Abstract
Purpose
Diabetes is a chronic lifelong condition, and adherence to medications and self-monitoring of blood glucose are challenging for diabetic patients. The dramatic increase in the prevalence of diabetes is largely due to the incidence of type 2 diabetes in low- and middle-income countries (LMIc) besides high-income countries (HIc). We aimed to evaluate whether pharmacist care (PC) service model in LMIc and HIc could improve clinical outcomes in diabetic patients by performing a meta-analysis.
Methods
PubMed, Embase, and ProQuest Dissertations Unlimited Published Literature database were searched to find publications pertaining to pharmacist-led intervention in patients with diabetes. The inclusion criteria were as follows: 1) randomized controlled trials, 2) confirmed diabetic patients (type 1 or type 2), 3) pharmaceutical care intervention by clinical pharmacist or/and multidisciplinary team, and 4) reporting HbA1c at baseline and end of study or the mean change in these values.
Results
A total of 37 articles were included in the meta-analysis. The overall result was significant and in favor of PC intervention on HbA1c change (standard difference in mean values [SDM]: 0.379, 95% CI: 0.208–0.550, P<0.001). The stratified meta-analysis showed that PC was significant in both HIc (n=20; SDM: 0.351, 95% CI: 0.207–0.495) and LMIc (n=15; SDM: 0.426, 95% CI: 0.071–0.780). More than 6 months is needed to obtain adequate effects on clinical diabetes parameters.
Conclusion
Our study presented that an adequate duration of pharmacist-led pharmaceutical care was effective in improving HbA1c in patients with diabetes in both LMIc and HIc.
Keywords: pharmacist care, multidisciplinary team care, diabetes, high-income country, low-and middle-income country
Introduction
Diabetes is a serious and chronic disease that can lead to various complications and premature death. According to the “Global Report on Diabetes (2016)” by World Health Organization (WHO), the number of diabetic adults has quadrupled to 422 million since 1980. This recent dramatic rise is largely due to the incidence of type 2 diabetes in low- and middle-income countries (LMIc). In all, 43% of deaths in a total or 3.7 million deaths related to diabetes in 2012 is attributable to higher than optimal blood glucose, and this occurs before the age of 70,1 which is much shorter than the life expectancy of 81.3 mean years among the Organisation for Economic Co-operation and Development (OECD) countries in 2015.2 Since diabetes is a chronic lifelong condition, adherence to medications and self-monitoring of blood glucose are quite challenging to the patients. Blood glucose concentration is a sensitive marker affected by numerous outer environments such as food intake, exercise, stress and medication.3 On the contrary, HbA1c concentration in the blood reflects the average blood glucose over the previous 8–12 weeks. The HbA1c level can predict the clinical outcome of microvascular4,5 and macrovascular complications6 as well, and the American Diabetes Association (ADA) recommend that HbA1c should be measured at regular intervals in all patients with diabetes.7 Thus, many researches on diabetes management are using HbA1c as a surrogate marker for clinical outcomes. There have been numerous efforts to implement pharmaceutical care in diabetic patients to improve disease outcomes. Improved management with the consistent support of multidisciplinary pharmaceutical care services can lead to better control of diabetes and fewer complications.8 For example, in Medication Therapy Management (MTM), a range of services including education, counseling, and assessing each medication and medication-related problems are provided to patients by clinical pharmacists to optimize and improve therapeutic outcomes in the USA.9 Together with hospital-based clinician-monitored programs, pharmacist-led community/hospital-based pharmaceutical care programs can be designed in an effort to achieve better glycemic, metabolic outcome and blood pressure control in this patient group.10
A recent meta-analysis11 and a systematic review12 of pharmacist for blood pressure and cardiovascular diseases showed that the implementation of a pharmacist care (PC) model provided improvement in outcomes. The systematic analysis and meta-analysis of PC for diabetic patients showed positive impact on HbA1c outcomes.13–15 However, recent studies reported no significantly different clinical parameters between the PC group and usual care (UC) group,16–18 rendering the need to reevaluate PC. Moreover, they did not present the effectiveness of PC in LMIc apart from high-income countries (HIc). Since the 2016 report of WHO revealed a considerable increase in the number of diabetic patients in LMIc, thus we aimed to evaluate whether the PC service model in HIc and LMIc could improve the clinical outcomes of diabetic patients by performing a meta-analysis including the up-to-date studies.
Methods
Search strategy
A systematic review protocol conforming to the Effective Practice and Organization of Care (EPOC) guideline was developed and prepared following the PRISMA recommendations.19 Electronic databases of PubMed, Embase, and ProQuest Dissertations Unlimited Published Literature database were searched by using the following keywords: “diabetes”, “diabetes mellitus”, “type one diabetes”, “type two diabetes”, “diabetes type 1”, “diabetes type 2”, “community pharmacy”, “community pharmacies”, “community pharmacist”, “community pharmacists”, “pharmacy”, “pharmacist”, “hospital pharmacy”, “hospital pharmacist”, “hospital pharmacists”, “pharmacy services”, “pharmacist intervention”, “pharmaceutical care”, “pharmac*”. A manual review was performed to search for unindexed articles in the Journal of Research in Medical Sciences, Journal of American Pharmacists Association and reference lists of related articles.
Inclusion and exclusion criteria
The literature search was performed to include studies published up to July 27, 2017, by two independent reviewers. Any disagreement was resolved by discussion among the two reviewers and a third researcher. The inclusion criteria for full-text review were as follows: 1) randomized controlled trial (RCT); 2) confirmed adult diabetic patients (type 1 or type 2); 3) pharmaceutical care intervention by clinical pharmacist or/and multidisciplinary team (PC includes working in cooperation with the patient and other health care providers to assess, monitor, initiate, and modify medication use and to provide education service to health care professionals as well as to the patients); and 4) each article should have reported HbA1c or fasting blood glucose (FBG) level at baseline and end of study or the mean change in these values.
The exclusion criteria were as follows: non-English language, editorials, commentaries, narrative reviews, clinical practice guidelines, conference abstracts, and literature not in peer-reviewed journals. The same reviewers independently evaluated the full text of all identified studies in the first stage of screening and resolved any disagreements.
Outcome assessment
HbA1c concentration in the blood reflects the average blood glucose over the previous 8–12 weeks. The HbA1c level can predict the clinical outcome of microvascular4,5 and macrovascular complications6 as well, and ADA recommend HbA1c to be measured at regular intervals in all patients with diabetes.7 Thus, HbA1c has been utilized as an additional stable criterion for assessing glucose control. In this aspect, we chose the difference of HbA1c change and the proportion of patients achieving target HbA1c level (<7%) between two groups as the main outcome measure.
Data extraction
The following information was extracted from the full text of included studies by two independent researchers: first author, year of publication, study type, country of study site, disease type of patients, age, service providers, intervention type, and laboratory data pertaining to HbA1c and the number of patients achieving HbA1c goal. The income levels were searched to pool outcomes by income level using the data from the World Bank Group.20 The duration of intervention was stratified and designated as 1 (<6 months), 2 (≥6 and <12 months), and 3 (≥12 months).
Quality score assessment
The quality of individual study was assessed by two independent reviewers using the EPOC risk of bias tool. This risk of bias tool is used when the clinical trials involve patient care, educational intervention, patient performance measure, health care quality measure.21 The standard risk of bias tool includes assessment of domains such as allocation concealment, baseline outcome, baseline characteristics, blinding, and selective reporting.
A domain with a low risk of bias is indicated by “low” and that with a high risk of bias is indicated by “high”. If a particular domain has ambiguity or uncertainty due to lack of information, then it is indicated as “unclear”.
Statistical analyses
The association between HbA1c levels after PC intervention and clinical outcomes was evaluated quantitatively by meta-analysis. The pooled OR were calculated for the included articles stratified by income status of the countries and duration of follow-up (3–5 months, 6–11 months, and ≥12 months). The primary outcome of this study was to evaluate the association between PC and HbA1c change.
Between-study heterogeneity was assessed by Q-statistic (heterogeneity was considered statistically significant if P<0.1)22 and quantified by I2 value. Both fixed- and random-effects models were used to combine the aggregate data determined by the I2 value. When I2 was >50%, the random-effects model was used for analysis. Potential publication bias was assessed using the Egger’s linear regression test.23
Statistical analyses were performed using Comprehensive Meta-Analysis (ver 3; Biostat, Inc., Engelwood, NJ, USA) and IBM SPSS (ver 21; IBM Corporation, Armonk, NY, USA). All tests were two sided, and P<0.05 was considered as significant unless otherwise specified.
Results
PRISMA flow for study selection
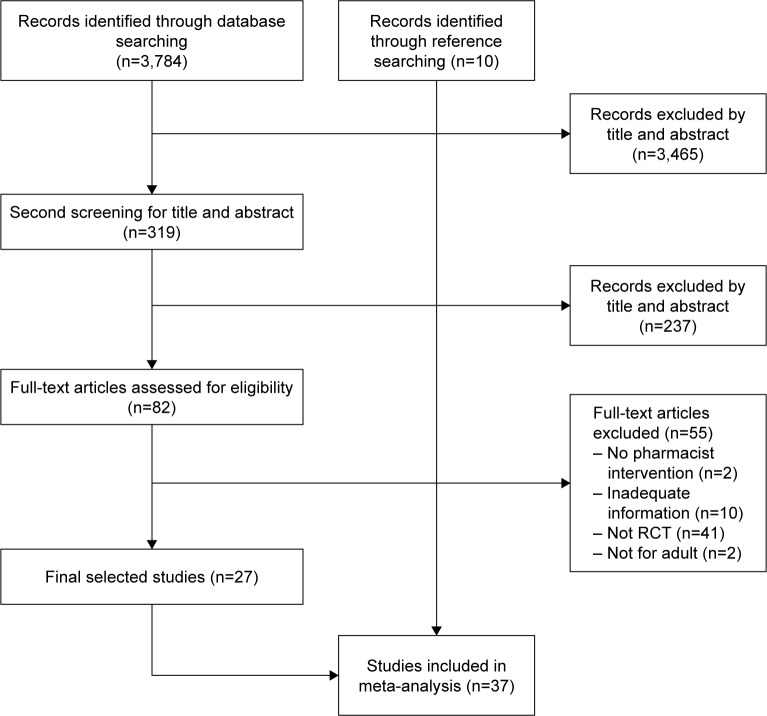
As shown in Figure 1, of the 3,794 publications identified, 35 publications were found eligible for meta-analysis.
Figure 1.
PRISMA flow diagram of selected publications in systematic review and meta-analysis.
Abbreviation: RCT, randomized controlled trial.
Among the identified publications, 3,465 articles were excluded as inappropriate by title and abstract review. In all, 82 articles were eligible for full-text review. After excluding studies with no pharmacist intervention (n=2), inadequate information (n=10), non-RCT studies (n=41), and non-adult studies (n=2), 27 articles were finally selected. Upon searching for the reference review, 10 additional articles were found to be eligible for meta-analysis; therefore finally, 37 studies were included in the meta-analysis.
Overall review
In all, 14 articles were published in the North American region (USA [n=13] and Canada [n=1]), three in the European region (UK, Spain, and Belgium), eight in Asia (Thailand [n=3], Hong Kong, Taiwan, Malaysia, Pakistan, and India), six in the Middle East (Jordan [n=2], Iraq, Iran [n=2], and UAE), three in Brazil, and three in Australia. Brazil, Iran, Iraq, Malaysia, Pakistan, Thailand, Jordan, UAE, and India were classified as LMIc.20 The intervention period was stratified as follows: intervention period <6 months (n=7), between 6 and 12 months (n=10), and ≥12 months (n=12). All the trials were conducted in ambulatory settings, including private clinic, hospital-based clinic, community pharmacies, and nationwide health care system or regional health care system (Table 1).
Table 1.
Characteristics of randomized controlled studies included in the final analysis
| Study ID | Country | Patients | PC/UC (n) | Setting | Care initiative | Intervention type | Duration (months) | Clinical outcomes |
|---|---|---|---|---|---|---|---|---|
| Jaber 199642 | USA | T2DM | 17/22 | University- affiliated internal medicine outpatient clinic | Pharmacist | Dosage evaluation, patient education, training on hyper and hypoglycemia, medication counseling, dietary regulation and exercise plan, and self-monitoring of blood glucose | 4 | HbA1c, FBG |
| Clifford 200243 | Australia | T1DM, T2DM | 48/25 | Hospital | MTC | Education and a brochure on risk factors, point-of-care cholesterol measurement, referral to their physician, and drug monitoring | 6 | HbA1c |
| Raji 200244 | USA | T1DM, T2DM | 50/56 | Veterans health care system | MTC | 3.5 day-structured curriculum, disease education, group discussion, lifestyle management by direct counseling or telephone intervention, and newsletter provided | 12 | HbA1c |
| Choe 200545 | USA | T2DM | 29/36 | University- affiliated primary care clinic | Pharmacist | Medication review and reconciliation, telephone intervention, lifestyle management, and self-monitoring blood glucose | 12 | HbA1c |
| Clifford 200546 | Australia | T2DM | 92/88 | Fremantle Diabetes Study | Pharmacist | Bimonthly newsletter, educational pamphlets, pharmacotherapeutic intervention, diet, exercise, and compliance with home blood glucose monitoring | 12 | HbA1c |
| Rothman 200547 | USA | T2DM | 112/105 | University of North Carolina General Internal Medicine Practice | Pharmacist | Intensive education and counseling, medication management, and applying evidence-based treatment algorithms | 12 | HbA1c |
| Suppapitiporn 200548 | Thailand | T2DM | 180/180 | Hospital | Pharmacist | Patient counseling, drug education, special medication container, and booklet provided | 6 | HbA1c, FBG |
| Fornos 200649 | Spain | T2DM | 56/56 | 14 community pharmacies | Pharmacist | Pharmacotherapy follow-up program, adherence education, and medication reconciliation | 14 | HbA1c, FBG |
| Scott 200650 | USA | T2DM | 76/73 | Community Health Center | MTC | Group session appointment, medication review, aspirin therapy and influenza vaccination education, lifestyle management, and telephone follow-up | 9 | HbA1c, FBG |
| Krass 200751 | Australia | T2DM | 149/140 | Quality care pharmacy program affiliated to 56 pharmacies | Pharmacist | Review of self-monitoring of blood glucose, disease, medication, and lifestyle education | 6 | HbA1c |
| Phumipamorn 200852 | Thailand | T1DM, T2DM | 67/68 | 30-bed community hospital | Pharmacist | Medication adherence, lifestyle management, and leaflet provided | 10 | HbA1c |
| Al Mazroui 200853 | UAE | T2DM | 117/117 | Military hospital | MTC | Drug education, lifestyle management, leaflet, and medication reconciliation | 12 | FBG |
| Edelman 201016 | USA | T1DM, T2DM | 133/106 | Two VA medical centers | MTC | Group medical clinic participation, disease education, disease, and medication review | 12.8 | HbA1c |
| Farsaei 201126 | Iran | T2DM | 87/87 | One outpatient clinic | MTC | Education and telephone counseling | 3 | HbA1c, FBG |
| Jameson 201018 | USA | T1DM, T2DM | 52/51 | AHPN | Pharmacist | Individualized education regarding diabetes self-management (diet, exercise, blood glucose level testing, medications, and insulin), early switching to insulin therapy after failure of two oral medications | 12 | HbA1c |
| Kirwin 201054 | USA | T1DM, T2DM | 150/151 | Four medical clinics | MTC | Medication review and treatment recommendation letter to physician | 10 | HbA1c, LDL |
| Taveira 201055 | USA | T2DM | 58/51 | VA medical center | MTC | Patients’ didactic education and behavioral and pharmacological intervention by pharmacist | 4 | HbA1c |
| Cohen 201156 | USA | T2DM | 50/49 | VA medical center | MTC | Four once weekly 2-hour sessions of education and behavioral and pharmacologic intervention review | 6 | HbA1c |
| Mehuys 201157 | Belgium | T2DM | 153/135 | 66 community pharmacies | MTC | Disease education, lifestyle management, medication adherence, and regular checkup reminding | 6 | HbA1c, FBG |
| Obreli-Neto 201127 | Brazil | T1DM, T2DM | 97/97 | Public primary health care unit | MTC | Group discussion, drug education, lifestyle management, patients’ counseling, and medication reconciliation | 36 | HbA1c, FBG |
| Simpson 201158 | Canada | T2DM | 131/129 | Five primary care clinics | Pharmacist | Medication review and implementation of guideline concordant recommendations | 12 | HbA1c |
| Siriam 201159 | India | T2DM | 60/60 | Multi-specialty tertiary care teaching hospital | Pharmacist | Medication counseling, dietary regulation, exercise, and lifestyle modifications | 3 | HbA1c, FBG |
| Ali 201260 | UK | T2DM | 23/23 | Two community pharmacies | Pharmacist | Lifestyle management, medication review, disease education, and medication reconciliation | 12 | HbA1c |
| Chan 201261 | Hong Kong | T2DM | 51/54 | 250-bed public convalescent hospital | Pharmacist | Disease education, medication adherence, and provided color stickers to identify drugs | 9 | HbA1c, FBG |
| Jacobs 201262 | USA | T2DM | 72/92 | Ambulatory general internal medicine setting | Pharmacist | Medication review, physical assessment, patients’ counseling, disease education, and lifestyle management | 12 | HbA1c |
| Jarab 201235 | Jordan | T2DM | 85/86 | 762-bed RMS hospital | Pharmacist | Structured patient education and discussion about type 2 diabetes, risks and types of complications from diabetes, prescribed drug therapy, and proper dosage | 6 | HbA1c |
| Kraemer 20115 | USA | T1DM, T2DM | 36/31 | Several employer-based health care plans | Pharmacist | Disease education, patients’ counseling, and referral to physician | 12 | HbA1c, FBG |
| Mahwi 201328 | Iraq | T2DM | 62/61 | Diabetic center | Pharmacist | Drug therapy problems and compliance by pill count and Morisky–Green test for drug adherence | 4 | HbA1c, FBG |
| Mourao 201334 | Brazil | T2DM | 50/50 | Six primary health care units integrated into the Brazilian public health system | Pharmacist | Patient education and/or pharmacotherapy changes | 6 | HbA1c |
| Samtia 201329 | Pakistan | T2DM | 174/168 | Diabetes clinics | Pharmacist | Disease education, drug education, and monitoring | 5 | HbA1c, FBG |
| O’Connor 201463 | USA | T1DM, T2DM | 92/103 | Kaiser Permanente Health Group | MTC | Protocol-structured telephone call and medication adherence reinforcement method | 6 | HbA1c |
| Chung 201464 | Thailand | T2DM | 120/121 | Major teaching hospital | Pharmacist | Medication review, solving drug-related problem, education on diabetes, hypertension, and hyperlipidemia | 12 | HbA1c, FBG |
| Cani 201531 | Brazil | T2DM | 41/37 | Teaching hospital | Pharmacist | Individualized pharmaceutical care plan | 6 | HbA1c |
| Jahangard- Rafsanjani 201532 | Iran | T2DM | 51/50 | Community pharmacy | Pharmacist | Blood glucose self-monitoring device, special logbook and education pamphlets, and medication reconciliation | 5 | HbA1c |
| Wishah 201530 | Jordan | T2DM | 52/54 | University hospital | MTC | Structured patients’ education and counseling for disease, medication, and lifestyle modification | 6 | HbA1c, FBG |
| Chen 201665 | Taiwan | T2DM | 50/50 | Hospital | Pharmacist | Assessment of adherence, pillbox, insulin injection technique, and medication regiment appropriateness (medication reconciliation) | 6 | HbA1c |
| Lim 201633 | Malaysia | T2DM | 39/37 | Hospital | Pharmacist | Booklet for disease and medication information, medication counseling, and education | 32 | HbA1c |
Abbreviations: PC/UC, pharmacist care/usual care; T2DM, type 2 diabetes mellitus; FBG, fasting blood glucose; T1DM, type 1 diabetes mellitus; MTC, Multidisciplinary Team Care; VA, Veterans Affairs; AHPN, Advantage Health Physician Network; RMS, royal medical services; LDL, low density lipoprotein.
All 37 studies included 2,961 PC and 2,899 UC patients. The overall period of pharmacist intervention was mean 9.07 months (SD 5.73) ranging from 3 to 32 months. In 27 studies, >100 diabetic patients were enrolled, and in 15 studies, the follow-up period was ≥12 months. The interventions were given from 2-week to 3-month interval, and several studies did not report the interval. The PC was conducted by pharmacists in 24 studies and MTC in 13 studies. The PC program consisted of information on disease and medications, adherence education, survival skills regarding hypo- and hyperglycemia incidence, and insulin injection skills. The delivery type of education or intervention was face-to-face intervention, telephone counseling, or group appointments, meeting, or education sessions. Adjunctive tools such as booklets, disease or medication information sheets, pillbox, and stickers were provided in many studies (Table 1).
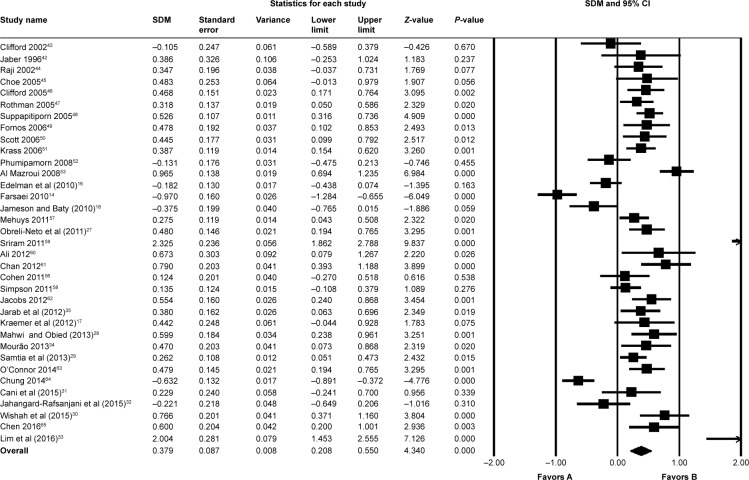
The overall pooled analysis for HbA1c change included 35 articles out of total 37 studies (Table S1). Owing to the high I2 value (89.380), the random-effects model was used. The result was significant and in favor of pharmacist-led intervention on HbA1c change (standard difference in mean values [SDM]: 0.379, 95% CI: 0.208–0.550, P=0.001), indicating the positive effect of pharmacist intervention in the improvement of clinical parameters in diabetes patients. The HbA1c level was 37.9% more reduced in the PC group than in the UC group (Figure 2).
Figure 2.
The overall comparison of PC and UC on the improvement of HbA1C level changes.
Abbreviations: PC, pharmacist care; UC, usual care; SDM, standard difference in mean values.
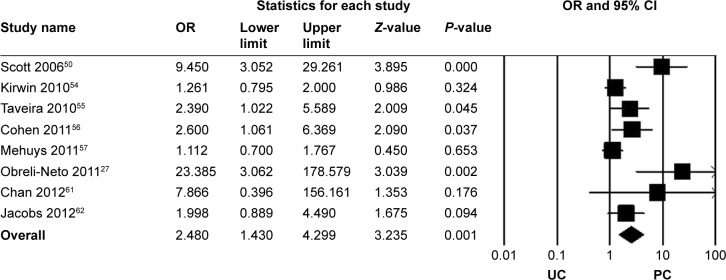
The proportion of patients achieving HbA1c goals was evaluated using eight articles that reported targeted outcomes out of total 37 included studies (Table S2). All the seven studies set the HbA1c target <7%, and the pooled result for the articles was significant and in favor of pharmacist intervention (OR: 2.48, 95% CI: 1.430–4.299, P=0.001). Approximately three times more patients achieved their HbA1c goal in the PC group compared to that in the UC group (Figure 3).
Figure 3.
Meta-analysis of proportion of patients achieving target HbA1c levels between the PC and UC groups.
Abbreviations: PC, pharmacist care; UC, usual care.
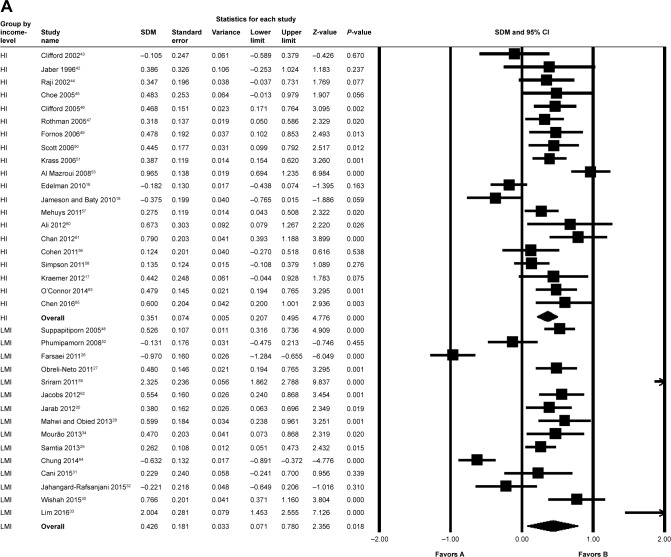
Group analysis for income status and intervention period
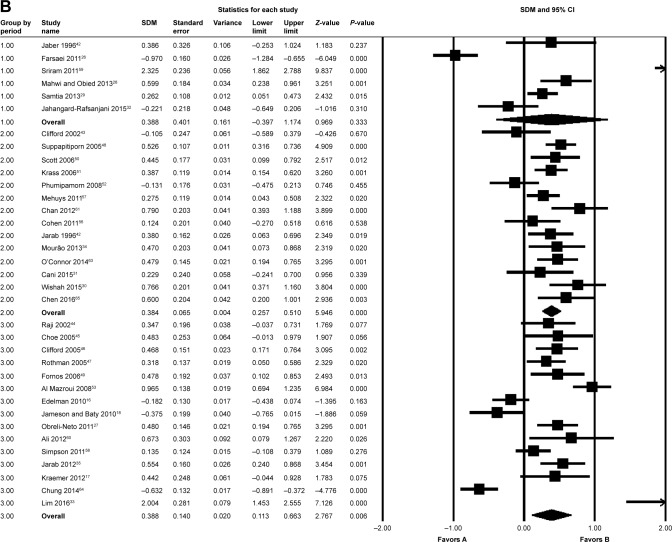
The stratified meta-analysis showed that PC was significant in both 20 HIc (SDM: 0.351, 95% CI: 0.207–0.495) and 15 LMIc (SDM: 0.426, 95% CI: 0.071–0.780; Figure 4A). The analysis for intervention period showed that interventions <6 months did not affect the clinical parameters of the patient (P=0.333). In the second group, 6–12 months of pharmacist intervention showed an improved effect, and the patients exhibited 36.4% more mean HbA1c level changes than the UC group (P<0.001). The longest intervention period of ≥12 months exhibited better effect on HbA1c reduction, with 38.8% more change in levels of HbA1c than the UC group (P=0.006; Figure 4B).
Figure 4.
Effect of PC and UC in the improvement of HbA1C levels stratified by income level (A) and intervention period (B).
Abbreviations: PC, pharmacist care; UC, usual care; SDM, standard difference in mean values.
Risk of bias score assessment by EPOC
The quality score of each study was graded by EPOC risk of bias tool by two independent researchers. As the selected primary literature had a low risk of bias in the domain of baseline outcome measure and characteristics, the baseline characteristics between two groups were similar. The reporting of results section had little risk either. However, the risks on blinding, allocation concealment, and contamination were high due to the nature of educational intervention studies (Table S3).
Publication bias
As widely accepted tools for publication bias, funnel plot visualization and Egger’s regression method were used to detect publication bias. Overall, the funnel plot and Egger’s regression (P=0.183) methods did not detect publication bias (Figure S1).
Discussion
In this study, we found a significant association between pharmacist-led pharmaceutical care and clinical diabetes management. This finding is corroborated by previous meta-analysis and systematic analysis for cardiovascular disease patients.11,12 Well-trained clinical pharmacists and a medical system utilizing active pharmacist-driven patient care can improve the quality, outcomes, and efficiency of patient management. Because this analysis included 20 studies from HIc and 15 from LMIc, the group analysis by income level showed that PC intervention was helpful in improving clinical outcomes in patients with diabetes in both HIc and LMIc. The positive outcomes observed in LMIc are particularly important considering the recent increase in the number of patients with diabetes and metabolic diseases in LMIc. The rapid spread of Western diet and lifestyle, as well as the improvement of socioeconomic status in LMIc, accelerates the incidence of obesity and chronic metabolic diseases in these countries. However, the introduction of clinical PC, such as MTM or multidisciplinary team care, is relatively rare in LMIc compared to that in HIc. A recent review reported that only 12% of clinical PC service is available for drug monitoring activities in Saudi Arabia.24 Controlling the glucose levels at a recommended level is a difficult task, and therefore, <57% of these patients achieved control of blood glucose as measured by HbA1c concentrations.25
A meta-analysis by Li et al14 included 14 RCTs and reported higher mean change in HbA1c (0.68) than that in our study (0.370), and another meta-analysis by Poolsup et al15 included 22 RCTs and reported the same mean change of 0.68 between PC and UC groups. We tried not to include heterogeneous population and excluded the research on adolescents and gestational diabetes patients. We excluded some studies that reported inadequate information to incorporate into meta-analysis that were included in the previous meta-analyses, which might be the reason of the different result. Furthermore, we included additionally 10 recently published studies conducted in LMIc,26–35 and this factor impacted the different results as well.
Generally, the care itself and the social/individual treatment costs of passive medical service administration are challenging. Therefore, more active and interactive multisec-tor collaboration work is essential to manage complicated diseases such as diabetes. In addition, the length of the intervention period is important in achieving adequate effects on clinical parameter improvement.
Another important finding of this study is that the longer intervention period of >6 months showed significant impact on the clinical parameters, while the intervention period of <6 months did not. These factors suggest the need for expanded training in primary care, with at least 6 months of education and intervention, to improve the comprehensiveness and quality of care provided to the growing number of patients with diabetes.
From the aspect of intervention tools, most interventions comprise a face-to-face method between pharmacists and patients, supplemented with leaflets and telephone outreach. The growing information age has enabled the availability of high-technology information and education tool kits. To educate diabetic patients, high-technology investments should be accelerated by country-level funding as suggested by a few studies36–38 in which the participants showed a considerable decrease in the HbA1c level and several technological suggestions were provided. The technologies for health care providers include electronic database identifying and tracking patients and computer software designed for clinical decision support to the providers and telemedicine and telecare services, which currently equipped in HIc widely. Specific tool for patients focuses on the self-management skill improvement by the internet-, telephone- and mobile-based tools. If PC service model incorporates these high technologies into the PC, the care can produce much better clinical outcomes. Since most of the HIc have already adopted or are adopting pharmacist-led pharmaceutical care, the results of this study can encourage the utilization of pharmaceutical care in LMIc. A trend was observed in the following LMIc studies conducted in recent years: Obreli-Neto et al,27 2011 (Brazil); Mahwi et al,28 2013 (Iraq); Samtia et al,29 2013 (Pakistan); Cani et al,31 2015 (Brazil); Jahangard-Rafsanjani et al,32 2015 (Iran); Wishah et al,30 2015 (Jordan); and Lim et al,33 2016 (Malaysia), except for Jahangard-Rafsanjani et al,32 2015 (Iran) and Wishah et al,30 2015 (Jordan), in that all the studies showed promising outcomes for pharmacist-led pharmaceutical care strategy in diabetes care in LMIc. A study evaluating the clinical outcome of blood pressure control reported that after stopping the PC, patient behavior returned to pre-intervention level, meaning consistent PC care is needed to better contribute to patients’ clinical outcome.39
There are some limitations to our study. The risk of bias evaluated by EPOC guideline showed that some of the included publications lack methodical robust in blinding, allocation concealment, and reporting of contaminations. These factors can be considered in future clinical studies to make the results more reliable. The big heterogeneity of included studies is another limitation of this study. This heterogeneity is not from the clinical factor but is derived from statistical or unexplainable factors, so we adopted the random-effects model into the meta-analysis by using a statistic that indicates the percentage of variance in a meta-analysis that is attributable to study heterogeneity (I2). This model sets an assumption that the effects being estimated in the different studies are not identical but follow some distribution. Even though the random-effects model confronts some criticism but simulations have proven that this method is relatively robust even under wide range of distributional assumptions, both in estimating heterogeneity40 and calculating an overall effect size.41 Thus, by using random-effects model in our analysis, the heterogeneity of included studies has been overcome in our research.
Conclusion
Clinical pharmacists can make a comparative evaluation of medications based on sound knowledge of medications. The multitasking of clinical pharmacists, which includes healthy communication with health care workers and active interaction with patients, can lead to adherence to clinical therapeutic guidelines and medications. Pharmacist-led pharmaceutical care is a robust health care strategy maximizing therapeutic efficacy and improving lifelong care in diabetes patients in both HIc and LMIc.
Supplementary materials
Publication bias visualized by funnel plot.
Abbreviation: SDM, standard difference in mean values.
Table S1.
The changes in HbA1C between PC group and UC group
| Study ID | Intervention group
|
Control group
|
Sample size
|
P-value | |||
|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | PC | UC | ||
| Jaber 199612 | 11.5±2.9 | 9.2±2.1 | 12.2±3.5 | 12.1±3.7 | 17 | 22 | 0.003 |
| Clifford 200213 | 8.4±1.4 | 8.2±1.5 | 8.5±1.6 | 8.1±1.6 | 48 | 25 | >0.05 |
| Raji 200214 | 9.9±1.3 | 8±1.4 | 9.8±1.2 | 8.6±1.8 | 50 | 56 | 0.03 |
| Choe 200515 | 10.1±1.8 | 8±1.4 | 10.2±1.7 | 9.3±2.1 | 29 | 36 | 0.03 |
| Clifford 200516 | −0.5 (−0.7 to −0.3) | 0 (−0.2 to 0.2) | 92 | 88 | 0.002 | ||
| Rothman 200517 | 0.8 (0–1.7%) | 112 | 105 | 0.05 | |||
| Suppapitiporn 200518 | 8.16±1.44 | 7.91±1.27 | 8.01±1.51 | 8.8±1.36 | 180 | 180 | 0.001 |
| Fornos 200619 | 8.4±1.8 | 7.9±1.7 | 7.8±1.7 | 8.5±1.9 | 56 | 56 | 0.001 |
| Scott 200620 | 8.8±1.72 | 7.08±1.72 | 8.7±0.7 | 8±0.7 | 64 | 67 | 0.012 |
| Krass 200721 | 8.9±1.4 | 7.9±1.2 | 8.3±1.3 | 8.0±1.2 | 125 | 107 | <0.01 |
| Phumipamorn 200822 | 8.7±1.5 | 7.9±1.4 | 8.7±1.6 | 8.1±1.9 | 63 | 67 | 0.56 |
| Al Mazroui 200923 | 8.5 (8.3–8.7) | 6.9 (6.7–7.1) | 8.4 (8.2–8.6) | 8.3 (8.1–8.5) | 117 | 117 | 0.001 |
| Edelman 20101 | 9.2 | 8.3 | 9.2 | 8.6 | 133 | 106 | 0.159 |
| −0.33 (−0.80 to 0.13) | |||||||
| Farsaei 201024 | 9.3±1.7 | 7.5±1.6 | 8.9±1.1 | 9.0±1.2 | 87 | 87 | >0.05 |
| Jameson 201025 | −1.5 (−0.03 to −2.68) | −0.40 (0.5 to −2.10) | 52 | 51 | 0.06 | ||
| Cohen 201126 | −0.41 (−0.74 to −0.07) | −0.20 (−0.61 to 0.21) | 50 | 49 | 0.028 | ||
| Mehuys 201127 | 7.7±1.7 | 7.1±1.1 | 7.3±1.2 | 7.2±1 | 153 | 135 | 0.009 |
| Obreli-Neto 20113 | −0.7 (−0.9 to 0.5) | 0.0 (−0.1 to 0.1) | 97 | 97 | 0.001 | ||
| Simpson 201128 | −0.15 (−0.36 to 0.05) | 0.03 (−0.22 to 0.28) | 131 | 129 | <0.05 | ||
| Siriam 201129 | 8.44±0.29 | 6.73±0.21 | 9.03±0.46 | 8.3±0.16 | 60 | 60 | 0.010 |
| Ali 201230 | 8.2±1.65 | 6.6±0.59 | 8.1±0.97 | 7.5±0.64 | 23 | 23 | 0.001 |
| Chan 201231 | −1.57%+1.50% | −0.40%+1.19% | 51 | 54 | <0.00 | ||
| Jacobs 201232 | 9.5±1.1 | 7.7±1.3 | 9.2±1 | 8.4±1.6 | 72 | 92 | 0.003 |
| Jarab 20124 | −0.8 (−1.6 to 0.1) | 0.1 (−0.4 to 0.7) | 77 | 79 | 0.019 | ||
| Kraemer 20125 | 7.28 | 6.78 | 7.38 | 7.22 | 36 | 31 | 0.0757 |
| −0.5 (change in mean values) | −0.16 (change in mean values) | ||||||
| Mahwi 20136 | 11.53±1.83 | 9.2±2 | 9.97±2.75 | 9.5±2.1 | 62 | 61 | 0.001 |
| Mourao 201333 | −0.6 (−1.1 to −0.02) | 0.7 (0.2–1.3) | 50 | 50 | 0.001 | ||
| Samtia 20137 | 8.51±1.62 | 7.5±1.26 | 8.54±1.55 | 8.08±1.49 | 178 | 170 | 0.001 |
| O’Connor 201434 | −0.9±1.85 | −1.08±1.78 | 92 | 103 | 0.001 | ||
| Cani 20158 | 9.78±1.55 | 9.21±1.41 | 9.61±1.38 | 9.53±1.68 | 34 | 36 | 0.001 |
| Jahangard-Rafsanjani 20159 | 7.6±1.6 | 6.6±1.5 | 7.5±1.9 | 7.0±1.7 | 51 | 50 | 0.09 |
| Wishah 201510 | 8.9±1.6 | 7.2±0.9 | 8.2±1.3 | 7.9±1.3 | 52 | 54 | >0.05 |
| Chen 201635 | 9.22±1.7 | 8.39±1.2 | 8.94±1.5 | 9.37±1.5 | 50 | 50 | 0.002 |
| Lim 201611 | 10.11±0.26 | 9.21±0.27 | 9.71±0.34 | 9.63±0.29 | 39 | 37 | 0.001 |
Abbreviations: PC, pharmacist care; UC, usual care.
Table S2.
Proportion of patients achieving HbA1c goal between PC group and UC group
| Study ID | Goal | Intervention group
|
Control group
|
||
|---|---|---|---|---|---|
| Total (n) | Event (n) | Total (n) | Event (n) | ||
| Scott 200620 | A1C<7% | 64 | 24 | 67 | 4 |
| Kirwin 201036 | A1C<7% | 150 | 65 | 151 | 57 |
| Taveira 201037 | A1C<7% | 58 | 23 | 51 | 11 |
| Cohen 201126 | A1C<7% | 50 | 20 | 49 | 10 |
| Mehuys 201127 | A1C<7% | 153 | 80 | 135 | 67 |
| Obreli-Neto 20113 | A1C<7% | 97 | 19 | 97 | 1 |
| Chan 201231 | A1C<7% | 51 | 3 | 54 | 0 |
| Jacobs 201238 | A1C<7% | 55 | 19 | 67 | 14 |
Abbreviations: PC, pharmacist care; UC, usual care.
Table S3.
Quality check for included studies (randomized controlled studies) by EPOC risk of bias
| Study ID | Sequence generation | Allocation concealment | Baseline outcome measurements | Baseline characteristics | Incomplete outcome data | Blinding of participants, personnel | Protection against contamination | Selective outcome reporting | Other sources of bias |
|---|---|---|---|---|---|---|---|---|---|
| Jaber 199612 | Unclear | Unclear | Low | Low | Low | Unclear | Unclear | Low | Unclear |
| Clifford 200213 | Low | Unclear | Low | Low | Low | Unclear | Unclear | Low | Unclear |
| Raji 200214 | Unclear | Unclear | Low | Low | Low | Unclear | Unclear | Low | Unclear |
| Choe 200515 | Low | Unclear | Low | Low | Low | High | Low | Low | Unclear |
| Clifford 200516 | Unclear | Unclear | Low | Low | Low | Low | Low | Low | Unclear |
| Rothman 200517 | Low | Low | Low | Low | Low | Unclear | Low | Low | Unclear |
| Suppapitiporn 200518 | Unclear | Unclear | Low | Low | Low | Unclear | Unclear | Low | Unclear |
| Fornos 200619 | Low | Unclear | Low | Low | Low | High | Low | Unclear | Unclear |
| Scott 200620 | Low | Unclear | Low | Low | Low | High | Low | Unclear | Unclear |
| Krass 200721 | Unclear | Unclear | Low | Low | Low | High | Low | Low | Unclear |
| Phumipamorn 200822 | Low | High | Unclear | Unclear | Low | Unclear | Low | Low | Unclear |
| Al Mazroui 200923 | Unclear | Unclear | Low | Low | Unclear | Unclear | Unclear | Low | Unclear |
| Edelman 20101 | Low | Unclear | Low | Low | Unclear | High | Low | Low | Unclear |
| Farsaei 201024 | Unclear | Unclear | Low | Low | Unclear | Unclear | Unclear | Low | Unclear |
| Jameson 20102 | Low | Low | Low | Low | Low | High | Unclear | Low | Unclear |
| Kirwin 201036 | Unclear | Unclear | High | Low | Unclear | Unclear | High | High | Unclear |
| Taveira 201037 | Low | Unclear | High | High | Unclear | Unclear | Unclear | High | Unclear |
| Cohen 201126 | Unclear | Unclear | Low | Low | Low | Unclear | Low | Low | Unclear |
| Mehuys 201127 | Low | Unclear | Low | Low | Unclear | Unclear | Unclear | Low | Unclear |
| Obreli-Neto 20113 | Low | Unclear | Low | Low | High | High | Unclear | Low | Unclear |
| Simpson 201128 | Low | Unclear | Low | Low | Unclear | Low | Low | Low | Low |
| Siriam 201129 | Unclear | Unclear | Low | Low | Low | Low | Unclear | Low | Unclear |
| Ali 201230 | Low | Low | Low | Low | Low | Unclear | Low | Low | Unclear |
| Chan 201231 | Low | Low | Low | Low | Unclear | Unclear | Unclear | Low | Unclear |
| Jacobs 201232 | Low | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low | Unclear |
| Jarab 20124 | Low | Unclear | Low | Low | Low | Unclear | Unclear | Low | Unclear |
| Kraemer 20125 | Low | Unclear | Low | Low | Unclear | Unclear | Unclear | Low | Unclear |
| Mahwi 20136 | Low | Low | Low | Low | Unclear | Unclear | Unclear | Low | Unclear |
| Mourao 201333 | Low | Unclear | Low | Low | Low | Unclear | Unclear | Unclear | Unclear |
| Samtia 20137 | Unclear | Unclear | Low | Low | Unclear | Unclear | Unclear | Low | Unclear |
| Chung 201439 | Unclear | Unclear | Low | Low | Low | Low | Low | Unclear | Unclear |
| O’Connor 201434 | Low | Low | Low | Low | Low | Low | Unclear | Low | Unclear |
| Cani 20158 | Unclear | Unclear | Low | Low | Low | Low | Unclear | Low | Unclear |
| Jahangard-Rafsanjani | Low | Low | Low | Low | Low | Low | Unclear | Low | Unclear |
| 20159 | |||||||||
| Wishah 201510 | Low | Low | Low | Low | Low | Low | Unclear | Low | Unclear |
| Chen 201635 | Low | Low | Low | Low | Unclear | Unclear | Unclear | Low | Unclear |
| Lim 201611 | Unclear | Unclear | Low | Low | Low | Low | Unclear | Low | Unclear |
Abbreviation: EPOC, Effective Practice and Organization of Care.
References
- 1.Edelman D, Fredrickson SK, Melnyk SD, et al. Medical clinics versus usual care for patients with both diabetes and hypertension: a random-ized trial. Ann Intern Med. 2010;152(11):689–696. doi: 10.7326/0003-4819-152-11-201006010-00001. [DOI] [PubMed] [Google Scholar]
- 2.Jameson JP, Baty PJ. Pharmacist collaborative management of poorly controlled diabetes mellitus: a randomized controlled trial. Am J Manag Care. 2010;16(4):250–255. [PubMed] [Google Scholar]
- 3.Obreli-Neto PR, Guidoni CM, de Oliveira Baldoni A, et al. Effect of a 36-month pharmaceutical care program on pharmacotherapy adherence in elderly diabetic and hypertensive patients. Int J Clin Pharm. 2011;33(4):642–649. doi: 10.1007/s11096-011-9518-x. [DOI] [PubMed] [Google Scholar]
- 4.Jarab AS, Alqudah SG, Mukattash TL, Shattat G, Al-Qirim T. Random-ized controlled trial of clinical pharmacy management of patients with type 2 diabetes in an outpatient diabetes clinic in Jordan. J Manag Care Pharm. 2012;18(7):516–526. doi: 10.18553/jmcp.2012.18.7.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kraemer DF, Kradjan WA, Bianco TM, Low JA. A randomized study to assess the impact of pharmacist counseling of employer-based health plan beneficiaries with diabetes: the EMPOWER study. J Pharm Pract. 2012;25(2):169–179. doi: 10.1177/0897190011418513. [DOI] [PubMed] [Google Scholar]
- 6.Mahwi TO, Obied KA. Role of the pharmaceutical care in the management of patients with type 2 diabetes mellitus. IJPSR. 2013;4(4):1363–1369. [Google Scholar]
- 7.Samtia AM, Rasool MF, Ranjha NM, Usman F, Javed I. A multifactorial intervention to enhance adherence to medications and disease-related knowledge in type 2 diabetic patients in Southern Punjab, Pakistan. Trop J Pharm Res. 2013;12(5):851–856. [Google Scholar]
- 8.Cani CG, Lopes LS, Queiroz M, Nery M. Improvement in medication adherence and self-management of diabetes with a clinical pharmacy program: a randomized controlled trial in patients with type 2 diabetes undergoing insulin therapy at a teaching hospital. Clinics. 2015;70(2):102–106. doi: 10.6061/clinics/2015(02)06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jahangard-Rafsanjani Z, Sarayani A, Nosrati M, et al. Effect of a community pharmacist-delivered diabetes support program for patients receiving specialty medical care: a randomized controlled trial. Diabetes Educ. 2015;41(1):127–135. doi: 10.1177/0145721714559132. [DOI] [PubMed] [Google Scholar]
- 10.Wishah RA, Al-Khawaldeh OA, Albsoul AM. Impact of pharmaceutical care interventions on glycemic control and other health-related clinical outcomes in patients with type 2 diabetes: randomized controlled trial. Diabetes Metab Syndr. 2015;9(4):271–276. doi: 10.1016/j.dsx.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 11.Lim PC, Lim K, Embee ZC, Hassali MA, Thiagarajan A, Khan TM. Study investigating the impact of pharmacist involvement on the outcomes of diabetes medication therapy adherence program Malaysia Pak. J Pharm Sci. 2016;29(2):595–601. [PubMed] [Google Scholar]
- 12.Jaber LA, Halapy H, Fernet M, Tunmalapalli S, Diwakaran A. Evaluation of a pharmaceutical care model on diabetes management. The Annals of Pharmacotherapy. 1996;30:238–243. doi: 10.1177/106002809603000305. [DOI] [PubMed] [Google Scholar]
- 13.Clifford RM, Batty KT, Davis TME, Davis W, Stein G, Stewart G, et al. A randomised controlled trial of a pharmaceutical care programme in high-risk diabetic patients in an outpatient clinic. Int J Pharm Pract. 2002;10:85–89. [Google Scholar]
- 14.Raji A, Gomes H, Beard JO, MacDonald P, Conlin PR. A randomized trial comparing intensive and passive education in patients with Diabetes Mellitus. Arch Intern Med. 2002;162:1301–1304. doi: 10.1001/archinte.162.11.1301. [DOI] [PubMed] [Google Scholar]
- 15.Choe HM, Mitrovich S, Dubay D, Hayward RA, Krein SL, Vijan S. Proactive case management of high-risk patients with type 2 diabetes mellitus by a clinical pharmacist: a randomized controlled trial. Am J Manag Care. 2005;11:253–260. [PubMed] [Google Scholar]
- 16.Clifford RM, Davis WA, Batty KT, Davis TME. Effect of a Pharmaceutical Care Program on Vascular Risk Factors in Type 2 Diabetes: The Fremantle Diabetes Study. Diabetes Care. 2005;28:771–776. doi: 10.2337/diacare.28.4.771. [DOI] [PubMed] [Google Scholar]
- 17.Rothman R, Malone R, Bryant B, Shintani AK, Crigler B, Dewalt DA, et al. A randomized trial of a primary care–based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetes. The American Journal of Medicine. 2005;118:276–284. doi: 10.1016/j.amjmed.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 18.Suppapitiporn S, Chindavijak B, Onsanit S. Effects of Diabetes Drug Counseling by Pharmacist, Diabetic Disease Booklet and Special Medication Containers on Glycemic Control of Type 2 Diabetes Mellitus. J Med Assoc of Thai. 2005;88(Suppl 4):S134–S141. [PubMed] [Google Scholar]
- 19.Fornos JA, ´s NFA, ´s JCA, Guerra MM, Egea B. A pharmacotherapy follow-up program in patients with type-2 diabetes in community pharmacies in Spain. Pharm World Sci. 2006;28:65–72. doi: 10.1007/s11096-006-9003-0. [DOI] [PubMed] [Google Scholar]
- 20.Scott DM, T Boyd S, Stephan M, Augustine SC, Reardon TP. Outcomes of pharmacist-managed diabetes care services in a community health center. Am J Health-Syst Pharm. 2006;63:2116–2122. doi: 10.2146/ajhp060040. [DOI] [PubMed] [Google Scholar]
- 21.Krass I, Armour CL, Mitchell B, Brillant M, Dienaar R, Hughes J, et al. The Pharmacy Diabetes Care Program: assessment of a community pharmacy diabetes service model in Australia. Diabetic Medicine. 2006;24:677–683. doi: 10.1111/j.1464-5491.2007.02143.x. [DOI] [PubMed] [Google Scholar]
- 22.Phumipamorn S, Pongwecharak J, Soorapan S, Pattharachayakul S. Effects of the pharmacist’s input on glycaemic control and cardiovascular risks in Muslim diabetes. Prim Care Diabetes. 2008;2(1):31–37. doi: 10.1016/j.pcd.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 23.Mazroui NRA, Kamal MM, Ghabash NM, Yacout TA, Kole PL, McElnay JC. Influence of pharmaceutical care on health outcomes in patients with Type 2 diabetes mellitus. Br J Clin Pharmacol. 2008;67(5):547–557. doi: 10.1111/j.1365-2125.2009.03391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Farsaei S, Sabzghabaee AM, Zargarzadeh AH, Amini M. Effect of pharmacist-led patient education on glycemic control of type 2 diabetics: a randomized controlled trial. J Res Med Sci. 2011;16(1):43–49. [PMC free article] [PubMed] [Google Scholar]
- 25.Jameson JP, Baty PJ. Pharmacist collaborative management of poorly controlled diabetes mellitus: a randomized controlled trial. Am J Manag Care. 2010;16(4):250–255. [PubMed] [Google Scholar]
- 26.Cohen LB, Taveira TH, Khatana SAM, Dooley AG, Pirraglia PA, Wu W-C. Pharmacist-Led Shared Medical Appointments for Multiple Cardiovascular Risk Reduction in Patients With Type 2 Diabetes. The Diabetes Educator. 2011;37:800–809. doi: 10.1177/0145721711423980. [DOI] [PubMed] [Google Scholar]
- 27.Mehuys E, Bortel LV, Bolle LD, Tongelen IV, Tongelen LA, Annemans L, et al. Effectiveness of a community pharmacist intervention in diabetes care: a randomized controlled trial. Journal of Clinical Pharmacy and Therapeutics. 2011;36:602–613. doi: 10.1111/j.1365-2710.2010.01218.x. [DOI] [PubMed] [Google Scholar]
- 28.Simpson S, Lewanczuk R, Majumdar S, Spooner R, Tsuyuki R, Johnson J. Effect of Adding Pharmacists to Primary Care Teams on Blood Pressure Control in Patients With Type 2 Diabetes: A random-ized controlled trial. Diabetes Care. 2011;34:20–26. doi: 10.2337/dc10-1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sriram S, Chack LE, Ramasamy R, Ghasemi A, Ravi TK, Sabzghabaee AM. Impact of pharmaceutical care on quality of life in patients with type 2 diabetes mellitus. JRMS. 2011;16:412–418. [PMC free article] [PubMed] [Google Scholar]
- 30.Ali MFS, Robinson P, Phillips G, Doherty L, Melnick P, Laming L, Sinclair A, Dhillon S.Impact of community pharmacy diabetes monitoring and education programme on diabetes management: a randomized controlled study Diabetic Medicine 2012c326–c33.61.. [DOI] [PubMed] [Google Scholar]
- 31.Chan C-W, Siu S-C, Wong CKW, Lee VWY. A Pharmacist Care Program: Positive Impact on Cardiac Risk in Patients With Type 2 Diabetes. Journal of Cardiovascular Pharmacology and Therapeutics. 2012;17(1):57–64. doi: 10.1177/1074248410396216. [DOI] [PubMed] [Google Scholar]
- 32.Jacobs M, Sherry P, Taylor L, Amato M, Tataronis G, Cushing G. Pharmacist Assisted Medication Program Enhancing the Regulation of Diabetes (PAMPERED) study. J Am Pharm Assoc. 2012;52(5):613–622. doi: 10.1331/JAPhA.2012.10183. [DOI] [PubMed] [Google Scholar]
- 33.Mourão AO, Ferreira WR, Martins MA, et al. Pharmaceutical care program for type 2 diabetes patients in Brazil: a randomised controlled trial. Int J Clin Pharm. 2013;35(1):79–86. doi: 10.1007/s11096-012-9710-7. [DOI] [PubMed] [Google Scholar]
- 34.O’Connor P, Schmittdiel J, Pathak R, Harris R, Newton K, Ohnsorg K, et al. Randomized trial of telephone outreach to improve medication adherence and metabolic control in adults with diabetes. Diabete Care. 2014;37(12):3317–3324. doi: 10.2337/dc14-0596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen J, Ou H, Lin T, Lai E, Kao Y. Pharmaceutical care of elderly patients with poorly controlled type 2 diabetes mellitus: a randomized controlled trial. Int J Clin Pharm. 2016;38(1):88–95. doi: 10.1007/s11096-015-0210-4. [DOI] [PubMed] [Google Scholar]
- 36.Kirwin JL, Cunningham RJ, Sequist TD. Pharmacist Recommendations to Improve the Quality of Diabetes Care: A Randomized Controlled Trial. J Manag Care Pharm. 2010;16(2):104–113. doi: 10.18553/jmcp.2010.16.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Taveira TH, Friedmann PD, Cohen LB, Dooley AG, Khatana SAM, Pirraglia PA, et al. Pharmacist-Led Group Medical Appointment Model in Type 2 Diabetes. The Diabetes Educator. 2010;36:109–117. doi: 10.1177/0145721709352383. [DOI] [PubMed] [Google Scholar]
- 38.Jacobs M, Sherry P, Taylor L, Amato M, Tataronis G, Cushing G. Pharmacist Assisted Medication Program Enhancing the Regulation of Diabetes (PAMPERED) study. J Am Pharm Assoc. 2012;52(5):613–621. doi: 10.1331/JAPhA.2012.10183. [DOI] [PubMed] [Google Scholar]
- 39.Chung WW, Chua SS, Lai PSM, Chan SP. Effects of a pharmaceutical care model on medication adherence and glycemic control of people with type 2 diabetes. Patient Preference and Adherence. 2014;8:1185–1194. doi: 10.2147/PPA.S66619. [DOI] [PMC free article] [PubMed] [Google Scholar]
Acknowledgments
We thank our colleagues of Drug Therapy Evaluation and Management (DrugTEAM™) group including Jung Mi Oh and Jeong-Hyun Yoon for their priceless support. This study was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI13C0731).
Footnotes
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.World Health Organization [webpage on the Internet] Diabetes: Global Report on Diabetes. World Health Organization; 2016. [Accessed July 26, 2017]. Available from: http://www.who.int/diabetes/global-report/en/ [Google Scholar]
- 2.OECD [webpage on the Internet] OECD. Stat. 2015. [Accessed July 26, 2017]. Available from: http://stats.oecd.org/index.aspx?DataSetCode=HEALTH_STAT.
- 3.Sacks DB. A1C versus glucose testing: a comparison. Diabetes Care. 2011;34(2):518–523. doi: 10.2337/dc10-1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nathan DM, Genuth S, Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 5.UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–853. [PubMed] [Google Scholar]
- 6.Nathan D, Cleary P, Backlund J, Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643–2653. doi: 10.1056/NEJMoa052187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Diabetes Association Standards of medical care in diabetes – 2012. Diabetes Care. 2012;35(suppl 1):S11–S63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization . Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. Geneva: World Health Organization; 2013. [Google Scholar]
- 9.American Pharmacists Association, The National Association of Chain Drug Stores Foundation Medication therapy management in pharmacy practice. Core elements of an MTM service model version 2.0. J Am Pharm Assoc (2003) 2008;48(3):341–353. doi: 10.1331/JAPhA.2008.08514. [DOI] [PubMed] [Google Scholar]
- 10.Wermeille J, Bennie M, Brown I, Mcknight J. Pharmaceutical care model for patients with type 2 diabetes: integration of the community pharmacist into the diabetes team – a pilot study. Pharm World Sci. 2004;26(1):18–25. doi: 10.1023/b:phar.0000013465.24857.a8. [DOI] [PubMed] [Google Scholar]
- 11.Santschi V, Chiolero A, Colosimo AL, et al. Improving blood pressure control through pharmacist interventions: a meta-analysis of randomized controlled trials. J Am Heart Assoc. 2014;3(2):e000718. doi: 10.1161/JAHA.113.000718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koshman SL, Charrois TL, Simpson SH, Mcalister FA, Tsuyuki RT. Pharmacist care of patients with heart failure: a systematic review of randomized trials. Arch Intern Med. 2008;168(7):687–694. doi: 10.1001/archinte.168.7.687. [DOI] [PubMed] [Google Scholar]
- 13.Machado M, Bajcar J, Guzzo GC, Einarson TR. Sensitivity of patient outcomes to pharmacist interventions. Part I: systematic review and meta-analysis in diabetes management. Ann Pharmacother. 2007;41(10):1569–1582. doi: 10.1345/aph.1K151. [DOI] [PubMed] [Google Scholar]
- 14.Li X, Mao M, Ping Q. Effect of pharmaceutical care programs on glycemic control in patients with diabetes mellitus: a meta-analysis of randomized controlled trials. J Pharm Technol. 2010;26(5):255–263. [Google Scholar]
- 15.Poolsup N, Suksomboon N, Intarates M. Effect of pharmacist’s interventions on glycemic control in diabetic patients: a systematic review and meta-analysis of randomized controlled trials. Mahidol Univ J Pharm Sci. 2013;40(4):17–30. [Google Scholar]
- 16.Edelman D, Fredrickson SK, Melnyk SD, et al. Medical clinics versus usual care for patients with both diabetes and hypertension: a random-ized trial. Ann Intern Med. 2010;152(11):689–696. doi: 10.7326/0003-4819-152-11-201006010-00001. [DOI] [PubMed] [Google Scholar]
- 17.Kraemer DF, Kradjan WA, Bianco TM, Low JA. A randomized study to assess the impact of pharmacist counseling of employer-based health plan beneficiaries with diabetes: the EMPOWER study. J Pharm Pract. 2012;25(2):169–179. doi: 10.1177/0897190011418513. [DOI] [PubMed] [Google Scholar]
- 18.Jameson JP, Baty PJ. Pharmacist collaborative management of poorly controlled diabetes mellitus: a randomized controlled trial. Am J Manag Care. 2010;16(4):250–255. [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 20.The World Bank [webpage on the Internet] [Accessed July 26, 2017]. Data Available from: https://data.worldbank.org/income-level/high-income.
- 21.The Editorial Team of Effective Practice and Organisation of Care (EPOC), Cochrane Effective Practice and Organisation of Care (EPOC) [webpage on the Internet] EPOC Resources for Review Authors. Cochrane Library; 2017. [Accessed July 26, 2017]. Available from: http://epoc.cochrane.org/epoc-resources-review-authors. [Google Scholar]
- 22.Harbord RM, Egger M, Sterne JA. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med. 2006;25(20):3443–3457. doi: 10.1002/sim.2380. [DOI] [PubMed] [Google Scholar]
- 23.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Makeen HA. Clinical pharmacists as medication therapy experts in diabetic clinics in Saudi Arabia – not just a perception but a need. Saudi Pharm J. 2017;25(6):939–943. doi: 10.1016/j.jsps.2017.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cheung BM, Ong KL, Cherny SS, Sham PC, Tso AW, Lam KS. Diabetes prevalence and therapeutic target achievement in the United States, 1999 to 2006. Am J Med. 2009;122(5):443–453. doi: 10.1016/j.amjmed.2008.09.047. [DOI] [PubMed] [Google Scholar]
- 26.Farsaei S, Sabzghabaee AM, Zargarzadeh AH, Amini M. Effect of pharmacist-led patient education on glycemic control of type 2 diabetics: a randomized controlled trial. J Res Med Sci. 2011;16(1):43–49. [PMC free article] [PubMed] [Google Scholar]
- 27.Obreli-Neto PR, Guidoni CM, de Oliveira Baldoni A, et al. Effect of a 36-month pharmaceutical care program on pharmacotherapy adherence in elderly diabetic and hypertensive patients. Int J Clin Pharm. 2011;33(4):642–649. doi: 10.1007/s11096-011-9518-x. [DOI] [PubMed] [Google Scholar]
- 28.Mahwi TO, Obied KA. Role of the pharmaceutical care in the management of patients with type 2 diabetes mellitus. IJPSR. 2013;4(4):1363–1369. [Google Scholar]
- 29.Samtia AM, Rasool MF, Ranjha NM, Usman F, Javed I. A multifactorial intervention to enhance adherence to medications and disease-related knowledge in type 2 diabetic patients in Southern Punjab, Pakistan. Trop J Pharm Res. 2013;12(5):851–856. [Google Scholar]
- 30.Wishah RA, Al-Khawaldeh OA, Albsoul AM. Impact of pharmaceutical care interventions on glycemic control and other health-related clinical outcomes in patients with type 2 diabetes: randomized controlled trial. Diabetes Metab Syndr. 2015;9(4):271–276. doi: 10.1016/j.dsx.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 31.Cani CG, Lopes LS, Queiroz M, Nery M. Improvement in medication adherence and self-management of diabetes with a clinical pharmacy program: a randomized controlled trial in patients with type 2 diabetes undergoing insulin therapy at a teaching hospital. Clinics. 2015;70(2):102–106. doi: 10.6061/clinics/2015(02)06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jahangard-Rafsanjani Z, Sarayani A, Nosrati M, et al. Effect of a community pharmacist-delivered diabetes support program for patients receiving specialty medical care: a randomized controlled trial. Diabetes Educ. 2015;41(1):127–135. doi: 10.1177/0145721714559132. [DOI] [PubMed] [Google Scholar]
- 33.Lim PC, Lim K, Embee ZC, Hassali MA, Thiagarajan A, Khan TM. Study investigating the impact of pharmacist involvement on the outcomes of diabetes medication therapy adherence program Malaysia Pak. J Pharm Sci. 2016;29(2):595–601. [PubMed] [Google Scholar]
- 34.Mourão AO, Ferreira WR, Martins MA, et al. Pharmaceutical care program for type 2 diabetes patients in Brazil: a randomised controlled trial. Int J Clin Pharm. 2013;35(1):79–86. doi: 10.1007/s11096-012-9710-7. [DOI] [PubMed] [Google Scholar]
- 35.Jarab AS, Alqudah SG, Mukattash TL, Shattat G, Al-Qirim T. Random-ized controlled trial of clinical pharmacy management of patients with type 2 diabetes in an outpatient diabetes clinic in Jordan. J Manag Care Pharm. 2012;18(7):516–526. doi: 10.18553/jmcp.2012.18.7.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Quinn CC, Shardell MD, Terrin ML, Barr EA, Ballew SH, Gruber-Baldini AL. Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care. 2011;34(9):1934–1942. doi: 10.2337/dc11-0366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bu D, Pan E, Walker J, et al. Benefits of information technology-enabled diabetes management. Diabetes Care. 2007;30(5):1137–1142. doi: 10.2337/dc06-2101. [DOI] [PubMed] [Google Scholar]
- 38.Alhodaib H, [webpage on the Internet] Information Technology in DM: DIAPEDIA: The living Textbook of Diabetes. 2014. [Accessed July 26, 2017]. Available from: https://www.diapedia.org/81040851628/rev/7.
- 39.Kicklighter CE, Nelson KM, Humphries TL, Delate T. An evaluation of a clinical pharmacy-directed intervention on blood pressure control. Pharm Pract (Granada) 2006;4(3):110–116. [PMC free article] [PubMed] [Google Scholar]
- 40.Kontopantelis E, Springate DA, Reeves D. A re-analysis of the Cochrane Library data: the dangers of unobserved heterogeneity in meta-analyses. PLoS One. 2013;8(7):e69930. doi: 10.1371/journal.pone.0069930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kontopantelis E, Reeves D. Performance of statistical methods for meta-analysis when true study effects are non-normally distributed: a simulation study. Stat Methods Med Res. 2012;21(4):409–426. doi: 10.1177/0962280210392008. [DOI] [PubMed] [Google Scholar]
- 42.Jaber LA, Halapy H, Fernet M, Tunmalapalli S, Diwakaran A. Evaluation of a pharmaceutical care model on diabetes management. The Annals of Pharmacotherapy. 1996;30:238–243. doi: 10.1177/106002809603000305. [DOI] [PubMed] [Google Scholar]
- 43.Clifford RM, Batty KT, Davis TME, Davis W, Stein G, Stewart G, et al. A randomised controlled trial of a pharmaceutical care programme in high-risk diabetic patients in an outpatient clinic. Int J Pharm Pract. 2002;10:85–89. [Google Scholar]
- 44.Raji A, Gomes H, Beard JO, MacDonald P, Conlin PR. A randomized trial comparing intensive and passive education in patients with Diabetes Mellitus. Arch Intern Med. 2002;162:1301–1304. doi: 10.1001/archinte.162.11.1301. [DOI] [PubMed] [Google Scholar]
- 45.Choe HM, Mitrovich S, Dubay D, Hayward RA, Krein SL, Vijan S. Proactive case management of high-risk patients with type 2 diabetes mellitus by a clinical pharmacist: a randomized controlled trial. Am J Manag Care. 2005;11:253–260. [PubMed] [Google Scholar]
- 46.Clifford RM, Davis WA, Batty KT, Davis TME. Effect of a Pharmaceutical Care Program on Vascular Risk Factors in Type 2 Diabetes: The Fremantle Diabetes Study. Diabetes Care. 2005;28:771–776. doi: 10.2337/diacare.28.4.771. [DOI] [PubMed] [Google Scholar]
- 47.Rothman R, Malone R, Bryant B, Shintani AK, Crigler B, Dewalt DA, et al. A randomized trial of a primary care–based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetes. The American Journal of Medicine. 2005;118:276–284. doi: 10.1016/j.amjmed.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 48.Suppapitiporn S, Chindavijak B, Onsanit S. Effects of Diabetes Drug Counseling by Pharmacist, Diabetic Disease Booklet and Special Medication Containers on Glycemic Control of Type 2 Diabetes Mellitus. J Med Assoc of Thai. 2005;88(Suppl 4):S134–S141. [PubMed] [Google Scholar]
- 49.Fornos JA, ´s NFA, ´s JCA, Guerra MM, Egea B. A pharmacotherapy follow-up program in patients with type-2 diabetes in community pharmacies in Spain. Pharm World Sci. 2006;28:65–72. doi: 10.1007/s11096-006-9003-0. [DOI] [PubMed] [Google Scholar]
- 50.Scott DMT, Boyd S, Stephan M, Augustine SC, Reardon TP. Outcomes of pharmacist-managed diabetes care services in a community health center. Am J Health-Syst Pharm. 2006;63:2116–2122. doi: 10.2146/ajhp060040. [DOI] [PubMed] [Google Scholar]
- 51.Krass I, Armour CL, Mitchell B, Brillant M, Dienaar R, Hughes J, et al. The Pharmacy Diabetes Care Program: assessment of a community pharmacy diabetes service model in Australia. Diabetic Medicine. 2007;24:677–683. doi: 10.1111/j.1464-5491.2007.02143.x. [DOI] [PubMed] [Google Scholar]
- 52.Phumipamorn S, Pongwecharak J, Soorapan S, Pattharachayakul S. Effects of the pharmacist’s input on glycaemic control and cardiovascular risks in Muslim diabetes. Prim Care Diabetes. 2008;2(1):31–37. doi: 10.1016/j.pcd.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 53.Mazroui NRA, Kamal MM, Ghabash NM, Yacout TA, Kole PL, McElnay JC. Influence of pharmaceutical care on health outcomes in patients with Type 2 diabetes mellitus. Br J Clin Pharmacol. 2008;67(5):547–557. doi: 10.1111/j.1365-2125.2009.03391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kirwin JL, Cunningham RJ, Sequist TD. Pharmacist Recommendations to Improve the Quality of Diabetes Care: A Randomized Controlled Trial. J Manag Care Pharm. 2010;16(2):104–113. doi: 10.18553/jmcp.2010.16.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Taveira TH, Friedmann PD, Cohen LB, Dooley AG, Khatana SAM, Pirraglia PA, et al. Pharmacist-Led Group Medical Appointment Model in Type 2 Diabetes. The Diabetes Educator. 2010;36:109–117. doi: 10.1177/0145721709352383. [DOI] [PubMed] [Google Scholar]
- 56.Cohen LB, Taveira TH, Khatana SAM, Dooley AG, Pirraglia PA, Wu W-C. Pharmacist-Led Shared Medical Appointments for Multiple Cardiovascular Risk Reduction in Patients With Type 2 Diabetes. The Diabetes Educator. 2011;37:800–809. doi: 10.1177/0145721711423980. [DOI] [PubMed] [Google Scholar]
- 57.Mehuys E, Bortel LV, Bolle LD, Tongelen IV, Tongelen LA, Annemans L, et al. Effectiveness of a community pharmacist intervention in diabetes care: a randomized controlled trial. Journal of Clinical Pharmacy and Therapeutics. 2011;36:602–613. doi: 10.1111/j.1365-2710.2010.01218.x. [DOI] [PubMed] [Google Scholar]
- 58.Simpson S, Lewanczuk R, Majumdar S, Spooner R, Tsuyuki R, Johnson J. Effect of Adding Pharmacists to Primary Care Teams on Blood Pressure Control in Patients With Type 2 Diabetes: A random-ized controlled trial. Diabetes Care. 2011;34:20–26. doi: 10.2337/dc10-1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sriram S, Chack LE, Ramasamy R, Ghasemi A, Ravi TK, Sabzghabaee AM. Impact of pharmaceutical care on quality of life in patients with type 2 diabetes mellitus. JRMS. 2011;16:412–418. [PMC free article] [PubMed] [Google Scholar]
- 60.Ali MFS, Robinson P, Phillips G, Doherty L, Melnick P, Laming L, Sinclair A, Dhillon S. Impact of community pharmacy diabetes monitoring and education programme on diabetes management: a randomized controlled study. Diabetic Medicine. 2012:c326–c333. doi: 10.1111/j.1464-5491.2012.03725.x. [DOI] [PubMed] [Google Scholar]
- 61.Chan C-W, Siu S-C, Wong CKW, Lee VWY. A Pharmacist Care Program: Positive Impact on Cardiac Risk in Patients With Type 2 Diabetes. Journal of Cardiovascular Pharmacology and Therapeutics. 2012;17(1):57–64. doi: 10.1177/1074248410396216. [DOI] [PubMed] [Google Scholar]
- 62.Jacobs M, Sherry P, Taylor L, Amato M, Tataronis G, Cushing G. Pharmacist Assisted Medication Program Enhancing the Regulation of Diabetes (PAMPERED) study. J Am Pharm Assoc. 2012;52(5):613–621. doi: 10.1331/JAPhA.2012.10183. [DOI] [PubMed] [Google Scholar]
- 63.O’Connor P, Schmittdiel J, Pathak R, Harris R, Newton K, Ohnsorg K, et al. Randomized trial of telephone outreach to improve medication adherence and metabolic control in adults with diabetes. Diabete Care. 2014;37(12):3317–3324. doi: 10.2337/dc14-0596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chung WW, Chua SS, Lai PSM, Chan SP. Effects of a pharmaceutical care model on medication adherence and glycemic control of people with type 2 diabetes. Patient Preference and Adherence. 2014;8:1185–1194. doi: 10.2147/PPA.S66619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chen J, Ou H, Lin T, Lai E, Kao Y. Pharmaceutical care of elderly patients with poorly controlled type 2 diabetes mellitus: a randomized controlled trial. Int J Clin Pharm. 2016;38(1):88–95. doi: 10.1007/s11096-015-0210-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Publication bias visualized by funnel plot.
Abbreviation: SDM, standard difference in mean values.
Table S1.
The changes in HbA1C between PC group and UC group
| Study ID | Intervention group
|
Control group
|
Sample size
|
P-value | |||
|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | PC | UC | ||
| Jaber 199612 | 11.5±2.9 | 9.2±2.1 | 12.2±3.5 | 12.1±3.7 | 17 | 22 | 0.003 |
| Clifford 200213 | 8.4±1.4 | 8.2±1.5 | 8.5±1.6 | 8.1±1.6 | 48 | 25 | >0.05 |
| Raji 200214 | 9.9±1.3 | 8±1.4 | 9.8±1.2 | 8.6±1.8 | 50 | 56 | 0.03 |
| Choe 200515 | 10.1±1.8 | 8±1.4 | 10.2±1.7 | 9.3±2.1 | 29 | 36 | 0.03 |
| Clifford 200516 | −0.5 (−0.7 to −0.3) | 0 (−0.2 to 0.2) | 92 | 88 | 0.002 | ||
| Rothman 200517 | 0.8 (0–1.7%) | 112 | 105 | 0.05 | |||
| Suppapitiporn 200518 | 8.16±1.44 | 7.91±1.27 | 8.01±1.51 | 8.8±1.36 | 180 | 180 | 0.001 |
| Fornos 200619 | 8.4±1.8 | 7.9±1.7 | 7.8±1.7 | 8.5±1.9 | 56 | 56 | 0.001 |
| Scott 200620 | 8.8±1.72 | 7.08±1.72 | 8.7±0.7 | 8±0.7 | 64 | 67 | 0.012 |
| Krass 200721 | 8.9±1.4 | 7.9±1.2 | 8.3±1.3 | 8.0±1.2 | 125 | 107 | <0.01 |
| Phumipamorn 200822 | 8.7±1.5 | 7.9±1.4 | 8.7±1.6 | 8.1±1.9 | 63 | 67 | 0.56 |
| Al Mazroui 200923 | 8.5 (8.3–8.7) | 6.9 (6.7–7.1) | 8.4 (8.2–8.6) | 8.3 (8.1–8.5) | 117 | 117 | 0.001 |
| Edelman 20101 | 9.2 | 8.3 | 9.2 | 8.6 | 133 | 106 | 0.159 |
| −0.33 (−0.80 to 0.13) | |||||||
| Farsaei 201024 | 9.3±1.7 | 7.5±1.6 | 8.9±1.1 | 9.0±1.2 | 87 | 87 | >0.05 |
| Jameson 201025 | −1.5 (−0.03 to −2.68) | −0.40 (0.5 to −2.10) | 52 | 51 | 0.06 | ||
| Cohen 201126 | −0.41 (−0.74 to −0.07) | −0.20 (−0.61 to 0.21) | 50 | 49 | 0.028 | ||
| Mehuys 201127 | 7.7±1.7 | 7.1±1.1 | 7.3±1.2 | 7.2±1 | 153 | 135 | 0.009 |
| Obreli-Neto 20113 | −0.7 (−0.9 to 0.5) | 0.0 (−0.1 to 0.1) | 97 | 97 | 0.001 | ||
| Simpson 201128 | −0.15 (−0.36 to 0.05) | 0.03 (−0.22 to 0.28) | 131 | 129 | <0.05 | ||
| Siriam 201129 | 8.44±0.29 | 6.73±0.21 | 9.03±0.46 | 8.3±0.16 | 60 | 60 | 0.010 |
| Ali 201230 | 8.2±1.65 | 6.6±0.59 | 8.1±0.97 | 7.5±0.64 | 23 | 23 | 0.001 |
| Chan 201231 | −1.57%+1.50% | −0.40%+1.19% | 51 | 54 | <0.00 | ||
| Jacobs 201232 | 9.5±1.1 | 7.7±1.3 | 9.2±1 | 8.4±1.6 | 72 | 92 | 0.003 |
| Jarab 20124 | −0.8 (−1.6 to 0.1) | 0.1 (−0.4 to 0.7) | 77 | 79 | 0.019 | ||
| Kraemer 20125 | 7.28 | 6.78 | 7.38 | 7.22 | 36 | 31 | 0.0757 |
| −0.5 (change in mean values) | −0.16 (change in mean values) | ||||||
| Mahwi 20136 | 11.53±1.83 | 9.2±2 | 9.97±2.75 | 9.5±2.1 | 62 | 61 | 0.001 |
| Mourao 201333 | −0.6 (−1.1 to −0.02) | 0.7 (0.2–1.3) | 50 | 50 | 0.001 | ||
| Samtia 20137 | 8.51±1.62 | 7.5±1.26 | 8.54±1.55 | 8.08±1.49 | 178 | 170 | 0.001 |
| O’Connor 201434 | −0.9±1.85 | −1.08±1.78 | 92 | 103 | 0.001 | ||
| Cani 20158 | 9.78±1.55 | 9.21±1.41 | 9.61±1.38 | 9.53±1.68 | 34 | 36 | 0.001 |
| Jahangard-Rafsanjani 20159 | 7.6±1.6 | 6.6±1.5 | 7.5±1.9 | 7.0±1.7 | 51 | 50 | 0.09 |
| Wishah 201510 | 8.9±1.6 | 7.2±0.9 | 8.2±1.3 | 7.9±1.3 | 52 | 54 | >0.05 |
| Chen 201635 | 9.22±1.7 | 8.39±1.2 | 8.94±1.5 | 9.37±1.5 | 50 | 50 | 0.002 |
| Lim 201611 | 10.11±0.26 | 9.21±0.27 | 9.71±0.34 | 9.63±0.29 | 39 | 37 | 0.001 |
Abbreviations: PC, pharmacist care; UC, usual care.
Table S2.
Proportion of patients achieving HbA1c goal between PC group and UC group
| Study ID | Goal | Intervention group
|
Control group
|
||
|---|---|---|---|---|---|
| Total (n) | Event (n) | Total (n) | Event (n) | ||
| Scott 200620 | A1C<7% | 64 | 24 | 67 | 4 |
| Kirwin 201036 | A1C<7% | 150 | 65 | 151 | 57 |
| Taveira 201037 | A1C<7% | 58 | 23 | 51 | 11 |
| Cohen 201126 | A1C<7% | 50 | 20 | 49 | 10 |
| Mehuys 201127 | A1C<7% | 153 | 80 | 135 | 67 |
| Obreli-Neto 20113 | A1C<7% | 97 | 19 | 97 | 1 |
| Chan 201231 | A1C<7% | 51 | 3 | 54 | 0 |
| Jacobs 201238 | A1C<7% | 55 | 19 | 67 | 14 |
Abbreviations: PC, pharmacist care; UC, usual care.
Table S3.
Quality check for included studies (randomized controlled studies) by EPOC risk of bias
| Study ID | Sequence generation | Allocation concealment | Baseline outcome measurements | Baseline characteristics | Incomplete outcome data | Blinding of participants, personnel | Protection against contamination | Selective outcome reporting | Other sources of bias |
|---|---|---|---|---|---|---|---|---|---|
| Jaber 199612 | Unclear | Unclear | Low | Low | Low | Unclear | Unclear | Low | Unclear |
| Clifford 200213 | Low | Unclear | Low | Low | Low | Unclear | Unclear | Low | Unclear |
| Raji 200214 | Unclear | Unclear | Low | Low | Low | Unclear | Unclear | Low | Unclear |
| Choe 200515 | Low | Unclear | Low | Low | Low | High | Low | Low | Unclear |
| Clifford 200516 | Unclear | Unclear | Low | Low | Low | Low | Low | Low | Unclear |
| Rothman 200517 | Low | Low | Low | Low | Low | Unclear | Low | Low | Unclear |
| Suppapitiporn 200518 | Unclear | Unclear | Low | Low | Low | Unclear | Unclear | Low | Unclear |
| Fornos 200619 | Low | Unclear | Low | Low | Low | High | Low | Unclear | Unclear |
| Scott 200620 | Low | Unclear | Low | Low | Low | High | Low | Unclear | Unclear |
| Krass 200721 | Unclear | Unclear | Low | Low | Low | High | Low | Low | Unclear |
| Phumipamorn 200822 | Low | High | Unclear | Unclear | Low | Unclear | Low | Low | Unclear |
| Al Mazroui 200923 | Unclear | Unclear | Low | Low | Unclear | Unclear | Unclear | Low | Unclear |
| Edelman 20101 | Low | Unclear | Low | Low | Unclear | High | Low | Low | Unclear |
| Farsaei 201024 | Unclear | Unclear | Low | Low | Unclear | Unclear | Unclear | Low | Unclear |
| Jameson 20102 | Low | Low | Low | Low | Low | High | Unclear | Low | Unclear |
| Kirwin 201036 | Unclear | Unclear | High | Low | Unclear | Unclear | High | High | Unclear |
| Taveira 201037 | Low | Unclear | High | High | Unclear | Unclear | Unclear | High | Unclear |
| Cohen 201126 | Unclear | Unclear | Low | Low | Low | Unclear | Low | Low | Unclear |
| Mehuys 201127 | Low | Unclear | Low | Low | Unclear | Unclear | Unclear | Low | Unclear |
| Obreli-Neto 20113 | Low | Unclear | Low | Low | High | High | Unclear | Low | Unclear |
| Simpson 201128 | Low | Unclear | Low | Low | Unclear | Low | Low | Low | Low |
| Siriam 201129 | Unclear | Unclear | Low | Low | Low | Low | Unclear | Low | Unclear |
| Ali 201230 | Low | Low | Low | Low | Low | Unclear | Low | Low | Unclear |
| Chan 201231 | Low | Low | Low | Low | Unclear | Unclear | Unclear | Low | Unclear |
| Jacobs 201232 | Low | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Low | Unclear |
| Jarab 20124 | Low | Unclear | Low | Low | Low | Unclear | Unclear | Low | Unclear |
| Kraemer 20125 | Low | Unclear | Low | Low | Unclear | Unclear | Unclear | Low | Unclear |
| Mahwi 20136 | Low | Low | Low | Low | Unclear | Unclear | Unclear | Low | Unclear |
| Mourao 201333 | Low | Unclear | Low | Low | Low | Unclear | Unclear | Unclear | Unclear |
| Samtia 20137 | Unclear | Unclear | Low | Low | Unclear | Unclear | Unclear | Low | Unclear |
| Chung 201439 | Unclear | Unclear | Low | Low | Low | Low | Low | Unclear | Unclear |
| O’Connor 201434 | Low | Low | Low | Low | Low | Low | Unclear | Low | Unclear |
| Cani 20158 | Unclear | Unclear | Low | Low | Low | Low | Unclear | Low | Unclear |
| Jahangard-Rafsanjani | Low | Low | Low | Low | Low | Low | Unclear | Low | Unclear |
| 20159 | |||||||||
| Wishah 201510 | Low | Low | Low | Low | Low | Low | Unclear | Low | Unclear |
| Chen 201635 | Low | Low | Low | Low | Unclear | Unclear | Unclear | Low | Unclear |
| Lim 201611 | Unclear | Unclear | Low | Low | Low | Low | Unclear | Low | Unclear |
Abbreviation: EPOC, Effective Practice and Organization of Care.