Abstract
Background
Understanding which therapeutic innovations in diabetes represent the best value requires rigorous economic evaluation. Data from randomised controlled trials and observational studies indicate that insulin degludec has a hypoglycemia advantage versus insulin glargine 100 units/mL (glargine U100), the most widely prescribed basal insulin analogue in the UK. This analysis was done to more rigorously assess cost-effectiveness in a UK setting.
Methods
Data from two double-blinded, randomised, two-period crossover trials in type 1 (SWITCH 1) and type 2 (SWITCH 2) diabetes mellitus were used to assess the cost-effectiveness of degludec vs. glargine U100 with an economic model. Cost-effectiveness was analysed over a 1-year time horizon based on the different rates of hypoglycaemia and actual doses of insulin used, rather than glycaemic control due to the treat-to-target trial design.
Results
In type 1 diabetes mellitus, degludec was highly cost-effective compared with glargine U100, with an incremental cost-effectiveness ratio of £984 (increased costs of only £23/year and improvement in participant health of 0.0232 quality-adjusted life-years (QALYs)). In type 2 diabetes mellitus, it was estimated that quality of life was improved (0.0065 QALYs gain) with degludec compared with glargine U100 at an increased annual cost of £117 (incremental cost-effectiveness ratio, £17,939). One-way sensitivity analyses showed that the results were robust to changes in parameters in both type 1 and type 2 diabetes mellitus.
Conclusions
The rigorous design of the SWITCH trials, coupled with a representative patient population and a definition of hypoglycaemia that is relevant for real-world patients, makes the results of these trials highly generalisable. The within-trial analysis has the added value of being able to include doses and event rates directly from the trials. This short-term economic analysis estimated that IDeg would be cost-effective relative to IGlar U100 in both type 1 and type 2 diabetes mellitus in the UK.
Trial Registration
SWITCH 1 (NCT02034513); SWITCH 2 (NCT02030600).
Funding
Novo Nordisk, Søborg, Denmark.
Electronic supplementary material
The online version of this article (10.1007/s13300-018-0478-1) contains supplementary material, which is available to authorised users.
Keywords: Cost-effectiveness, Diabetes, Hypoglycaemia, Insulin degludec, Insulin glargine, Pharmacoeconomics, Type 1 diabetes, Type 2 diabetes
Introduction
Healthcare systems are under increasing financial pressure from a growing chronic disease burden, particularly diabetes, which involves the cost of treating the disease as well as its complications [1]. In type 1 diabetes mellitus (T1DM), insulin replacement is an absolute requirement, and insulin is also often necessary to achieve satisfactory glycaemic control in people with more advanced type 2 diabetes mellitus (T2DM). Basal insulin analogues represent one of many therapeutic innovations in diabetes care, and understanding which treatments represent best value—thus meriting reimbursement or inclusion in guidelines or formularies—requires robust economic evaluation as well as solid clinical data. However, for evaluations to be truly representative, the data upon which they are based need to be as reflective of clinical practice as much as possible. Data from randomised clinical trials are limited because the participants enrolled are not typically reflective of those who will eventually be prescribed the medications in routine clinical care. By comparison, real-world studies of participants in regular clinical practice tend to lack the rigour of randomised controlled trials, and the data may suffer from various selection biases due to being observational and open label.
Here we report a cost-effectiveness analysis (CEA) of a novel basal insulin analogue, insulin degludec (degludec), from a UK perspective. The analysis is based on data from two unique, randomised, two-period crossover trials (SWITCH 1 in T1DM [2] and SWITCH 2 in T2DM [3]), which overcomes many of the limitations mentioned above. Consequently, data from these two trials provide robust evidence of cost-effectiveness in order to help clinicians and payers make the most informed decisions about treatment and reimbursement.
Degludec has a distinct pharmacokinetic and pharmacodynamic profile [4–6]. Studies have shown that, depending on the type of diabetes and how hypoglycaemia is assessed (e.g. confirmed, nocturnal confirmed or severe hypoglycaemia), in the general population of enrolled patients who meet the inclusion criteria of these regulatory trials, degludec is associated with a reduction in hypoglycaemic events of between 17 and 86% compared with glargine U100 [7]. This is important because hypoglycaemia is a key driver of avoidable healthcare costs and decreased quality of life for participants, and it limits their ability to achieve desired glycaemic targets [8–11]. Hypoglycaemia was the primary endpoint in the SWITCH trials, and they were powered for that endpoint. The robustness and generalisability of the data from these two trials lend themselves to a confirmatory analysis of cost-effectiveness. As glargine U100 is the most prescribed basal insulin analogue in the UK, these results should be of interest to both healthcare providers and payers.
Methods
Sources of Data
In both SWITCH trials, degludec was compared to insulin glargine 100 units/mL (glargine U100). Importantly, both trials included participants with a higher risk of hypoglycaemia as determined by trial inclusion criteria (i.e. at least one of the following: experienced at least one severe hypoglycemic episode within the last year; moderate chronic renal failure; hypoglycemic symptom unawareness; exposure to insulin for longer than 5 years; or an episode of hypoglycemia (symptoms and/or blood glucose level ≤ 70 mg/dL) within the previous 12 weeks) [3], and thus are considered to be more representative of real-world clinical practice than the group of randomised controlled trials conducted for regulatory purposes, which excluded such patients (BEGIN® clinical trial programme). Secondly, the SWITCH trials used a two-period (32 weeks each) crossover design in which each participant ultimately received both treatments, thereby minimising treatment bias. Finally, the trials were each double-blinded, so that neither participants nor investigators knew which insulin was being injected. Double-blinding is typically difficult to implement in large clinical trials of insulin analogues because they are marketed in proprietary, pen-type delivery devices unique to each product. In the SWITCH trials, each native formulation was administered using indistinguishable vials and syringes. Trial designs and key findings are summarised in Table 1.
Table 1.
Characteristics and primary findings of the SWITCH 1 and SWITCH 2 trials
| SWITCH 1a (NCT02034513) |
SWITCH 2b (NCT02030600) |
|
|---|---|---|
| Design | Multicentre (84 sites in US and 6 in Poland), randomised, double-blinded, two-period (32 weeks each) crossover | Multicentre (152 sites in US), randomised, double-blinded, two-period (32 weeks each) crossover |
| Participants | Type 1 diabetes mellitus; n = 501 adults | Type 2 diabetes mellitus; n = 721 adults |
| Eligibility | ≥1 hypoglycaemia risk factors and previously treated with either a basal–bolus regimen or continuous subcutaneous insulin infusion for ≥ 26 weeks | ≥1 hypoglycaemia risk factors and previously treated with basal insulin with or without oral antidiabetic drugs for ≥ 26 weeks. Participants treated with bolus/premixed insulin or sulfonylurea/meglitinide within 26 weeks of the first trial visit were excluded |
| Treatment |
Basal–bolus therapy Degludec or glargine U100 once daily, administered either in the morning or in the evening as determined by randomisation. Insulin aspart was the mealtime insulin |
Basal-only therapy IDeg or glargine U100 once daily, administered either in the morning or in the evening as determined by randomisation. Pre-trial OAD(s) were continued |
| Duration | 2 × 32 weeks (titration: weeks 1–16 and 32–48; maintenance: weeks 17–32 and 49–64) | 2 × 32 weeks (titration: weeks 1–16 and 32–48; maintenance: weeks 17–32 and 49–64) |
| Efficacy findings | Non-inferiority of degludec vs. glargine U100 with respect to HbA1c was confirmed for the titration period and the maintenance period (6.9 vs. 6.8% [52 mmol/mol vs. 51 mmol/mol] and 7.0 vs. 7.0% [52 mmol/mol vs. 53 mmol/mol], for weeks 32 and 64, respectively) | Non-inferiority of IDeg vs. glargine U100 with respect to HbA1c was confirmed for the titration period and the maintenance period (7.1 vs. 7.0% [54 mmol/mol vs. 53 mmol/mol] and 7.1 vs. 7.1% [54 mmol/mol vs. 54 mmol/mol], for weeks 32 and 64, respectively) |
| Safety findings | The cumulative rates of severe hypoglycaemia for the three different hypoglycaemia endpointsc were significantly lower, by 6–36%, depending on the endpoint and time period, for degludec vs. glargine U100 during both the maintenance period and the full treatment period | The cumulative rate of severe hypoglycaemia was numerically lower, by 23–51%, for degludec vs. glargine U100, and these differences were statistically significant for all but one of the endpoints |
Secondary confirmatory endpoints: number of severe or BG-confirmed symptomatic nocturnal (00:01–05:59) hypoglycaemic episodes and proportion of participants with severe hypoglycaemia during the maintenance period
Glargine U100, insulin glargine 100 units/mL
aLane et al. [2]
bWysham et al. [3]
cPrimary endpoint: number of severe (requiring third-party aid, externally adjudicated) or blood glucose (BG)-confirmed (< 56 mg/dL) symptomatic hypoglycaemic episodes during the maintenance period
Economic Model
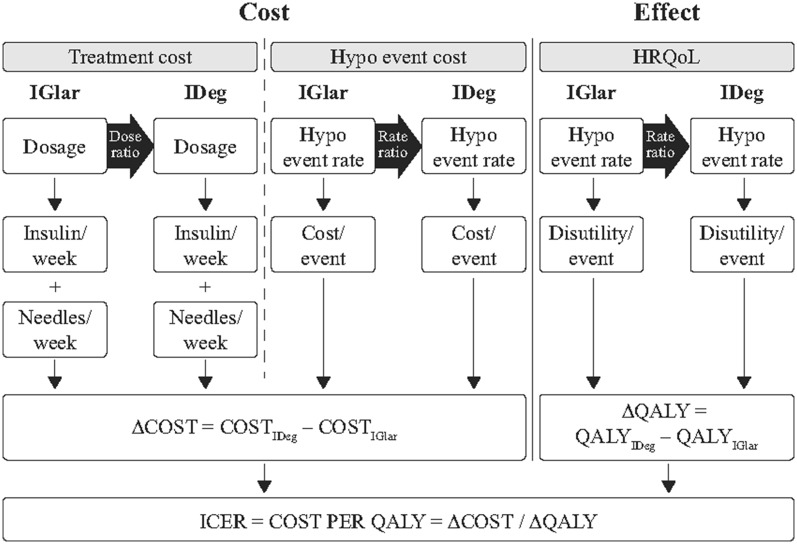
A cost-effectiveness model with QALYs as the effect measure (also called a cost-utility model) was used to compare degludec with glargine U100 based on clinical data from SWITCH 1 [2] and SWITCH 2 [3]. The framework for the cost-effectiveness model has been published previously [12].
The SWITCH trials [2, 3] were conducted in accordance with the Declaration of Helsinki and ICH Good Clinical Practice. Prior to trial initiation, the protocol, consent form and patient information sheet were reviewed and approved by appropriate health authorities and an independent ethics committee/institutional review board. All patients provided signed informed consent.
The modelling process is shown in Fig. 1. The cost-effectiveness of degludec was analysed over a 1-year time horizon. This represents the average annual cost-effectiveness in a steady state and not necessarily only the results after 1 year. This short-term approach based on the different rates of hypoglycaemia and actual doses of insulin used is appropriate since the treat-to-target efficacy trials required by regulatory bodies do not generally result in differences in glycaemic control between comparators; therefore, modelling long-term glycaemic control would not result in differences other than random variation. The model uses only treatment effects for which a statistically significant difference between the treatment arms is documented, and assumes that all other differences are due to random variation (i.e. equivalent to classical statistical tests where the null hypothesis could not be rejected). However, nonsignificant differences were explored in the sensitivity analysis. As the time horizon for the analysis was 1 year, no discounting (adjustment of future values to the present value) was applied. The analysis was conducted from the perspective of the UK National Health Service.
Fig. 1.
Cost-effectiveness modelling of degludec. Reprinted with the permission of the publisher (Taylor & Francis Ltd, http://www.tandfonline.com) [12]. HRQoL health-related quality of life, hypo hypoglycaemia, ICER incremental cost-effectiveness ratio, IDeg insulin degludec, IGlar insulin glargine U100, QALY quality-adjusted life-year
Insulin Use
Units of basal insulin used per day for the degludec and glargine U100 treatment groups were captured from the clinical trial data, and dose reductions were estimated with log-transformed end-of-trial doses, employing treatment, period, dosing time and visit as fixed effects, subject as a random effect and the log-transformed baseline dose as a covariate. For type 1 diabetes mellitus, the glargine U100 basal dose (40.58 units/day) and degludec/glargine U100 basal dose ratio (0.97 [0.94; 0.99] 95 % confidence interval [CI], p < 0.05) were derived from SWITCH 1. The bolus dose used in the glargine U100 arm (31.93 U/day) and the bolus dose ratio for the two arms (degludec/glargine U100) (0.97 [0.94; 1.01] 95 % CI, p > 0.05) were also derived from SWITCH 1. The dose ratios, adjusted for covariates, were used to calculate the corresponding doses in the degludec arm, as can be seen in Table 2. For type 2 diabetes mellitus, only basal insulin was used (BOT, basal-only therapy). The glargine U100 basal dose (82.66 units/day) and degludec/glargine U100 basal dose ratio [0.96 (0.94; 0.98) 95 % CI, p < 0.05] were derived from SWITCH 2.
Table 2.
Use of basal and bolus insulin in the SWITCH 1 and SWITCH 2 trials
| Treatment group | Observed glargine U100 (units/day) | Dose ratio (degludec/glargine U100) [95% CI] |
Calculated degludec (units/day) |
|---|---|---|---|
| SWITCH 1: T1DMB/B | |||
| Total dose (U) | 0.97 [0.95; 0.99] | ||
| Basal insulin (U) | 40.58 | 0.97 [0.95; 0.99] | 39.36a |
| Bolus insulin (U) | 31.93 | 0.97 [0.94; 1.01] (NS) | 31.93 |
| SWITCH 2: T2DMBOT | |||
| Total dose (U) | 0.96 [0.94; 0.98] | ||
| Basal insulin (U) | 82.66 | 0.96 [0.94; 0.98] | 79.35 |
| Bolus insulin (U) | N/A | N/A | N/A |
aObserved glargine U100 units/day × dose ratio
A dose ratio of 1.0 was used when the difference was not statistically significant
B/B basal–bolus therapy, BOT basal-only therapy, CI confidence interval, glargine U100 insulin glargine 100 units/mL, N/A not applicable, NS not significant, T1DM type 1 diabetes mellitus, T2DM type 2 diabetes mellitus
Hypoglycaemic Events
Hypoglycaemic events were obtained by pooling data from the two full crossover periods in the SWITCH 1 [2] and SWITCH 2 trials [3]. For the purposes of our cost-effectiveness model, rates of hypoglycaemia were divided into three mutually exclusive groups: severe events, nonsevere events occurring during the day (diurnal including unknown time) and nonsevere events occurring during the night (nocturnal). These groups were meaningful in terms of costs and impact on quality of life. By ensuring that the groups were mutually exclusive due to stringent criteria for defining hypoglycemia, double counting of events was avoided. In both trials, non-severe hypoglycaemia was defined as a symptomatic event with a confirmed blood glucose level < 3.1 mmol/L (56 mg/dL). Hypoglycaemic events were pre-specified: nocturnal hypoglycaemia was defined as an event occurring between 00:01 and 05:59 am, and severe hypoglycaemia was defined as an episode of hypoglycaemia requiring medical assistance and/or assistance from a third party [13].
The number of events for the rate ratios were analysed using a Poisson model with logarithm of the exposure time as offset (Table 3). The model included treatment, period, sequence and dosing time as fixed effects and subject as a random effect. Rate ratios and 95% CIs used in the model for various types of hypoglycaemic event are shown in Table 3 for type 1 and type 2 diabetes mellitus. The degludec/glargine U100 rate ratios, adjusted for covariates, were applied to the glargine U100 hypoglycaemia rates per person-year to estimate the degludec hypoglycaemia rates, as can be seen in Table 3.
Table 3.
Calculation of hypoglycaemic event rates
| Nonsevere hypoglycaemia | Severe hypoglycaemia | ||
|---|---|---|---|
| Daytime | Nocturnal | ||
| SWITCH 1 T1DMB/B | |||
| Total events per patient per year for glargine U100 | 17.18 | 3.45 | 1.05 |
| Degludec/glargine U100 hypoglycaemic event rate ratio [95% CI] | 0.98 [0.94; 1.03] p = 0.457 | 0.76 [0.69; 0.84] p < 0.0001 | 0.74 [0.61; 0.91] p = 0.0037 |
| Calculated degludec hypoglycaemic event ratea | 17.18 | 2.62 | 0.78 |
| SWITCH 2 T2DMBOT | |||
| Total events per patient per year for glargine U100 | 1.79 | 0.86 | 0.09 |
| Degludec/glargine U100 hypoglycaemic event rate ratio [95% CI] | 0.80 [0.71; 0.89] p = 0.0001 | 0.76 [0.64; 0.89] p = 0.0011] | 0.49 [0.26; 0.94] p = 0.0306 |
| Calculated degludec hypoglycaemic event ratea | 1.43 | 0.65 | 0.05 |
aTotal events per patient-year × rate ratio
A rate ratio of 1.0 was used when the difference was not statistically significant
B/B basal–bolus therapy, BOT basal-only therapy, CI confidence interval, glargine U100 insulin glargine 100 units/mL, T1DM type 1 diabetes mellitus, T2DM type 2 diabetes mellitus
Treatment Costs
Cost of insulin was based on the Monthly Index of Medical Specialties (MIMS) [14] for April 2018, which includes the updated price of insulin glargine U100. The unit costs were multiplied by the number of units per day from Table 2. The number of needles and self-measured blood glucose (SMBG) tests were assumed to be the same in both arms (one needle and one SMBG test per injection).
Cost of Hypoglycaemia
The costs of nonsevere nocturnal, nonsevere diurnal and severe hypoglycaemic events were derived from two sources. The cost of a severe hypoglycaemic event (type 1 diabetes mellitus, £178; type 2 diabetes mellitus BOT, £427) was calculated based on a study specifically designed to evaluate the cost of severe hypoglycaemia across Germany, Spain and the UK [15]. The cost estimate from the UK (in pounds sterling or GBP) was derived by excluding the indirect costs and adjusting for inflation using the estimates from the Hospital & Community Health Services index [16]. The cost of a nonsevere hypoglycaemic event (daytime: type 1 diabetes mellitus, £2.44; type 2 diabetes mellitus BOT, £3.48; nocturnal: type 1 diabetes mellitus, £3.04; type 2 diabetes mellitus BOT, £5.56) was calculated based on a real-world study that investigated the frequency of self-reported nonsevere hypoglycaemic events across 11 European countries, including the UK (the Hypoglycaemia in Insulin-Treated Patients (HIT) study) [17].
Impact of Hypoglycaemia on QALYs
Quality-adjusted life-years (QALYs) were calculated by applying a disutility per hypoglycaemic event. A large-scale time trade-off (TTO) study was used to obtain the disutility incurred per hypoglycaemic event, and the following disutilities were obtained: 0.0054 and 0.0077 for nonsevere daytime and nonsevere nocturnal events, respectively, and 0.0623 for severe events based on preferences of the UK general population [18]. Severe events were not divided by the time of day at which they occurred. This was because there were no significant differences reported in the cost or utility for these events, so the impact of a severe hypoglycaemic episode was considered the same irrespective of the time at which it occurred. To estimate the incremental impact of degludec, the disutility per hypoglycaemic event was multiplied by the number of events observed in each treatment group and subtracted from a baseline level.
Outcomes
Results are presented as costs in GBP and a breakdown of the costs, effects in QALYs and incremental cost-effectiveness ratio (ICER) as cost per QALY. Two types of sensitivity analyses were conducted. The first was a one-way sensitivity analysis in which we analysed the effect of single changes in the most important parameters: hypoglycaemia rates, use of nonsignificant rate ratios, changes in hypoglycaemia cost parameters, SMBG tests per week for degludec, hypoglycaemic event disutility, insulin doses, needles and work loss arising from hypoglycaemia. The second was a probabilistic sensitivity analysis to capture the uncertainty of the results caused by statistical uncertainty with respect to the parameter inputs. Probabilistic sensitivity analysis allows the model parameters to be varied simultaneously, based on the parameters’ standard error distributions. The probabilistic sensitivity analysis was conducted using the uncertainties for all stochastic parameters in the models. Each probabilistic sensitivity analysis was run with 1000 iterations. Parameters, standard errors and distributions can be found in Table S1 of the Electronic supplementary material (ESM).
Results
Costs (and the cost breakdown for pharmacy and hypoglycaemic events), QALYs and the ICER for degludec vs. glargine U100 in type 1 and type 2 diabetes mellitus are shown in Table 4. Pharmacy costs were higher for degludec but were partly offset by hypoglycaemia costs in type 1 diabetes mellitus and type 2 diabetes mellitus. QALYs were in favour of degludec for type 1 diabetes mellitus (QALY gain degludec vs. glargine U100: 0.0232). In type 1 diabetes mellitus, the estimated ICER was small but positive (ICER = £984), meaning that patient health is improved in terms of QALYs at a low cost. QALYs were also in favour of degludec for type 2 diabetes mellitus (QALY gain: 0.0065). The ICER was £17,939, which falls just below the commonly accepted threshold for cost-effectiveness of £20,000/QALY [19].
Table 4.
Cost-effectiveness analysis of IDeg vs. IGlar U100 in type 1 and type 2 diabetes mellitus
| Type 1 diabetes mellitus | Degludec (£) | Glargine U100 (£) | Incremental cost (degludec – glargine U100) (£) |
|---|---|---|---|
| Pharmacy costs (total) | 1339 | 1265 | 73 |
| Insulina | 685 | 611 | 73 |
| Needlesb | 142 | 142 | 0 |
| SMBG testsc | 512 | 512 | 0 |
| Hypoglycaemic events (total) | 189 | 239 | − 51 |
| Nonsevere daytime events | 42 | 42 | 0 |
| Nonsevere nocturnal events | 8 | 10 | − 3 |
| Severe events | 139 | 187 | − 48 |
| Total costs | 1527 | 1505 | 23 |
| Effects | |||
| QALYs | 0.7741 | 0.7509 | 0.0232 |
| ICER (cost per QALY) | 984 | ||
| Type 2 diabetes mellitus | Degludec (£) | Glargine U100 (£) | Incremental cost (degludec – glargine U100) (£) |
|---|---|---|---|
| Pharmacy costs (total) | 1064 | 924 | 140 |
| Insulina | 900 | 760 | 140 |
| Needlesb | 35 | 35 | 0 |
| SMBG testsc | 128 | 128 | 0 |
| Hypoglycaemic events (total) | 28 | 51 | − 23 |
| Nonsevere daytime events | 5 | 6 | − 1 |
| Nonsevere nocturnal events | 4 | 5 | − 1 |
| Severe events | 20 | 40 | − 20 |
| Total costs | 1092 | 975 | 117 |
| Effects | |||
| QALYs | 0.8864 | 0.8798 | 0.0065 |
| ICER (cost per QALY) | 17,939 | ||
Numbers in the table are rounded to the nearest integer for costs and to four decimal places for QALYs
Glargine U100 insulin glargine 100 units/mL, ICER incremental cost-effectiveness ratio, QALYs quality-adjusted life-years, SMBG self-measured blood glucose
aIDeg (in FlexTouch® pen) £46.60 for 1500 units, resulting in cost/unit £0.031; Lantus® (in Solostar® pen) £37.77 for 1500 units, resulting in cost/unit £0.025; insulin aspart (in FlexPen®) £30.60 for 1500 units, resulting in cost/unit £0.020
bBD MicroFine® 5 mm: £9.69 per 100 needles, resulting in a needle price of £0.097
cSMBG test costs of £0.3507 based on the use of one Aviva test strip and one FastClix lancet per test
One-way sensitivity analyses showed that the results were robust to changes in parameters in both type 1 (Table S2 in the ESM) and type 2 diabetes mellitus (Table S3 in the ESM). All of the estimated ICER values were also below the normally accepted threshold of £20,000–£30,000/QALY, indicating that the results were robust to changes in assumptions and parameters. Probabilistic sensitivity analyses also show that degludec is cost-effective (Figs. S1 and S2 in the ESM). At a threshold value of £20,000/QALY, the probability that degludec will be cost-effective against glargine U100 is 99.8% for type 1 and 62.1% for type 2 diabetes mellitus.
Discussion
This short-term analysis leveraged results from two unique, double-blind, randomised, controlled, two-period crossover trials (SWITCH 1 [2] and SWITCH 2 [3]) to demonstrate the cost-effectiveness of degludec vs. glargine U100 in participants in the UK with type 1 or type 2 diabetes. To enhance the generalisability of the results, the SWITCH trial data were based on a more clinically relevant definition of hypoglycaemia (i.e. including only symptomatic blood-glucose confirmed events), and included participants who were more representative of those in regular clinical practice (i.e. with a history of hypoglycaemia) than those used in the series of randomised, parallel-group, open-label trials that comprised the BEGIN® clinical development programme for degludec. By including participants at higher risk of hypoglycaemia, we considered the sample to be more representative of participants in the UK. Despite the inclusion of these participants in the SWITCH trials, the rates were still somewhat lower than reported in real-world studies [20].
These results are consistent with an analysis that used hypoglycaemia rates from participants with type 2 diabetes mellitus from the BEGIN® clinical development programme for degludec. Analyses using data from BEGIN® suggested an ICER between £13,078 and £15,795 [21]. A re-analysis of the cost-effectiveness of degludec vs. glargine U100 suggested even lower ICERs [22]. However, changes in the prices of degludec and glargine U100 make comparisons with previous analyses difficult.
These findings are also consistent with evidence from observational studies in type 1 diabetes mellitus. For example, one retrospective single-centre case series of 35 consecutive participants with type 1 diabetes mellitus in real-world practice in the UK concluded that degludec was highly cost-effective for participants who switched from either glargine U100 or insulin detemir [23]. Degludec was dominant against glargine U100/insulin detemir; even when benefits beyond hypoglycaemia reduction were excluded, the predicted cost per QALY of switching to degludec was £10,754 projected over a lifetime. Those results should be considered conservative, as the cost of degludec in the UK has recently been lowered. Analysis of data from a larger observational study of 476 consecutive participants with type 1 diabetes mellitus in Sweden also concluded that degludec was dominant compared with glargine U100 [24].
Currently marketed basal insulins in the UK include the basal insulin analogues studied here (degludec and glargine U100) as well as neutral protamine Hagedorn insulin (NPH). In the UK, the most widely prescribed basal insulin is glargine U100. Furthermore, for health economic analysis, the next best alternative is usually considered the appropriate comparator [25]. Compared with NPH, in type 1 diabetes mellitus, basal insulin analogues have been shown to provide small but statistically significant improvements in HbA1c and clinically important reductions in nocturnal and symptomatic hypoglycaemia [26]. The reduced risk of nocturnal hypoglycaemia with an all-analogue basal–bolus regimen compared with a human insulin basal–bolus regimen has been demonstrated in people with type 1 diabetes mellitus prone to recurrent severe hypoglycaemia [27]. In type 2 diabetes mellitus, basal insulin analogues are also associated with a significantly reduced risk of nocturnal and symptomatic hypoglycaemia [28]. In addition, the SWITCH trials did not include any direct comparison vs. NPH, and indirect comparisons were out of the scope of this analysis. There are also no other published data that directly compare degludec and NPH. However, a systematic review of 15 modelling studies found that another basal insulin analogue, insulin detemir, was cost-effective vs. NPH and at least as cost-effective as glargine U100 in both type 1 and type 2 diabetes mellitus [29]. Data from the UK have also shown that insulin detemir was cost-effective vs. NPH in type 1 diabetes mellitus [30, 31].
This study is limited (as are all model-based evaluations) by the need to estimate input parameters. Some of our cost estimates were derived from multiple sources and national settings, and therefore may not reflect the true health economic impact in the UK. In contrast, the use of data from actual trial results for insulin doses and hypoglycaemia rates is a strength of the study. Furthermore, the sensitivity analysis demonstrated that the results were robust, and using rates of hypoglycaemia from other published sources leads to even more improved cost-effectiveness results. A new, more concentrated formulation of insulin glargine, 300 units/mL (IGlar U300), has recently been introduced; however, a cost-effectiveness analysis of IGlar U300 vs. degludec using head-to-head data will not be possible until clinical trials are conducted. Finally, although an association between hypoglycemic events and subsequent cardiovascular outcomes and mortality was demonstrated previously, a causal link is yet to be established beyond doubt, so we were unable to include it in a cost-effectiveness analysis [32–36].
Conclusion
Analysis of data from a pair of rigorously designed randomised controlled trials in both type 1 (SWITCH 1) and type 2 (SWITCH 2) diabetes mellitus indicates that degludec is a cost-effective treatment option vs. glargine U100 in participants with type 1 diabetes mellitus using basal–bolus therapy and in participants with type 2 diabetes mellitus using basal-only therapy in the UK. The balance of internal and external validity achieved with the SWITCH trials in terms of trial design and population inclusion adds important information to the value discussion.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Firstly, we wish to thank the patients who participated in the SWITCH 1 and SWITCH 2 trials.
Funding
This manuscript and article processing charges were supported by Novo Nordisk, Søborg, Denmark.
Role of Funding Source
Novo Nordisk contributed to the study design, statistical analyses, data interpretation, manuscript preparation and the decision to submit this manuscript for publication. All of the authors had access to the study data and take full responsibility for the content of the manuscript and the decision to submit it for publication.
Medical Writing, Editorial, and Other Assistance
Medical writing and submission support were provided by Gary Patronek and Beverly La Ferla of Watermeadow Medical, an Ashfield company, part of UDG Healthcare plc, funded by Novo Nordisk. We also thank Deniz Tutkunkardas (Novo Nordisk) for his review and input to the manuscript.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Individual contributions were as follows: study concept and design: Barrie Chubb, Jens Gundgaard; acquisition, analysis or interpretation of data: Marc Evans, Roopa Mehta, Jens Gundgaard, Barrie Chubb; health economic analysis: Barrie Chubb, Jens Gundgaard; writing and review of manuscript: Marc Evans, Roopa Mehta, Jens Gundgaard, Barrie Chubb.
Disclosures
Marc Evans has received honoraria and research awards from Novo Nordisk, Sanofi-Aventis, MSD and Novartis. Roopa Mehta has received honoraria from Novo Nordisk, Boehringer Ingelheim, Amgen, AstraZeneca, Janssen, MSD, Novartis, Stendahl and Abbott. Jens Gundgaard is an employee of Novo Nordisk and also holds stock in Novo Nordisk. Barrie Chubb is also an employee of Novo Nordisk and also holds stock in Novo Nordisk.
Compliance with Ethics Guidelines
The SWITCH trials [2, 3] were conducted in accordance with the 1964 Helsinki Declaration and its later amendments and ICH Good Clinical Practice. Prior to trial initiation, the protocol, consent form, and patient information sheet were reviewed and approved by appropriate health authorities and an independent ethics committee/institutional review board. All patients provided signed informed consent.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Footnotes
Enhanced Digital Features
To view enhanced digital features for this article go to 10.6084/m9.figshare.6871481.
References
- 1.Levin P. The cost-effectiveness of insulin glargine vs. neutral protamine Hagedorn insulin in type 2 diabetes: a focus on health economics. Diabetes Obes Metab. 2008;10(Suppl. 2):66–75. doi: 10.1111/j.1463-1326.2008.00845.x. [DOI] [PubMed] [Google Scholar]
- 2.Lane Wendy, Bailey Timothy S., Gerety Gregg, Gumprecht Janusz, Philis-Tsimikas Athena, Hansen Charlotte Thim, Nielsen Thor S. S., Warren Mark. Effect of Insulin Degludec vs Insulin Glargine U100 on Hypoglycemia in Patients With Type 1 Diabetes. JAMA. 2017;318(1):33. doi: 10.1001/jama.2017.7115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wysham Carol, Bhargava Anuj, Chaykin Louis, de la Rosa Raymond, Handelsman Yehuda, Troelsen Lone N., Kvist Kajsa, Norwood Paul. Effect of Insulin Degludec vs Insulin Glargine U100 on Hypoglycemia in Patients With Type 2 Diabetes. JAMA. 2017;318(1):45. doi: 10.1001/jama.2017.7117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heise T, Nosek L, Bottcher SG, Hastrup H, Haahr H. Ultra-long-acting insulin degludec has a flat and stable glucose-lowering effect in type 2 diabetes. Diabetes Obes Metab. 2012;14:944–950. doi: 10.1111/j.1463-1326.2012.01638.x. [DOI] [PubMed] [Google Scholar]
- 5.Heise Tim, Korsatko Stefan, Nosek Leszek, Coester Hans Veit, Deller Sigrid, Roepstorff Carsten, Segel Stine, Kapur Rahul, Haahr Hanne, Hompesch Marcus. Steady state is reached within 2-3 days of once-daily administration of degludec, a basal insulin with an ultralong duration of action. Journal of Diabetes. 2015;8(1):132–138. doi: 10.1111/1753-0407.12266. [DOI] [PubMed] [Google Scholar]
- 6.Heise T, Hermanski L, Nosek L, Feldman A, Rasmussen S, Haahr H. Insulin degludec: four times lower pharmacodynamic variability than insulin glargine under steady-state conditions in type 1 diabetes. Diabetes Obes Metab. 2012;14:859–864. doi: 10.1111/j.1463-1326.2012.01627.x. [DOI] [PubMed] [Google Scholar]
- 7.Ratner R, Gough SC, Mathieu C, Del Prato S, Bode B, Mersebach H, et al. Hypoglycaemia risk with insulin degludec compared with insulin glargine in type 2 and type 1 diabetes: a pre-planned meta-analysis of phase 3 trials. Diabetes Obes Metab. 2013;15:175–184. doi: 10.1111/dom.12032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farmer AJ, Brockbank KJ, Keech ML, England EJ, Deakin CD. Incidence and costs of severe hypoglycaemia requiring attendance by the emergency medical services in South Central England. Diabet Med. 2012;29:1447–1450. doi: 10.1111/j.1464-5491.2012.03657.x. [DOI] [PubMed] [Google Scholar]
- 9.Harris SB, Khunti K, Landin-Olsson M, Galbo-Jørgensen CB, Bøgelund M, Chubb B, et al. Descriptions of health states associated with increasing severity and frequency of hypoglycemia: a patient-level perspective. Patient Prefer Adherence. 2013;7:925–936. doi: 10.2147/PPA.S46805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heller SR, Frier BM, Hersløv ML, Gundgaard J, Gough SC. Severe hypoglycaemia in adults with insulin-treated diabetes: impact on healthcare resources. Diabet Med. 2016;33:471–477. doi: 10.1111/dme.12844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Willis WD, Diago-Cabezudo JI, Madec-Hily A, Aslam A. Medical resource use, disturbance of daily life and burden of hypoglycemia in insulin-treated patients with diabetes: results from a European online survey. Expert Rev Pharmacoecon Outcomes Res. 2013;13:123–130. doi: 10.1586/erp.12.80. [DOI] [PubMed] [Google Scholar]
- 12.Evans M, Wolden M, Gundgaard J, Chubb B, Christensen T. Cost-effectiveness of insulin degludec compared with insulin glargine in a basal-bolus regimen in patients with type 1 diabetes mellitus in the UK. J Med Econ. 2015;18:56–68. doi: 10.3111/13696998.2014.971160. [DOI] [PubMed] [Google Scholar]
- 13.Seaquist ER, Anderson J, Childs B, Cryer P, Dagogo-Jack S, Fish L, et al. Hypoglycaemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care. 2013;36:1384–1395. doi: 10.2337/dc12-2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haymarket Media Group. MIMS (Monthly Index of Medical Specialties). Available at www.mims.co.uk. Last accessed 28 June 2018.
- 15.Hammer M, Lammert M, Mejías SM, Kern W, Frier BM. Costs of managing severe hypoglycaemia in three European countries. J Med Econ. 2009;12:281–290. doi: 10.3111/13696990903336597. [DOI] [PubMed] [Google Scholar]
- 16.HCHS: The Hospital & Community Health Services (HCHS) index. Available at https://kar.kent.ac.uk/65559/40/65559_rep_UCR-2017-v13finalKAR.pdf. Last accessed 16 April 2018.
- 17.Chubb B, Tikkanen C. The Cost of Non-Severe Hypoglycaemia In Europe. Value in Health. 2015;18(7):A611. doi: 10.1016/j.jval.2015.09.2118. [DOI] [Google Scholar]
- 18.Evans M, Khunti K, Mamdani M, Galbo-Jørgensen CB, Gundgaard J, Bøgelund M, et al. Health-related quality of life associated with daytime and nocturnal hypoglycaemic events: a time trade-off survey in five countries. Health Qual Life Outcomes. 2013;11:90. doi: 10.1186/1477-7525-11-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adalsteinsson Erpur, Toumi Mondher. Benefits of probabilistic sensitivity analysis – a review of NICE decisions. Journal of Market Access & Health Policy. 2013;1(1):21240. doi: 10.3402/jmahp.v1i0.21240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elliott Lisa, Fidler Carrie, Ditchfield Andrea, Stissing Trine. Hypoglycemia Event Rates: A Comparison Between Real-World Data and Randomized Controlled Trial Populations in Insulin-Treated Diabetes. Diabetes Therapy. 2016;7(1):45–60. doi: 10.1007/s13300-016-0157-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Evans M, Wolden M, Gundgaard J, Chubb B, Christensen T. Cost-effectiveness of insulin degludec compared with insulin glargine for patients with type 2 diabetes treated with basal insulin—from the UK health care cost perspective. Diabetes Obes Metab. 2014;16:366–375. doi: 10.1111/dom.12250. [DOI] [PubMed] [Google Scholar]
- 22.Evans Marc, Chubb Barrie, Gundgaard Jens. Cost-effectiveness of Insulin Degludec Versus Insulin Glargine in Adults with Type 1 and Type 2 Diabetes Mellitus. Diabetes Therapy. 2017;8(2):275–291. doi: 10.1007/s13300-017-0236-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Evans Marc, McEwan Phil, Foos Volker. Insulin degludec early clinical experience: does the promise from the clinical trials translate into clinical practice—a case-based evaluation. Journal of Medical Economics. 2014;18(2):96–105. doi: 10.3111/13696998.2014.975234. [DOI] [PubMed] [Google Scholar]
- 24.Landstedt-Hallin L, Gundgaard J, Ericsson Å, Ellfors-Zetterlund S. Cost-effectiveness of switching to insulin degludec from other basal insulins: evidence from Swedish real-world data. Curr Med Res Opin. 2017;33:647–655. doi: 10.1080/03007995.2016.1277194. [DOI] [PubMed] [Google Scholar]
- 25.Karlsson G, Johannesson M. The decision rules of cost-effectiveness analysis. Pharmacoeconomics. 1996;9:113–120. doi: 10.2165/00019053-199609020-00003. [DOI] [PubMed] [Google Scholar]
- 26.Monami M, Marchionni N, Mannucci E. Long-acting insulin analogues vs. NPH human insulin in type 1 diabetes. A meta-analysis. Diabetes Obes Metab. 2009;11:372–378. doi: 10.1111/j.1463-1326.2008.00976.x. [DOI] [PubMed] [Google Scholar]
- 27.Kristensen P. L., Tarnow L., Bay C., Nørgaard K., Jensen T., Parving H.-H., Perrild H., Beck-Nielsen H., Christiansen J. S., Thorsteinsson B., Pedersen-Bjergaard U. Comparing effects of insulin analogues and human insulin on nocturnal glycaemia in hypoglycaemia-prone people with Type 1 diabetes. Diabetic Medicine. 2017;34(5):625–631. doi: 10.1111/dme.13317. [DOI] [PubMed] [Google Scholar]
- 28.Monami M, Marchionni N, Mannucci E. Long-acting insulin analogues versus NPH human insulin in type 2 diabetes: a meta-analysis. Diabetes Res Clin Pract. 2008;81:184–189. doi: 10.1016/j.diabres.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 29.Suh DC, Aagren M. Cost-effectiveness of insulin detemir: a systematic review. Expert Rev Pharmacoecon Outcomes Res. 2011;11:641–655. doi: 10.1586/erp.11.73. [DOI] [PubMed] [Google Scholar]
- 30.Palmer AJ, Roze S, Valentine WJ, Smith I, Wittrup-Jensen KU. Cost-effectiveness of detemir-based basal/bolus therapy versus NPH-based basal/bolus therapy for type 1 diabetes in a UK setting: an economic analysis based on meta-analysis results of four clinical trials. Curr Med Res Opin. 2004;20:1729–1746. doi: 10.1185/030079904X5661. [DOI] [PubMed] [Google Scholar]
- 31.Palmer AJ, Valentine WJ, Ray JA, Foos V, Lurati F, Smith I, et al. An economic assessment of analogue basal-bolus insulin versus human basal-bolus insulin in subjects with type 1 diabetes in the UK. Curr Med Res Opin. 2007;23:895–901. doi: 10.1185/030079907X182194. [DOI] [PubMed] [Google Scholar]
- 32.Johnston SS, Conner C, Aagren M, Smith DM, Bouchard J, Brett J. Evidence linking hypoglycemic events to an increased risk of acute cardiovascular events in patients with type 2 diabetes. Diabetes Care. 2011;34:1164–1170. doi: 10.2337/dc10-1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khunti K, Davies M, Majeed A, Thorsted BL, Wolden ML, Paul SK. Hypoglycemia and risk of cardiovascular disease and all-cause mortality in insulin-treated people with type 1 and type 2 diabetes: a cohort study. Diabetes Care. 2015;38(2):316–322. doi: 10.2337/dc14-0920. [DOI] [PubMed] [Google Scholar]
- 34.Lung TW, Petrie D, Herman WH, Palmer AJ, Svensson AM, Eliasson B, Clarke PM. Severe hypoglycemia and mortality after cardiovascular events for type 1 diabetic patients in Sweden. Diabetes Care. 2014;37:2974–2981. doi: 10.2337/dc14-0405. [DOI] [PubMed] [Google Scholar]
- 35.Paty B. The role of hypoglycemia in cardiovascular outcomes in diabetes. Can J Diabetes. 2015;39(Suppl. 5):S155–S159. doi: 10.1016/j.jcjd.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 36.Snell-Bergeon JK, Wadwa RP. Hypoglycemia, diabetes, and cardiovascular disease. Diabetes Technol Ther. 2012;14(Suppl. 1):S51–S58. doi: 10.1089/dia.2012.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.