Abstract
Background:
The Global Unite Shoulder System is the next generation of implant from the Depuy Global Shoulder line. The primary feature of the Global Unite is adaptability through the interchangeable modular bodies, modular suture collars, and stems. Short-term functional and radiographic outcomes of the Global Unite Platform Shoulder System were assessed as well as complication and revision rates.
Methods:
95 subjects were enrolled prospectively between 2013 and 2015 that underwent anatomic or reverse shoulder arthroplasty utilizing the DePuy Global Unite Anatomic Platform Shoulder System. Functional outcome data (ASES and SANE) as well as radiographic data was collected on these patients pre-operatively, and at 6 months, 1 year and 2 years post-operatively.
Results:
The cohort consisted of 97 shoulders in 95 patients of which 54 (56.8%) are males and 41 (43.2%) are female. There were 55/97 (56.7%) were primary anatomic total shoulder arthroplasties, 37/97 (38.1%) primary reverse shoulder arthroplasties, and 3/97 (3.1%) revision procedures to a reverse shoulder arthroplasty. Outcome scores demonstrated an increase in ASES score from a mean of 33.00 to 79.56 and SANE score of 21.30 to 84.08.
Conclusion:
The Depuy Global Unite shoulder system demonstrated very good short-term results in this two-year outcome study. Functional outcome scores are similar to current literature for anatomic and reverse primary cases. Radiographic measures at two years are promising with only 2 cases of grade 1 scapular notching and one case of grade 2 scapular notching. Overall the Depuy Global Unite is a versatile shoulder system with very good early outcomes.
Key Words: Anatomic total shoulder arthroplasty, Convertible, Modular, Reverse shoulder arthroplasty, Revision shoulder arthroplasty
Introduction
Shoulder arthroplasty dates to the late 1800s, when platinum and rubber prosthesis were implanted for the treatment of joint disease due to tuberculosis (1). In the 1950s Neer developed first a hemiarthroplasty, then ultimately the first modern design of a total shoulder arthroplasty (2, 3). Constrained reverse ball-and-socket prosthesis were introduced in the 1970s for treatment of arthritis with rotator cuff tears. Due to the high mechanical failure rate, this led to semi-constrained reverse arthroplasty systems, specifically the Grammont style prosthesis in the 1980s (4). The medialized center of rotation decreased the forces of the glenosphere and baseplate fixation, allowing for increased implant longevity (5). Today shoulder hemiarthroplasty, total shoulder arthroplasty, and reverse total shoulder arthroplasty are used to treat a wide range of conditions including glenohumeral arthritis, rotator cuff arthropathy, proximal humerus fractures, rotator cuff tears, and osteonecrosis (6).
DePuy first introduced the Global Unite Shoulder System in 2013 focusing on features on adaptability while maintaining the simplicity of a single arthroplasty system for anatomic, reverse, and fracture management. The system, composed of interchangeable modular bodies and stems, is designed to better recreate the patient’s anatomy, while an optional suture collar is available to aid in reconstruction of the tuberosities. Additionally, the system is convertible to a reverse by integrating with the Delta Xtend epiphyseal and glenoid components with the ability of version correction.
The goal of this study was to examine the short-term functional outcomes, radiographic results, and revision rates of patients treated with the Global Unite Platform Shoulder System. Both primary and revision arthroplasty patients were followed for a minimum of 2 years from their surgery. Anatomic and reverse arthroplasty patients were included in the study.
Materials and Methods
This is a prospective, Institutional Review Board approved study. Between August 2013 and September 2015, at a single institution, 97 shoulders in 95 patients underwent anatomic or reverse shoulder arthroplasty by the senior authors (GRW, SN, JAA), utilizing the DePuy Global Unite Anatomic Platform Shoulder System. Two of the 95 patients who were included in the study underwent staged bilateral shoulder arthroplasty. These shoulders were treated independently for all outcome and data analysis purposes. The mean age of the patients at surgery was 71 years (46 to 96). There were 41 men and 54 women. Of the 97subjects who underwent primary or revision anatomic or reverse total shoulder arthroplasty, outcome data were available for 89 with 6-months follow-up, 77 at 1-year, and 64 at 2-years postoperative. In some cases, at time of follow-up, either outcome scores or radiographic data was missing. Ninety-two procedures were primary arthroplasty, while five were revision from prior arthroplasty. Of the five revision procedures, none were performed on patients who underwent primary arthroplasty as part of this study. The primary outcome of this study was to determine implant survivorship during this time, which was evaluated by the removal or intended removal of the device, validated outcome scores were the secondary outcome measures.
Surgical Technique
The operations were performed under general anesthesia with interscalene block, unless contrain-dicated or patient refused regional anesthesia. All procedures were performed through a deltopectoral exposure except one in which a superior deltoid split was performed was during a primary reverse shoulder arthroplasty. A subscapularis peel or lesser-tuberosity osteotomy was used in all exposures, as selected by the surgeon based on preferred method. The subscapularis was repaired after implantation. Postoperative rehabilitation included sling immobilization for 2 weeks followed by the initiation of passive range-of-motion exercises at 2-4 weeks, active range-of-motion exercises at 4-8 weeks and incorporation of strengthening from weeks 12-20.
Assessment
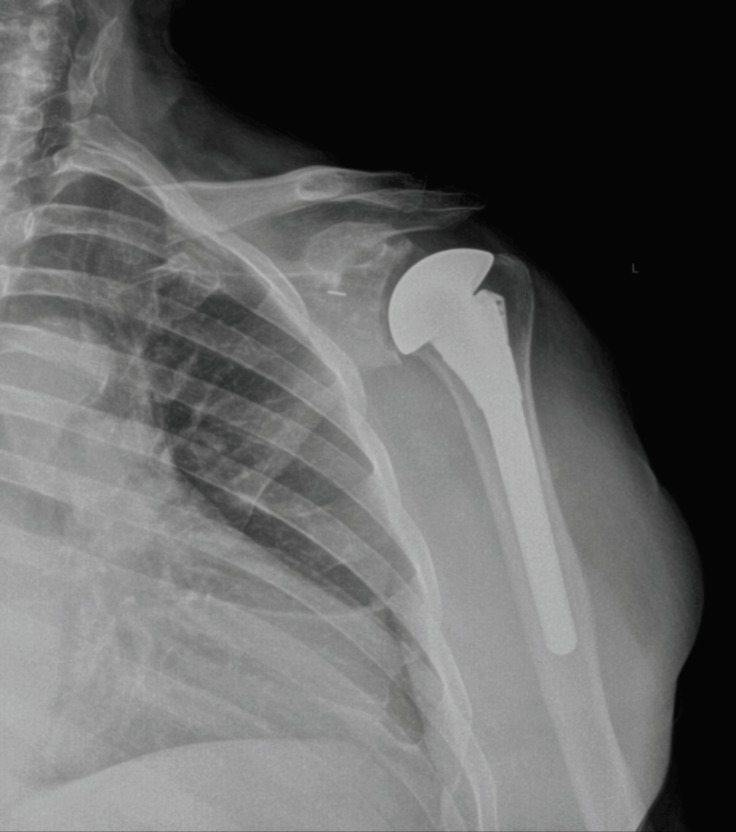
All patients were assessed prior to surgery using the American Shoulder and Elbow Surgeons (ASES) Assessment and the Single Assessment Numerical Evaluation (SANE). Radiographs were obtained and reviewed for acromion-greater tuberosity distance (AGT) and acromial-humeral interval using at anteroposterior series in external rotation. Primary cases were classified according to Favard, Hamada, and Sirveaux (7-9). Demographic and surgical information including post-operative complications were collected for analysis of contributing factors including age, sex, operative side, height, weight, body mass index (BMI), surgical approach, size of implants (humeral stem and glenosphere), and prior procedures. At time of follow-up ASES and SANE scores were again obtained. Post-operative radiographs were evaluated for acromion-greater tuberosity distance, stem position, and scapular notching [Figure 1].
Figure 1.
Radiographs of the left shoulder of an 81-year-old male after anatomic TSA with a DePuy Global Unite
Results
Demographics
The cohort of all patients, consisting of both anatomic and reverse arthroplasty as primary and revision procedures includes 97 shoulders in 95 patients, of which 41 are male and 54 are female [Table 1]. There were fifty-five primary anatomic total shoulder arthroplasties and thirty-seven primary reverse shoulder arthroplasties. There were two revision procedures to an anatomic total shoulder arthroplasty and three revision procedures to a reverse shoulder arthroplasty. Sixty-two cases were performed on the right side and thirty-five on the left. The average age of the complete cohort at time of surgery was 71 years (range 46 to 96), and a subject’s average age at the 2-year follow-up visit was 72 years (range 46 to 88). The average weight, height, and BMI of the complete cohort was 182.33 lbs. (range 98 to 335), 65.9 inches (range 59-73), and 29.55 kg/m2 (range 19 to 51). Those who subjects who attended a 2-year follow-up visit, had an average weight of 187.22 lbs. (range 98 to 335), an average height of 66.1 inches (range 59-73), and an average BMI of 30.11 kg/m2 (range 19 to 51).
Table 1.
Patient Characteristics of Complete Cohort at Time of Surgery
| All Cases (n=97) | Primary Anatomic (n=55) | Primary Reverse (n=37) | Revision to Anatomic (n=2) | Revision to Reverse (N=3) | |
|---|---|---|---|---|---|
|
Age at Surgery (Years)
Mean ± Standard Deviation |
71.49 ± 8.49 | 70.38 ± 7.34 | 74.07 ± 8.68 | 53.37 ± 7.73 | 72.34 ± 6.84 |
| Male | Female Patients | 42 | 55 | 27 | 28 | 11 | 26 | 0 | 2 | 1 | 2 |
| Right Side Involved (%) | 63.9% | 58.1% | 67.6% | 100% | 100% |
|
BMI (kg/m
2
)
Mean ± Standard Deviation |
29.55 ± 5.62 | 29.24 ± 5.69 | 29.95 ± 5.26 | 26.50 ± 7.73 | 32.23 ± 7.50 |
Primary Anatomic Total Shoulder Arthroplasty
The average age of the fifty-five primary anatomic total shoulder arthroplasty cases at the time of surgery was 70.38 ± 7.34 years. Twenty-seven cases were performed in males and twenty-eight in females. The average weight was 184.29 ± 38.68 pounds. The average height was 66.6 ± 3.84inches. The average BMI was 29.24 ± 5.69 kg/m2. The surgery was performed on the right side in 32 patients (58.1%). All cases were performed through a deltopectoral approach. Thirty-eight cases utilized a standard Anchor Peg Glenoid®, fifteen cases utilized a Steptech Anchor Peg Glenoid®, while two cases utilized an inlay mini-glenoid in the setting of glenoid deficiency.
Preoperative radiographs were available for all fifty-five patients while ASES and SANE scores were available for 54 patients. The mean preoperative AGT distance measured 14.19 ± 5.22mm, while the mean preoperative AH distance measured 8.01 ± 3.54mm. The preoperative Favard classification for primary anatomic cases were: 21 Favard Group A, 28 Favard Group B, and 6 Favard Group C. The preoperative Hamada classification for primary cases were: 29 at Grade 1, 0 at Grade 2, 5 at Grade 3, 15 at Grade 4, and 6 at Grade 5. The preoperative Sirveaux classification for primary cases was: 7 at E0, 26 at E1, 9 at E2, and 13 at E3. Preoperative mean ASES score was 37.38 ± 17.43 and mean SANE score was 31.16 ± 23.87.
At one-year follow-up, postoperative radiographs were available for forty-two patients (76.4%). The mean AGT distance measured 18.03 ± 6.41mm. Stem position was neutral in thirty-two patients, valgus in one, and varus in nine. There were four radiographs with proximal migration of the humerus, one with mild lesser tuberosity fragmentation, and one with calcification of the long-head of the triceps. Mean ASES score at one-year was 85.10 ± 17.34 and mean SANE score was 84.61 ± 16.79.
At two-year follow-up, postoperative radiographs were available for sixteen patients (29.1%). The mean AGT distance measured 18.01 ± 7.46 mm. Stem position was neutral in twelve patients and varus in four. There was one radiograph with proximal migration of the humerus, one with medial dislocation of the humerus, and two with calcification of the long-head of the triceps. Outcome scores, available for thirty-seven patients (67.3%), demonstrated a mean ASES score at two-years of 86.74 ± 15.51 and SANE score of 83.66 ± 19.90.
Primary Reverse Total Shoulder Arthroplasty
The average age of the thirty-seven primary reverse total shoulder arthroplasty cases at the time of surgery was 74.07 ± 8.68 years. Eleven cases were performed in males and twenty-six in females. The average weight was 177.05 ± 33.50 pounds. The average height was 64.57 ± 3.92 inches. The average BMI was 29.95 ± 5.26 kg/m2. The surgery was performed on the right side in 25 patients (67.6%). All cases were performed through a deltopectoral approach except one which was performed through a superior approach. Thirty-two cases utilized a 38mm glenosphere and five cases utilized a 42mm glenosphere.
Preoperative radiographs, ASES and SANE scores were available for thirty-one patients. Five patients did not have pre-operative evaluations and radiographic measurements because they sustained proximal humerus fractures, while for one patient the information was unavailable. The mean preoperative AGT distance measured 11.07 ± 6.73mm, while the mean preoperative AH distance measured 5.59 ± 5.50mm. The preoperative Favard classification for primary reverse cases were: 23 Favard Group A, 8 Favard Group B, and 0 Favard Group C. The preoperative Hamada classification for primary cases were: 9 at Grade 1, 1 at Grade 2, 11 at Grade 3, 8 at Grade 4, and 2 at Grade 5. The preoperative Sirveaux classification for primary cases was: 3 at E0, 19 at E1, 7 at E2, and 2 at E3. Preoperative mean ASES score was 33.00 ± 20.15 and mean SANE score was 21.30 ± 20.64.
At one-year follow-up, postoperative radiographs were available for thirty patients (81.1%). The mean AGT distance measured 33.89 ± 10.44 mm. There were four cases of Sirveaux grade 1 scapular notching. Stem position was neutral in twenty-six patients, valgus in two, and varus in two. Radiographic data showed one subject with a humeral shaft fracture, one subject with a medial dislocation of the humerus, and seven with calcification of the long-head of the triceps. Mean ASES score at one-year was 73.63 ± 17.35 and mean SANE score was 78.15 ± 14.16.
At two-year follow-up, postoperative radiographs were available for twelve patients (32.4%). The mean AGT distance measured 33.80 ± 9.09mm. There were two cases of Sirveaux grade 1 scapular notching, and one case of grade 2 scapular notching. Stem position was neutral in eleven patients and varus in one patient. There were five radiographs with calcification of the long-head of the triceps. Outcome scores, available for 23 patients (62.2%), demonstrated a mean ASES score at two-years of 79.56 ± 15.72 and SANE score of 84.08 ± 14.04.
Revision to Anatomic or Reverse Total Shoulder Arthroplasty
There were two cases in which anatomic components were placed as a revision procedure. One case was for a painful total shoulder arthroplasty and the subject underwent a humeral revision due to stem malposition with maintenance of the well-fixed glenoid component. The second case was placement of an anatomic total shoulder arthroplasty from a painful hemiarthroplasty cement spacer. The spacer had been placed for management of a prior infected humeral resurfacing implant. There was no radiographic data available at two-years and only one case (hemiarthroplasty) had outcome scores available at two years. In this case, the ASES score improved from 18 pre-operatively to 29.22 at two-years, while the SANE score improved from 12.69 to 19.97. Radiographic data for this patient at one-year follow up showed an AGT distance of 13mm with a neutral stem and no scapular notching, though calcification of the long-head of the triceps was noted.
There were three cases in which reverse components were used for revision. Two of these cases were conversions from a prior hemiarthroplasty cement spacer to a reverse total shoulder arthroplasty, while one case was revision from a prior hemiarthroplasty, placed for fracture, now with a rotator cuff tear and glenoid arthrosis. Two-year radiographic data were available for two patients (66.7%) and showed a mean AGT distance of 33.65 ± 3.15. Sirveaux grade 1 scapular notching was noted in one of the two patients with radiographs. Stem position was neutral in one patient and valgus in the other. The patient with scapular notching also had the valgus stem. Both patients were found to have calcification of the long-head of the triceps. Outcome scores were available for three patients (100%) at two-years and showed improvement from a pre-operative mean ASES score of 25.08 ± 9.48 and mean SANE score of 25.53 ± 19.89 to a mean ASES score of 80.74 ± 21.44 and mean SANE score of 78.12 ± 26.66.
Discussion
Shoulder arthroplasty procedures in the United States continue to increase, with growth rates exceeding those of hip and knee arthroplasty (10). Total shoulder arthroplasty is a proven treatment method for glenohumeral arthritis, inflammatory arthropathy of the shoulder, avascular necrosis with excellent long term results (11, 12). Similar results were found in this study utilizing the Global Unite prosthesis at two-years. ASES scores increased from a mean of 37.38 preoperatively to 86.74 at two-years, with parallel findings in the SANE score showing an increased in a mean from 31.16 to 83.66.
Reverse shoulder arthroplasty has seen excellent growth in its utilization, as well as its operative indications. While first popularized as a treatment for rotator cuff tear arthroplasty, the reverse shoulder arthroplasty is now being employed as a treatment strategy for proximal humerus fractures, glenoid bone loss in the setting of primary osteoarthritis (B2 glenoids), irreparable rotator cuff tears, posttraumatic deformity, and revision cases amongst other indications (11, 14).
The Delta Xtend reverse shoulder arthroplasty was shown by Gruber to have very good results with mean modified subjective constant score improving from 39.2 preoperative to 71.7 at 5-years postoperative (15). The mean Constant score at 5 years was 65.8 and the mean age and gender-adjusted constant score was 92%. In their study, scapular notching was found in 7/11 (64%) patients for which imaging was available. All notching was limited to Sirveaux Grade 1 or 2. These findings, as expected, are very similar to the two-year results utilizing the Delta Xtend with the Global Unite stem in our study. Of those radiographs available at two years, we found only three cases of scapular notching. Two of these cases were Sirveaux Grade 1 and one was Grade 2. Outcome scores demonstrated an increase in ASES score from a mean of 33.00 to 79.56 and SANE score mean increase of 21.30 to 84.08.
Along with increased primary procedures, revision arthroplasty burden also increases (10). One major benefit of the Global Unite system, is the ability to convert the stem from anatomic to reverse without stem removal at time of revision. Revision-to-reverse shoulder arthroplasty has been shown to have favorable results, though complication rates are double those of primary procedures (16). Convertible stems were introduced to minimize component exchange during revision procedures when converting an anatomic total shoulder arthroplasty to a reverse shoulder arthroplasty. Crosby et al. retrospectively reviewed 102 revision anatomic total shoulder arthroplasties to reverse shoulder arthroplasty, of which 29 retained the convertible-platform humeral component (17). They demonstrated shorter operative times, less blood loss, and lower complication rates in those patients where the humeral component was retained. Though none of the revisions in our study were from primary patients with a well-fixed anatomic Global Unite stem in place, we did find that the Global Unite system was well equipped to handle revision cases both to anatomic as well as reverse shoulder arthroplasty.
There were several limitations of this study. Foremost of all is number of subjects who either did not return for follow-up at 2 years or had other incomplete data, either missing outcome scores, or radiographs. Though great efforts were utilized to ensure appropriate scheduled follow-up for the prospective study, some loss to follow-up is to be expected. Also, the limited numbers of patients in the revision groups make it difficult to draw conclusions. Another limitation is that all procedures in this study were performed by high-volume shoulder arthroplasty surgeons and the results may not be reproducible in the general population (18).
The DePuy Global Unite shoulder system demonstrated very good short-term results in this two-year outcome study. This includes primary as well as revision cases utilizing both anatomic and reverse components. Functional outcome scores are similar to current literature for anatomic and reverse primary cases. Radiographic measures at two years are promising with only 2 cases of grade 1 scapular notching and one case of grade 2 scapular notching. The acromion-greater tuberosity distance was well maintained with both anatomic and reverse prosthesis. The ability to maintain the convertible stem at time of revision is another benefit of this system, though further long-term data will be needed to evaluate this as no revisions from anatomic Global Unite to reverse Global Unite with the Delta Xtend occurred in this study. Overall the DePuy Global Unite is a versatile shoulder system with very good early outcomes.
References
- 1.Lugli T. Artificial shoulder joint by péan (1893): the facts of an exceptional intervention and the prosthetic method. Clin Orthop Relat Res. 1978;133:215–8. [PubMed] [Google Scholar]
- 2.Neer CS. Articular replacement for the humeral head. J Bone Joint Surg Am. 1955;37-A(2):215–28. [PubMed] [Google Scholar]
- 3.Neer CS 2nd, Watson KC, Stanton FJ. Recent experience in total shoulder replacement. J Bone Joint Surg Am. 1982;64(3):319–37. [PubMed] [Google Scholar]
- 4.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006;15(5):527–40. doi: 10.1016/j.jse.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005;14(1 Suppl S):147S–61S. doi: 10.1016/j.jse.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 6.Williams AA, Tischler EH, Sholder D, Nicholson TA, Maltenfort MG, Getz C, et al. Identification of risk factors for abnormal postoperative chemistry labs after primary shoulder arthroplasty. Arch Bone Jt Surg. 2018;6(4):282–8. [PMC free article] [PubMed] [Google Scholar]
- 7.Favard L, Lautmann S, Clement P. Osteoarthritis with massive rotator cuff-tear: the limitation of its current definitions. Berlin: Heidelberg: Springer Berlin Heidelberg; 1999. pp. 261–5. [Google Scholar]
- 8.Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears A long-term observation. Clin Orthop Relat Res. 1990;254:92–6. [PubMed] [Google Scholar]
- 9.Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86(3):388–95. doi: 10.1302/0301-620x.86b3.14024. [DOI] [PubMed] [Google Scholar]
- 10.Day JS, Lau E, Ong KL, Williams GR, Ramsey ML, Kurtz SM. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elbow Surg. 2010;19(8):1115–20. doi: 10.1016/j.jse.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 11.Wiater JM, Fabing MH. Shoulder arthroplasty: prosthetic options and indications. J Am Acad Orthop Surg. 2009;17(7):415–25. doi: 10.5435/00124635-200907000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Deshmukh AV, Koris M, Zurakowski D, Thornhill TS. Total shoulder arthroplasty: long-term survivorship, functional outcome, and quality of life. J Shoulder Elbow Surg. 2005;14(5):471–9. doi: 10.1016/j.jse.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 13.Nicholson T, Maltenfort M, Getz C, Lazarus M, Williams G, Namdari S. Multimodal pain management protocol versus patient controlled narcotic analgesia for postoperative pain control after shoulder arthroplasty. Arch Bone Jt Surg. 2018;6(3):196–202. [PMC free article] [PubMed] [Google Scholar]
- 14.Gerber C, Pennington SD, Nyffeler RW. Reverse total shoulder arthroplasty. J Am Acad Orthop Surg. 2009;17(5):284–95. doi: 10.5435/00124635-200905000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Gruber S, Schoch C, Geyer M. The reverse shoulder arthroplasty Delta Xtend: Mid-term results. Orthopade. 2017;46(3):222–6. doi: 10.1007/s00132-016-3355-5. [DOI] [PubMed] [Google Scholar]
- 16.Austin L, Zmistowski B, Chang ES, Williams GR Jr. Is reverse shoulder arthroplasty a reasonable alternative for revision arthroplasty? Clin Orthop Relat Res. 2011;469(9):2531–7. doi: 10.1007/s11999-010-1685-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crosby LA, Wright TW, Yu S, Zuckerman JD. Conversion to reverse total shoulder arthroplasty with and without humeral stem retention: the role of a convertible-platform stem. J Bone Joint Surg Am. 2017;99(9):736–42. doi: 10.2106/JBJS.16.00683. [DOI] [PubMed] [Google Scholar]
- 18.Weinheimer KT, Smuin DM, Dhawan A. Patient Outcomes as a function of shoulder surgeon volume: a systematic review. Arthroscopy. 2017;33(7):1273–81. doi: 10.1016/j.arthro.2017.03.005. [DOI] [PubMed] [Google Scholar]