements, and Fundus Color Photographs
In the Healthy Twin study, all subjects underwent history taking, systemic blood pressure measurements, blood glucose measurements, visual acuity (VA) assessment, intraocular pressure measurement, nondilated refraction measurement with an autorefractor (Topcon AT; Topcon Corp., Tokyo, Japan), and axial length measurement by corneal touch A-scan ultrasonography (Model 820; Allergan-Humphrey, San Leandro, CA). After pupil dilation, color fundus photography was taken with a fundus camera TRC 50 (Topcon, Paramus, New Jersey) or nonmyd 7 (Kowa, Tokyo, Japan). OCT images were obtained with standard and EDI techniques using Spectralis HRA+OCT (version 1.7.0.0; Heidelberg Engineering, Heidelberg, Germany). The cross-sectional line scan centered at the fovea was performed horizontally and consisted of 768 A lines, 9.0 mm long with 100 frame averaging. The automatic real-time mode using an eye-tracker system was activated.
Two retinal specialists (S.Y.P. and M.K.) evaluated clinical records, ocular measurements, color fundus photographs, and OCT images. Eyes with previous history of ocular surgery or ocular conditions that might affect choroidal visualization, such as severe cataract, epiretinal membrane, diabetic retinopathy, retinal vein occlusion, age-related macular degeneration, and signal strength of OCT image ≤ 15 dB (range, 0–30 dB), were excluded. Eyes with incomplete scan data also were excluded.
Analysis of OCT Images
Conventional OCT images of study subjects were analyzed blindly by two well-trained senior residents in the ophthalmology department (G.H. and D.Y.C.) who were blind to each other's measurements. After finishing measurement of all conventional OCT images, the observers analyzed EDI-OCT images blindly to their previous measurements with conventional OCT images. Two (inner and outer) choroidal borders were identified, and SFCT was measured manually using software supplied with the SD-OCT device in eyes having identified two choroidal borders. SFCT was defined as the distance from the outer edge of the hyperreflective line corresponding to the retinal pigment epithelium to the inner surface of the sclera. Interobserver agreement between two observers was evaluated for measurement of SFCT with conventional SD-OCT and EDI-OCT, respectively. Eyes were classified into five thickness groups (SFCT ranges of <241, 241–280, 281–320, 321–360, and >360 μm), according to the SFCT measured by EDI-OCT. If there was disagreement between twi observers on classification, another observer (D.-I.H) made the final decision. The rate of successful measurement with conventional OCT, and the intraobserver agreement of measured SFCT between two OCT methods were evaluated in five thickness groups.
Statistical Analyses
All statistical analyses were performed using SPSS 23.0 software (IBM, Armonk, NY). Agreement of the classification between two observers about visualization of the outer choroidal border on either OCT was calculated, and the level of agreement was determined by the Cohen's κ. Interpretation of κ values was as follows: 0–0.20, slight agreement; 0.21–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, substantial agreement; >0.81, highest agreement.19 P < 0.05 was considered statistically significant. The interobserver reproducibility was evaluated by computing the inter- and intraclass correlation coefficients (ICCs) for the SFCT measurement. ICC values >0.75 were considered to represent excellent repeatability.20 The within subject standard deviation (SW) and the analysis of variance components also were calculated. The clinically relevant magnitude of the difference between the two protocols was evaluated by Bland-Altman plots with 95% confidence intervals (CIs) for the mean difference.21
Results
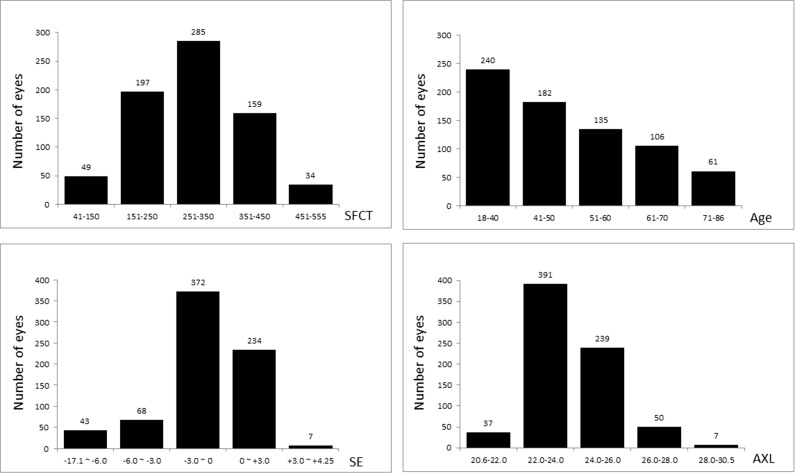
Of 820 eyes of 410 patients, 96 eyes of 60 subjects were excluded: 48 eyes did not complete either the conventional or EDI SD-OCT protocol and 48 had retinal or choroidal abnormalities (two diabetic retinopathies, 15 epiretinal membranes, three retinal vein occlusions, five retinal or subretinal deposits from various etiologies, and 23 age-related macular degeneration eyes). Finally, 724 eyes of 374 subjects (169 males and 205 females) were included. Mean subject age was 49.2 ± 13.6 years (range, 18–86), mean axial length was 23.9 ± 1.3 mm (range, 20.65–30.54), and mean spherical equivalent (SE) was −1.03 ± 2.68 (range, –17.1–+4.25). Table 1 showed clinical characteristics of all study subjects, and Figure 1 depicted the distributions of age, refractive error, and axial length.
Table 1.
Clinical Characteristics of Study Subjects
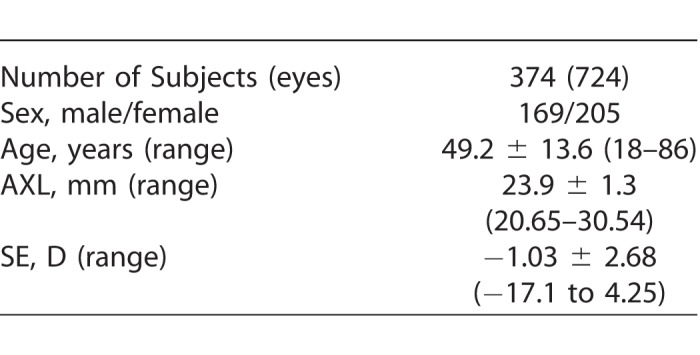
Figure 1.
The number and distribution of eyes in this study according to SFCT, age, SE, and axial length (AXL).
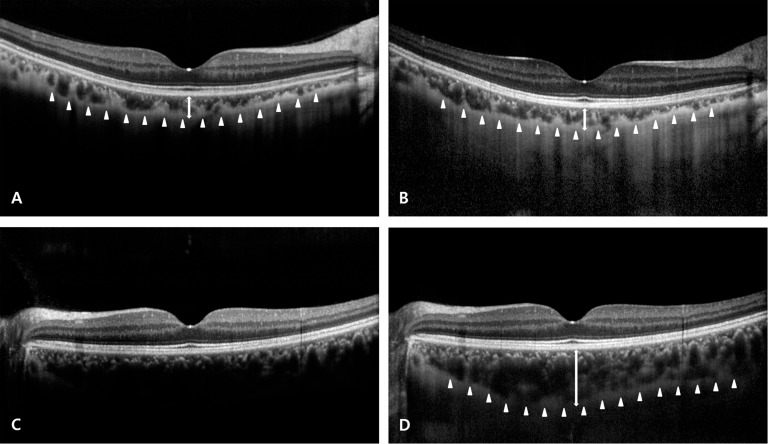
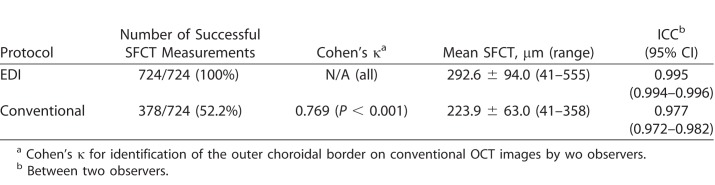
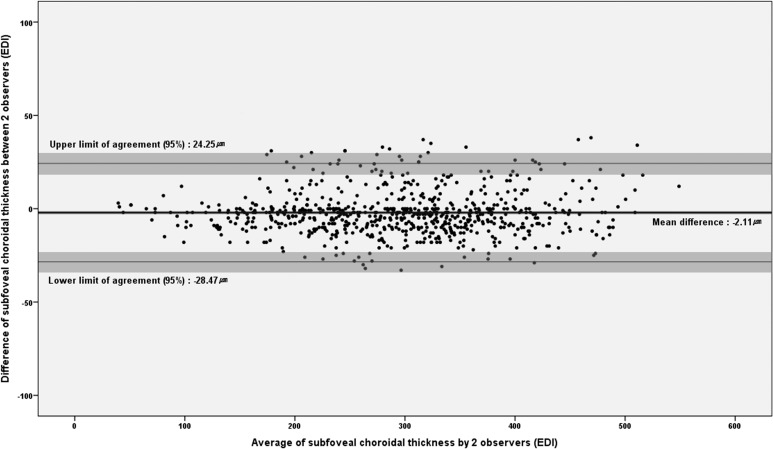
The inner and outer choroidal borders were identified on all EDI-OCT images from 724 eyes. The inner choroidal border also was identified on all standard images from 724 eyes. However, the outer choroidal border was identified only on 378 of 724 (52.2%) conventional OCT images (Fig. 2, Table2). The Cohen's κ for classification according to the identification of outer choroidal border on conventional OCT images by two observers was 0.769 (P < 0.001). SFCT was measured on all EDI-OCT images, and mean SFCT was 292.6 ± 94.0 μm (range, 41–555). The ICC and SW of SFCT measurements with EDI-OCT between 2 observers (G.H. and D.Y.C.) were 0.995 (P < 0.001, 95% CI = 0.994–0.996) and 9.620 μm, respectively (Table 2). Bland-Altman plots were created to analyze the agreement of measurements between two observers with 724 eyes on EDI-OCT images (Fig. 3).
Figure 2.
(A, B) Images of the right eye from a 28-year-old man. (A) The conventional OCT image. The outer choroidal border was clearly visible (white arrowheads) and SFCT was 137 μm (white arrow). (B) The EDI-OCT image. The outer choroidal border (white arrowheads) was visible and SFCT was 139 μm (white arrow). (C, D) Images of the left eye from a 49-year-old woman. (C) The conventional OCT image. The outer choroidal border was invisible and SFCT could not be measured. (D) The EDI-OCT image. The outer choroidal border (white arrowheads) was visible and SFCT was 385 μm (white arrow).
Table 2.
Results of SFCT Measurement With EDI or Conventional OCT Protocol
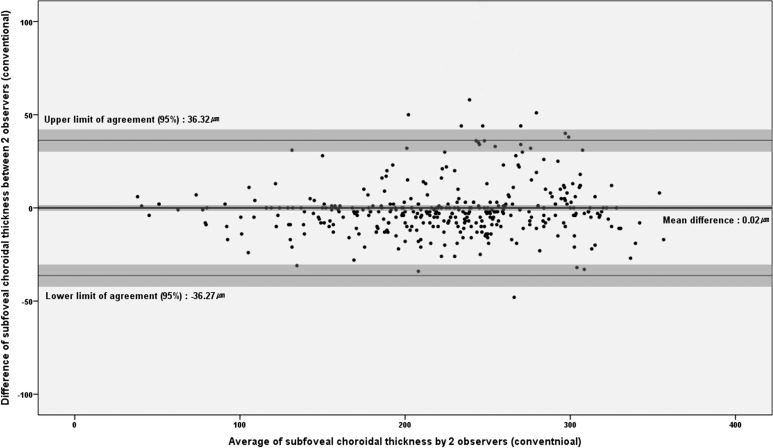
Figure 3.
Bland-Altman plots of the difference by the 2 observers (G.H. and D.Y.C.) in SFCT measurement of EDI-OCT images in 724 eyes. Shaded regions represent the CIs on the mean bias and limits of agreement (LOA). The 95% CIs of the mean bias, upper, and lower LOA were (−3.093, −1.131), (18.671, 29.825), and (−34.049, −22.895), respectively.
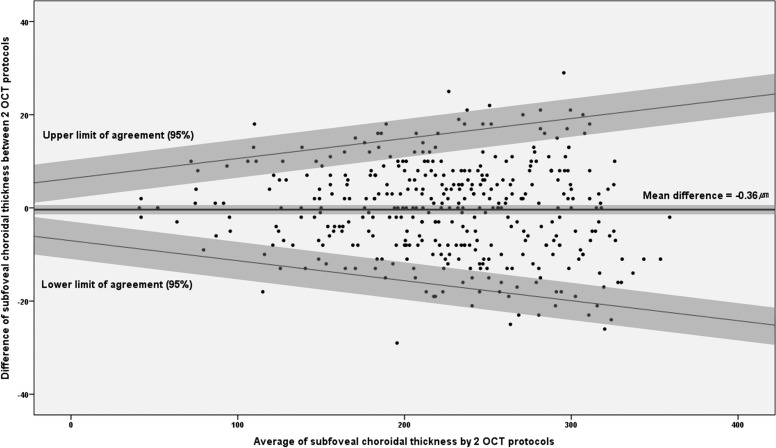
SFCT was measured on 378 conventional OCT images, and mean SFCT was 223.9 ± 63.0 μm (range, 41–358 μm). The ICC and SW of SFCT measurements with conventional OCT between two observers (G.H. and D.Y.C.) was 0.977 (P < 0.001, 95% CI = 0.972–0.982) and 13.078 μm, respectively (Table 2). Bland-Altman plots for analysis of the agreement between two observers with 378 eyes on conventional OCT images are shown in Figure 4. The ICC and SW between measurements of EDI-OCT and conventional OCT by G.H. was 0.994 (P < 0.001, 95% CI = 0.992–0.995) and 7.153 μm, respectively. Variance components models are shown in Supplemental Tables S1 to S3.
Figure 4.
Bland-Altman plots of the difference by the two observers (G.H. and D.Y.C.) in SFCT measurement of conventional OCT images in 378 eyes. Shaded regions represent the CIs on the mean bias and LOA. The 95% CIs of the mean bias, upper and lower LOA were (−1.849, 1.897), (30.247, 42.395), and (−42.347, −30.199), respectively.
Eyes were classified into five thickness groups according to the SFCT measured by EDI-OCT. The number of conventional OCT images on which SFCT was measured was 221 of 221 (100%), 77 of 88 (87.5%), 62 of 129 (48.1%), and 18 of 114 (33.0%) in the thickness group having SFCT of <241, 241–280, 281–320, and 321–360 μm, respectively. SFCT could not be measured in any conventional OCT image in the thickness group with SFCT > 360 μm. Overall, the accumulated rate of successful measurement was 100% (221/221), 96.4% (298/309), 82.2% (360/438), 68.5% (378/522), and 52.2% (378/724) in the SFCT ranges of ≤240, ≤280, ≤320, ≤360, and ≤555 μm, respectively. Numbers of SFCT measured images, successful measurement rate, and ICC according to the SFCT range are presented in Table 3.
Table 3.
Number of SFCT Measured Images and Agreement of SFCT Measured by Conventional SD-OCT With SFCT Measured by EDI SD-OCT
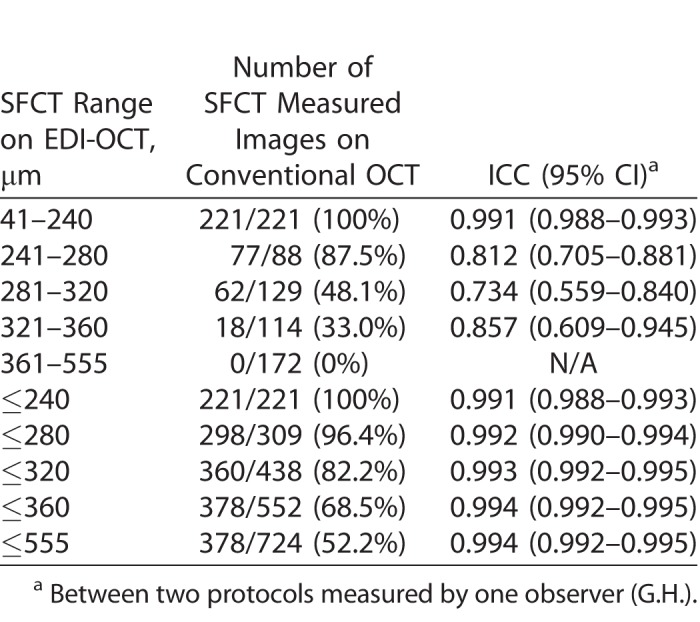
A Bland-Altman plot was created to analyze the individual differences in measurements between the conventional OCT and EDI-OCT protocols in 378 eyes in which SFCT was measured on conventional and EDI-OCT images (Fig. 5). The differences in SFCT between the two protocols were normally distributed (Shapiro-Wilcoxon test, P = 0.263). When the differences in SFCT between the two protocols were plotted against the average values measured by the conventional and EDI protocols, the mean difference in SFCT between both protocols was −0.36 μm.
Figure 5.
Bland-Altman plots of the difference by the two OCT scan protocols (conventional versus EDI scan) in SFCT measurement of 378 eyes. Shaded regions represent the CIs on the mean bias and LOA. The 95% CIs of the mean bias were (−1.386, 0.664). The 95% upper and lower LOAs were Y = (0.021X + 3.409) × (±1.96) − 0.360. The 95% CIs of upper and lower LOA were Y = (0.021X + 3.409 ± 1.095 × 1.96) × 1.96 − 0.360 and Y = (0.021X + 3.409 ± 1.095 × 1.96) × (−1.96) − 0.360, respectively.
Discussion
EDI-OCT or SS-OCT, instead of conventional OCT, has become the general modality to visualize the choroidal layer in eyes with choroidal or retinochoroidal disorder, because of insufficient capability of conventional OCT to visual the choroidal layer.3–10 However, in eyes with a thin choroid, even conventional OCT can visualize the whole choroid, including the outer choroidal border, which is essential for reliable SFCT measurement. However, the capability of conventional OCT to measure choroidal thickness remains unclear. To our knowledge, this study is the first investigation of the measurable range of SFCT, which is the range showing the whole choroidal layer including the visible outer choroidal border, for conventional OCT.
In this study, 240 μm was the upper value of the SFCT range in which SFCT of all eyes can be measured with conventional OCT, and 280 μm is the upper value of the SFCT range in which SFCT of almost all eyes is measurable. Furthermore, SFCT could be measured with conventional OCT in more than 3/4 of eyes having an SFCT of not more than 320 μm. The normal choroidal thickness in healthy subjects is approximately 250 to 350 μm, which varies, depending on many factors, including age, sex, refractive error, and diurnal variation.22–32 Considering the normal SFCT and average SFCT (292.6 μm) values in this study, it appears that SFCT can be measured by conventional OCT in most eyes having SFCT less than the normal average value.
This study also investigated the agreement of measured SFCT between conventional OCT and EDI-OCT. The agreement was acceptably high in all measurable SFCT ranges. However, the Bland-Altman plots showed a trend that difference in measurements between two protocols increases as the choroidal thickness increases. Therefore, further studies are needed, considering that the number of study eyes in the range of severely thick choroid was relatively small, and some pathologic eyes could have a choroid thicker than 555 μm, which were not included in this study.
The current results have the following clinical significance. First, according to the current data, conventional OCT using the Spectralis HRA+OCT with 100 frame averaging, can be used to measure retinal and choroidal thickness in some thin-choroid eyes, such as those with high myopia, reticular pseudodrusen, and age-related choroidal atrophy, reducing the scan time and patient discomfort. Conversely, it also is speculated that in an eye with a thick choroid where the outer choroidal border is not seen on conventional OCT, EDI-OCT should be considered to measure choroidal thickness.
Second, in clinical practice, if the outer choroidal border is visible on images of conventional OCT, SFCT can be measured by conventional OCT with high agreement with EDI-OCT, even if SFCT is higher than the mean SFCT of normal eyes. EDI-OCT is not obligatorily required in this case. Third, in designing the clinical study, requirement of the EDI-OCT or SS-OCT technique can be determined according to the known choroidal characteristics of study subjects. There are many thin choroid disorders, including high myopia and age-related choroidal atrophy. In clinical studies of some thin choroid disorders, conventional OCT can be used instead of EDI-OCT or SS-OCT. Fourth, measurements of SFCT by conventional OCT could be used interchangeably with those made by EDI-OCT if the outer choroidal border was visible in conventional OCT.
In this study, the measurability of SFCT was dependent on the visibility of the outer choroidal border, which appeared to be determined, not only by choroidal thickness, but also by many other factors. Lens or vitreous opacity and pigmentation of RPE affected the visibility, although further studies are needed.
Eyes with high myopia and a long axial length up to 30.54 mm were included in this study, and SFCT measurement was successful on all images of these eyes. Thus, high myopia with long axial length does not appear to be an obstacle for SFCT measurement by conventional OCT.
We previously investigated the EDI-OCT measurements of retinal thickness and volume and found a high agreement with those of conventional OCT.11 EDI-OCT could be used to evaluate the retina and choroid in normal eyes and in eyes with some forms of chorioretinal disorder. Conversely, our study showed that conventional OCT could measure retinal thickness and SFCT in some eyes. Thus, if the capability of conventional or EDI-OCT is better known, they can be used more flexibly without losing reliability of measured data, and such flexibility in OCT imaging could reduce scanning time and patient discomfort.
This study had several limitations. Various kind of pathologic eyes, such as those with age-related macular degeneration, reticular pseudodrusen, and retinitis pigmentosa, were not included in the study subjects. Some pathologic eyes have retinal or retinal pigment epithelial changes that could affect visualization of the choroid by OCT. Thus, further studies are needed to evaluate the influence of such changes on the SFCT measurement with conventional OCT. Only one SD-OCT device was used for the evaluation, although various kinds of commercially available SD-OCT devices exist with a scan mode similar to the EDI technique. Further studies are needed for other SD-OCT devices. On some conventional images, an imaginary line might be used for SFCT measurement if the outer choroidal border is unidentifiable. However, we did not use the imaginary line technique, because it could induce some errors in measurement and difficulties in the interpretation of data if subjective decision is used.
In summary, conventional SD-OCT could be used for to measure choroidal thickness in eyes with a thin choroid. In addition, if the outer choroidal border was visible on conventional OCT images, SFCT measurements by conventional OCT were almost the same as those by EDI-OCT.
Supplementary Material
Acknowledgments
Supported by the National Research Foundation of Korea (Grant Number #2011-220-E00006 and # 2010-0029113), a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI, funding HI14C0064) and by Global Research Network Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (#2011-220-E00006 & #2012-0004255). The authors alone are responsible for the content and writing of this paper.
Involved in conception and design (M.K., S.Y.P., J.S., D.-I.H.) and conduct of the study (M.K., D.Y.C., G.H., S.Y.P., J.S., D.-I.H.); collection, management and interpretation of data (M.K., D.Y.C., G.H., Y.-M.S., S.Y.P., J.S., D.-I.H.); data analysis (M.K., D.Y.C., G.H., Y.-M.S., S.Y.P., J.S., S.H., D.-I.H.); writing the article (M.K., D.-I.H.); and preparation, review, and approval of the manuscript (M.K., J.S., D.-I.H.).
Disclosure: M. Kong, None; D.Y. Choi, None; G. Han, None; Y.-M. Song, None; S.Y. Park, None; J. Sung, None; S. Hwang, None; D.-I. Ham, None
References
- 1.Domalpally A, Gangaputra S, Peng Q, Danis RP. Repeatability of retinal thickness measurements between spectral-domain and time-domain optical coherence tomography images in macular disease. Ophthalmic Surg Lasers Imaging. 2010;41(suppl):S34–S41. doi: 10.3928/15428877-20100325-01. [DOI] [PubMed] [Google Scholar]
- 2.Lammer J, Scholda C, Prunte C, Benesch T, Schmidt-Erfurth U, Bolz M. Retinal thickness and volume measurements in diabetic macular edema: a comparison of four optical coherence tomography systems. Retina. 2011;31:48–55. doi: 10.1097/IAE.0b013e3181e095a4. [DOI] [PubMed] [Google Scholar]
- 3.Barteselli G, Chhablani J, El-Emam S, et al. Choroidal volume variations with age, axial length, and sex in healthy subjects: a three-dimensional analysis. Ophthalmology. 2012;119:2572–2578. doi: 10.1016/j.ophtha.2012.06.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chhablani J, Barteselli G, Wang H, et al. Repeatability and reproducibility of manual choroidal volume measurements using enhanced depth imaging optical coherence tomography. Invest Ophthalmol Vis Sci. 2012;53:2274–2280. doi: 10.1167/iovs.12-9435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirata M, Tsujikawa A, Matsumoto A, et al. Macular choroidal thickness and volume in normal subjects measured by swept-source optical coherence tomography. Invest Ophthalmol Vis Sci. 2011;52:4971–4978. doi: 10.1167/iovs.11-7729. [DOI] [PubMed] [Google Scholar]
- 6.Spaide RF, Koizumi H, Pozzoni MC. Enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol. 2008;146:496–500. doi: 10.1016/j.ajo.2008.05.032. [DOI] [PubMed] [Google Scholar]
- 7.Ho M, Liu DT, Chan VC, Lam DS. Choroidal thickness measurement in myopic eyes by enhanced depth optical coherence tomography. Ophthalmology. 2013;120:1909–1914. doi: 10.1016/j.ophtha.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 8.Maruko I, Iida T, Sugano Y, Ojima A, Ogasawara M, Spaide RF. Subfoveal choroidal thickness after treatment of central serous chorioretinopathy. Ophthalmology. 2010;117:1792–1799. doi: 10.1016/j.ophtha.2010.01.023. [DOI] [PubMed] [Google Scholar]
- 9.Razavi S, Souied EH, Cavallero E, Weber M, Querques G. Assessment of choroidal topographic changes by swept source optical coherence tomography after photodynamic therapy for central serous chorioretinopathy. Am J Ophthalmol. 2014;157:852–860. doi: 10.1016/j.ajo.2013.12.029. [DOI] [PubMed] [Google Scholar]
- 10.Ueda-Arakawa N, Ooto S, Ellabban AA, et al. Macular choroidal thickness and volume of eyes with reticular pseudodrusen using swept-source optical coherence tomography. Am J Ophthalmol. 2014;157:994–1004. doi: 10.1016/j.ajo.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 11.Park SY, Kim SM, Song YM, Sung J, Ham DI. Retinal thickness and volume measured with enhanced depth imaging optical coherence tomography. Am J Ophthalmol. 2013;156:557–566. doi: 10.1016/j.ajo.2013.04.027. e552. [DOI] [PubMed] [Google Scholar]
- 12.Fujiwara T, Imamura Y, Margolis R, Slakter JS, Spaide RF. Enhanced depth imaging optical coherence tomography of the choroid in highly myopic eyes. Am J Ophthalmol. 2009;148:445–450. doi: 10.1016/j.ajo.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 13.Ikuno Y, Jo Y, Hamasaki T, Tano Y. Ocular risk factors for choroidal neovascularization in pathologic myopia. Invest Ophthalmol Vis Sci. 2010;51:3721–3725. doi: 10.1167/iovs.09-3493. [DOI] [PubMed] [Google Scholar]
- 14.Ikuno Y, Tano Y. Retinal and choroidal biometry in highly myopic eyes with spectral-domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2009;50:3876–3880. doi: 10.1167/iovs.08-3325. [DOI] [PubMed] [Google Scholar]
- 15.Querques G, Querques L, Forte R, Massamba N, Coscas F, Souied EH. Choroidal changes associated with reticular pseudodrusen. Invest Ophthalmol Vis Sci. 2012;53:1258–1263. doi: 10.1167/iovs.11-8907. [DOI] [PubMed] [Google Scholar]
- 16.Spaide RF. Age-related choroidal atrophy. Am J Ophthalmol. 2009;147:801–810. doi: 10.1016/j.ajo.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 17.Sung J, Cho SI, Lee K, et al. Healthy Twin: a twin-family study of Korea--protocols and current status. Twin Res Hum Genet. 2006;9:844–848. doi: 10.1375/183242706779462822. [DOI] [PubMed] [Google Scholar]
- 18.Sung J, Cho SI, Song YM, et al. Do we need more twin studies? The Healthy Twin Study, Korea. Int J Epidemiol. 2006;35:488–490. doi: 10.1093/ije/dyi294. [DOI] [PubMed] [Google Scholar]
- 19.Lin DY, Blumenkranz MS, Brothers RJ, Grosvenor DM. The sensitivity and specificity of single-field nonmydriatic monochromatic digital fundus photography with remote image interpretation for diabetic retinopathy screening: a comparison with ophthalmoscopy and standardized mydriatic color photography. Am J Ophthalmol. 2002;134:204–213. doi: 10.1016/s0002-9394(02)01522-2. [DOI] [PubMed] [Google Scholar]
- 20.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8:135–160. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- 21.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 22.Branchini L, Regatieri CV, Flores-Moreno I, Baumann B, Fujimoto JG, Duker JS. Reproducibility of choroidal thickness measurements across three spectral domain optical coherence tomography systems. Ophthalmology. 2012;119:119–123. doi: 10.1016/j.ophtha.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Copete S, Flores-Moreno I, Montero JA, Duker JS, Ruiz-Moreno JM. Direct comparison of spectral-domain and swept-source OCT in the measurement of choroidal thickness in normal eyes. Br J Ophthalmol. 2014;98:334–338. doi: 10.1136/bjophthalmol-2013-303904. [DOI] [PubMed] [Google Scholar]
- 24.Ding X, Li J, Zeng J, et al. Choroidal thickness in healthy Chinese subjects. Invest Ophthalmol Vis Sci. 2011;52:9555–9560. doi: 10.1167/iovs.11-8076. [DOI] [PubMed] [Google Scholar]
- 25.Fujiwara A, Shiragami C, Shirakata Y, Manabe S, Izumibata S, Shiraga F. Enhanced depth imaging spectral-domain optical coherence tomography of subfoveal choroidal thickness in normal Japanese eyes. Jpn J Ophthalmol. 2012;56:230–235. doi: 10.1007/s10384-012-0128-5. [DOI] [PubMed] [Google Scholar]
- 26.Kim M, Kim SS, Koh HJ, Lee SC. Choroidal thickness, age, and refractive error in healthy Korean subjects. Optom Vis Sci. 2014;91:491–496. doi: 10.1097/OPX.0000000000000229. [DOI] [PubMed] [Google Scholar]
- 27.Manjunath V, Taha M, Fujimoto JG, Duker JS. Choroidal thickness in normal eyes measured using Cirrus HD optical coherence tomography. Am J Ophthalmol. 2010;150:325–329. doi: 10.1016/j.ajo.2010.04.018. e321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ozdogan Erkul S, Kapran Z, Uyar OM. Quantitative analysis of subfoveal choroidal thickness using enhanced depth imaging optical coherence tomography in normal eyes. Int Ophthalmol. 2014;34:35–40. doi: 10.1007/s10792-013-9787-6. [DOI] [PubMed] [Google Scholar]
- 29.Rahman W, Chen FK, Yeoh J, Patel P, Tufail A, Da Cruz L. Repeatability of manual subfoveal choroidal thickness measurements in healthy subjects using the technique of enhanced depth imaging optical coherence tomography. Invest Ophthalmol Vis Sci. 2011;52:2267–2271. doi: 10.1167/iovs.10-6024. [DOI] [PubMed] [Google Scholar]
- 30.Ruiz-Medrano J, Flores-Moreno I, Pena-Garcia P, Montero JA, Duker JS, Ruiz-Moreno JM. Macular choroidal thickness profile in a healthy population measured by swept-source optical coherence tomography. Invest Ophthalmol Vis Sci. 2014;55:3532–3542. doi: 10.1167/iovs.14-13868. [DOI] [PubMed] [Google Scholar]
- 31.Shao L, Xu L, Chen CX, et al. Reproducibility of subfoveal choroidal thickness measurements with enhanced depth imaging by spectral-domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2013;54:230–233. doi: 10.1167/iovs.12-10351. [DOI] [PubMed] [Google Scholar]
- 32.Yamashita T, Yamashita T, Shirasawa M, Arimura N, Terasaki H, Sakamoto T. Repeatability and reproducibility of subfoveal choroidal thickness in normal eyes of Japanese using different SD-OCT devices. Invest Ophthalmol Vis Sci. 2012;53:1102–1107. doi: 10.1167/iovs.11-8836. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.