Abstract
Objective
To examine whether previous observed inverse associations of dairy intake with systolic blood pressure and risk of hypertension were causal.
Design
Mendelian randomization study using the single nucleotide polymorphism rs4988235 related to lactase persistence as an instrumental variable.
Setting
CHARGE (Cohorts for Heart and Aging Research in Genomic Epidemiology) Consortium.
Participants
Data from 22 studies with 171 213 participants, and an additional 10 published prospective studies with 26 119 participants included in the observational analysis.
Main outcome measures
The instrumental variable estimation was conducted using the ratio of coefficients approach. Using meta-analysis, an additional eight published randomized clinical trials on the association of dairy consumption with systolic blood pressure were summarized.
Results
Compared with the CC genotype (CC is associated with complete lactase deficiency), the CT/TT genotype (TT is associated with lactose persistence, and CT is associated with certain lactase deficiency) of LCT-13910 (lactase persistence gene) rs4988235 was associated with higher dairy consumption (0.23 (about 55 g/day), 95% confidence interval 0.17 to 0.29) serving/day; P<0.001) and was not associated with systolic blood pressure (0.31, 95% confidence interval −0.05 to 0.68 mm Hg; P=0.09) or risk of hypertension (odds ratio 1.01, 95% confidence interval 0.97 to 1.05; P=0.27). Using LCT-13910 rs4988235 as the instrumental variable, genetically determined dairy consumption was not associated with systolic blood pressure (β=1.35, 95% confidence interval −0.28 to 2.97 mm Hg for each serving/day) or risk of hypertension (odds ratio 1.04, 0.88 to 1.24). Moreover, meta-analysis of the published clinical trials showed that higher dairy intake has no significant effect on change in systolic blood pressure for interventions over one month to 12 months (intervention compared with control groups: β=−0.21, 95% confidence interval −0.98 to 0.57 mm Hg). In observational analysis, each serving/day increase in dairy consumption was associated with −0.11 (95% confidence interval −0.20 to −0.02 mm Hg; P=0.02) lower systolic blood pressure but not risk of hypertension (odds ratio 0.98, 0.97 to 1.00; P=0.11).
Conclusion
The weak inverse association between dairy intake and systolic blood pressure in observational studies was not supported by a comprehensive instrumental variable analysis and systematic review of existing clinical trials.
Introduction
Raised blood pressure is an important risk factor for cardiovascular disease and has been the top single contributor to the global burden of morbidity and mortality, leading to 9.4 million deaths each year.1 In clinical trials, lowering blood pressure has been shown to be effective in reducing the incidence of cardiovascular disease.2 Each 5 mm Hg reduction in blood pressure is associated with a 20% lower risk of coronary heart disease and a 29% lower risk of stroke.3
Maintaining a healthy diet is critical for the prevention of hypertension4; whether dairy products should be incorporated into such a diet is, however, controversial. In epidemiological studies, the association of dairy consumption with blood pressure has been inconsistent. Several observational studies have reported inverse associations of dairy consumption with systolic blood pressure and risk of hypertension5 6 7; however, such associations were not observed in other studies.8 9 10 Two meta-analyses of prospective cohort studies consistently indicated that dairy consumption was associated with lower systolic blood pressure and lower risk of hypertension.11 12 Owing to the observational nature of the studies included, the reported associations might not indicate causality.
In recent years, Mendelian randomization analysis has been widely used to assess potential causal estimates of various risk factors with health outcomes. This approach has the advantage over traditional observational studies of minimizing confounding by using genetic markers as instrumental variables of environmental risk factors. An SNP (single nucleotide polymorphism) rs4988235 upstream from the lactase persistence gene (LCT-13910) has been consistently related to dairy intake in multiple populations,13 14 representing a strong instrumental variable for analyzing the causal relation between dairy intake and disease risk.
In this study, using data collected from 32 studies with 197 332 participants, we performed an instrumental variable analysis to examine the possible causal effect of dairy consumption on systolic blood pressure and risk of hypertension. In addition we conducted a meta-analysis to summarize the results of eight randomized clinical trials assessing dairy intake intervention on changes in systolic blood pressure.
Methods
Study design and population
We used an instrumental variable approach to examine associations of dairy consumption with systolic blood pressure and risk of hypertension. We collected data from 22 observational studies with 171 213 participants within the CHARGE (Cohorts for Heart and Aging Research in Genomic Epidemiology) Consortium. All participants provided written informed consent. The web appendix describes the studies in the analysis.
To provide comprehensive evidence on associations of dairy intake with systolic blood pressure and risk of hypertension, we conducted a systematic review of previously published cohort studies and randomized clinical trials. In the web appendix, we describe the process of the systematic review in detail.
Dairy consumption
Dairy products included skim/low fat milk, whole milk, ice cream, yogurt, cottage/ricotta cheese, cream cheese, other cheese, and cream. In most of the studies, dairy intake was self reported by food frequency questionnaire. We calculated total dairy consumption as the sum of all dairy categories (see table 1 in the web appendix for a detailed description of dairy consumption in the included studies).
Outcome measures
The outcome of our Mendelian randomization included systolic blood pressure and risk of hypertension. Given that systolic blood pressure is superior to diastolic blood pressure as a major risk factor of cardiovascular disease, we used systolic blood pressure as the main outcome in our analysis (see table 1 in the web appendix for the detailed measurement of systolic blood pressure in the included studies). For participants taking antihypertensive drugs, we added 15 mm Hg to systolic blood pressure to adjust for treatment effects.15 16 17 Hypertension was defined as a systolic blood pressure of 140 mm Hg or higher or current use of antihypertensive drugs.
SNP rs4988235
Table 1 in the web appendix shows genotyping platforms, genotype frequencies, Hardy-Weinberg equilibrium P values, and call rates for lactase persistence SNP rs4988235. The SNP rs4988235 was not genotyped or imputed in two studies; proxy SNPs (rs309137: r2=0.77; rs1446585: r2=1.00) were used instead.
Statistical analyses
We initially conducted statistical analyses within each included study in accordance with a standard analysis plan. As lactase persistence is inherited as a dominant trait,3 we used dominant models (CC v CT/TT genotype) to examine associations of LCT-13910 rs4988235 with dairy intake, systolic blood pressure, and risk of hypertension adjusting for baseline age, sex, ethnicity, and region. We examined associations of dairy consumption with systolic blood pressure and risk of hypertension using linear or logistic models adjusting for baseline age, body mass index, blood pressure, smoking status, physical activity, total energy intake, alcohol consumption, sex, ethnicity, region, and years of follow-up. For results collected from all studies using linear or logistic models, we combined results across studies using random effects models. We meta-analyzed the results of observed associations of dairy intake with systolic blood pressure and risk of hypertension within the CHARGE Consortium with results extracted from published cohort studies. The effect of dairy intake on systolic blood pressure from published randomized clinical trials was also meta-analyzed using a random effects model. Statistical heterogeneity across studies was assessed by Cochrane Q test, with P<0.1 indicating significant between study heterogeneity. In addition, we calculated the I2 statistic to evaluate the percentage of heterogeneity that was due to between study variation.18
After pooling the association between LCT-13910 rs4988235 and dairy intake across studies by meta-analysis, we quantified the strength of the single SNP as an instrumental variable by Z statistic and P value of the pooled effect estimate. We considered LCT-13910 rs4988235 a strong instrumental variable if the Z statistic was more than 3.2 or the P value was less than 0.0016, which was equivalent to an F statistic greater than 10.19 20 We used the instrumental variable ratio method to estimate the possible causal relation of dairy consumption with systolic blood pressure and risk of hypertension. The instrumental variable estimate was calculated as the ratio of the association of the instrumental variable with outcome to the association of the exposure with outcome. We estimated the variance of the instrumental variable ratio using first order Taylor expansion.21
We further conducted stratified analysis on the causal estimates of dairy intake with systolic blood pressure and risk of hypertension by frequency of CC alleles (≤12%, >12%), region or country (northern Europe, southern Europe, US), race (white, other), study design (cross sectional, prospective), and measurement of systolic blood pressure (self reported, clinical). We used metaregression to evaluate effect modification by each study level characteristics. In sensitivity analyses, we applied instrumental variable analysis within each study and combined the instrumental variable estimates through meta-analysis; we repeated our analyses using additive (we assumed 0, 1, and 2 for TT, CT, and CC alleles) and recessive models (CC/CT v TT). We conducted restriction analyses by excluding studies that used proxy SNPs, studies that used LCT-13910 rs4988235 in Hardy-Weinberg disequilibrium, or studies where LCT-13910 rs4988235 was not statistically significantly associated with higher dairy intake.
All meta-analyses were conducted at Harvard TH Chan School of Public Health using Stata version 11.2 (STATA Corp, College Station, TX).
Patient involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in developing plans for design or implementation of the study. No patients were asked to advise on interpretation or writing up of results. There are no plans to disseminate the results of the research to study participants or the relevant patient community.
Results
We included 22 studies with 171 213 participants from the CHARGE (Cohorts for Heart and Aging Research in Genomic Epidemiology) Consortium. Table 1 shows the baseline characteristics of the studies. Of the 22 studies, nine were conducted in the US, nine in countries in northern Europe, three in countries in southern Europe, and one in Australia. The frequency of CC alleles varied across studies. In most of the studies, participants were white, and dairy intake was assessed prospectively before measuring systolic blood pressure.
Table 1.
Baseline characteristics of included cohorts
| Study name | Ethnicity | Country | No of participants | Follow-up (years) | Men (%) | Age (years) | SBP (mm Hg) | Hypertension (%) | Antihypertensive drugs (%) | rs4988235 frequency (%) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CC | CT | TT | ||||||||||
| CGPS | White | Denmark | 74 219 | 0 | 45 | 57 | 140 | 20 | 20 | 6 | 36 | 58 |
| WGHS | White | USA | 19 743 | 4 | 0 | 54 | 126 | 13 | 13 | 11 | 38 | 51 |
| GESUS | White | Denmark | 14 815 | 0 | 46 | 57 | 142 | 10 | 23 | 6 | 36 | 58 |
| NHS | White | USA | 11 287 | 26 | 0 | 53 | NA | 9 | NA | 14 | 41 | 45 |
| ARIC (white) | White | USA | 8233 | 6 | 47 | 54 | 118 | 29 | 19 | 9* | 39* | 52* |
| ARIC (African-American) | African | USA | 1889 | 6 | 36 | 53 | 127 | 55 | 41 | 74* | 25* | 2* |
| HPFS | White | USA | 6914 | 24 | 100 | 55 | NA | 22 | NA | 18 | 39 | 43 |
| INTER99 | White | Denmark | 6514 | 5 | 49 | 46 | 130 | 31 | 7 | 6 | 36 | 57 |
| D.E.S.I.R. | White | France | 3378 | 9 | 50 | 47 | 131 | 35 | 9 | 22 | 49 | 30 |
| Rotterdam Study | White | Netherlands | 3215 | 7 | 41 | 66 | 136 | 54 | 27 | 9 | 39 | 52 |
| MDCS | White | Sweden | 3199 | 17 | 40 | 56 | 139 | 53 | 14 | 6† | 33† | 61† |
| GLACIER | White | Sweden | 2763 | 10 | 37 | 45 | 124 | 19 | 4 | 7 | 36 | 58 |
| MESA | Mixed | USA | 2424 | 10 | 47 | 61 | 132 | 35 | 28 | 20 | 49 | 30 |
| FamHS | White | USA | 2167 | 8 | 45 | 51 | 127 | 44 | 36 | 12 | 42 | 46 |
| CHS | White | USA | 1964 | 9 | 38 | 71 | 133 | 49 | 35 | 4 | 43 | 53 |
| YFS | White | Finland | 1370 | 0 | 43 | 38 | 120 | 9 | 7 | 15 | 47 | 38 |
| DCH Study‡ | White | Denmark | 1297 | 0 | 45 | 56 | 135 | 47 | 13 | 5 | 32 | 63 |
| DIOGENES‡ (controls) | White | Denmark | 1002 | 0 | 51 | 54 | 135 | 38 | 7 | 6 | 36 | 58 |
| DIOGENES‡ (weight gainers) | White | Denmark | 813 | 0 | 49 | 53 | 135 | 42 | 10 | 5 | 35 | 60 |
| PREDIMED-VALENCIA | White | Spain | 940 | 2 | 36 | 67 | 147 | 84 | 63 | 38 | 46 | 16 |
| BPRHS | Puerto Rican | USA | 845 | 0 | 28 | 57 | 136 | 78 | 56 | 61 | 34 | 5 |
| GOLDN | White | USA | 818 | 0 | 50 | 49 | 118 | 26 | 21 | 10 | 40 | 50 |
| Raine | Mixed§ | Australia | 728 | 2 | 48 | 20 | 117 | 4 | 0 | 15 | 39 | 46 |
| InCHIANTI | White | Italy | 647 | 0 | 45 | 64 | 142 | 64 | 49 | 2 | 30 | 68 |
See web appendix for full titles of studies.
SBP=systolic blood pressure.
rs1446585 used as a proxy.
rs309137 used as a proxy.
Subsamples from Danish Diet, Cancer and Health cohort.
Dominantly white, white-admixed (participants with one or both white parents).
By conducting a systematic review, we additionally identified 10 published cohort studies with 26 119 participants and eight randomized clinical trials with 735 participants. Figure 1 in the web appendix shows the flowchart of study selection. The clinical trials examined the effect of dairy intake on systolic blood pressure over one month to 12 months of interventions.22 23 24 25 26 27 28 29 In the cohort studies, seven assessed systolic blood pressure as the outcome5 6 7 8 9 10 30 31 and five used hypertension as the outcome.5 30 31 32 33 Tables 2 and 3 in the web appendix show the characteristics of the published trials and cohorts.
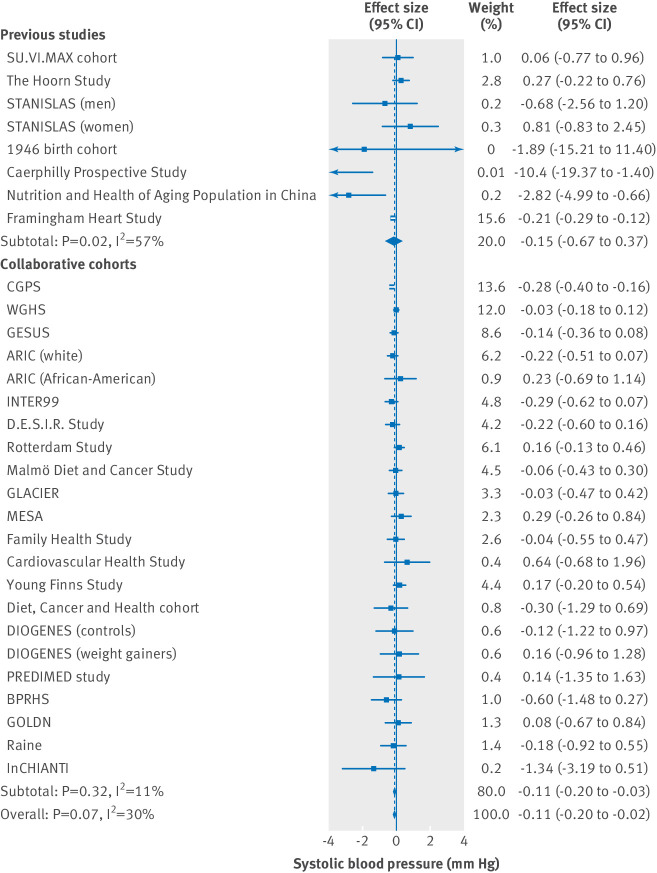
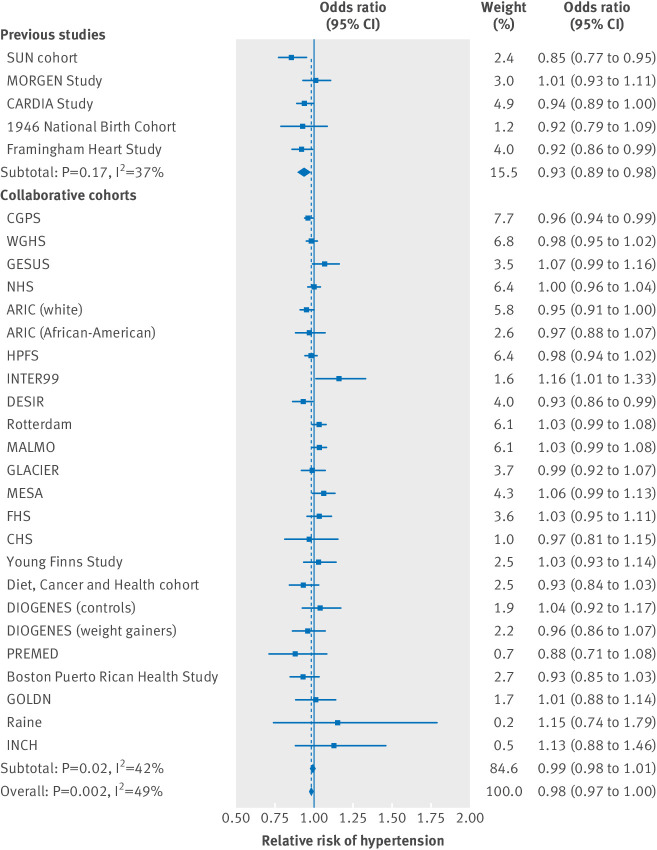
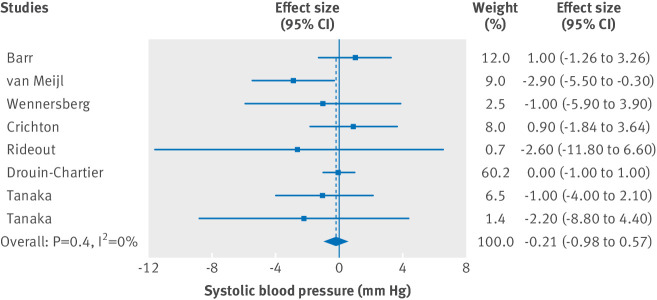
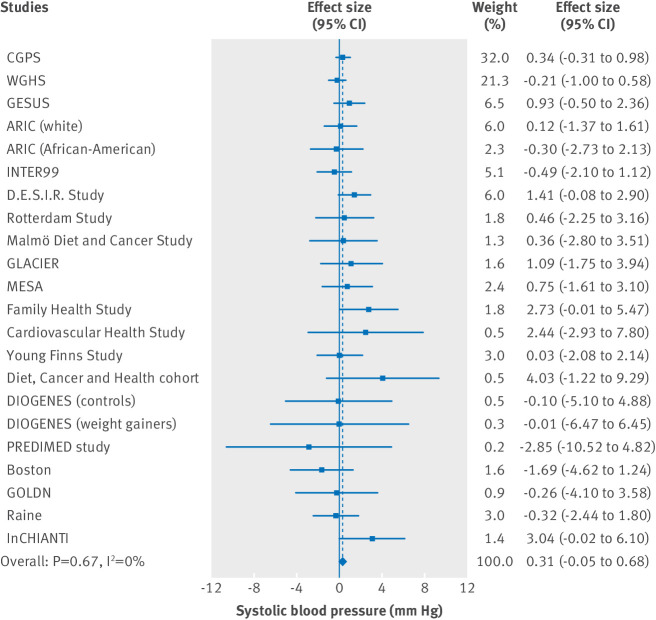
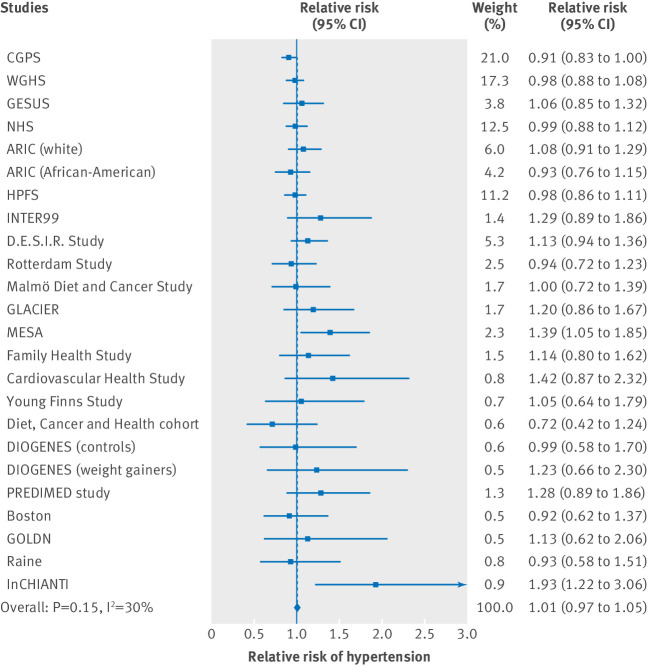
In observational analysis, each serving/day increase in dairy consumption was associated with lower systolic blood pressure (β=−0.11, 95% confidence interval −0.20 to −0.02 mm Hg; P=0.02) and was not associated with a lower relative risk of hypertension (odds ratio 0.98, 95% confidence interval 0.97 to 1.00; P=0.11) (figs 1 and 2). In the randomized clinical trials, however, dairy intake did not show a significant effect on changes in systolic blood pressure over one month to 12 months of interventions (comparing intervention with control group: β=−0.21, −0.98 to 0.57 mm Hg; P=0.60) (fig 3). No publication bias of included cohorts and clinical trials was found (systolic blood pressure in cohorts: Egger’s test P=0.51; hypertension in cohorts: P=0.46; randomized clinical trials: P=0.33) (fig 2 in the web appendix).
Fig 1.
Association of baseline dairy consumption (serving/day) with systolic blood pressure in observational cohort studies. Linear regression was used in collaborative cohorts adjusted for sex, ethnicity, region or country, and years of follow-up, as well as for age, body mass index, blood pressure/hypertension, smoking status, physical activity, total energy intake, and alcohol consumption at baseline
Fig 2.
Association of baseline dairy consumption (serving/day) with relative risk of hypertension in observational cohort studies. Logistic regression was used in collaborative cohorts adjusted for sex, ethnicity, region or country, and years of follow-up, as well as for age, body mass index, blood pressure/hypertension, smoking status, physical activity, total energy intake, and alcohol consumption at baseline
Fig 3.
Association of baseline dairy consumption (serving/day) with systolic blood pressure in randomized clinical trials
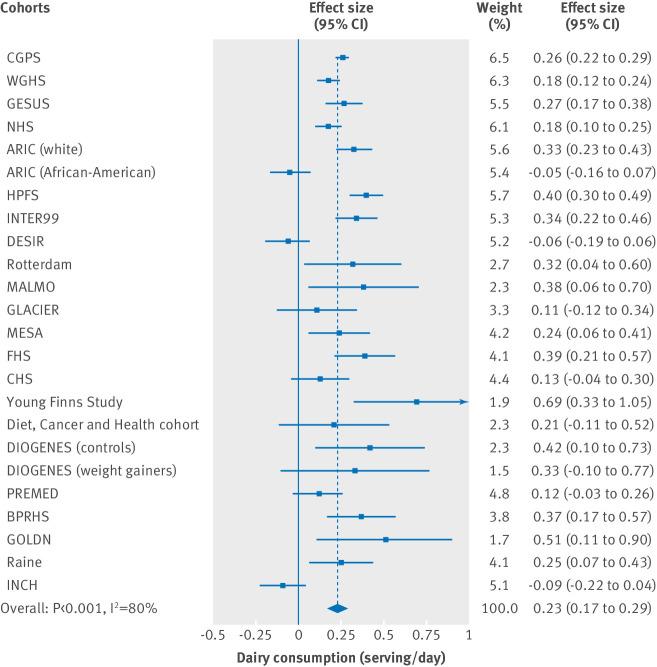
Compared with the CC genotype, the CT/TT genotype of LCT-13910 rs4988235 was associated with higher dairy consumption (0.23 (95% confidence interval 0.17 to 0.29) serving/day (about 55 g/day); P<0.001), and the Z statistic was 7.51, showing that the instrumental variable was strong and valid (fig 4). However, significant heterogeneity was found across studies (I2=80.0%; P<0.001 for heterogeneity). Compared with the CC genotype, the CT/TT genotype of LCT-13910 rs4988235 was not associated with systolic blood pressure (0.31, −0.05 to 0.68 mm Hg; P=0.09) or risk of hypertension (odds ratio 1.01, 95% confidence interval 0.97 to 1.05; P=0.27) (figs 5 and 6). Using LCT-13910 rs4988235 as the instrumental variable, we estimated that genetically determined dairy consumption was not associated with systolic blood pressure (β=1.35, 95% confidence interval −0.28 to 2.97 mm Hg for each serving/day) or risk of hypertension (odds ratio 1.04, 0.88 to 1.24).
Fig 4.
Association of SNP rs4988235 with dairy consumption using dominant model (CT/TT v CC genotype). Linear regression adjusted for baseline age, sex, ethnicity, and region or country
Fig 5.
Association of SNP rs4988235 with systolic blood pressure using dominant model (CT/TT v CC genotype). Linear regression adjusted for baseline age, sex, ethnicity, and region or country
Fig 6.
Association of SNP rs4988235 with relative risk of hypertension using dominant model (CT/TT v CC genotype). Logistic regression adjusted for baseline age, sex, ethnicity, and region or country
To explore sources of heterogeneity in the association of LCT-13910 rs4988235 with dairy intake, we conducted stratified analyses by region or country, frequency of the CC genotype, race, study design, and measurement of systolic blood pressure. We classified Denmark, the Netherlands, Sweden, and Finland as northern European countries and Italy, Spain, and France as southern European countries. Among studies with a CC genotype frequency of 12% or less, or studies conducted in northern European countries, we found no heterogeneity of LCT-13910 rs4988235 with dairy intake, and the instrumental variable remained strong in both subgroups. Genetically determined dairy consumption was unrelated to systolic blood pressure and risk of hypertension within each stratum, which was consistent with the main finding (table 2). No effect modification on causal estimates was found by CC frequency, region or country, race, study design, and systolic blood pressure measurement.
Table 2.
Stratified analysis on causal estimates of dairy consumption (serving/day) with systolic blood pressure (mm Hg) and risk of hypertension (odds ratio). Values in brackets are 95% confidence intervals unless stated otherwise
| Variables | No of observations | Instrumental variable | SBP | Hypertension | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| SNP rs4988235 with dairy intake | Z statistic (P value) | I2 (%) (P value) | SNP rs4988235 with SBP | Dairy intake with SBP, instrumental variable estimation | SNP rs4988235 with risk of hypertension | Dairy intake with risk of hypertension, instrumental variable estimation | ||||
| CC genotype frequency *: | ||||||||||
| ≤12% | 14 | 0.27 (0.22 to 0.31) | 11.64 (<0.001) | 34.4 (0.10) | 0.27 (−0.14 to 0.67) | 1.00 (−0.51 to 2.51) | 0.99 (0.93 to 1.04) | 0.96 (0.78 to 1.19) | ||
| >12% | 9 | 0.21 (0.08 to 0.34) | 3.26 (0.001) | 87.4 (<0.001) | 0.30 (−0.55 to 1.15) | 1.43 (−2.71 to 5.57) | 1.03 (0.95 to 1.11) | 1.15 (0.79 to 1.68) | ||
| Region or country†: | ||||||||||
| Northern Europe | 10 | 0.28 (0.23 to 0.33) | 11.11 (<0.001) | 10.5 (0.31) | 0.37 (−0.13 to 0.87) | 1.32 (−0.48 to 3.12) | 0.96 (0.89 to 1.03) | 0.86 (0.67 to 1.12) | ||
| Southern Europe | 3 | −0.01 (−0.14 to 0.11) | 0.22 (0.83) | 5.2 (0.08) | NA | NA | NA | NA | ||
| USA | 10 | 0.25 (0.16 to 0.34) | 5.32 (<0.001) | 51.5 (<0.001) | 0.01 (−0.59 to 0.62) | 0.04 (−2.38 to 2.46) | 1.01 (0.96 to 1.07) | 1.04 (0.84 to 1.29) | ||
| Race: | ||||||||||
| White | 20 | 0.23 (0.17 to 0.30) | 7.22 (<0.001) | 78.8 (<0.001) | 0.31 (−0.09 to 0.70) | 1.35 (−0.41 to 3.11) | 1.03 (0.97 to 1.09) | 1.14 (0.88 to 1.47) | ||
| Other | 4 | 0.20 (0.01 to 0.39) | 2.05 (0.04) | 86.4 (<0.001) | 0.36 (−0.67 to 1.38) | 1.80 (−3.60 to 7.20) | 1.06 (0.89 to 1.27) | 1.34 (0.53 to 3.40) | ||
| Study design: | ||||||||||
| Cross sectional | 9 | 0.28 (0.16 to 0.40) | 4.51 (<0.001) | 73.7 (<0.001) | 0.36 (−0.01 to 0.73) | 1.29 (−0.15 to 2.72) | 1.03 (0.88 to 1.20) | 0.96 (0.75 to 1.24) | ||
| Cohort | 15 | 0.21 (0.13 to 0.29) | 5.41 (<0.001) | 36.8 (<0.001) | 0.09 (−0.14 to 0.32) | 0.43 (−0.68 to 1.54) | 1.03 (0.98 to 1.09) | 1.10 (0.95 to 1.27) | ||
| SBP measurement: | ||||||||||
| Self reported | 5 | 0.25 (0.15 to 0.34) | 5.23 (<0.001) | 17.0 (0.002) | −0.14 (−0.84 to 0.57) | −0.56 (−3.39 to 2.27) | 1.01 (0.93 to 1.09) | 1.04 (0.85 to 1.27) | ||
| Clinical | 19 | 0.23 (0.15 to 0.31) | 5.60 (<0.001) | 97.8 (<0.001) | 0.48 (0.05 to 0.90) | 2.09 (0.10 to 4.07) | 1.05 (0.98 to 1.14) | 1.04 (0.90 to 1.21) | ||
SNP=single nucleotide polymorphism; SBP=systolic blood pressure; NA=not available.
InCHIANTI was excluded owing to an extremely low CC frequency of 2%.
Raine study was not included as it was conducted in Australia.
In sensitivity analyses, we applied the instrumental variable analysis within each study and combined the instrumental variable estimates using meta-analysis. The results were consistent with the main findings (fig 3 in the web appendix). We examined the associations of dairy consumption with systolic blood pressure and risk of hypertension by modeling the LCT-13910 genotype in recessive and additive inheritance manner (figs 4 and 5 in the web appendix). Genetically determined dairy consumption was not associated with systolic blood pressure or risk of hypertension using the recessive model, and it was weakly associated with higher systolic blood pressure using the additive model (table 4 in the web appendix).
In restriction analysis, the instrumental variable estimates were consistent with the main findings when excluding studies that used proxy SNPs, studies that used LCT-13910 rs4988235 in Hardy-Weinberg disequilibrium, or studies where LCT-13910 rs4988235 was not statistically significantly associated with higher dairy intake using dominant models.
Discussion
In this study, using Mendelian randomization analysis in 32 studies (22 observational studies, 10 previously published cohort studies) with 197 332 participants, we examined the potential causal effect of dairy consumption on systolic blood pressure and risk of hypertension. Using the LCT-13910 gene variant affecting lactase persistence as the instrumental variable, our study showed that genetically determined dairy intake did not affect systolic blood pressure or risk of hypertension. Furthermore, a meta-analysis of the results from published randomized clinical trials showed that dairy consumption had no effect on changes of systolic blood pressure in response to interventions over one month to 12 months.
Strengths and weaknesses of this study
Our study has several strengths. First, we carried out a large instrumental variable analysis on the causality of dairy intake on systolic blood pressure and hypertension. The large sample size provided us with enough power to estimate the causal effect of dairy intake on systolic blood pressure. Second, the single nucleotide polymorphism (SNP) rs4988235 for lactase persistence is a well established variant associated with dairy intake, with a solid biological basis, and is therefore a highly valid instrumental variable. Third, we summarized published randomized clinical trials on dairy consumption with systolic blood pressure. Although clinical trials have shorter follow-up time than cohort studies, they still provided further supportive evidence to the instrumental variable results.
Our study has several limitations. First, given the variability of the CC allele across studies and the different prevalence of hypertension across countries, population stratification might exist. However, as most of the studies included were genetically homogeneous, we performed instrumental variable analysis within each study first and combined the instrumental variable results through meta-analysis. The instrumental variable results were consistent with the main findings. Second, the pleiotropic effect of SNP rs4988235 is not known. However, SNP rs4988235 was located in the MCM6 gene upstream from LCT-13910, and neither gene has been found to have additional biological function besides lactase persistence.13 Third, dairy consumption was self reported by questionnaire and might be affected by measurement errors. If measurement errors were random, the observed associations would be biased to the null. However, the results for instrumental variable estimates would not be biased, although the confidence interval might be larger. Fourth, we included total dairy intake as the main exposure; however, lactase content differs between dairy products. For example, Swiss cheese and mozzarella contain trivial amounts of lactase. Similar to the measurement error of dairy intake, the variability in lactase content of dairy products might not bias the instrumental variable estimates but might widen the confidence intervals. Fifth, several studies examined dairy consumption and systolic blood pressure using a cross sectional study design, and even if instrumental variable analysis was used this might result in reverse causation. However, no statistically significant effect modification by study design was found in stratified analysis, indicating that reverse causation caused by study design might be minimal.
Strengths and weaknesses in relation to other studies
In our study we observed an inverse association between dairy intake and systolic blood pressure. Consistently, cross sectional studies showed an inverse association between dairy intake and systolic blood pressure.34 35 36 Previous cohort studies have been summarized in two meta-analyses.11 12 One meta-analysis involving approximately 45 000 participants showed that dairy products were associated with lower risks of raised systolic blood pressure.11 In line with this, another meta-analysis, which included nine cohort studies with a sample size of 57 256, found an inverse association between dairy foods and risk of hypertension.12 However, in both meta-analyses, the associations of high fat dairy products, including whole milk, cream, and cream cheese, and low fat dairy products, including skim milk and yogurt with systolic blood pressure were inconsistent. In the two published meta-analyses, the observed inverse association was mainly due to consumption of low fat dairy products.11 12 Furthermore, a meta-analysis summarizing 14 clinical trials found that probiotic fermented milk, including yogurt, resulted in a statistically significant reduction in systolic blood pressure.37 Clinical trials also showed that tripeptides and peptides derived from milk have hypotensive effects in prehypertensive and hypertensive participants.38 39
Possible explanations and implications
Compared with the CC genotype, the CT/TT genotype was associated with 0.23 serving/day (about 55 g/day) higher dairy intake. In previous cohort studies, a 55 g/day increment in dairy intake was estimated to be statistically significantly associated with 0.03 mm Hg lower systolic blood pressure, and 1%, 2%, and 1% lower risks of hypertension,12 type 2 diabetes,40 and cardiovascular disease,41 respectively. However, in our study, the CT/TT genotype was associated with a 0.31 mm Hg higher systolic blood pressure, and genetically determined dairy consumption did not decrease systolic blood pressure or risk of hypertension using instrumental variable estimation. Moreover, the meta-analyzed results of clinical trials showed that dairy intake had no effect on changes in systolic blood pressure. There could be two reasons that the reported associations from observational studies were inconsistent with our instrumental variable results. First, even if yogurt and specific nutrients in dairy such as milk peptides have antihypertensive effects, specific dairy products such as yogurt only compose a small fraction of total dairy products and could not explain the general observational association between dairy intake and outcome. Second, higher low fat dairy intake was more likely to be associated with a healthy diet and lifestyle.42 Therefore, the observed inverse association of particularly low fat dairy intake with systolic blood pressure might be due to confounding of intake of other food items and a healthy lifestyle. However, as one fundamental assumption for the instrumental variable to be valid is that the instrumental variable is associated with the outcome only through the exposure under study,43 we could not separate the effect of individual dairy products in our study to further explain the inconsistency between observational and instrumental results using the current instrumental variable. And it is difficult to find a specific instrumental variable for each dairy product.
To tackle the heterogeneity of the association between SNP rs4988235 and dairy intake across studies, we conducted stratified analysis by CC frequency and region or country. SNP rs4988235 was consistently associated with higher dairy intake across subgroups, showing the robustness of our instrumental variable. No heterogeneity was found among studies conducted in northern Europe or among studies with a CC frequency of 12% or less, perhaps because these populations consume a relatively high amount of dairy products,44 and SNP rs4988235 was found to be associated completely with lactase persistence in north Europeans.13 No associations of genetically determined dairy intake with systolic blood pressure and risk of hypertension were found in both subgroups, which were consistent with our main finding.
Conclusion
The weak inverse association between dairy intake and systolic blood pressure in observational studies was not supported by our comprehensive instrumental variable analysis and systematic review of existing clinical trials.
What is already known on this topic
Observational studies showed that dairy intake was associated with lower systolic blood pressure and lower risk of hypertension
What this study adds
Using a Mendelian randomization approach, we found that genetically determined dairy consumption was not associated with systolic blood pressure or risk of hypertension
Acknowledgments
Members of the CHARGE Consortium:
Alexis C Frazier-Wood, assistant professor,1 Stella Aslibekyan, assistant professor,2 Kari E North, professor,3 4 Trudy Voortman, research fellow,5 Mariaelisa Graff, research assistant professor,3 Caren E Smith, scientist,6 Chao-Qiang Lai, research geneticist,6 Anette Varbo, doctoral student, assistant professor,7 8 Rozenn N Lemaitre, research associate professor,9 Ester AL de Jonge, research fellow,5 10 Frédéric Fumeron, associate professor,11 12 13 14 Dolores Corella, professor,15 16 Carol A Wang, research officer,17 Anne Tjønneland, research leader,18 Kim Overvad, professor,19 20 Thorkild IA Sørensen, professor,21 22 Mary F Feitosa, associate professor,23 Mary K Wojczynski, assistant professor,23 Mika Kähönen, professor,24 25 Shafqat Ahmad, research fellow,26 27 Frida Renström, research fellow,27 28 Bruce M Psaty, professor,9 14 29 30 David S Siscovick, professor,31 Inês Barroso, senior group leader,32 33 34 Ingegerd Johansson, professor,35 Dena Hernandez, biologist,36 Luigi Ferrucci, scientific director,37 Stefania Bandinelli, geriatrician,38 Allan Linneberg, professor,39 40 Camilla Helene Sandholt, research fellow,21 Oluf Pedersen, professor,21 41 Torben Hansen, professor,21 42 Christina-Alexandra Schulz, doctoral student,43 Emily Sonestedt, associate professor,43 Marju Orho-Melander, professor,43 Tzu-An Chen, senior statistician,1 Jerome I Rotter, professor,44 Mathew A Allison, professor,45 Stephen S Rich, professor,46 Jose V Sorlí, professor,15 16 Oscar Coltell, professor,16 47 Craig E Pennell, professor,17 Peter R Eastwood, professor,48 Albert Hofman, professor,5 49 Andre G Uitterlinden, professor,10 MCarola Zillikens, associate professor,10 Frank JA van Rooij, research associate,5 Audrey Y Chu, research fellow,50 Lynda M Rose, associate professor,50 Paul M Ridker, professor,50 51 Jorma Viikari, professor,52 53 Olli Raitakari, project coordinator professor,54 55 Terho Lehtimäki, professor,56 57 Vera Mikkilä, associate professor,55 58 Walter C Willett, professor,26 49 59 Yujie Wang, biostatistician,3 Katherine L Tucker, professor,60 Jose M Ordovas, senior scientist,6 61 62 Tuomas O Kilpeläinen, associate professor,21 Michael A Province, professor,23 Paul W Franks, professor,26 27 63 Donna K Arnett, professor,2 Toshiko Tanaka, staff scientist,37 Ulla Toft, associate professor,39 Ulrika Ericson, associate researcher,43 Oscar H Franco, professor,5 CHARGE consortium, Dariush Mozaffarian, professor,64 Frank B Hu, professor,26 49 59 Daniel I Chasman, associate professor,50 65 66
1. USDA/ARS Children's Nutrition Research Center, Baylor College of Medicine, Houston, TX, USA; 2. Department of Epidemiology, University of Alabama at Birmingham, Birmingham, AL, USA; 3. Department of Epidemiology, University of North Carolina, Chapel Hill, NC, USA; 4. Carolina Center for Genome, Sciences University of North Carolina, Chapel Hill, NC, USA; 5. Department of Epidemiology Erasmus MC, University Medical Center, Rotterdam, Netherlands; 6. Jean Mayer USDA Human Nutrition Research Center on Aging, Tufts University Boston, MA, USA; 7. Faculty of Health and Medical Sciences, University of Copenhagen, Denmark; 8. Department of Clinical Biochemistry and the Copenhagen General Population Study, Herlev and Gentofte Hospital, Copenhagen University Hospital, Denmark; 9. Department of Medicine, University of Washington, WA, USA; 10. Department of Internal Medicine Erasmus MC, University Medical Center, Rotterdam, Netherlands; 11. INSERM UMR_S 1138, Centre de Recherche des Cordeliers, Paris, France; 12. Univ Paris Diderot Sorbonne Paris Cité, UMR_S 1138, Centre de Recherche des Cordeliers, Paris, France; 13. Sorbonne Universités UPMC Univ Paris 06, UMR_S 1138, Centre de Recherche des Cordeliers, Paris, France; 14. Université Paris Descartes, Sorbonne Paris Cité, UMR_S 1138, Centre de Recherche des Cordeliers, Paris; 15. Department of Preventive Medicine and Public Health, University of Valencia, Valencia, Spain; 16. CIBER Fisiopatología de la Obesidad y Nutrición, Instituto de Salud Carlos III, Madrid, Spain; 17. School of Women’s and Infants’ Health, University of Western Australia, Australia; 18. Danish Cancer Society Research Center, Copenhagen, Denmark; 19. Department of Public Health, Section for Epidemiology, Aarhus University, Aarhus C, Denmark; 20. Department of Cardiology, Aalborg University Hospital, Aalborg, Denmark; 21. Novo Nordisk Foundation Center for Basic Metabolic Research, Section of Metabolic Genetics, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark; 22. Institute of Preventive Medicine Bispebjerg and Frederiksberg Hospitals, The Capital Region, Copenhagen, Denmark; 23. Department of Genetics Washington University School of Medicine, Saint Louis, MO, USA; 24. Department of Clinical Physiology, Tampere University Hospital, Finland; 25. Department of Clinical Physiology, University of Tampere School of Medicine, Finland; 26. Department of Nutrition, Harvard School of Public Health, Boston, MA, USA; 27. Department of Clinical Sciences, Genetic and Molecular Epidemiology Unit, Lund University, Malmö, Sweden; 28. Department of Biobank Research, Umeå University, Umeå, Sweden; 29. Department of Epidemiology, University of Washington, WA, USA; 30. Department of Health Sciences, University of Washington, WA, USA; 31. New York Academy of Medicine, New York, NY, USA; 32. Wellcome Trust Sanger Institute, Wellcome Trust Genome Campus, Hinxton, Cambridge, UK; 33. NIHR Cambridge Biomedical Research Centre, Institute of Metabolic Science, Addenbrooke's Hospital, Cambridge, UK; 34. University of Cambridge, Metabolic Research Laboratories Institute of Metabolic Science, Addenbrooke’s Hospital, Cambridge, UK; 35. Department of Biobank Research, Umeå University, Umeå, Sweden; 36. Laboratory of Neurogenetics National Institute on Aging, Bethesda MD, USA; 37. Translational Gerontology Branch, Baltimore, MD, USA; 38. Geriatric Unit, Local Health Tuscany Center (LHTC), Florence, Italy; 39. Research Centre for Prevention and Health, the Capital Region of Denmark, Copenhagen, Denmark; 40. Department of Clinical Experimental Research Rigshospitalet, Glostrup, Denmark; 41. Faculty of Health Sciences, University of Aarhus, Aarhus, Denmark; 42. Faculty of Health Sciences, University of Southern Denmark, Odense, Denmark; 43. Department of Clinical Sciences in Malmö, Lund University, Sweden; 44. Institute for Translational Genomics and Population Sciences, Los Angeles Biomedical Research Institute and Department of Pediatrics at Harbor-UCLA Medical Center, Torrance, CA, USA; 45. Division of Preventive Medicine, Department of Family Medicine and Public Health, University of California San Diego, La Jolla, CA, USA; 46. Center for Public Health Genomics, 3232 West Complex, University of Virginia, Charlottesville, VA, USA; 47. Department of Computer Languages and Systems, University Jaume I, Castellon, Spain; 48. Centre for Sleep Science, School of Anatomy Physiology and Human Biology, University of Western Australia, Australia; 49. Department of Epidemiology, Harvard School of Public Health, Boston, MA, USA; 50. Division of Preventive Medicine, Brigham and Women’s Hospital and Harvard Medical School, Boston, MA USA; 51. Division of Cardiovascular Medicine, Brigham and Women's Hospital and Harvard Medical Schoo, Boston, MA, USA; 52. Division of Medicine, Turku University Hospital, Finland; 53. Department of Medicine, University of Turku, Finland; 54. Department of Clinical Physiology and Nuclear Medicine, Turku University Hospital, Finland; 55. Research Centre of Applied and Preventive Cardiovascular Medicine, University of Turku, Finland; 56. Department of Clinical Chemistry Fimlab Laboratories, Tampere University Hospital, Finland; 57. Department of Clinical Chemistry, University of Tampere School of Medicine, Finland; 58. Department of Food and Environmental Sciences, University of Helsinki, Finland; 59. Channing Division of Network Medicine, Department of Medicine, Brigham and Women’s Hospital and Harvard Medical School, Boston, MA, USA; 60. Department of Biomedical and Nutritional Sciences, Center for Population Health, University of Massachusetts Lowell, Lowell, MA, USA; 61. Department of Epidemiology and Population Genetics, Centro Nacional Investigación Cardiovasculares, Madrid, Spain; 62. Instituto Madrileño de Estudios Avanzados en Alimentación Madrid, Spain; 63. Department of Public Health and Clinical Medicine Section for Medicine, Umeå University, Umeå, Sweden; 64. Friedman School of Nutrition Science and Policy, Tufts University, Boston, MA, USA; 65. Division of Genetics, Brigham and Women’s Hospital and Harvard Medical School, Boston MA, USA; 66. Broad Institute of MIT and Harvard, Cambridge MA, USA
Web extra.
Extra material supplied by authors
Supplementary appendix: additional information
The authors of the GLACIER Study acknowledge the funding agencies supporting the Northern Sweden Diet Database and the Västerbotten Intervention Project, including the Swedish Research Council. The authors of the YFS gracefully acknowledge the expert technical assistance in the statistical analyses by Ville Aalto, Irina Lisinen, and Mika Helminen. The authors of the Raine study are grateful to the Raine participants and their families, and to the Raine research staff for cohort coordinaion and data collection. This work was supported by resources provided by the Pawsey Supercomputing Centre with funding from the Australian Government and the Government of Western Australia. The authors also gratefully acknowledge the NH&MRC for their long term funding to the study over the past 25 years and also the following institutes for providing funding for core management of the Raine study: University of Western Australia (UWA); Curtin University; Raine Medical Research Foundation; UWA Faculty of Medicine, Dentistry, and Health Sciences; Telethon Kids Institute, Women’s and Infant’s Research Foundation (King Edward Memorial Hospital); and Edith Cowan University. We acknowledge the assistance of the Western Australian DNA Bank (National Health and Medical Research Council of Australia National Enabling Facility); the Raine study participants for their ongoing participation; the Raine study team for study coordination and data collection; the UWA Centre for Science for use of its facility; and the Sleep Study Technicians. The authors of the ARIC study thank the staff and participants for their important contributions. Dr Dolores Corella acknowledges the collaboration of the Real Colegio Complutense at Harvard University, Cambridge. MA, USA.
Contributors: LQ obtained funding from the National Institutes of Health. MD, TH, HKB, CE, and LQ designed the study. MD and TH collected the data. MD, TH, and HKB provided statistical expertise. MD analyzed the data and wrote the first draft of the manuscript. All authors contributed to the interpretation of the results and critical revision of the manuscript for important intellectual content and approved the final version of the manuscript. MD, TH, HKB, BGN, CE, and LQ are the guarantors of this investigation and contribute equally to this work.
Funding: Funding: LQ is recipient of the National Heart, Lung, and Blood Institute (HL071981, HL034594, HL126024), the National Institute of Diabetes and Digestive and Kidney Diseases (DK091718, DK100383, DK078616), the Boston Obesity Nutrition Research Center (DK46200), the United States–Israel Binational Science Foundation grant (2011036), and the American Heart Association Scientist Development Award (0730094N) for the Mendelian randomization study. The CGPS is was funded by the Danish Council for Independent Research; Medical Sciences (FSS); Herlev Hospital, Copenhagen University Hospital; Copenhagen County Foundation; and Chief Physician Johan Boserup and Lise Boserup’s Fund, Denmark. The GESUS was funded by the Region Zealand Foundation, Naestved Hospital Foundation. Edith and Henrik Henriksens Memorial Scholarship, Johan and Lise Boserup Foundation, TrygFonden, Johannes Fog’s Foundation, Region Zealand, Naestved Hospital, National Board of Health, and Local Government Denmark Foundation. The WGHS is supported by HL043851 and HL080467 from the National Heart, Lung, and Blood Institute and CA047988 from the National Cancer Institute, the Donald W Reynolds Foundation and the Fondation Leducq, with collaborative scientific support and funding for genotyping provided by Amgen. The NHS and the HPFS was supported by grants UM1 CA186107, P01 CA87969, R01 CA49449, R01 HL034594, R01 HL088521, UM1 CA167552, R01 HL35464, HL073168, CA87969, CA49449, CA055075, HL34594, HL088521, U01HG004399, DK080140, P30, U01CA137088, U54CA155626, DK58845, DK098311, U01HG004728, EY015473, CA134958, DK70756, and DK46200 from the National Institutes of Health, with additional support for genotyping from Merck Research Laboratories, North Wales, PA. LRP is supported by the Arthur Ashley Williams Foundation and a Harvard ophthalmology scholar award (Harvard Medical School) from the Harvard Glaucoma Center of Excellence. ATC is a Damon Runyon Cancer Foundation clinical investigator. The funding sources had no role in the design or conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript. ARIC is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C), R01HL087641, R01HL59367 and R01HL086694; National Human Genome Research Institute contract U01HG004402; and National Institutes of Health contract HHSN268200625226C. Infrastructure was partly supported by grant No UL1RR025005, a component of the National Institutes of Health and NIH roadmap for medical research. The Inter99 study was funded by the Danish Research Councils, Health Foundation, Danish Centre for Evaluation and Health Technology Assessment, Copenhagen County, Danish Heart Foundation, Ministry of Health and Prevention, Association of Danish Pharmacies, Augustinus Foundation, Novo Nordisk, Velux Foundation, Becket Foundation, and Ib Henriksens Foundation. The D.E.S.I.R. study has been supported by INSERM contracts with CNAMTS, Lilly, Novartis Pharma, and Sanofi-Aventis; by INSERM (Réseaux en Santé Publique, Interactions entre les déterminants de la santé, Cohortes Santé TGIR 2008), the Association Diabète Risque Vasculaire, the Fédération Française de Cardiologie, La Fondation de France, ALFEDIAM, CNIEL, ONIVINS, Société Francophone du Diabète, Ardix Medical, Bayer Diagnostics, Becton Dickinson, Cardionics, Merck Santé, Novo Nordisk, Pierre Fabre, Roche, Topcon. The funding sources had no role in the design or conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript. The D.E.S.I.R. Study Group: INSERM CESP U1018: B Balkau, P Ducimetière, E Eschwège; INSERM U367: F. Alhenc-Gelas; CHU d’Angers: A Girault; Bichat Hospital: F Fumeron, M Marre, R Roussel; CHU de Rennes: F Bonnet; CNRS UMR8090, Lille: S Cauchi P Froguel; Centres d’Examens de Santé: Alençon, Angers, Blois, Caen, Chartres, Chateauroux, Cholet, Le Mans, Orléans, Tours; Institute de Recherche Médecine Générale: J Cogneau; General practitioners of the region; Institute inter-Regional pour la Santé: C Born, E Caces, N Copin, JG Moreau, O Lantieri, F Rakotozafy, J Tichet, S Vol. The Rotterdam Study is funded by Erasmus Medical Center and Erasmus University, Rotterdam, Netherlands Organization for the Health Research and Development (ZonMw), the Research Institute for Diseases in the Elderly (RIDE), the Ministry of Education, Culture and Science, the Ministry for Health, Welfare and Sports, the European Commission (DG XII), and the Municipality of Rotterdam. The authors are grateful to the study participants, the staff from the Rotterdam Study and the participating general practitioners and pharmacists. The generation and management of GWAS genotype data for the Rotterdam Study is supported by the Netherlands Organisation of Scientific Research NWO Investments (No 175.010.2005.011, 911-03-012). This study is funded by the Research Institute for Diseases in the Elderly (014-93-015; RIDE2), the Netherlands Genomics Initiative (NGI)/Netherlands Organisation for Scientific Research (NWO) project No 050-060-810. The MDCS was initiated and planned in collaboration with the International Agency for Research on Cancer, the Swedish Cancer Society, and Swedish Medical Research Council and the Faculty of Medicine Lund University, Sweden. The study is also funded by Region Skåne, City of Malmö, Påhlsson Foundation and the Swedish Heart and Lung Foundation.
The GLACIER Study was funded by project grants from the Swedish Heart-Lung Foundation, the Swedish Diabetes Association, the Påhlsson’s Foundation, Region Skåne, the Swedish Research Council, the Umeå Medical Research Foundation, Novo Nordisk, The Heart Foundation of Northern Sweden (all to PWF), and Wellcome Trust WT098051. The MESA study was supported by contracts HHSN268201500003I, N01-HC-95159,N01-HC-95160, N01-HC-95161, N01-HC-95162, N01-HC-95163, N01-HC-95164, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168 and N01-HC-95169 from the National Heart, Lung, and Blood Institute, and by grants UL1-TR-000040 and UL1-TR-001079 from NCRR. The FamHS was supported by grants DK089256 and HL117078 from the National Institutes of Health. Infrastructure for the CHARGE Consortium is supported in part by the National Heart, Lung, and Blood Institute grant R01HL105756. This CHS research was supported by NHLBI contracts HHSN268201200036C, HHSN268200800007C, N01HC55222, N01HC85079, N01HC85080, N01HC85081, N01HC85082, N01HC85083, N01HC85086; and NHLBI grants U01HL080295, R01HL087652, R01HL105756, R01HL103612, and R01HL120393 with additional contribution from the National Institute of Neurological Disorders and Stroke (NINDS). Additional support was provided through R01AG023629 from the National Institute on Aging (NIA). A full list of principal CHS investigators and institutions can be found at CHS-NHLBI.org.The provision of genotyping data was supported in part by the National Center for Advancing Translational Sciences, CTSI grant UL1TR000124, and the National Institute of Diabetes and Digestive and Kidney Disease Diabetes Research Center (DRC) grant DK063491 to the Southern California Diabetes Endocrinology Research Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The YFS has been financially supported by the Academy of Finland: grants 286284 (TL), 134309 (Eye), 126925, 121584, 124282, 129378 (Salve), 117787 (Gendi), and 41071 (Skidi); the Social Insurance Institution of Finland; Kuopio, Tampere and Turku University Hospital Medical Funds (grant X51001 for T.L.); Juho Vainio Foundation; Paavo Nurmi Foundation; Finnish Foundation of Cardiovascular Research (T.L.); Finnish Cultural Foundation; Tampere Tuberculosis Foundation (TL); Emil Aaltonen Foundation (TL); and Yrjö Jahnsson Foundation (TL). The DCH and the DIOGENES cohorts were a part of the research program of the UNIK: Food, Fitness and Pharma for Health and Disease (see www.foodfitnesspharma.ku.dk). The UNIK project was supported by the Danish Ministry of Science, Technology and Innovation. Tuomas O Kilpeläinen was supported by the Danish Council for Independent Research (DFF– 333-00124 and Sapere Aude program grant DFF–1331-00730B). The PREDIMED-VALENCIA study was supported by the Spanish Ministry of Health (Instituto de Salud Carlos III) and the Ministerio de Economía y Competitividad (projects G03/140, CIBER 06/03, RD06/0045 PI07-0954, CNIC-06, PI11/02505, SAF2009-12304, AGL2010-22319-C03-03 and PRX14/00527), Fondo Europeo de Desarrollo Regional, by the University Jaume I (Project P1-1B2013-54) and by the Generalitat Valenciana (AP111/10, AP-042/11, BEST/2015/087, GVACOMP2011-151, ACOMP/2011/145, ACOMP/2012/190 and ACOMP/2013/159.
The BPRHS was supported by the National Institutes of Health grants P01 AG023394 and P50 HL105185. The GOLDN Study was supported by National Heart, Lung, and Blood Institute (NHLBI) grant No U01HL072524 (Genetic and Environmental Determinants of Triglycerides), NHLBI R01 HL091357 (Genomewide Association Study of Lipid Response to Fenofibrate and Dietary Fat), NHLBI grant Nos HL54776 and HL078885; and by contracts 53-K06-5-10 and 58-1950-9-001 from the US Department of Agriculture, Agriculture Research Service. The Raine Study was supported by the National Health and Medical Research Council of Australia (grant Nos 403981 and 003209) and the Canadian Institutes of Health Research (grant No MOP-82893). The 22 year Raine Study follow-up was funded by NHMRC project grants 1027449, 1044840 and 1021855. Funding was also provided by Safework Australia. The InCHIANTI study baseline (1998-2000) was supported as a “targeted project” (ICS110.1/RF97.71) by the Italian Ministry of Health and in part by the US National Institute on Aging (contracts: 263 MD 9164 and 263 MD 821336). The sponsors have no role in: the study design; the collection, analysis, or interpretation of data; the writing of the report; or in the decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: The study protocol was approved by the institutional review boards of the Brigham and Women’s Hospital and the Harvard TH Chan School of Public Health. The completion of the self administered questionnaire was considered to imply informed consent.
Data sharing: No additional data available.
Transparency: The lead authors (the manuscript’s guarantors) affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
References
- 1. Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224-60. 10.1016/S0140-6736(12)61766-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507-20. 10.1001/jama.2013.284427 [DOI] [PubMed] [Google Scholar]
- 3. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension: 7. Effects of more vs. less intensive blood pressure lowering and different achieved blood pressure levels - updated overview and meta-analyses of randomized trials. J Hypertens 2016;34:613-22. 10.1097/HJH.0000000000000881 [DOI] [PubMed] [Google Scholar]
- 4. Mozaffarian D. Dietary and Policy Priorities for Cardiovascular Disease, Diabetes, and Obesity: A Comprehensive Review. Circulation 2016;133:187-225. 10.1161/CIRCULATIONAHA.115.018585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang H, Fox CS, Troy LM, Mckeown NM, Jacques PF. Longitudinal association of dairy consumption with the changes in blood pressure and the risk of incident hypertension: the Framingham Heart Study. Br J Nutr 2015;114:1887-99. 10.1017/S0007114515003578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zong G, Sun Q, Yu D, et al. Dairy consumption, type 2 diabetes, and changes in cardiometabolic traits: a prospective cohort study of middle-aged and older Chinese in Beijing and Shanghai. Diabetes Care 2014;37:56-63. 10.2337/dc13-0975 [DOI] [PubMed] [Google Scholar]
- 7. Livingstone KM, Lovegrove JA, Cockcroft JR, Elwood PC, Pickering JE, Givens DI. Does dairy food intake predict arterial stiffness and blood pressure in men?: Evidence from the Caerphilly Prospective Study. Hypertension 2013;61:42-7. 10.1161/HYPERTENSIONAHA.111.00026 [DOI] [PubMed] [Google Scholar]
- 8. Dauchet L, Kesse-Guyot E, Czernichow S, et al. Dietary patterns and blood pressure change over 5-y follow-up in the SU.VI.MAX cohort. Am J Clin Nutr 2007;85:1650-6. [DOI] [PubMed] [Google Scholar]
- 9. Snijder MB, van Dam RM, Stehouwer CD, Hiddink GJ, Heine RJ, Dekker JM. A prospective study of dairy consumption in relation to changes in metabolic risk factors: the Hoorn Study. Obesity (Silver Spring) 2008;16:706-9. 10.1038/oby.2007.93 [DOI] [PubMed] [Google Scholar]
- 10. Samara A, Herbeth B, Ndiaye NC, et al. Dairy product consumption, calcium intakes, and metabolic syndrome-related factors over 5 years in the STANISLAS study. Nutrition 2013;29:519-24. 10.1016/j.nut.2012.08.013 [DOI] [PubMed] [Google Scholar]
- 11. Ralston RA, Lee JH, Truby H, Palermo CE, Walker KZ. A systematic review and meta-analysis of elevated blood pressure and consumption of dairy foods. J Hum Hypertens 2012;26:3-13. 10.1038/jhh.2011.3 [DOI] [PubMed] [Google Scholar]
- 12. Soedamah-Muthu SS, Verberne LD, Ding EL, Engberink MF, Geleijnse JM. Dairy consumption and incidence of hypertension: a dose-response meta-analysis of prospective cohort studies. Hypertension 2012;60:1131-7. 10.1161/HYPERTENSIONAHA.112.195206 [DOI] [PubMed] [Google Scholar]
- 13. Enattah NS, Sahi T, Savilahti E, Terwilliger JD, Peltonen L, Järvelä I. Identification of a variant associated with adult-type hypolactasia. Nat Genet 2002;30:233-7. 10.1038/ng826 [DOI] [PubMed] [Google Scholar]
- 14. Ingram CJ, Mulcare CA, Itan Y, Thomas MG, Swallow DM. Lactose digestion and the evolutionary genetics of lactase persistence. Hum Genet 2009;124:579-91. 10.1007/s00439-008-0593-6 [DOI] [PubMed] [Google Scholar]
- 15. Vimaleswaran KS, Cavadino A, Berry DJ, et al. LifeLines Cohort Study investigators. International Consortium for Blood Pressure (ICBP) Cohorts for Heart and Aging Research in Genomic Epidemiology (CHARGE) consortium. Global Blood Pressure Genetics (Global BPGen) consortium. Caroline Hayward Association of vitamin D status with arterial blood pressure and hypertension risk: a mendelian randomisation study. Lancet Diabetes Endocrinol 2014;2:719-29. 10.1016/S2213-8587(14)70113-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ehret GB, Munroe PB, Rice KM, et al. International Consortium for Blood Pressure Genome-Wide Association Studies. CARDIoGRAM consortium. CKDGen Consortium. KidneyGen Consortium. EchoGen consortium. CHARGE-HF consortium Genetic variants in novel pathways influence blood pressure and cardiovascular disease risk. Nature 2011;478:103-9. 10.1038/nature10405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tobin MD, Sheehan NA, Scurrah KJ, Burton PR. Adjusting for treatment effects in studies of quantitative traits: antihypertensive therapy and systolic blood pressure. Stat Med 2005;24:2911-35. 10.1002/sim.2165 [DOI] [PubMed] [Google Scholar]
- 18. Petitti DB. Approaches to heterogeneity in meta-analysis. Stat Med 2001;20:3625-33. 10.1002/sim.1091 [DOI] [PubMed] [Google Scholar]
- 19. Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol 2013;37:658-65. 10.1002/gepi.21758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schmidheiny K. Short Guides to Microeconometrics. http://kurt.schmidheiny.name/teaching/iv2up.pdf. 2016.
- 21. Thomas DC, Lawlor DA, Thompson JR. Re: Estimation of bias in nongenetic observational studies using “Mendelian triangulation” by Bautista et al. Ann Epidemiol 2007;17:511-3. 10.1016/j.annepidem.2006.12.005 [DOI] [PubMed] [Google Scholar]
- 22. Drouin-Chartier JP, Gagnon J, Labonté ME, et al. Impact of milk consumption on cardiometabolic risk in postmenopausal women with abdominal obesity. Nutr J 2015;14:12. 10.1186/1475-2891-14-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tanaka S, Uenishi K, Ishida H, et al. A randomized intervention trial of 24-wk dairy consumption on waist circumference, blood pressure, and fasting blood sugar and lipids in Japanese men with metabolic syndrome. J Nutr Sci Vitaminol (Tokyo) 2014;60:305-12. 10.3177/jnsv.60.305 [DOI] [PubMed] [Google Scholar]
- 24. Drouin-Chartier JP, Gigleux I, Tremblay AJ, Poirier L, Lamarche B, Couture P. Impact of dairy consumption on essential hypertension: a clinical study. Nutr J 2014;13:83. 10.1186/1475-2891-13-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rideout TC, Marinangeli CP, Martin H, Browne RW, Rempel CB. Consumption of low-fat dairy foods for 6 months improves insulin resistance without adversely affecting lipids or bodyweight in healthy adults: a randomized free-living cross-over study. Nutr J 2013;12:56. 10.1186/1475-2891-12-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Crichton GE, Howe PR, Buckley JD, Coates AM, Murphy KJ. Dairy consumption and cardiometabolic health: outcomes of a 12-month crossover trial. Nutr Metab (Lond) 2012;9:19. 10.1186/1743-7075-9-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. van Meijl LE, Mensink RP. Low-fat dairy consumption reduces systolic blood pressure, but does not improve other metabolic risk parameters in overweight and obese subjects. Nutr Metab Cardiovasc Dis 2011;21:355-61. 10.1016/j.numecd.2009.10.008 [DOI] [PubMed] [Google Scholar]
- 28. Wennersberg MH, Smedman A, Turpeinen AM, et al. Dairy products and metabolic effects in overweight men and women: results from a 6-mo intervention study. Am J Clin Nutr 2009;90:960-8. 10.3945/ajcn.2009.27664 [DOI] [PubMed] [Google Scholar]
- 29. Barr SI, McCarron DA, Heaney RP, et al. Effects of increased consumption of fluid milk on energy and nutrient intake, body weight, and cardiovascular risk factors in healthy older adults. J Am Diet Assoc 2000;100:810-7. 10.1016/S0002-8223(00)00236-4 [DOI] [PubMed] [Google Scholar]
- 30. Heraclides A, Mishra GD, Hardy RJ, et al. Dairy intake, blood pressure and incident hypertension in a general British population: the 1946 birth cohort. Eur J Nutr 2012;51:583-91. 10.1007/s00394-011-0242-z [DOI] [PubMed] [Google Scholar]
- 31. Engberink MF, Geleijnse JM, de Jong N, Smit HA, Kok FJ, Verschuren WM. Dairy intake, blood pressure, and incident hypertension in a general Dutch population. J Nutr 2009;139:582-7. 10.3945/jn.108.093088 [DOI] [PubMed] [Google Scholar]
- 32. Alonso A, Beunza JJ, Delgado-Rodríguez M, Martínez JA, Martínez-González MA. Low-fat dairy consumption and reduced risk of hypertension: the Seguimiento Universidad de Navarra (SUN) cohort. Am J Clin Nutr 2005;82:972-9. [DOI] [PubMed] [Google Scholar]
- 33. Steffen LM, Kroenke CH, Yu X, et al. Associations of plant food, dairy product, and meat intakes with 15-y incidence of elevated blood pressure in young black and white adults: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Clin Nutr 2005;82:1169-77, quiz 1363-4. [DOI] [PubMed] [Google Scholar]
- 34. Djoussé L, Pankow JS, Hunt SC, et al. Influence of saturated fat and linolenic acid on the association between intake of dairy products and blood pressure. Hypertension 2006;48:335-41. 10.1161/01.HYP.0000229668.73501.e8 [DOI] [PubMed] [Google Scholar]
- 35. Ruidavets JB, Bongard V, Simon C, et al. Independent contribution of dairy products and calcium intake to blood pressure variations at a population level. J Hypertens 2006;24:671-81. 10.1097/01.hjh.0000217849.10831.16 [DOI] [PubMed] [Google Scholar]
- 36. Snijder MB, van der Heijden AA, van Dam RM, et al. Is higher dairy consumption associated with lower body weight and fewer metabolic disturbances? The Hoorn Study. Am J Clin Nutr 2007;85:989-95. [DOI] [PubMed] [Google Scholar]
- 37. Dong JY, Szeto IM, Makinen K, et al. Effect of probiotic fermented milk on blood pressure: a meta-analysis of randomised controlled trials. Br J Nutr 2013;110:1188-94. 10.1017/S0007114513001712 [DOI] [PubMed] [Google Scholar]
- 38. Xu JY, Qin LQ, Wang PY, Li W, Chang C. Effect of milk tripeptides on blood pressure: a meta-analysis of randomized controlled trials. Nutrition 2008;24:933-40. 10.1016/j.nut.2008.04.004 [DOI] [PubMed] [Google Scholar]
- 39. Cicero AF, Aubin F, Azais-Braesco V, Borghi C. Do the lactotripeptides isoleucine-proline-proline and valine-proline-proline reduce systolic blood pressure in European subjects? A meta-analysis of randomized controlled trials. Am J Hypertens 2013;26:442-9. 10.1093/ajh/hps044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gijsbers L, Ding EL, Malik VS, de Goede J, Geleijnse JM, Soedamah-Muthu SS. Consumption of dairy foods and diabetes incidence: a dose-response meta-analysis of observational studies. Am J Clin Nutr 2016;103:1111-24. 10.3945/ajcn.115.123216 [DOI] [PubMed] [Google Scholar]
- 41. Soedamah-Muthu SS, Ding EL, Al-Delaimy WK, et al. Milk and dairy consumption and incidence of cardiovascular diseases and all-cause mortality: dose-response meta-analysis of prospective cohort studies. Am J Clin Nutr 2011;93:158-71. 10.3945/ajcn.2010.29866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Chen M, Sun Q, Giovannucci E, et al. Dairy consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. BMC Med 2014;12:215. 10.1186/s12916-014-0215-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. VanderWeele TJ, Tchetgen Tchetgen EJ, Cornelis M, Kraft P. Methodological challenges in mendelian randomization. Epidemiology 2014;25:427-35. 10.1097/EDE.0000000000000081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bergholdt HK, Nordestgaard BG, Ellervik C. Milk intake is not associated with low risk of diabetes or overweight-obesity: a Mendelian randomization study in 97,811 Danish individuals. Am J Clin Nutr 2015;102:487-96. 10.3945/ajcn.114.105049 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary appendix: additional information