Abstract
Background
The importance of clinical leadership in ensuring high quality patient care is emphasized in health systems worldwide. Of particular concern are the high costs to health systems related to clinical litigation settlements. To avoid further cost, healthcare systems particularly in High-Income Countries invest significantly in interventions to develop clinical leadership among frontline healthcare workers at the point of care. In Low-Income Countries however, clinical leadership development is not well established. This review of the literature was conducted towards identifying a model to inform clinical leadership development interventions among frontline healthcare providers, particularly for improved maternal and newborn care.
Methods
A structural literature review method was used, articles published between 2004 and 2017 were identified from search engines (Google Scholar and EBSCOhost). Additionally, electronic databases (CINHAL, PubMed, Medline, Academic Search Complete, Health Source: Consumer, Health Source: Nursing/Academic, Science Direct and Ovid®), electronic journals, and reference lists of retrieved published articles were also searched.
Results
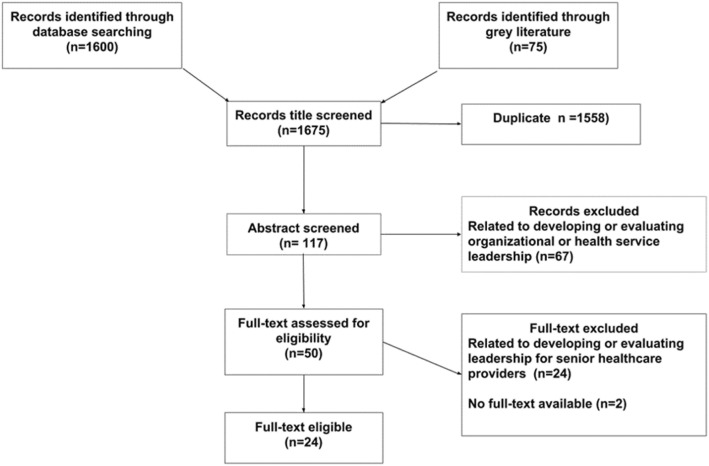
Employing pre-selected criteria, 1675 citations were identified. After screening 50 potentially relevant full-text papers for eligibility, 24 papers were excluded because they did not report on developing and evaluating clinical leadership interventions for frontline healthcare providers, 2 papers did not have full text available. Twenty-four papers met the inclusion criteria for review. Interventions for clinical leadership development involved the development of clinical skills, leadership competencies, teamwork, the environment of care and patient care. Work-based learning with experiential teaching techniques is reported as the most effective, to ensure the clinical leadership development of frontline healthcare providers.
Conclusions
All studies reviewed arose in High-Income settings, demonstrating the need for studies on frontline clinical leadership development in Low-and Middle-Income settings. Clinical leadership development is an on-going process and must target both novice and veteran frontline health care providers. The content of clinical leadership development interventions must encompass a holistic conceptualization of clinical leadership, and should use work-based learning, and team-based approaches, to improve clinical leadership competencies of frontline healthcare providers, and overall service delivery.
Keywords: Clinical leadership development, Clinical leadership evaluation, Frontline healthcare providers, Bedside
Background
Clinical leadership by frontline healthcare providers is a critical part of bedside care [1]. Clinical leadership is recommended for the potential impact on clinical practice and on the clinical care environment, and contributes to safe and quality patient care, and to job satisfaction and retention of frontline healthcare providers [1–6]. Frontline healthcare providers are well placed to identify work inefficiencies, motivate other members of the care team to act on patient care, and lead change initiatives to correct problems that arise in the clinical setting. Frontline healthcare providers can also identify inefficiencies related to organizational structures and work flows, and to poor policies and procedures for the delivery of optimal patient care [2, 5, 7–10]. Conversely, poor frontline clinical leadership in the clinical setting has been associated with adverse events and clinical litigation settlements, prompting many healthcare systems, particularly in High-Income Countries (HICs), to invest significantly in interventions that support clinical leadership development [3, 11].
However, in Low- and Middle-Income Countries (LMICs), clinical leadership development is not well established. As an example, in South African maternity services, maternal and perinatal deaths have been associated with deficiencies in frontline clinical leadership [12–18]. Albeit the need for clinical leadership development interventions has been identified, there is little evidence to support the planning, implementation and evaluation of such interventions, particularly among frontline healthcare providers, in LMICs [13–18].
Towards identifying a model to inform clinical leadership development among frontline healthcare providers in LMIC, including maternity services in South Africa, a literature review was conducted. The purpose of the literature review was to synthesize published evidence on frontline clinical leadership development and its evaluation and included multiple frontline-care contexts. A database was constructed to extract important dimensions of the clinical leadership development interventions. Further, to synthesize the reported findings on the evaluation of the effectiveness of clinical leadership interventions, Kirkpatrick’s evaluation approach was used [19, 20]. Kirkpatrick’s approach to evaluation comprises four levels, presented as a sequence, and includes evaluating the:
Reaction: what participants think and feel about the intervention
Learning: the resulting increase in knowledge or skills, and changes in attitude
Behaviour: change in practice because of the intervention
Result: the final result that occurs as a result of the intervention (e.g. service delivery, or patient outcomes) [19, 20].
The findings of the literature review will contribute to the design and evaluation of interventions to improve clinical leadership at the bedside in LMICs generally, and in the maternity services of South Africa specifically.
Methods
Aim
The aim of the literature review was to describe the characteristics and the evaluation of clinical leadership development interventions targeting frontline healthcare providers.
Design
A structured approach, the systematic quantitative literature review method [21], was used to search and identify the literature, and extract information on interventions for clinical leadership development.
Search methods
The searches were conducted using Google Scholar and EBSCOhost search engines. Additionally, electronic databases including CINHAL, PubMed, Medline, Academic Search Complete, Health Sources: Nursing/Academic Edition, Science Direct and Ovid®), were searched using the following keywords: ‘clinical leadership’, ‘frontline leadership’, ‘nursing leadership’, ‘ward leadership’, ‘medical leadership’, ‘clinician leadership’ in combination with: ‘development’, ‘programme’, ‘interventions’, ‘evaluation’ and ‘training’. A manual search was conducted to trace sources in the reference list of retrieved published articles.
Eligibility criteria
Inclusion criteria
Papers meeting the following criteria were included for review: (1) original research published in peer-reviewed journals; (2) grey literature; (3) reporting the implementation or evaluation of interventions for clinical leadership development; (4) published in English between 2004 and 2017.
Exclusion criteria
Papers exploring the implementation and/or the evaluation of interventions or approaches for the development of health service or organizational leadership, or development of senior healthcare leaders were excluded.
Assessment of publications
The database search generated 1600 records; grey literature (health services reports, research reports, theses, and dissertations) generated 75 records; of which 1558 were duplicate. On a review of abstracts 117 papers were excluded [related to developing or evaluating organizational or health services leadership]. On screening 50 potentially relevant full-text papers, 24 were excluded [did not report on developing or evaluating clinical leadership for frontline healthcare providers], and 2 [did not have full text available]. Twenty-four papers met the inclusion criteria and were captured in the database.
Figure 1 presents the search algorithm indicating the number of identified studies, included and excluded studies, and reasons for exclusion.
Fig. 1.
Search algorithm, indicating number of identified studies, included and excluded studies, and reasons for exclusion
The quality of the studies reviewed was appraised using the Standards for Reporting Implementation Studies (StaRI) [22]. Against the StaRI criteria, the studies reporting the interventions and the evaluation of interventions for clinical leadership development did not provide adequate descriptions of the interventions themselves, of the methods used in implementing the interventions, and of the evaluation of the interventions. However, they included sound descriptions of the aims and the target groups for which the interventions were designed. Two studies provided sufficient descriptions of the intervention, the implementation and the evaluation in order to produce transferable findings [23, 24]. Overall, the studies included in this review were of poor quality. However, the shortcomings identified did not detract from the purpose of the present literature review.
Constructing the database
A database was constructed to summarise the studies identified for the review. The following information was captured in the database: the country where the intervention/evaluation was implemented, the aim of the intervention/evaluation, the target population for which the intervention was designed, the content areas of the intervention, the educational approach used, the educational techniques used, the time frame of the intervention, how the impact of intervention was measured, the outcomes and limitations of the intervention as reported in the papers.
Results
The aim of this literature review was to establish, from the published corpus, how clinical leadership was developed among frontline healthcare providers. Interventions for clinical leadership were summarized and synthesized. A total of 24 papers exploring the implementation and the evaluation of interventions for clinical leadership development met the inclusion criteria. The interventions are summarized below.
Country where the intervention was implemented
All interventions for clinical leadership development included in this review were implemented in High-Income Countries (HIC). Thirteen papers reported on studies conducted in the United Kingdom (UK) (England, Ireland and Scotland) [25–37] while six reported studies in Australia [23, 38–42] and three in the United States of America (USA) [24, 43, 44]. One study was conducted in Belgium [45] and one in Switzerland [46] (Table 1).
Table 1.
Country where the intervention was implemented
| Author | Country | Year |
|---|---|---|
| Cleary et al. [38] | Australia | 2005 |
| Ferguson et al. [39] | Australia | 2007 |
| Williams et al. [40] | Australia | 2009 |
| Travaglia et al. [41] | Australia | 2011 |
| MacPhail et al. [23] | Australia | 2015 |
| Leggat et al. [42] | Australia | 2016 |
| Dierckx de Casterelé [45] | Belgium | 2008 |
| Miller and Dalton [25] | England | 2011 |
| Leeson and Millar [26] | England | 2013 |
| Enterkin et al. [27] | England | 2013 |
| Phillips and Byrne [31] | England | 2013 |
| Castillo and James [32] | England | 2013 |
| Stoll et al. [33] | England | 2011 |
| Miani et al. [34] | England | 2013 |
| Runnacle et al. [35] | England | 2013 |
| Lunn et al. [28] | Ireland | 2008 |
| McNamara et al. [29] | Ireland | 2014 |
| Fealy et al. [36] | Ireland | 2015 |
| Patton et al. [37] | Ireland | 2013 |
| Pearson et al. [30] | Scotland | 2010 |
| Martin et al. [46] | Switzerland | 2012 |
| Kling [43] | USA | 2010 |
| Abraham [44] | USA | 2011 |
| Lekan et al. [24] | USA | 2011 |
Aims of the interventions
The emphasis of most interventions was on developing clinical skills. Some interventions were designed to develop leadership competencies, to promote succession planning, to enhance the contribution of frontline healthcare providers to patient experiences, and to ensure quality and safe health services [23–31, 36, 37, 39–42, 44–46] (Table 2). Other interventions focused on preparing nursing students, medical students, and novice frontline healthcare providers for future leadership roles and for ensuring quality care and patient safety [33, 35, 43]. Some interventions were developed to transform managers into leaders [32].
Table 2.
Aim of the intervention
| Author | Country | Year | Aim of the intervention |
|---|---|---|---|
| Cleary et al. [38] | Australia | 2005 | Develop and consolidate clinical leadership skills |
| Ferguson et al. [39] | Australia | 2007 | Develop clinical leaders’ skills to observe clinical practices in a structured way to create a culture of quality and safety |
| Williams et al. [40] | Australia | 2009 | Develop necessary skills to act as clinical leaders |
| Travaglia et al. [41] | Australia | 2011 | Develop the skills to provide coordinated care |
| MacPhail et al. [23] | Australia | 2015 | Foster leadership capability and encourage engagement in decision making within their teams |
| Leggat et al. [42] | Australia | 2016 | Develop clinical leadership skills in ensuring high quality and safe health service |
| Dierckx de Casterelé [45] | Belgium | 2008 | Strengthen leadership competence in quality improvement projects |
| Miller and Dalton [25] | England | 2011 | Provide mentoring in clinical leadership |
| Leeson and Millar [26] | England | 2013 | Enable participants to take initiatives, focus on priorities and continuous quality improvement |
| Phillips and Byrne [31] | England | 2013 | Enhance ward managers’ contribution to patient experience and quality of care |
| Castillo and James [32] | England | 2013 | Transform managers into leaders |
| Stoll et al. [33] | England | 2011 | Develop future clinical leaders |
| Miani et al. [34] | England | 2013 | Foster a culture of quality improvement |
| Runnacle et al. [35] | England | 2013 | Prepare trainees to ensure safe and effective services |
| Enterkin et al. [27] | England | 2013 | Prepare participants for the role of ward sister |
| Lunn et al. [28] | Ireland | 2008 | Develop transformational leadership behaviours |
| McNamara et al. [29] | Ireland | 2014 | Develop clinical leadership skills |
| Fealy et al. [36] | Ireland | 2015 | Develop leadership competence to improve service delivery |
| Patton et al. [37] | Ireland | 2013 | Develop clinical leadership competencies |
| Pearson et al. [30] | Scotland | 2010 | Develop leadership potential |
| Martin et al. [46] | Switzerland | 2012 | Enhance leadership competence |
| Kling [43] | USA | 2010 | Maximize students learning |
| Abraham [44] | USA | 2011 | Enhance leadership skills |
| Lekan et al. [24] | USA | 2011 | Support the development of clinical leadership |
Target group for which interventions were implemented
Interventions for clinical leadership development targeted a variety of frontline health care providers (Table 3). Only a few interventions included frontline healthcare providers for maternal and child health [28–30, 32, 34, 36, 37, 41], while the remainder of interventions included early career nurses, qualified nurses, medical doctors, and allied healthcare professionals in hospital settings, including primary and secondary, acute, academic, community and regional hospitals, and mental health and geriatric wards [23, 26, 27, 31, 35, 38–40, 44, 45]. Other target groups include novice students, senior level nursing students, senior registrars, and postgraduate medical and dental students [24, 25, 42, 43].
Table 3.
Target group which interventions were implemented
| Author | Country | Year | Target group which interventions were implemented |
|---|---|---|---|
| Cleary et al. [38] | Australia | 2005 | Mental health nurses |
| Ferguson et al. [39] | Australia | 2007 | Clinical leaders in mental and occupational health, theatre, emergency, nursery, post-natal ward |
| Williams et al. [40] | Australia | 2009 | New graduates (nurses) |
| Travaglia et al. [41] | Australia | 2011 | Nursing and midwifery unit managers |
| MacPhail et al. [23] | Australia | 2015 | Medical doctors, nurses and allied health professionals |
| Leggat et al. [42] | Australia | 2016 | Medical doctors, nurses, and allied healthcare providers |
| Dierckx de Casterelé [45] | Belgium | 2008 | Head nurses |
| Miller and Dalton [25] | England | 2011 | Senior registrars |
| Leeson and Millar [26] | England | 2013 | Nurses and allied healthcare professionals |
| Enterkin et al. [27] | England | 2013 | Staff nurse and midwives, newly qualified nurses |
| Phillips and Byrne [31] | England | 2013 | Ward managers |
| Castillo and James [32] | England | 2013 | Wards managers, senior nurses and midwives |
| Stoll et al. [33] | England | 2011 | Junior doctors |
| Miani et al. [34] | England | 2013 | Doctors, nurses and midwives |
| Runnacle et al. [35] | England | 2013 | Trainees doctors |
| Lunn et al. [28] | Ireland | 2008 | Nurses and midwives |
| McNamara et al. [29] | Ireland | Nurses and midwives | |
| Fealy et al. [36] | Ireland | 2015 | Nurses and midwives |
| Patton et al. [37] | Ireland | 2013 | Nurses and midwives |
| Pearson et al. [30] | Scotland | 2010 | Early career and qualified nurses and midwives |
| Martin et al. [46] | Switzerland | 2012 | Nurse leaders |
| Kling [43] | USA | 2010 | Novice students |
| Abraham [44] | USA | 2011 | Registered nurses |
| Lekan et al. [24] | USA | 2011 | Senior level nursing students |
Content areas covered by the interventions
Development of clinical skills was common to the majority of interventions as summarized in Table 4 [24, 28, 30, 33, 35–39, 41–43, 45, 46]. Other content areas included personal development, teamwork, team management, team building, service delivery, care processes, and the environment of care needed to ensure quality and safe services [23, 26, 27, 29, 31, 32, 34, 40, 44].
Table 4.
Content areas covered by the interventions
| Author | Country | Year | Content areas covered by the interventions |
|---|---|---|---|
| Cleary et al. [38] | Australia | 2005 | Personal development, teamwork, clinical skills, service delivery |
| Ferguson et al. [39] | Australia | 2007 | Observation, feedback skills, clinical practice skills, patient care, teamwork, environment of care, quality improvement (QI) |
| Williams et al. [40] | Australia | 2009 | Leadership skills development |
| Travaglia et al. [41] | Australia | 2011 | Clinical skills and leadership skills development |
| MacPhail et al. [23] | Australia | 2015 | Leadership skills, multi-disciplinary teamwork |
| Leggat et al. [42] | Australia | 2016 | Clinical skills leadership skills, quality and safety skills |
| Dierckx de Casterelé [45] | Belgium | 2008 | Clinical and leadership skills, teamwork, care environment, care giving process |
| Miller and Dalton [25] | England | 2011 | Teamwork |
| Leeson and Millar [26] | England | 2013 | Leadership skills development |
| Enterkin et al. [27] | England | 2013 | Leadership skills development |
| Phillips and Byrne [31] | England | 2013 | Clinical skills development, teamwork and patient care |
| Castillo and James [32] | England | 2013 | Leadership skills development, team management, and service improvement |
| Stoll et al. [33] | England | 2011 | Personal development, clinical skills, service delivery |
| Miani et al. [34] | England | 2013 | Clinical skills and leadership skills, team management and the environment of care |
| Runnacle et al. [35] | England | 2013 | Clinical skills |
| Lunn et al. [28] | Ireland | 2008 | Personal development, clinical skills, team building, patient care |
| McNamara et al. [29] | Ireland | 2014 | Clinical leadership skills development |
| Fealy et al. [36] | Ireland | 2015 | Clinical skills for service delivery |
| Patton et al. [37] | Ireland | 2013 | Personal development and teamwork |
| Pearson et al. [30] | Scotland | 2010 | Personal development, team management |
| Martin et al. [46] | Switzerland | 2012 | Clinical and leadership practice |
| Kling [43] | USA | 2010 | Clinical skills, personal development, leadership skills |
| Abraham [44] | USA | 2011 | Leadership skills development |
| Lekan et al. [24] | USA | 2011 | Leadership skills development, clinical skills, and patient care |
Educational approaches
Primarily the interventions for clinical leadership development were offered in the form of in-service training using a work-based learning (WBL) educational approach within the clinical settings [28, 29, 31–34, 36–38, 42, 45, 46]. Classroom-based learning (CBL) conducted in classrooms outside of clinical settings [30, 43] or a combination of both were also used [27, 41, 44]. Some interventions were offered as postgraduate training programmes, using a combination of WBL and CBL [24, 25, 30, 35] (Table 5).
Table 5.
Educational approaches
| Author | Country | Year | Educational approaches |
|---|---|---|---|
| Cleary et al. [38] | Australia | 2005 | Work-based learning (WBL) as in-service training |
| Ferguson et al. [39] | Australia | 2007 | WBL as in-service training |
| Williams et al. [40] | Australia | 2009 | WBL as in-service training |
| Travaglia et al. [41] | Australia | 2011 | Classroom based learning (CBL) as in-service training with online interaction sessions |
| MacPhail et al. [23] | Australia | 2015 | WBL as in-service training and demonstration of best practices |
| Leggat et al. [42] | Australia | 2016 | WBL and Case-Based Learning as in-service training |
| Dierckx de Casterelé [45] | Belgium | 2008 | WBL as in-service training |
| Miller and Dalton [25] | England | 2011 | WBL as postgraduate programme |
| Leeson and Millar [26] | England | 2013 | WBL as in-service training |
| Enterkin et al. [27] | England | 2013 | WBL and CBL as in-service training |
| Phillips and Byrne [31] | England | 2013 | WBL as in-service training |
| Castillo and James [32] | England | 2013 | WBL as in-service training |
| Stoll et al. [33] | England | 2011 | WBL as in-service training |
| Miani et al. [34] | England | 2013 | WBL |
| Runnacle et al. [35] | England | 2013 | WBL postgraduate training |
| Lunn et al. [28] | Ireland | 2008 | WBL as in-service training |
| McNamara et al. [29] | Ireland | 2014 | WBL as in-service training |
| Fealy et al. [36] | Ireland | 2015 | WBL as in-service training |
| Patton et al. [37] | Ireland | 2013 | WBL as in-service training |
| Pearson et al. [30] | Scotland | 2010 | CBL postgraduate programme |
| Martin et al. [46] | Switzerland | 2012 | WBL as in-service training |
| Kling [43] | USA | 2010 | CBL as in-service training |
| Abraham [44] | USA | 2011 | WBL and CBL as in-service training |
| Lekan et al. [24] | USA | 2011 | WBL and CBL Postgraduate programme |
Educational techniques
Interventions for clinical leadership development targeting frontline healthcare providers made use of a variety of educational techniques, used singularly or in combination (Table 6.) A combination of action learning, mentorship and coaching was used in six interventions to develop various skills [28–30, 33, 36, 37]. Other educational approaches included inquiry-based learning, self-directed learning, case-based learning, problem-based learning, experiential learning, and shadowing [23, 25–27, 29, 31, 32, 35, 38–40, 42, 44–46]. Clinical supervision was used only in one intervention [24].
Table 6.
Educational techniques
| Author | Country | Year | Educational techniques |
|---|---|---|---|
| Cleary et al. [38] | Australia | 2005 | Self-directed, Learning (SDL) |
| Ferguson et al. [39] | Australia | 2007 | Observation of clinical practice by clinical leaders, feedback and reflection |
| Williams et al. [40] | Australia | 2009 | Mentoring and role modelling (unit managers to new nurses) |
| Travaglia et al. [41] | Australia | 2011 | Coaching |
| MacPhail et al. [23] | Australia | 2015 | SDL, Problem-based learning (PBL) |
| Leggat et al. [42] | Australia | 2016 | Enquiry based learning (EBL), SDL |
| Dierckx de Casterelé [45] | Belgium | 2008 | Action learning |
| Miller and Dalton [25] | England | 2011 | Mentoring (senior managers to registrars) |
| Leeson and Millar [26] | England | 2013 | PBL |
| Enterkin et al. [27] | England | 2013 | SDL, Action learning |
| Phillips and Byrne [31] | England | 2013 | CBL, Action learning |
| Castillo and James [32] | England | 2013 | Coaching Action learning |
| Stoll et al. [33] | England | 2011 | Coaching, Mentoring Action learning, QI projects |
| Miani et al. [34] | England | 2013 | Experiential learning, QI projects |
| Runnacle et al. [35] | England | 2013 | Experiential learning, QI projects |
| Lunn et al. [28] | Ireland | 2008 | Experiential learning, Action learning, Coaching, Shadowing |
| McNamara et al. [29] | Ireland | 2014 | Action learning Mentoring Coaching |
| Fealy et al. [36] | Ireland | 2015 | SDL Mentoring Coaching Action learning |
| Patton et al. [37] | Ireland | 2013 | SDL, Action Learning, Mentoring, Coaching |
| Pearson et al. [30] | Scotland | 2010 | Coaching, Mentoring, Action learning sets |
| Martin et al. [46] | Switzerland | 2012 | Case Based Learning (CBL) Coaching Action learning |
| Kling [43] | USA | 2010 | Peer mentoring (senior students to novice students) |
| Abraham [44] | USA | 2011 | Experiential learning |
| Lekan et al. [24] | USA | 2011 | Bedside clinical teaching. Clinical supervision |
Time frame of interventions for clinical leadership development
Most interventions for clinical leadership development were offered as multiple contact sessions of varying duration, ranging from a few days, to a few weeks, or to lasting several months [24, 26, 30, 33, 37–40, 44–46] (Table 7). Other interventions were offered as multiple contact sessions in postgraduates programmes [24, 30, 35]. One intervention was offered as a full-time master degree programme with no detail of the contact sessions provided [25].
Table 7.
Time frame of interventions for clinical leadership development
| Author | Country | Year | Time frame of interventions for clinical leadership development |
|---|---|---|---|
| Cleary et al. [38] | Australia | 2005 | 6 months (nature and length of contact sessions missing) |
| Ferguson et al. [39] | Australia | 2007 | 12 observations over 4 months |
| Williams et al. [40] | Australia | 2009 | 4 full time intensive weeks |
| Travaglia et al. [41] | Australia | 2011 | 5 face-to-face days and monthly collaborative coaching over 24 months (length of coaching sessions missing) |
| MacPhail et al. [23] | Australia | 2015 | One 2-h session once per month for 9 months |
| Leggat et al. [42] | Australia | 2016 | 12 months (length of contact sessions |
| Dierckx de Casterelé [45] | Belgium | 2008 | 12 months (nature and length of contact sessions missing) |
| Miller and Dalton [25] | England | 2011 | 1-year full time master’s programme (nature and length of contact sessions missing) |
| Leeson and Millar [26] | England | 2013 | 2 days per week, every week over 6 weeks |
| Enterkin et al. [27] | England | 2013 | 8 days, 1 day/ month over 8 months |
| Phillips and Byrne [31] | England | 2013 | Four modules, each 8-h days per day |
| Castillo and James [32] | England | 2013 | Three 1-day module, three ½ day action learning sets over 8 months |
| Stoll et al. [33] | England | 2011 | 12 months full time programme (nature and length of contact sessions missing) |
| Miani et al. [34] | England | 2013 | 2 days (internal fellows), and 4 days a week external fellows) over 12 months |
| Runnacle et al. [35] | England | 2013 | 1-h workshop; 6 months programme (2 full workshops 1 month apart; over 1-year full time fellowship |
| Lunn et al. [28] | Ireland | 2008 | 12 months (nature and length of contact sessions missing) |
| McNamara et al. [29] | Ireland | 2014 | 6 months’ (nature and length of contact sessions missing) |
| Fealy et al. [36] | Ireland | 2015 | 6 months tailored to participants needs |
| Patton et al. [37] | Ireland | 2013 | Tailored to individuals’ time frame over 6 months |
| Pearson et al. [30] | Scotland | 2010 | 1 year flying start, 2 years masters’ degree periodically, Action learning sets, over three years |
| Martin et al. [46] | Switzerland | 2012 | 18 days (1 day/month) over 12 months for the intervention phase and over 6 months in the follow up phase |
| Kling [43] | USA | 2010 | 3 h’ classroom, 6 h per week clinical component |
| Abraham [44] | USA | 2011 | 32 h/month over 6 months |
| Lekan et al. [24] | USA | 2011 | 3 weeks SDL and CBL, 3 weeks 8- h clinical rotation. 1-week reflective journal |
How interventions were measured
Best practice in measuring an intervention is to use pre-post evaluation. Nine out of twenty-four studies used pre-and post-test methods to measure the learning attainment, behaviour, and impact of the intervention [23, 24, 28, 35, 38, 41, 42, 44, 46]. Fifteen studies used only post-test methods to measure the effectiveness of the interventions (Table 8).
Table 8.
How interventions were assessed
| Author | Country | Year | How interventions were assessed |
|---|---|---|---|
| Cleary et al. [38] | Australia | 2005 | Pre-and post-assessment to measure the reaction, and learning attainment of participants using the Nurse Self-Concept Questionnaire |
| Ferguson et al. [39] | Australia | 2007 | Post-test to measure the learning attainment and behaviour of participants using review of observation documents |
| Williams et al. [40] | Australia | 2009 | Post-test to measure the reaction participants using a Questionnaire and focus group discussions (FDGs) |
| Travaglia et al. [41] | Australia | 2011 | Mid-term assessment to measure the learning attainment and behavior of participants, and impact on service delivery interviews and online survey |
| MacPhail et al. [23] | Australia | 2015 | Pre-and post-assessment and follow-up 18 moths post intervention to assess the reaction, and learning attainment of participants using structured evaluation survey and questionnaire |
| Leggat et al. [42] | Australia | 2016 | Pre-and post-assessment to measure participants behaviour and impact of the intervention using questionnaires and interviews |
| Dierckx de Casterelé [45] | Belgium | 2008 | Post-test assessment to measure the behaviour, learning attainment and impact of the intervention, using interviews, FDGs and observation of participants |
| Miller and Dalton [25] | England | 2011 | Post-test assessment to measure individuals’ reaction using FDGs, interviews, and online questionnaires |
| Leeson and Millar [26] | England | 2013 | Post-test assessment to measure the reaction and learning attainment, and behaviour of participants, using evaluation sheets |
| Enterkin et al. [27] | England | 2013 | Post-test assessment to measure participants’ reaction and learning attainment questionnaires |
| Phillips and Byrne [31] | England | 2013 | Post-test assessment to measure the reaction and learning of participants, using questionnaires |
| Castillo and James [32] | England | 2013 | Post-test assessment to measure participant reaction, learning, behaviour and impact of the intervention using questionnaires |
| Stoll et al. [33] | England | 2011 | Post-test assessment to measure, learning attainment and impact of the intervention, using questionnaires and interviews |
| Miani et al. [34] | England | 2013 | Post-test assessment to measure the learning of participant, behaviour, and impact of the intervention, using Online questionnaires and interviews |
| Runnacle et al. [35] | England | 2013 | Pre- and post- assessment to measure the reaction of participants |
| Lunn et al. [28] | Ireland | 2008 | Pre-and post-assessment to measure the reaction, learning and behaviour of participants, using questionnaires |
| McNamara et al. [29] | Ireland | 2014 | Post-test assessment to measure participants’ reactions using FDGs, and interviews |
| Fealy et al. [36] | Ireland | 2015 | Post-test assessment to measure the impact of the intervention, using service assessment tools |
| Patton et al. [37] | Ireland | 2013 | Post-test assessment to measure participants’ learning and behaviour using the leadership practice inventory, clinical leaders’ behaviour questionnaires, FGDs and group interviews |
| Pearson et al. [30] | Scotland | 2010 | Post-test assessment to measure participants’ reaction and behaviour, using FGDs and questionnaires |
| Martin et al. [46] | Switzerland | 2012 | Pre-and post- assessment to participants’ behaviour using, observation and self-assessment tools |
| Kling [43] | USA | 2010 | Post-test assessment at 6-month post intervention to measure participant reaction, learning attainment and behaviour using questionnaires |
| Abraham [44] | USA | 2011 | Pre-and post- assessment at 6 and 12 months following completion of intervention to measure participant learning, behaviour and impact of the intervention |
| Lekan et al. [24] | USA | 2011 | Pre-and post- test assessment to measure participant reaction, learning attainment, and impact of the intervention |
To categorize how the different articles evaluated their interventions, Kirkpatrick’s approach was used. Only one study included an evaluation at all four levels namely, the reaction, learning attainment and behaviour, and impact of the intervention on service delivery [32]. Measuring participant reactions to the interventions was common to most interventions [23–27, 29–32, 35, 38–40, 43]. Learning attainment, and the behavior of participants were also measured. The tools used to collect evaluation data included self-report questionnaires, online surveys, evaluation sheets, structured evaluation forms. Additional tools included in-depth-interviews, group interviews, FGDs, observations of action learning sets and document review.
Outcomes of the interventions as reported in the papers
The outcomes of the interventions recorded in the papers include: personal development [increased self-awareness and confidence, feelings of empowerment, time management, development of emotional intelligence skills and increased learning ability] [27, 32, 34, 37, 38, 45]; enhanced leadership knowledge and skills [communication, willingness to lead teams, delegation, ability to empower others, problem solving, decision making, ability to inspire a shared vision, team management] [24, 26–29, 32, 34–37, 41, 43–46]; improved clinical knowledge and skills [enhanced basic nursing knowledge and skills, improved clinical practices, understanding of contribution to patient care] [42], improved teamwork [ability to work as part of multi-disciplinary teams, ability to manage teams] [23, 25, 30, 31, 37, 40, 43], improved patient care [increased focus on patient care, improved patient outcomes], and service delivery [change in care processes] [24, 28, 33, 39, 41, 45] (Table 9).
Table 9.
Outcomes of the interventions as reported in the papers
| Author | Country | Year | Outcomes of the interventions as reported in the papers |
|---|---|---|---|
| Cleary et al. [38] | Australia | 2005 | Intervention useful to their work, Improved communication, clinical skills, teamwork |
| Ferguson et al. [39] | Australia | 2007 | Opportunity to review care practices, development of QI plans, improved observation and feedback skills, team building |
| Williams et al. [40] | Australia | 2009 | Evaluated positively bay all stakeholders |
| Travaglia et al. [41] | Australia | 2011 | Feeling of empowerment to implement change in the work environment, improved communication, unit performance and patient flow |
| MacPhail et al. [23] | Australia | 2015 | High satisfaction with the intervention, feasible, increased willingness to lead teams and work as part of multidisciplinary teams |
| Leggat et al. [42] | Australia | 2016 | Improved leadership practices, emotional intelligence, psychological empowerment patient safety skills |
| Dierckx de Casterelé [45] | Belgium | 2008 | Self-awareness enhanced communication skills, improvement of the work environment |
| Miller and Dalton [25] | England | 2011 | Successful in building teamwork and communication |
| Leeson and Millar [26] | England | 2013 | Positive experience, ability to take responsibility for action, change in working practices |
| Enterkin et al. [27] | England | 2013 | Feelings of empowerment, self-awareness and confidence, ability to delegate, and empower others, feeling of support from management |
| Phillips and Byrne [31] | England | 2013 | Increased understanding of participants’ contribution to patient care |
| Castillo and James [32] | England | 2013 | Improved confidence, better communication, increased problem-solving skills |
| Stoll et al. [33] | England | 2011 | Greater understand of service delivery, change in care processes and procedures |
| Miani et al. [34] | England | 2013 | Enhanced leadership and communication skills, team management skills, increased confidence, improved patient experience |
| Runnacle et al. [35] | England | 2013 | Improvement in use of quality improvement skills |
| Lunn et al. [28] | Ireland | 2008 | Enhanced communication, problem solving and decision-making skills, ability to empower teams |
| McNamara et al. [29] | Ireland | 2014 | Supportive and contributes to clinical leadership skills development |
| Fealy et al. [36] | Ireland | 2015 | Service development, improved care practices |
| Patton et al. [37] | Ireland | 2013 | Increased self-awareness, improved communication skills and team work |
| Pearson et al. [30] | Scotland | 2010 | Good in preparing participants for work challenges, increased ability to manage relationships |
| Martin et al. [46] | Switzerland | 2012 | Improved ability to inspire shared vision, and challenging the process |
| Kling [43] | USA | 2010 | Positive experience, enhanced basic nursing skills and knowledge, improved time management and delegation skills |
| Abraham [44] | USA | 2011 | Improved decision-making skills |
| Lekan et al. [24] | USA | 2011 | Improved communication skills, ability to delegate, skills to lead practice, patient outcomes, promotion of nurses to supervisory posts |
Limitations of the interventions
Of studies that reported the limitations of interventions the following were identified: difficulty in gaining consent from patients to be observed while care was being provided and some trainers may not be skilled enough to observe using direct observation [39]; interventions that were too intensive and demanding, affecting the motivation and ability of participants to attend all sessions [27, 30, 40]; time away from clinical duties, resistance from colleagues to implement changed practices, and nurses or midwives taking clinical leadership roles and lack of support from health service managers [23, 25, 34, 41]; short timeline for progamme implementation which did not allow for assessing the impact of interventions on participants, service users and on service delivery [23, 29, 34, 36]; and challenges with sustainability of gains made through the interventions [31, 38]. A lack of a control group in evaluating interventions was also considered a limitation in attributing changes to the intervention [24]. The transferability of the intervention was also questioned [42] (Table 10).
Table 10.
Limitations of the interventions
| Author | Country | Year | Limitations of the interventions |
|---|---|---|---|
| Cleary et al. [38] | Australia | 2005 | Sustainability of the intervention is challenging |
| Ferguson et al. [39] | Australia | 2007 | Difficulty in gaining consent from patient to be observed; skills of observer |
| Williams et al. [40] | Australia | 2009 | Too intensive thus affecting motivation and ability to attend all sessions |
| Travaglia et al. [41] | Australia | 2011 | Resistance from colleagues to change, and nurse/ midwives taking clinical leadership roles, time constraints |
| MacPhail et al. [23] | Australia | 2015 | Time away from clinical duties Short timeline from progamme implementation and limited evaluation of participants’ leadership knowledge and skills |
| Leggat et al. [42] | Australia | 2016 | * |
| Dierckx de Casterelé[45] | Belgium | 2008 | * |
| Miller and Dalton [25] | England | 2011 | Time away from the clinical setting |
| Leeson and Millar [26] | England | 2013 | * |
| Enterkin et al. [27] | England | 2013 | Intervention too long |
| Phillips and Byrne [31] | England | 2013 | Maintaining momentum generated by the intervention |
| Castillo and James [32] | England | 2013 | * |
| Stoll et al. [33] | England | 2011 | * |
| Miani et al. [34] | England | 2013 | Resistance to change from frontline healthcare providers who did not taking part in the programme. Short period of time to enable change |
| Runnacle et al. [35] | England | 2013 | * |
| Lunn et al. [28] | Ireland | 2008 | * |
| McNamara et al. [29] | Ireland | 2014 | * |
| Fealy et al. [36] | Ireland | 2015 | * |
| Patton et al. [37] | Ireland | 2013 | * |
| Pearson et al. [30] | Scotland | 2010 | Intervention very demanding |
| Martin et al. [46] | Switzerland | 2012 | |
| Kling [43] | USA | 2010 | * |
| Abraham [44] | USA | 2011 | * |
| Lekan et al. [24] | USA | 2011 | Without control group changes cannot be conclusively attributed to the intervention |
*represents missing data
Discussion
This literature review of the implementation and evaluation of interventions for clinical leadership development was conducted towards identifying a model to inform clinical leadership development among frontline healthcare providers in Low- and Middle-Income Countries (LMICs) generally, and for the delivery of optimal maternal and perinatal care in South Africa specifically.
All descriptions of interventions for clinical leadership development derive from studies implemented in HICs. This would limit the transferability of study findings to LMICs, where clinical leadership is still underdeveloped and healthcare systems are faced with different contextual challenges [8]. Studies are required to explore appropriate interventions to improve clinical leadership in LMICs, including South Africa.
Of note, clinical leadership development programmes targeted novice to veteran frontline healthcare providers, in both formal and informal leadership positions [23]. This could indicate a previous neglect of ongoing clinical leadership development amongst frontline healthcare workers across the health system. With the emphasis on developing clinical expertise, interventions for clinical leadership development must include frontline healthcare workers who have been practicing for some time and may serve the purpose of updating veteran healthcare workers to new evidence-based practices of care.
Some interventions for clinical leadership development reported in this review embraced a holistic conceptualization of clinical leadership, paying attention to clinical skills, leadership skills, team building, team management, the environment of care, and service delivery [34, 38, 45]. Other interventions were more selective, based on checklists of whether participants manifested certain clinical skills. Interventions that embrace a holistic conceptualization of clinical leadership are more detailed, and can produce well trained and skilled clinical leaders. However, they may be expensive, and may require longer training periods, as they include multiple dimensions of clinical leadership. Interventions based on a selective understanding of clinical leadership may be shorter in nature, as they may focus on fewer dimensions of clinical leadership. However, these interventions may not be able to produce skilled clinical leaders.
Most interventions for clinical leadership development used work-based learning as an educational approach to improve, develop, maintain or increase practicing professionals’ competence in the clinical setting [47, 48]. Work-based learning (WBL) has been shown to promote practical learning and to help practitioners relate new knowledge to their work environment [49, 50]. Classroom-based learning takes participants away from their work environment, a feature often considered as a major weakness of this approach [49, 50]. A systematic review evaluating in-service training suggests that WBL is the most appropriate approach to improve not only the knowledge of participants but also the skills, behaviors and attitudes of participants [51–53]. WBL with experiential teaching techniques, such as mentoring and coaching, can ensure effective clinical leadership development of frontline healthcare providers.
In many interventions, the actual length of exposure to contact sessions, and the balance of time between the delivery of training content, and hands-on activities, were not detailed. The paucity of information poses a challenge when trying to replicate the interventions to other settings. In the interventions that did indeed describe the length of exposure to the intervention, multiple contact sessions, over varying periods of time, were used to deliver the interventions. Intensive once-off training sessions are shown to have a negative impact on participants’ motivation [27, 40]. Multiple time-spaced contact sessions appear to be the most suitable approach to delivering in-service training programmes, as they provide participants with sufficient time and space to engage, reflect on the content of the training programme, and apply knowledge and skills to the work place [52, 54]. While designing interventions for clinical leadership development, there is a need to ensure that a reasonable timeframe tailored to participants’ needs is provided.
Most studies used only post-test evaluation to measure the effectiveness of the interventions. Post-test evaluation is outcome oriented and is concerned with the results of the intervention. The absence of pre-test observations and a lack of a control group in post-test evaluations limits the ability to attribute observed changes to the intervention [55]. Nonetheless, post-test is used in most interventions because of the logistical difficulties in obtaining pre-test observations due to time constraints [56].
Pre-post-test evaluation may be the most accurate way to provide a full picture of changes in participants over the course of the training programme. [56]. However, many interventions were implemented as once-off short interventions, over a couple of weeks. A short implementation timeline may not be sufficient to allow change to occur, and may not permit sufficient time to measure the impact of interventions in participants, teams, environments of care, or service delivery [23, 30, 34, 36].
Kirkpatrick’s approach to evaluation recommends four levels of evaluation to objectively measure the effectiveness of training programmes [19]. Most papers did not provide thorough descriptions of evaluation methods. Only one study reviewed included an evaluation at each of the four levels suggested by Kirkpatrick’s approach [32]. Most papers reporting the evaluation of interventions for clinical leadership development focused on the reactions of participants and learning attainment [27, 32, 34, 37, 38, 45]. Participants reported positive experiences, and indicated the acquisition of leadership knowledge and skills as result of the intervention [27, 32, 34, 37, 38, 45]. Some studies reported improved clinical knowledge and skills improved teamwork as the behavior of participants [23, 25, 29, 33, 34, 40, 42, 43]. The impact of interventions include improved patient care, improved patient outcomes, and change in care processes [24, 28, 33, 39, 41, 45].
Although some interventions used validated tools to evaluate the interventions, most outcomes recorded in this review used self-reported changes. Tools that elicit self-reported learning attainment and behaviour changes are considered to provide weak evaluation evidence and are of variable accuracy [57]. Factors that affect accuracy include information bias, influenced by recall bias and social desirability bias, and design bias, influenced by questionnaire design and mode of data collection [57]. To move beyond the weaknesses of to self-reported changes, the literature suggests the use of 360° assessments [58–60]. This method involves an individual and several other people (e.g. peers, supervisors, assessors, and managers) provide a comprehensive feedback on an individual’s behaviour and effectiveness [60]. It is suggested that used in combination with training programmes or interventions, 360° feedback can be an effective assessment tool [58–60]. Adequate descriptions of interventions, and rigorous description of methods used in implementing, and evaluating the interventions are required to ensure transferability of findings of interventions to other settings.
Most studies did not discuss the limitations of the interventions, or the sustainability of gains made through the intervention. One strategy to ensure sustainability of interventions for clinical leadership development is the team training approach [23]. A team training approach to clinical leadership development may serve a dual purpose: the transfer of skills and teambuilding. Teambuilding is an integral part of clinical leadership development, as well as an outcome of clinical leadership. A team training approach allows multiple professionals to be trained together, reduces resistance to change, and reduces the resistance to frontline healthcare leaders taking clinical leadership roles [23].
Strengths of the review
This review highlights the diversity, extent, and gaps of interventions for the development of clinical leadership among frontline healthcare providers. The review also highlights the conceptualizations of clinical leadership embedded in the interventions, and the challenges encountered in the implementation of interventions for clinical leadership development.
Limitations of the review
Although rigorous steps were carried out in this review, we are also aware of some limitations
Studies may have been omitted from the review if they were not published in the databases searched, or if they were published in languages other than English.
The choice to limit the search to articles that described the implementation or evaluation of interventions for clinical leadership development among frontline healthcare providers, and published between 2004 and 2017, may have reduced the range of articles included in the review.
Conclusions
The literature review was conducted towards identifying a model to inform clinical leadership development among frontline healthcare providers in LMIC settings. All studies reviewed arose in HIC settings, demonstrating the need for studies on frontline clinical leadership development in LMIC settings. The synthesis of studies conducted in HIC setting revealed what needs to be considered in the design of clinical leadership development interventions in LMIC settings. Firstly, clinical leadership development is an on-going process and must target both novice and veteran frontline health care providers. Secondly, the content of clinical leadership development interventions must encompass a holistic conceptualization of clinical leadership, with a focus on clinical skills and on competencies that support optimal clinical care. Thirdly, interventions for clinical leadership development should use work-based learning approaches, and experiential and practice-based learning techniques, as these are more likely to contribute to the sustainable development of clinical leadership among frontline healthcare providers, and to the improvement in overall service delivery. Fourthly, team-based approaches to clinical leadership development, implemented through multiple contacts over a period of time, allow the acquisition and the transfer of skills, and teambuilding. Fifthly, assessment of the expected learning and evaluation of expected outcomes need to be carefully planned in the design of clinical leadership development interventions, and measured preferable through pre-post assessments, and 3600 assessments. Lastly, adequate description of the implementation setting, of the intervention model, and of the methods used in implementing and evaluating the interventions are necessary to ensure transferability of an intervention to other settings. These guidelines established from this review of the literature, must be incorporated in the design of interventions for clinical leadership development in LMIC settings.
Acknowledgments
Funding
This paper is part of a Doctoral study partly funded through a scholarship from the College of Health Sciences at the University of KwaZulu-Natal.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- HICs
High-Income Countries
- LMICs
Low-and-Middle-Income Countries
- StaRI
Standards for Reporting Implementation Studies
- UK
United Kingdom
- USA
United States of America
- WBL
Work based learning
- CBL
Classroom based learning
- SDL
self-directed learning
- FGDs
focus group discussions
Author’s contributions
SM (University of KwaZulu-Natal) was the project leader involved throughout the study processes, from project design to write-up. AV (University of KwaZulu-Natal) is the first author’s PhD supervisor who made conceptual contributions and provided technical guidance throughout the writing processes (revising the article). Both authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Solange Mianda, Phone: +27842794310, Email: solange.zoe60@gmail.com.
Anna Voce, Email: voceas@ukkzn.ac.za.
References
- 1.Abraham A. Care and compassion? Report of the Health Service Ombudsman on ten investigations into NHS care of older people. London; 2011. https://www.ombudsman.org.uk/sites/default/files/2016-10/Care%20and%20Compassion.pdf.
- 2.Casey M, McNamara M, Fealy G, Geraghty R. Nurses’ and midwives’ clinical leadership development needs: a mixed methods study. J Adv Nurs. 2011;67:1502–1513. doi: 10.1111/j.1365-2648.2010.05581.x. [DOI] [PubMed] [Google Scholar]
- 3.Daly J, Jackson D, Mannix J, Davidson P, Hutchinson M. The importance of clinical leadership in the hospital setting. J Healthc Leadersh. 2014;6:75–83. doi: 10.2147/JHL.S46161. [DOI] [Google Scholar]
- 4.Edmonstone J. Evaluating clinical leadership: a case study. Leadersh Health Serv. 2009;22:210–224. doi: 10.1108/17511870910978132. [DOI] [Google Scholar]
- 5.Grindel C. Clinical leadership: a call to action. Medsurg Nurs. 2016;25:9–16. [PubMed] [Google Scholar]
- 6.Supamanee T, Krairiksh M, Singhakhumfu L, Turale S. Preliminary clinical nursing leadership competency model: a qualitative study from Thailand. Nurs Health Sci. 2011;13:433–439. doi: 10.1111/j.1442-2018.2011.00649.x. [DOI] [PubMed] [Google Scholar]
- 7.Doherty J. Leadership from ‘below’? Clinical staff and public hospitals in South Africa | municipal services project. 2014. http://www.municipalservicesproject.org/publication/leadership-below-clinical-staff-and-public-hospitals-south-africa. Accessed 22 May 2017.
- 8.Doherty J. Strengthening clinical leadership in hospitals: review of the international and south African literature. Municipal Service Project: South Africa; 2013. [Google Scholar]
- 9.Jonas S, McCay L, Keogh B. The importance of clinical leadership. In: Swanwick T, McKimm J, editors. ABC of clinical leadership. 1. Oxford: Blackwell Publishing Ltd; 2011. pp. 1–3. [Google Scholar]
- 10.Patrick A, Wong C, Finegan J, Laschinger HKS, Wong C, Finegan J, et al. Developing and testing a new measure of staff nurse clinical leadership: the clinical leadership survey. J Nurs Manag. 2011;19:449–460. doi: 10.1111/j.1365-2834.2011.01238.x. [DOI] [PubMed] [Google Scholar]
- 11.Wright L, Barnett P, Hendry C. Clinical leadership and clinical governance: a review of developments in New Zealand and internationally. 2001. [Google Scholar]
- 12.Schoon MG, Motlolometsi MW. Poor maternal outcomes: a factor of poor professional systems design. S Afr Med J. 2012;102:784. doi: 10.7196/SAMJ.6130. [DOI] [PubMed] [Google Scholar]
- 13.Pattinson R, Rhoda N. Saving babies 2012–2013: ninth report on perinatal care in South Africa for the PPIP group. Pretoria: Tshepesa Press; 2014. [Google Scholar]
- 14.Pattinson R, Sithembiso V, Hardy B, Moran N, Wilhelm S. Overview. In: Pattinson R, editor. Saving babies 2006–2007 sixth report on perinatal care in South Africa. Pretoria; 2009. p. 1–39. http://www.ppip.co.za/wp-content/uploads/Saving-babies-2006-7.pdf. Accessed 23 May 2017.
- 15.National Committee for the Confidential Enquiry into Maternal Deaths . Saving mothers. Pretoria. 1999. Saving mothers 1998: confidential enquiry into maternal deaths in South Africa. [Google Scholar]
- 16.National Committee for the Confidential Enquiry into Maternal Deaths . Pretoria. 2008. Saving mothers 2005-2007: fourth report on the confidential enquiry into maternal deaths in South Africa. [Google Scholar]
- 17.National Committee for the Confidential Enquiry into Maternal Deaths . Pretoria. 2014. Saving mothers 2011-2013: sixth report on the confidential enquiry into maternal deaths in South Africa. [Google Scholar]
- 18.Pattinson R, Tlebere P. Overview recommendations. In: Saving Babies 2003–2005: Fifth perinatal care survey of South Africa. 2007. p. 1–148.
- 19.Tian J, Atkinson NL, Portnoy B, Gold RS. A systematic review of evaluation in formal continuing medical education. J Contin Educ Heal Prof. 2007;27:16–27. doi: 10.1002/chp.89. [DOI] [PubMed] [Google Scholar]
- 20.Kirkpatrick D. The four levels of evaluation. Info line, tips, tools, and intelligence for trainers. 3rd edition. American society for training and development: Pewaukeen; 2007. [Google Scholar]
- 21.Pickering C, Grignon J, Steven R, Guitart D, Byrne J. Publishing not perishing: how research students transition from novice to knowledgeable using systematic quantitative literature reviews. Stud High Educ. 2015;40:1756–1769. doi: 10.1080/03075079.2014.914907. [DOI] [Google Scholar]
- 22.Pinnock H, Barwick M, Carpenter CR, Eldridge S, Grandes G. Standards for reporting implementation studies (StaRI): explanation and elaboration document. BMJ Open. 2017;7. http://digitalcommons.wustl.edu/open_access_pubs. Accessed 8 Feb 2018. [DOI] [PMC free article] [PubMed]
- 23.MacPhail A, Young C, Ibrahim JE. Workplace-based clinical leadership training increases willingness to lead. Leadersh Health Serv. 2015;28:100–118. doi: 10.1108/LHS-01-2014-0002. [DOI] [PubMed] [Google Scholar]
- 24.Lekan DA, Corazzini KN, Gilliss CL, Bailey DE, Corazzini KN, Colón-Emeric C, et al. Clinical leadership development in accelerated baccalaureate nursing students: an education innovation. J Prof Nurs. 2011;27:202–214. doi: 10.1016/j.profnurs.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 25.Miller S, Dalton K. Learning from an evaluation of Kent, Surrey and Sussex Deanery’s clinical leadership fellowship programme. Int J Clin Leadersh. http://eds.a.ebscohost.com/eds/detail/detail?vid=0&sid=a8955600-f640-4344-9fcc-d6150ec4bfa3%40sdc-v-sessmgr02&bdata=JnNpdGU9ZWRzLWxpdmU%3d#AN=61952376&db=a9h.
- 26.Leeson D, Millar M. Using the 7 habits programme to develop effective leadership. Nurs Manag. 2013;20:31–37. doi: 10.7748/nm2013.10.20.6.31.e1123. [DOI] [PubMed] [Google Scholar]
- 27.Enterkin J, Robb E, McLaren S. Clinical leadership for high-quality care: developing future ward leaders. J Nurs Manag. 2013;21:206–216. doi: 10.1111/j.1365-2834.2012.01408.x. [DOI] [PubMed] [Google Scholar]
- 28.Lunn C, Mac Curtain S, Mac Mahon J. Clinical leadership pilot: evaluation report. Nursing & Midwifery Planning & Development Unit HSE West; 2008. http://www.lenus.ie/hse/handle/10147/312631. Accessed 22 May 2017.
- 29.McNamara MS, Fealy GM, Casey M, O’Connor T, Patton D, Doyle L, et al. Mentoring, coaching and action learning: interventions in a national clinical leadership development programme. J Clin Nurs. 2014;23:2533–2541. doi: 10.1111/jocn.12461. [DOI] [PubMed] [Google Scholar]
- 30.Pearson P, Machin A, Rae A. Clinical leadership for the future: evaluation of the early clinical careers fellowship pilot programme. Scotland; 2010. http://www.nes.scot.nhs.uk/media/308771/pauline_pearson_presentation_june_2010.pdf. Accessed 22 May 2017.
- 31.Phillips N, Byrne G. Enhancing frontline clinical leadership in an acute hospital trust. J Clin Nurs. 2013;22:2625–2635. doi: 10.1111/jocn.12088. [DOI] [PubMed] [Google Scholar]
- 32.Castillo C, James S. How to turn ward managers into leaders. Nurs Times. 2013;109:18–19. [PubMed] [Google Scholar]
- 33.Stoll L, Swanwick T, Foster-Turner J, Foster-Turner J, Moss F. Leadership development for junior doctors. Int J Leadersh Public Serv. 2011;7:233–286. doi: 10.1108/17479881111194161. [DOI] [Google Scholar]
- 34.Miani C, Marjanovic S, Morgan M, Marshal M, Meikle S, Notle E. Barking, Havering and Redbridge University hospitals NHS trust fellowships in clinical leadership Programme an evaluation. London; 2013. http://www.rand.org/content/dam/rand/pubs/research_reports/RR300/RR367/RAND_RR367.pdf. Accessed 22 May 2017. [PMC free article] [PubMed]
- 35.Runnacles J, Moult B, Lachman P. Developing future clinical leaders for quality improvement: experience from a London children’s hospital. BMJ Qual Saf. 2013;22:956–963. doi: 10.1136/bmjqs-2012-001718. [DOI] [PubMed] [Google Scholar]
- 36.Fealy GM, McNamara MS, Casey M, O’Connor T, Patton D, Doyle L, et al. Service impact of a national clinical leadership development programme: findings from a qualitative study. J Nurs Manag. 2015;23:324–332. doi: 10.1111/jonm.12133. [DOI] [PubMed] [Google Scholar]
- 37.Patton D, Fealy G, Mcnamara M, Casey M, Connor T, Doyle L, et al. Individual-level outcomes from a national clinical leadership development programme. Contemp Nurse. 2013;45:56–63. doi: 10.5172/conu.2013.45.1.56. [DOI] [PubMed] [Google Scholar]
- 38.Cleary M, Freeman A, Sharrock L. The development, implementation, and evaluation of a clinical leadership programme for mental health nurses. Issues Ment Health Nurs. 2005;26:827–842. doi: 10.1080/01612840500184277. [DOI] [PubMed] [Google Scholar]
- 39.Ferguson L, Calvert J, Davie M, Fallon M, Fred N, Gersbach V, et al. Clinical leadership: using observations of care to focus risk management and quality improvement activities in the clinical setting. Contemp Nurse. 2007;24:212–224. doi: 10.5555/conu.2007.24.2.212. [DOI] [PubMed] [Google Scholar]
- 40.Williams AK, Parker VT, Milson-Hawke S, Cairney K, Peek C. Preparing clinical nurse leaders in a regional Australian teaching hospital. J Contin Educ Nurs. 2009;40:571–576. doi: 10.3928/00220124-20091119-04. [DOI] [PubMed] [Google Scholar]
- 41.Travaglia J, Debono D, Erez-Rein N, Milne J, Plumb J, Wiley J, et al. Report of the mid-program evaluation of “take the lead” Centre for Clinical Governance Research Australian Institute of health innovation. New South Wales; 2011. http://www.med.unsw.edu.au/medweb.nsf/page/ClinGov_About. Accessed 23 May 2017.
- 42.Leggat SG, Smyth A, Balding C, McAlpine I. Equipping clinical leaders for system and service improvements in quality and safety: an Australian experience. Aust N Z J Public Health. 2016;40:138–143. doi: 10.1111/1753-6405.12462. [DOI] [PubMed] [Google Scholar]
- 43.Kling VG. Clinical leadership project. J Nurs Educ. 2010;49:640–643. doi: 10.3928/01484834-20100831-02. [DOI] [PubMed] [Google Scholar]
- 44.Abraham PJ. Developing nurse leaders. Nurs Adm Q. 2011;35:306–312. doi: 10.1097/NAQ.0b013e31822ecc6e. [DOI] [PubMed] [Google Scholar]
- 45.Dierckx de Casterle B, Willemse A, Verschueren M, Milisen K. Impact of clinical leadership development on the clinical leader, nursing team and care-giving process: a case study. J Nurs Manag. 2008;16:753–763. doi: 10.1111/j.1365-2834.2008.00930.x. [DOI] [PubMed] [Google Scholar]
- 46.Martin JS, McCormack B, Fitzsimons D, Spirig R. Evaluation of a clinical leadership programme for nurse leaders. J Nurs Manag. 2012;20:72–80. doi: 10.1111/j.1365-2834.2011.01271.x. [DOI] [PubMed] [Google Scholar]
- 47.Crofts J, Ellis D, Draycott T, Winter C, Hunt L, Akande V. Change in knowledge of midwives and obstetricians following obstetric emergency training: a randomised controlled trial of local hospital, simulation Centre and teamwork training. BJOG An Int J Obstet Gynaecol. 2007;114:1534–1541. doi: 10.1111/j.1471-0528.2007.01493.x. [DOI] [PubMed] [Google Scholar]
- 48.Marinopoulos S, Dorman T, Ratanawongsa N, Wilson L, Ashar BH, Magaziner J, et al. Effectiveness of continuing medical education. Evid Rep Technol Assess (Full Rep). 2007:1–69 http://www.ncbi.nlm.nih.gov/pubmed/17764217. Accessed 22 May 2017. [PMC free article] [PubMed]
- 49.Cameron S, Rutherford I, Mountain K. Debating the use of work-based learning and interprofessional education in promoting collaborative practice in primary care: a discussion paper. Qual Prim Care. 2012;20:211–217. [PubMed] [Google Scholar]
- 50.Hardacre K, Schneider K. Work-based learning interim project report, overview of literature. PSE Consult Limited, People Ski Educ. 2007;5:1–35. [Google Scholar]
- 51.Coomarasamy A, Khan K. What is the evidence that postgraduate teaching in evidence based medicine changes anything? A systematic review. BMJ. 2004;329. https://www.ncbi.nlm.nih.gov/pubmed/15514348. [DOI] [PMC free article] [PubMed]
- 52.Bluestone J, Johnson P, Fullerton J, Carr C, Alderman J, BonTempo J, et al. Effective in-service training design and delivery: evidence from an integrative literature review. Hum Resour Health. 2013;11:51. doi: 10.1186/1478-4491-11-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Raza A, Coomarasamy A, Khan KS. Best evidence continuous medical education. Arch Gynecol Obstet. 2009;280:683–687. doi: 10.1007/s00404-009-1128-7. [DOI] [PubMed] [Google Scholar]
- 54.Kerfoot BP, Kearney MC, Connelly D, Ritchey ML. Interactive spaced education to assess and improve knowledge of clinical practice guidelines. Ann Surg. 2009;249:744–749. doi: 10.1097/SLA.0b013e31819f6db8. [DOI] [PubMed] [Google Scholar]
- 55.Shadish W, Cook T, Campbell D. Experiments and general causal inferences. In: Experiment and quasi-experimental designs for generalized causal inferences. New York; 2002. http://impact.cgiar.org/pdf/147.pdf. Accessed 22 May 2017.
- 56.Schilling K, Applegate R. Best methods for evaluating educational impact: a comparison of the efficacy of commonly used measures of library instruction. J Med Libr Assoc. 2012;100:258–269. doi: 10.3163/1536-5050.100.4.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bhandari A, Wagner T. Self-reported utilization of health care services: improving measurement and accuracy. Med Care Res Rev. 2006;63:217–235. doi: 10.1177/1077558705285298. [DOI] [PubMed] [Google Scholar]
- 58.West M, Armit K, Loewenthal L, Eckert R, West T, Lee A. Leadership and Leadership Development in Health Care. London; 2015. https://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/leadership-leadership-development-health-care-feb-2015.pdf. Accessed 24 May 2017.
- 59.Kluger AN, DeNisi A. The effects of feedback interventions on performance: a historical review, a meta-analysis, and a preliminary feedback intervention theory. Psychol Bull. 1996;119:254–284. doi: 10.1037/0033-2909.119.2.254. [DOI] [Google Scholar]
- 60.Seifert CF, Yukl G, Mcdonald RA. Effects of multisource feedback and a feedback facilitator on the influence behavior of managers toward subordinates. J Appl Psychol. 2003;88:561–569. doi: 10.1037/0021-9010.88.3.561. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.