Abstract
Onychomycosis is the most frequent nail disease, with an estimated prevalence of 2–8%. Current treatment strategies include the use of oral and topical antifungals, despite low cure rates following these treatments. The objectives of this study were to assess the therapeutic response of patients with onychomycosis to 1,064-nm Nd:YAG laser treatment, the clinical evaluation method available for this therapy, and the possible side effects of this treatment. Twenty patients with onychomycosis underwent laser therapy. A total of 34 nails with onychomycosis were assessed according to the Onychomycosis Severity Index (OSI). This index generates scores that classify onychomycosis as mild, moderate, or severe. The OSI was determined before treatment and after a mean follow-up period of 8 months. The comparison between the initial and the final OSI for all 34 nails treated with laser therapy showed a significant difference; however, a low association was shown between these variables. A general reduction in the area of involvement and in the OSI numerical scores was observed. These data show a trend toward improvement in onychomycosis treated with 1,064-nm Nd:YAG laser. The OSI allowed an adequate clinical assessment of the response to laser therapy. Laser treatment did not cause marked discomfort in most patients, indicating that laser is a well-tolerated procedure.
Keywords: Onychomycosis; 1,064-nm Nd:YAG laser; Onychomycosis Severity Index
Introduction
Onychomycosis is the most frequent nail disease, representing more than 50% of all onychopathies. The prevalence of onychomycosis in the general population ranges from 2 to 8% [1]. Previously, onychomycosis was regarded as an essentially aesthetic problem; currently, however, it is considered a debilitating disease [2].
The absence of fungi in mycological investigations does not reflect the absence of disease, as direct microscopy has low sensitivity and fungal culture has a high percentage of false-negative results (30–50%) [3, 4]. Therefore, algorithms are being developed for the clinical diagnosis of onychomycosis [5].
Treatments with antifungals may not be successful due to several factors, including the time required to apply topical medications, the side effects of systemic drugs, and the failure to apply medication in sufficient concentrations to the target area. Even with adequate systemic or topical therapy, persistence of fungal infections in not uncommon [6].
Recently, therapies with different mechanisms of action, such as laser and photodynamic therapy, have been considered because they may have higher efficacy in comparison with currently used therapies [7]. Laser therapy is an emergent area in the treatment of onychomycosis. In recent years, laser device options have been expanding rapidly. A widely used category is the 1,064-nm neodymium:yttrium-aluminium-garnet (Nd:YAG) laser [8].
Laser Action Mechanism in Onychomycosis
According to Hochman [9], the Nd:YAG laser emits 1,064-nm wavelength energy that may cross the nail plate and overheat fungal material, leading to fungal cellular damage and death.
Some studies have assessed the in vitro growth inhibition of Trichophyton rubrum using 1,064- and 532-nm Nd:YAG lasers [6, 10]. In addition to thermal damage, the results obtained were probably due to the presence of xanthomegnin – a red pigment produced by T. rubrum – that acts as a chromophore at 532-nm, and melanin, found in the cell walls of Trichophyton species, which is a chromophore at the 1,064-nm wavelength [6, 11].
Clinical Studies Using the Nd:YAG Laser for Onychomycosis Treatment
In vivo studies, such as the one conducted by Kozarev and Vižintin [12], have shown improvement and even cure of onychomycosis following laser therapy. These authors treated 72 patients (194 nails with onychomycosis) with 1,064-nm Nd:YAG laser (Dualis SP; Fotona, Slovenia). Laser treatment was performed in 4 sessions with a 1-week interval between sessions. A fluence of 35–40 J/cm2 was applied with a 4-mm diameter spot size, pulse duration of 35 ms, and repetition rate of 1 Hz. The mean temperature reached was 45 ± 5°C. Three months after treatment, 95.8% of patients had been cured.
Zawar et al. [13] used the Q-switched Nd-YAG laser to treat a patient with severe onychomycosis recalcitrant to treatment with itraconazole and amorolfine nail lacquer. Laser therapy included 3 sessions with an interval of 2 weeks, fluence of 500 mJ, and a 1.5-mm spot size. Clinical and mycological improvements were attained.
The objectives of this study were to assess the response to 1,064-nm Nd:YAG laser therapy, the clinical evaluation methods available for this therapy, and the possible side effects of its use.
Materials and Methods
Study Design, Setting, and Patients
This was a case study of onychomycosis patients treated with 1,064-nm Nd:YAG laser. The patients, diagnosed and treated, were selected from a private Dermatology Clinic located in Vitória, Espírito Santo, Brazil. The study was approved by the Research Ethics Committee of the Health Sciences Centre of the Federal University of Espírito Santo (Universidade Federal do Espírito Santo – UFES).
The inclusion criteria were patients with at least 2 nail abnormalities compatible with a clinical diagnosis of onychomycosis; patients who did not use systemic or topical antifungal drugs in the previous 6 months; and patients of both genders, older than 18 years, who signed the informed consent form. Patients who did not undergo at least 5 laser therapy sessions, who did not return for follow-up after laser therapy, or who did not agree to provide information about the laser treatment were excluded from the study.
To perform the clinical assessment of nails diagnosed with onychomycosis, the Onychomycosis Severity Index (OSI) – a classification system that grades the severity of distal subungual onychomycosis developed by Carney et al. [14] – was used. The clinical characteristics used to define OSI are the area of involvement, the proximity of disease to the nail matrix, the occurrence of dermatophytoma, and the presence of severe subungual hyperkeratosis (> 2 mm).
Mild onychomycosis is classified by a score from 1 to 5; moderate from 6 to 15; and severe from 16 to 35. Clinical cure scores 0 points. Table 1 shows the OSI score calculation.
Table 1.
Onychomycosis Severity Index (OSI)
| Area of involvement |
Proximity of disease to matrix |
Presence of dermatophytoma or subungual hyperkeratosis >2 mm |
|||
|---|---|---|---|---|---|
| affected nail, % | points | amount of involvement from distal edge | points | present | points |
| 0 | 0 | <1/4 | 1 | no | 0 |
| 1–10 | 1 | 1/4–1/2 | 2 | yes | 10 |
| 11–25 | 2 | >1/2–3/4 | 3 | ||
| 26–50 | 3 | >3/4 | 4 | ||
| 51–75 | 4 | matrix involvement | 5 | ||
| 76–100 | 5 | ||||
Source: Carney et al. [14].
A specific protocol was used for this study, and onychomycosis clinical data were collected for each patient. Mycological tests (direct microscopy and culture) were performed only before the start of the treatment. Clinical cure of onychomycosis was assessed in accordance with the scores described by Carney et al. [14]. Photographs were taken before and after laser therapy to record any changes. Another protocol regarding side effects – the appearance of bruises and other skin and ungual lesions as well as discomfort (pain/burning/stinging) during the procedure – was used. The level of discomfort was measured using a scale from 0 to 10 (0 – no discomfort, 1 to 3 – mild discomfort, 4 to 6 – moderate discomfort, 7 to 9 – intense discomfort, 10 – unbearable discomfort).
Intervention
Long-pulsed 1,064-nm Nd:YAG laser (Synchro; Deka, Calenzano, Florence, Italy) was applied using a 7-mm diameter spot size; fluence of 20 J/cm2 for fingernails, 40 J/cm2 for the big toe nail, and 50 J/cm2 for thicker big toe nails; pulse duration of 10 ms; and repetition rate of 2 Hz. Treatment was composed of 4 pulses for fingernails and 6 pulses for big toe nails, covering the entire nail plate. Five applications were performed, 1 min apart from each other. The mean temperature reached was 40°C, as assessed by an infrared digital thermometer. No topical anesthetic was applied before treatment. Five sessions of laser therapy were performed, 1–2 weeks apart. One patient underwent 8 sessions because of a dermatophytoma.
Evaluation
Clinical and photographic assessments were performed to determine the OSI scores before treatment and after a post-treatment follow-up period of 5–12 months (mean: 8 months).
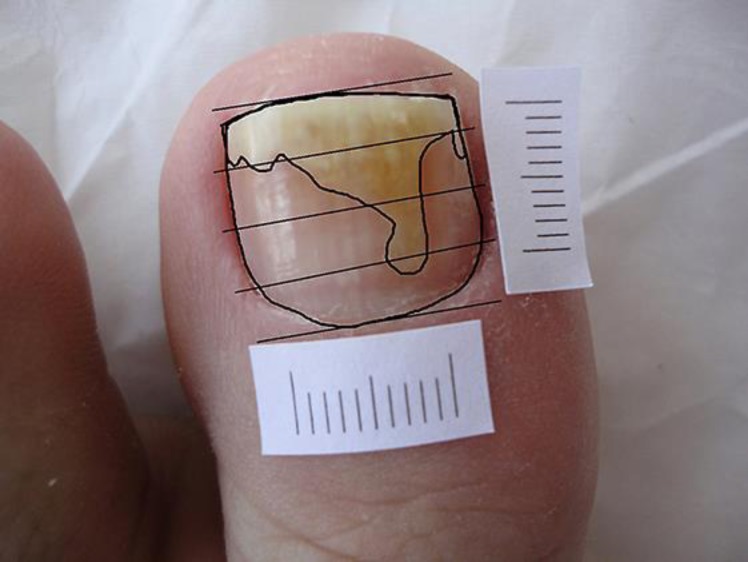
The area of involvement of the infected nails was quantified by the ratio between the surface area of involvement and the total surface area, using the image analysis software Image J, version 1.47 (NIH, Bethesda, MD, USA). The same software was used to divide the nails into 4 cross-sections (Fig. 1).
Fig. 1.
Software demonstration: image of area of involvement versus total area, and the nail divided into 4 cross-sections.
Statistical Analysis
Statistical analysis was performed using IBM SPSS version 22 (IBM Corp., Armonk, NY, USA). Due to the objective of the study, a relationship or association was assumed between the variables OSI grade, area of involvement, and OSI score before and after laser therapy. To test this hypothesis, the interaction between the variables was analyzed using statistical tests, such as the χ2 test (for the qualitative variable OSI) and Student's t test (for the quantitative variables area of involvement and OSI scores). The significance level adopted was 5%.
Results
A total of 24 patients started laser therapy. One patient underwent only 2 sessions and did not return to continue therapy, claiming improvement; 3 patients underwent 5 laser therapy sessions but did not return for follow-up (1 had an acute myocardial infarction, and 2 did not provide a reason). Of the 24 patients, 20 completed the follow-up and were included in the study (14 women and 6 men). The mean patient age was 50.25 years (ranging from 23 to 72 years). A total of 34 nails (32 big toe nails and 2 thumb nails) with a clinical diagnosis of onychomycosis were assessed for response to laser therapy.
Mycological tests were performed for 32 of the 34 evaluated nails. Direct microscopy revealed dermatophytes in 13 nails (40.6%), yeasts in 7 nails (21.9%), and non-dermatophyte fungus in 1 nail (3.1%), but revealed no fungi in 11 nails (34.4%). The culture was positive for Candida species in 7 samples (21.9%), Trichophyton species in 5 samples (15.6%), and Fusarium species in 1 sample (3.1%), but was negative in 19 samples (59.4%).
All 34 nails analyzed were classified as distal and lateral subungual onychomycosis. Five to 12 months after laser treatment, the patients returned for a final clinical and photographic nail assessment.
Regarding local side effects, patients reported a local sensation of heat, needle pricking, and pain, which would immediately disappear when the laser application ended. The frequency of discomfort level sensed by patients during treatment was as follows: absent (0), mild (3/15%), moderate (15/75%), intense (2/10%), and unbearable (0). No other local or systemic side effects were observed during the laser treatment sessions or during follow-up.
Analysis of Initial and Final OSI
Before the beginning of therapy, the nails were classified according to the OSI as presenting mild, moderate, or severe onychomycosis. After follow-up, these nails were reclassified as mild, moderate, severe, no involvement, or cured. Of the 34 nails treated, 3 nails classified as mild and 1 nail classified as moderate disease progressed to clinical cure. In the remaining nails, decreased, unchanged, and increased OSI grades were observed (Table 2).
Table 2.
Changes in Onychomycosis Severity Index (OSI) for the 34 nails treated with laser therapy
| Final OSI |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| none or cure (0 points) |
mild (1–5 points) |
moderate (6–15 points) |
severe (16–35 points) |
Total |
||||||
| freq. | % | freq. | % | freq. | % | freq. | % | freq. | % | |
| Initial OSI | ||||||||||
| Mild (1–5 points) | 3a | 75.0a | 1b | 16.7b | 3c | 15.8c | 0 | 0.0 | 7 | 20.6 |
| Moderate (6–15 points) | 1a | 25.0a | 5a | 83.3a | 11b | 57.9b | 0 | 0.0 | 17 | 50.0 |
| Severe (16–35 points) | 0 | 0.0 | 0 | 0.0 | 5a | 26.3a | 5b | 100.0b | 10 | 29.4 |
| Total | 4 | 100.0 | 6 | 100.0 | 19 | 100.0 | 5 | 100.0 | 34 | 100.0 |
Cases with a decrease in OSI grade.
Cases with no change in OSI grade.
Cases with an increase in OSI grade.
By analyzing the data from Table 2, we obtained the following final result: 14 nails showed relative improvement in onychomycosis with OSI grade reduction; 17 nails were unchanged and maintained the same OSI grade after laser therapy; and 3 nails showed clinical worsening with an increase in OSI grade.
A χ2 test was performed using a significance level α = 5%. The result obtained (p = 0.004) denotes dependence between the initial OSI and the final OSI, indicating a significant relationship. However, the low association scores obtained (Phi, Pearson's C, and Cramer's V: p = 0.004) indicate a weak association between these variables. This weak association may be due to the small sample size, which directly affects χ2 test results.
Analysis of Initial and Final Areas of Involvement
The “initial area of involvement” was determined for all treated nails before treatment began. The mean initial area of involvement was 36.48% with a standard deviation of 24.07%. The mean “final area of involvement” was calculated after follow-up as 27.84% with a standard deviation of 20.99%. To test whether a significant difference existed between the initial and final mean areas, the correlation between samples (0.668) was assessed, indicating an association between the values obtained at the two assessment times. Thus, Student's t test for paired samples was used, which showed a significant difference between the analyzed means (p = 0.010). Overall, a reduction in the area of involvement following laser therapy was observed.
Analysis of Initial and Final Scores
The OSI scores were also determined before therapy started (“initial score”: mean = 11.47, standard deviation = 8.45) and after follow-up (“final score”: mean = 8.53, standard deviation = 7.41). The correlation between paired samples was assessed. The value obtained (0.770) indicated the existence of a significant correlation, with a high association between scores. Student's t test for paired samples was then performed and showed a significant difference between the analyzed means (p = 0.004). Thus, in general, a reduction in OSI score was observed following onychomycosis treatment.
Next, we present data and photographs of 1 patient with onychomycosis before laser therapy and after follow-up (Fig. 2 and 3, respectively). The OSI grades (mild and moderate) are shown. The area of involvement (in %) and the OSI score are also shown.
Fig. 2.
Patient 13 (left hallux) before laser therapy. Initial OSI: moderate; initial area: 41.44%; initial score: 15.
Fig. 3.
Patient 13 (left hallux) after laser therapy (8-month follow-up period). Final OSI: mild; final area: 8.87%; final score: 1.
Discussion
This study concerns 20 patients diagnosed as having onychomycosis who were treated with 1,064-nm Nd:YAG laser. The mycological tests were performed before the treatment in 32 of the 34 nails evaluated. Negative results were found in 34% of the direct microscopies and in 59% of the cultures. Although clinical diagnosis should be supported by a positive mycological test, the absence of a proof is not a proof of absence. With regard to definitions of cure in clinical trials, in the complete absence of clinical signs of onychomycosis, mycological tests are not required [15].
A comparison between the initial and final OSI performed for all 34 nails treated with laser therapy showed an OSI grade decrease in 14 nails, no change in 17 nails, and an increase in 3 nails. The variables initial and final OSI were found to be dependent, which signifies that their relationship is significant (p = 0.04). However, when measuring the association between these variables, the test values indicated a weak association. Regarding this aspect, the therapeutic response to laser therapy was not satisfactory.
Analysis of the area of involvement before therapy and after follow-up showed a significant difference between these values (p = 0.010). A reduction in the area of involvement after laser therapy was observed. The comparison of the OSI numerical scores before therapy and after follow-up also showed a significant difference between these scores (p = 0.004). A reduction in the OSI score was observed following onychomycosis treatment. Therefore, the reduction in the area of involvement and OSI score indicate a trend toward onychomycosis improvement following treatment with laser therapy. The number of patients assessed was low, which probably negatively affected the capacity to obtain a definitive conclusion about this treatment.
The importance of using the OSI warrants emphasis, which measures not only area of involvement but also localization of infection, that is, how close the area of involvement is to the nail matrix. Thus, the OSI provides an objective clinical analysis of onychomycosis instead of the traditional assessment based on subjective criteria. This index may be applied only to distal and lateral onychomycosis; however, because these are the most common forms of onychomycosis, the OSI is a highly useful index. The OSI was found to be a satisfactory analytic method to assess response to laser therapy.
The present study evaluated the clinical response to nail laser therapy, and it was not possible to make an inference regarding the fungal species that responded to treatment, due to the small sample size.
Regarding side effects following Nd:YAG laser therapy, the patients reported local effects: heat sensation, needle pricking sensation, and pain. These side effects generated a moderate discomfort level in 75% of the patients. However, the discomfort was tolerable and did not interfere with treatment continuity, and therefore, the interruption of laser therapy was not necessary.
Importantly, the mean follow-up period after treatment varied greatly (from 5 to 12 months). The loss of 4 patients (16.6%) might have affected the final study results.
To determine the therapeutic efficacy of 1,064-nm Nd:YAG laser for the treatment of nail fungal infections, clinical studies with larger sample sizes are necessary. Identification of fungal species and the use of standard criteria for clinical nail assessment, such as the OSI, would be important to correctly interpret results following therapy. Additionally, current treatment protocols vary widely. Therefore, the definition of optimal parameters (fluence, pulse duration, number of treatment sessions) for laser therapy is imperative.
In parallel, research aimed at understanding the exact mechanism of action of laser on fungi, focused on identifying target chromophores and optimal wavelengths, is also needed.
Statement of Ethics
The patients signed an informed consent form approved by the Research Ethics Committee of the Health Sciences Centre of the Federal University of Espírito Santo (UFES) under the reference number 282.875.
Disclosure Statement
There is no conflict of interest of any of the authors with the results of this study.
References
- 1.Effendy I, Lecha M, Feuilhade de Chauvin M, Di Chiacchio N, Baran R, European Onychomycosis Observatory Epidemiology and clinical classification of onychomycosis. J Eur Acad Dermatol Venereol. 2005 Sep;19((s1 Suppl 1)):8–12. doi: 10.1111/j.1468-3083.2005.01281.x. [DOI] [PubMed] [Google Scholar]
- 2.Lecha M, Effendy I, Feuilhade de Chauvin M, Di Chiacchio N, Baran R, Taskforce on Onychomycosis Education Treatment options—development of consensus guidelines. J Eur Acad Dermatol Venereol. 2005 Sep;19((s1 Suppl 1)):25–33. doi: 10.1111/j.1468-3083.2005.01284.x. [DOI] [PubMed] [Google Scholar]
- 3.Bao F, Fan Y, Sun L, Yu Y, Wang Z, Pan Q, et al. Comparison of fungal fluorescent staining and ITS rDNA PCR-based sequencing with conventional methods for the diagnosis of onychomycosis. J Eur Acad Dermatol Venereol. 2018 Jun;32((6)):1017–21. doi: 10.1111/jdv.14843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gräser Y, Czaika V, Ohst T. Diagnostic PCR of dermatophytes—an overview. J Dtsch Dermatol Ges. 2012 Oct;10((10)):721–6. doi: 10.1111/j.1610-0387.2012.07964.x. [DOI] [PubMed] [Google Scholar]
- 5.Fletcher CL, Hay RJ, Smeeton NC. Onychomycosis: the development of a clinical diagnostic aid for toenail disease. Part I. Establishing discriminating historical and clinical features. Br J Dermatol. 2004 Apr;150((4)):701–5. doi: 10.1111/j.0007-0963.2004.05871.x. [DOI] [PubMed] [Google Scholar]
- 6.Vural E, Winfield HL, Shingleton AW, Horn TD, Shafirstein G. The effects of laser irradiation on Trichophyton rubrum growth. Lasers Med Sci. 2008 Oct;23((4)):349–53. doi: 10.1007/s10103-007-0492-4. [DOI] [PubMed] [Google Scholar]
- 7.Gupta AK, Uro M, Cooper EA. Onychomycosis therapy: past, present, future. J Drugs Dermatol. 2010 Sep;9((9)):1109–13. [PubMed] [Google Scholar]
- 8.Gupta AK, Simpson FC. Laser therapy for onychomycosis. J Cutan Med Surg. 2013 Sep-Oct;17((5)):301–7. doi: 10.2310/7750.2012.12060. [DOI] [PubMed] [Google Scholar]
- 9.Hochman LG. Laser treatment of onychomycosis using a novel 0.65-millisecond pulsed Nd:YAG 1064-nm laser. J Cosmet Laser Ther. 2011 Feb;13((1)):2–5. doi: 10.3109/14764172.2011.552616. [DOI] [PubMed] [Google Scholar]
- 10.Xu ZL, Xu J, Zhuo FL, Wang L, Xu W, Xu Y, et al. Effects of laser irradiation on Trichophyton rubrum growth and ultrastructure. Chin Med J (Engl) 2012 Oct;125((20)):3697–700. [PubMed] [Google Scholar]
- 11.Hashimoto T, Wu-Yuan CD, Blumenthal HJ. Isolation and characterization of the rodlet layer of Trichophyton mentagrophytes microconidial wall. J Bacteriol. 1976 Sep;127((3)):1543–9. doi: 10.1128/jb.127.3.1543-1549.1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kozarev J, Vižintin Z. Novel Laser Therapy in Treatment of Onychomycosis. Journal of the Laser and Health Academy [Internet] 2010 Apr [cited 2012 Jan 06];1:[about 8 p.]. Available from: https://www.laserandhealthacademy.com/media/objave/academy/priponke/novel_laser_therapy_in_treatment_of_onychomycosis.pdf. [Google Scholar]
- 13.Zawar V, Sarda A, De A. Clearance of Recalcitrant Onychomycosis Following Q-switched Nd-Yag Laser. J Cutan Aesthet Surg. 2017 Oct-Dec;10((4)):226–7. doi: 10.4103/JCAS.JCAS_18_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carney C, Tosti A, Daniel R, Scher R, Rich P, DeCoster J, et al. A new classification system for grading the severity of onychomycosis: Onychomycosis Severity Index. Arch Dermatol. 2011 Nov;147((11)):1277–82. doi: 10.1001/archdermatol.2011.267. [DOI] [PubMed] [Google Scholar]
- 15.Scher RK, Tavakkol A, Sigurgeirsson B, Hay RJ, Joseph WS, Tosti A, et al. Onychomycosis: diagnosis and definition of cure. J Am Acad Dermatol. 2007 Jun;56((6)):939–44. doi: 10.1016/j.jaad.2006.12.019. [DOI] [PubMed] [Google Scholar]