Abstract
Background:
Pilon fracture is one of the challenging injuries in orthopedic surgery. Associated soft tissue injury is an important factor in choosing treatment options. Two major methods of treatment are considered as one-stage open reduction internal fixation (ORIF) and two-stage treatment (primary external fixation and secondary ORIF). The latter is most accepted in literature. In the current study, we compared the results of these two methods.
Methods:
In a retrospective study, 41 patients were assigned to two groups containing one-stage primary ORIF (21 patients) group, and two-stage group included external fixation and secondary ORIF (20 patients). The rate of infection (superficial or deep infection, osteomyelitis), malunion, nonunion, duration of hospital stay, neurovascular injury, pain intensity, and patients’ satisfaction with AOFAS score, were compared between the two groups.
Results:
There was no significant difference between the two groups in measured variables except hospital stay which was significantly longer for the two-stage group.
Conclusion:
Based on our findings, we recommend using one stage ORIF for a patient with Pilon fractures type C and Tscherne 1, 2 if the patient is planned to be operated on during the first 24 hours after the injury.
Key Words: External fixation, Infection, Open reduction internal fixation, Pilon fracture, Two-stage surgery
Introduction
Pilon fracture accounts for 1% of lower extremity fractures and 5-7% of tibial fractures (1, 2). Despite the fact that the treatment of these fractures has been developed significantly within the recent years, best treatment has been remained difficult and challenging mainly due to severe injured soft tissue, high-energy pattern of the fracture and severe edema (2-4). Thus, the choice of an appropriate treatment remains controversial (5, 6).
Several options, having various advantages and disadvantages, have been introduced for the treatment of Pilon fractures including close reduction and casting, combined intramedullary nailing and plate fixation, open reduction and internal fixation (ORIF), minimally invasive plate osteosynthesis, external fixation (EF), the two-stage treatment with EF and ORIF (7-13).
In addition to controversies about the most superior treatment option, the appropriate time for treatment of Pilon fractures is also conflicting (14). Numerous investigators have suggested the two-stage approach including primary fixation with EF followed by definite internal fixation after soft tissue healing is the most commonly used treatment for these injuries, especially for AO/OTA type C Pilon fractures (15-18). A major drawbacks of this method is its long-term hospital stay and increased risk of infection and lack of anatomical reduction due to delayed operation (14, 19-21). For these reasons, some surgeons prefer to perform early primary ORIF, which was associated with good outcomes, especially in less severe fractures (22-24). However, once the soft tissue is severely injured, the patient must be hospitalized for a long time because of delayed wound healing and superficial or deep infection. This may necessitate several surgeries and even amputation (24-28). These complications have been reported even for minimally invasive treatment of Pilon fractures (29).
There are limited studies comparing the outcomes of primary ORIF (PORIF) and two stage approaches in treatment of Pilon fractures resulted in conflicting outcomes (14). In current prospective study, we aimed to compare the clinical, functional and radiologic outcomes and the rate of soft tissue complications in treatment of Pilon fractures with PORIF and two-stage approaches.
Materials and Methods
In a retrospective study, all patients admitted with diagnosis of Pilon farcture (AO/ OTA type 43.C) in Taleghani Hospital (Affiliated with Shaheed Beheshti University of Medical Sciences, Tehran, Iran) between 2012 and 2014 were reviewed. Among them, 10 patients were excluded due to the open fractures (2 patients), rheumatoid arthritis (2 patients), concomitant fracture in the lower limb (2 patients), severe soft tissue damage (Tscherne grade 3) (2 patients), varicose vein (one patient), and compartment syndrome (one patient). Primary ORIF was performed on 21 patients by the first author and the two-stage treatment was used by the second author. After the usual preoperative clinical and radiological examination (CT scanning and X-rays), eligible patients were asked to sign the informed consent. Research process confirmed by Taleghani Hospital ethics committee board.
The patients in the PORIF group underwent surgery within the first 24 hours after the accident using anteromedial approach, medial distal anatomical plate and additional lateral plates if necessary for Pilon fractures and one-third tubular plates for fibula fracture. In the two-stage group, the fracture was fixated using a delta frame external fixator along with fibula fixation within 24 hours after the accident [Figures 1-3]. Patients were discharged from hospital 24 to 48 hours after first stage surgery according to patients clinical examination. The definite treatment (ORIF) was performed after one to two weeks when the soft tissue inflammation resolved, [Figure 4]. The distal articular surface of the tibia was reduced through anteromedial approach. Tibial metaphyseal comminution was also fixed using medial distal tibial anatomical locking plate and lateral plates if necessary.
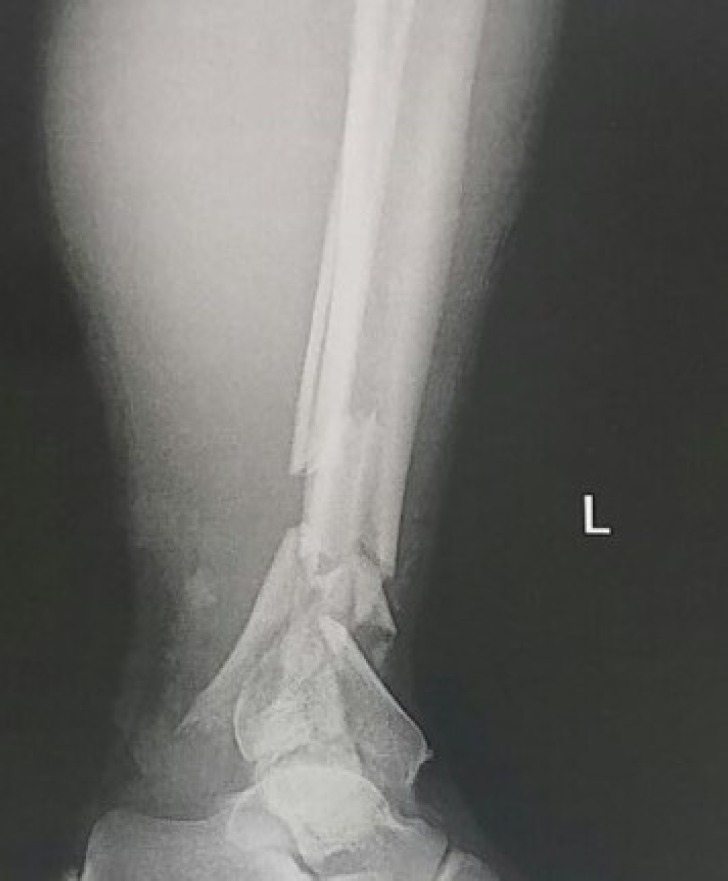
Figure 1.
Antposterior ankle xray
Figure 3.
postoperative xray after provisional fixation
Figure 4.
aostoperative xray after defenitive fixation
After the surgery, identical rehabilitation protocol was started for patients in both groups. Patients were examined clinically at 2 weeks after discharge. Clinical and radiographic examinations were performed at 4 weeks, 2, 3, 6 and 9 months post-surgery. VAS score and AOFAS score were detected at the final follow-up. Partial weight bearing was allowed when the callus formation was observed on X-rays. The patients were allowed for full weight bearing ambulation after complete union. The union was defined as three bridging cortices in two orthogonal planes and lack of feeling pain under manual pressure and the ability of full weigh bearing walking. Patients were followed for two years after the surgery.
The main outcomes measured included time of hospital stay (in staged ORIF group, sum of two hospital admissions period), deep and superficial infection, osteomyelitis, neurovascular problems, nonunion and malunion. In this study, each soft tissue infection that was treated by oral antibiotics and without the need for surgical intervention was considered as the mild infection, while any soft tissue infection that required intravenous antibiotics or irrigation and debridement was considered as a severe infection (12, 14). Nonunion was defined as the absence of clinical and radiographic evidences for fracture healing after 9 months and the lack of healing process progression for three consecutive months (12, 30). Any angulation more than 5° in the sagittal and coronal planes was considered as malunion (12, 31).
At the final visit, patients were asked to rate their pain intensity using visual-analogue scale (VAS). On this scale, 0 represented no pain while 10 represented maximal pain. In addition, patients expressed their satisfaction level from the surgical outcomes with the same criteria in which 0 indicated dissatisfaction and 10 revealed the maximal satisfaction. The American Orthopedic Foot and Ankle Score (AOFAS) was completed in order to evaluate the functional outcomes of treatment (32).
Data was analyzed using SPSS statistical software ver.16. Independent samples t-test or Mann-Whitney U test were used in order to compare the quantitative variables between two groups. The qualitative data was compared using Chi-square test or Fisher’s exact test. P<0.05 was considered significance.
Results
The patients of both groups had no significant difference in terms of age, gender, mechanism of fracture and follow-up time [Table 1]. Hospital stay of PORIF group was 8.3±1.8 days versus 13.4±2.6 days in Two-stage group. It was significantly shorter in PORIF group (p=0.027) [Table 2]. It was also found that pain intensity, satisfaction, and AOFAS were not significantly different in both groups [Table 2]. The incidence of fractures and surgical complications in both groups were presented and compared in Table 3. In our study, none of the patients developed severe infection and osteomyelitis. Neurovascular injury was not occurred. Two patients in PROIF group and four patients in two-stage group developed mild superficial infections (p=0.41). All patients were treated with antibiotics. One patient in PORIF developed nonunion. However, the incidence of all complications was similar in both groups [Table 3]. Two patients in the two-stage group and 3 patients of the PORIF group suffered from malunion but the rate was not significantly different between two groups) p=1).
Table 1.
Comparing the demographic variables
| group | PORIF (n=21) | Two-stage (n=20) | P-value | |
|---|---|---|---|---|
| Age (y) | 37.5±12.3 (24-57) |
38.9±15.1 (28-61) |
0.361 | |
| Sex | Male | 18 | 19 | 0.606 |
| female | 3 | 1 | ||
| Mechanism | Vehicle accident | 13 | 15 | 0.386 |
| Sport injury | 8 | 5 | ||
| classification | C1 | 11 | 13 | 0.618 |
| C2 | 7 | 4 | ||
| C3 | 3 | 3 | ||
Table 2.
Comparing the hospital stay, pain intensity, satisfaction and AOFAS
| group | PORIF (n=21) | Two-stage (n=20) | P-value |
|---|---|---|---|
| Hospital stay (d) | 1.8 (6-10) ±8.3 | 2.6 (7-16)±13.4 | 0.027 |
| Pain (VAS) | 4.9±1.1 (2-7) | 5.3±1.5 (2-8) | 0.272 |
| Satisfaction (VAS) | 6.6±1.5 (4-9) | 7.1±1.3 (4-9) | 0.183 |
| AOFAS | 81.6±13.3 (67-88) | 83.3±15.3 (71-91) | 0.52 |
Table 3.
Comparing the incidence of complications
| group | PORIF (n=21) | Two-stage (n=20) | P-value |
|---|---|---|---|
| Superficial infection | 2 | 4 | 0.41 |
| Deep infection | 0 | 0 | - |
| osteomyelitis | 0 | 0 | - |
| Neurovascular injury | 0 | 0 | - |
| Nonunion | 1 | 0 | 1 |
| Anteroposterior malunion | 2 | 1 | 1 |
| Mediolateral malunion | 1 | 1 | 1 |
| Total | 6 | 6 | - |
Discussion
The most important finding of this study was that the clinical, radiographic, functional and subjective outcomes of treating Pilon fracture (type C) without severe soft tissue damage were identical in both PORIF and two-stage methods.
Figure 2.
lateral ankle xray.pilon fracture with comminution
Pilon fractures are of the most challenging injuries in orthopedic surgery. Treatments of these injuries are very challenging which are often associated with less favorable results. Since these fractures are usually caused by severe trauma and are associated with involvement of the articular surface, the desired results are not achieved in many patients and many of them will have life-long struggle with pain and discomfort of this problem.
Currently, appropriate method and timing for the treatment of Pilon fracture is not yet clear. It is assumed that high levels of infection and wound healing problems related to the surgery, is due to the damaged and swollen soft tissue in these fractures (17, 25, 33). Therefore, a two-stage protocol including maintaining the primary fibular length and external fixation of tibia and then delayed ORIF during the improvement of the soft tissue was widely used (15-18).
In a retrospective study by Dickson et al. it was found that the perfect articular reduction and anatomical joint alignment were obtained in 81% and 96% of patients who were treated by a two-step method, respectively. Radiographic studies revealed 28% of patients had degenerative changes. Postoperative complications were observed in 35% of patients, including loss of reduction (11%) that necessitates arthrodesis (11%) and amputation below the knee following failed arthrodesis (3%) (15). Recently Lavini et al. reported that using external fixator and ORIF could be very helpful for improving the soft tissue. However, it is stated that maintaining the external fixator after plate fixation had an important role in reducing the complications (34). Patterson et al. treated 22 Pilon fractures and found that 77% of patients had good results. Additionally, anatomic reduction was achieved in 73% of patients. In this study, there was no case of infection or complications in soft tissue (16). Sirkin et al. also treated open and close Pilon fractures with a two-stage procedure. They concluded that the high rate of infection and soft tissue complications in patients was due to the early ORIF while the soft tissue was damaged. In the study of Sirkin and his colleagues, 17% of patients with close Pilon fractures suffered from partial-thickness skin necrosis and one patient (3.4%) developed a chronic draining sinus secondary to osteomyelitis. All of these patients were treated well. In the open fracture group, 10.5% had partial-thickness skin necrosis and 10.5% had osteomyelitis, which in one case led to below-knee amputation (18).
In addition to prolonging the hospital stay and treatment period with consequent increasing financial burden, there is also a concern that delayed surgery could increase the risk of complications such as infection or difficulty in achieving anatomical reduction (19-21). These problems have caused some surgeons to consider PORIF for Pilon fractures. White and his colleagues treated 95 patients with Pilon fractures using PORIF. 88% of patients underwent surgery within the first 48 hours after the injury. Reduction was anatomical in 90% of the patients. Deep infection or dehiscence required debridement had occurred in 6 patients (35). Additionally Chen et al. and Gao et al. reported good results and few complications in the treatment of Pilon fractures with ORIF (23, 24). In the study of Li and his colleagues, the LCP plate with MIPO technique was used in order to treat Pilon fractures and the outcomes were very satisfactory. Superficial infection was observed in only one patient (36). In another study, Paluvadi et al. used MIPO technique and concluded that MIPO led to an increased union time, however, this technique had important role in reducing the rate of nonunion and infection. The superficial and deep infection had occurred in 10% and 2% of the patients (11). Richards et al. compared ORIF and external fixation in the treatment of Pilon fractures, and concluded that both techniques were associated with union of the fractures, sufficient articular reduction and the same rate of infection. However, the early outcomes seemed to be superior in patients with ORIF group (10).
Despite recent advancements in medical science and technology, the treatment of Pilon fractures has remained challenging, and none of the available treatment methods could not be considered as the gold standard (1). Noteworthy the problem might be due to different design studies, several survey methods and different statistical samples.
Bacon and his colleagues compared the results of two-stage method with definitive external fixation. It was concluded that the period of fracture union was longer for two-stage group (1.39 to 5.24 weeks), but the rate of nonunion (16% vs. 8.30%), malunion (8% vs. 1.23%) and infection (12% vs. 5.38%) were higher in the external fixator group. However, differences were not statistically significant between the two groups. The authors noted that they couldn’t comment on the superiority of any of these methods and future clinical trials are needed (12). Blauth et al. also compared clinical and radiological outcomes of 51 Pilon fractures treated with a) primary ORIF, b) minimally invasive osteosynthesis for reconstruction of the articular surface and transarticular external fixation for 4 weeks, and c) the two-stage method in a retrospective study. They found that significantly none of the patients from the two-stage group required the arthrodesis. In addition, for two-stage group, the range of ankle motion and rate of return to normal activities were higher. Also, pain intensity and the limitations in leisure activities were lower for this group. However, the differences were not significant for the mentioned resuls. Finally Blauth et al. concluded that the treatment of Pilon fracture with two-stage method was preferable to other methods (37). In a recent study by Tang et al., it was revealed that the incidence of superficial and deep infection, rate of union and mean of AOFAS were identical in PORIF and delayed ORIF groups. However, the time for fracture union, duration of surgery and hospitalization period were significantly shorter in the PORIF group (6).
In the current study, we compared the results of PORIF with two-stage treatment of Pilon fractures type C without severe soft tissue damage (Tscherne type 3). In the two-stage group, ORIF delayed soft tissue healing between 7 to 14 days. Actually the goal of our study was to investigate the efficacy level of using two-stage method on improving outcomes and prevention of complications such as infection effectively. No patient was found with severe infection or osteomyelitis, and although the rate of mild infection was higher in the two-stage group but the difference was not statistically significant. Nonunion occurred in one case of PORIF group, hospitalized in a psychiatric hospital, who did not cooperate with the treatment that likely played an important role in the occurrence of nonunion. Two patients in the two-stage group and 3 patients of the PORIF group suffered from malunion. The results of subjective evaluation (pain intensity and satisfaction) were similar in both groups. It should be noted that in overall the intensity of the persistent pain was high in both groups and many of the patients required different painkillers resulted in low satisfaction from the treatment outcomes. Based on the expectations, the duration of hospitalization in the two- stage group was significantly higher than PORIF group, which was pointed out in previous studies. This finding can play an important role in choosing the treatment method based on the costs and designing a more favorable psychological environment for patients and their relatives with earlier discharge.
Similar to all other studies, the current study also had its limitations. The number of the patients in the studied groups did not seem enough. By increasing the number of patients, the difference between the two groups could become statistically significant in some variables. In addition, our patients were followed for a short period, and mid- and long-term results are needed. We did not compare articular surface reduction and it is recommended for future researches.
Treatment of type C AO-OTA Pilon fractures in patients with Tscherne grade 1, 2 of soft tissue using PORIF or two-stage method including primary external fixation and delayed ORIF was associated with the same clinical, radiological, functional and subjective outcomes. Furthermore, the rate of complications was identical. Thus, given the shorter hospital stay, the authors recommend using PORIF in treatment of Pilon fractures without severely damaged soft tissue.
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
References
- 1.Calori GM, Tagliabue L, Mazza E, de Bellis U, Pierannunzii L, Marelli BM, et al. Tibial pilon fractures: which method of treatment? Injury. 2010;41(11):83–90. doi: 10.1016/j.injury.2010.08.041. [DOI] [PubMed] [Google Scholar]
- 2.Kilian O, Bündner MS, Horas U, Heiss C, Schnettler R. Long-term results in the surgical treatment of pilon tibial fractures A retrospective study. Chirurg. 2002;73(1):65–72. doi: 10.1007/s104-002-8031-1. [DOI] [PubMed] [Google Scholar]
- 3.Çeçen GS, Gülabi D, Yanık E, Pehlivanoğlu G, Bekler H, Elmalı N. Effect of BMI on the clinical and radiological outcomes of pilon fractures. Acta Orthop Traumatol Turc. 2014;48(5):570–5. doi: 10.3944/AOTT.2014.14.0073. [DOI] [PubMed] [Google Scholar]
- 4.Lau TW, Leung F, Chan CF, Chow SP. Wound complication of minimally invasive plate osteosynthesis in the distal tibia fractures. Int Orthop. 2007;32(5):697–703. doi: 10.1007/s00264-007-0384-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan R, Taylor BC, Gentile J. Optimal management of high-energy pilon fractures. Orthopedics. 2015;38(8):e708–14. doi: 10.3928/01477447-20150804-59. [DOI] [PubMed] [Google Scholar]
- 6.Tang X, Tang PF, Wang MY, Lü DC, Liu MZ, Liu CJ. Pilon fractures: a new classification and therapeutic strategies. Chin Med J (Engl) 2012;125(14):2487–92. [PubMed] [Google Scholar]
- 7.Abd-Almageed E, Marwan Y, Esmaeel A, Mallur A, El-Alfy B. Hybrid external fixation for Arbeitsgemeinschaft für Osteosynthesefragen (AO) 43-C tibial plafond fractures. J Foot Ankle Surg. 2015;54(6):1031–6. doi: 10.1053/j.jfas.2015.04.022. [DOI] [PubMed] [Google Scholar]
- 8.Borens O, Kloen P, Richmond J, Roederer G, Levine DS, Helfet DL. Minimally invasive treatment of pilon fractures with a low profile plate: preliminary results in 17 cases. Arch Orthop Trauma Surg. 2009;129(5):649–59. doi: 10.1007/s00402-006-0219-1. [DOI] [PubMed] [Google Scholar]
- 9.Yoon RS, Bible J, Marcus MS, Donegan DJ, Bergmann KA, Siebler JC, et al. Outcomes following combined intramedullary nail and plate fixation for complex tibia fractures: a multi-centre study. Injury. 2015;46(6):1097–101. doi: 10.1016/j.injury.2015.03.019. [DOI] [PubMed] [Google Scholar]
- 10.Richards JE, Magill M, Tressler MA, Shuler FD, Kregor PJ, Obremskey WT, et al. External fixation versus ORIF for distal intra-articular tibia fractures. Orthopedics. 2012;35(6):e862–7. doi: 10.3928/01477447-20120525-25. [DOI] [PubMed] [Google Scholar]
- 11.Paluvadi SV, Lal H, Mittal D, Vidyarthi K. Management of fractures of the distal third tibia by minimally invasive plate osteosynthesis - A prospective series of 50 patients. J Clin Orthop Trauma. 2014;5(3):129–36. doi: 10.1016/j.jcot.2014.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bacon S, Smith WR, Morgan SJ, Hasenboehler E, Philips G, Williams A, et al. A retrospective analysis of comminuted intra-articular fractures of the tibial plafond: open reduction and internal fixation versus external Ilizarov fixation. Injury. 2008;39(2):196–202. doi: 10.1016/j.injury.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Gupta A, Anjum R, Singh N, Hackla S. Outcome of distal both bone leg fractures fixed by intramedulary nail for fibula & MIPPO in tibia. Arch Bone Jt Surg. 2015;3(2):119–23. [PMC free article] [PubMed] [Google Scholar]
- 14.Tang X, Liu L, Tu CQ, Li J, Li Q, Pei FX. Comparison of early and delayed open reduction and internal fixation for treating closed tibial pilon fractures. Foot Ankle Int. 2014;35(7):657–64. doi: 10.1177/1071100714534214. [DOI] [PubMed] [Google Scholar]
- 15.Dickson KF, Montgomery S, Field J. High energy plafond fractures treated by a spanning external fixator initially and followed by a second stage open reduction internal fixation of the articular surface-preliminary report. Injury. 2001;32(Suppl 4):SD92–8. doi: 10.1016/s0020-1383(01)00163-2. [DOI] [PubMed] [Google Scholar]
- 16.Patterson MJ, Cole JD. Two-staged delayed open reduction and internal fixation of severe pilonfractures. J Orthop Trauma. 1999;13(2):85–91. doi: 10.1097/00005131-199902000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Mauffrey C, Vasario G, Battiston B, Lewis C, Beazley J, Seligson D. Tibial pilon fractures: a review of incidence, diagnosis, treatment, and complications. Acta Orthop Belg. 2011;77(4):432–40. [PubMed] [Google Scholar]
- 18.Sirkin M, Sanders R, DiPasquale T, Herscovici D Jr. A staged protocol for soft tissue management in the treatment of complex pilonfractures. J Orthop Trauma. 2004;18(8 Suppl):S32–8. doi: 10.1097/00005131-200409001-00005. [DOI] [PubMed] [Google Scholar]
- 19.Hoiness P, Stromsoe K. The influence of the timing of surgery on soft tissue complications and hospital stay: a review of 84 closed ankle fractures. Ann Chir Gynaecol. 2000;89(1):6–9. [PubMed] [Google Scholar]
- 20.Saithn A, Moody W, Jenkinson E, Almazedi B, Sargeant I. The influence of timing of surgery on soft tissue complications in closed ankle fractures. Eur J Orthop Surg Traumatol. 2009;19(7):481–4. [Google Scholar]
- 21.Singh BI, Balaratnam S, Naidu V. Early versus delayed surgery for ankle fractures: a comparison of results. Eur J Orthop Surg Traumatol. 2005;15(1):23–7. [Google Scholar]
- 22.Leung F, Kwok HY, Pun TS, Chow SP. Limited open reduction and Ilizarov external fixation in the treatment of distal tibial fractures. Injury. 2004;35(3):278–83. doi: 10.1016/s0020-1383(03)00172-4. [DOI] [PubMed] [Google Scholar]
- 23.Chen DW, Li B, Aubeeluck A, Yang YF, Zhou JQ, Yu GR. Open reduction and internal fixation of posterior pilon fractures with buttress plate. Acta Ortop Bras. 2014;22(1):48–53. doi: 10.1590/S1413-78522014000100009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gao H, Zhang CQ, Luo CF, Zhou ZB, Zeng BF. Fractures of the distal tibia treated with polyaxial locking plating. Clin Orthop Relat Res. 2009;467(3):831–7. doi: 10.1007/s11999-008-0459-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scolaro J, Ahn J. Pilon fractures. Clin Orthop Relat Res. 2011;469(2):621–3. doi: 10.1007/s11999-010-1509-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dillin L, Slabaugh P. Delayed wound healing, infection, and nonunion following open reduction and internal fixation of tibial plafond fractures. J Trauma. 1986;26(12):1116–9. doi: 10.1097/00005373-198612000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Kapukaya A, Subasi M, Arslan H, Tuzuner T. Non-reducible, open tibial plafond fractures treated with a circular external fixator (is the current classification sufficient for identifying fractures in this area?) Injury. 2005;36(12):1480–7. doi: 10.1016/j.injury.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 28.Wyrsch B, McFerran MA, McAndrew M, Limbird TJ, Harper MC, Johnson KD. Operative treatment of fractures of the tibial plafond A randomized, prospective study. J Bone Joint Surg. 1996;78(11):1646–57. doi: 10.2106/00004623-199611000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Karbalaeikhani A, Saied A, Heshmati A. Effectiveness of the gastrocsoleous flap for coverage of soft tissue defects in leg with emphasis on the distal third. Arch Bone Jt Surg. 2015;3(3):193–7. [PMC free article] [PubMed] [Google Scholar]
- 30.Ronga M, Longo UG, Maffulli N. Minimally invasive locked plating of distal tibia fractures is safe and effective. Clin Orthop Relat Res. 2010;468(4):975–82. doi: 10.1007/s11999-009-0991-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nehme A, Tannous Z, Wehbe J, Moucharafieh R, Maalouf G. Arthroscopically assisted reconstruction and percutaneous screw fixation of a pilon tibial malunion. J Foot Ankle Surg. 2007;46(6):502–7. doi: 10.1053/j.jfas.2007.08.010. [DOI] [PubMed] [Google Scholar]
- 32.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;5(7):349–53. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 33.He X, Hu Y, Ye P, Huang L, Zhang F, Ruan Y. The operative treatment of complex pilon fractures: a strategy of soft tissue control. Indian J Orthop. 2013;47(5):487–92. doi: 10.4103/0019-5413.118205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lavini F, Dall’Oca C, Mezzari S, Maluta T, Luminari E, Perusi F, et al. Temporary bridging external fixation in distal tibial racture. Injury. 2014;45(6):S58–63. doi: 10.1016/j.injury.2014.10.025. [DOI] [PubMed] [Google Scholar]
- 35.White TO, Guy P, Cooke CJ, Kennedy SA, Droll KP, Blachut PA, et al. The results of early primary open reduction and internal fixation for treatment of OTA 43C-type tibial pilon fractures: a cohort study. J Orthop Trauma. 2010;24(12):757–63. doi: 10.1097/BOT.0b013e3181d04bc0. [DOI] [PubMed] [Google Scholar]
- 36.Li Q, Zhao WB, Tu CQ, Yang TF, Fang Y, Zhang H, et al. Locking compression plate (LCP) combined with minimally invasive percutaneous plate osteosynthesis (MIPPO) for the treatment of pilon fracture. Zhongguo Gu Shang. 2014;27(12):1029–32. [PubMed] [Google Scholar]
- 37.Blauth M, Bastian L, Krettek C, Knop C, Evans S. Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. J Orthop Trauma. 2001;15(3):153–60. doi: 10.1097/00005131-200103000-00002. [DOI] [PubMed] [Google Scholar]