Abstract
Objective:
Adolescence is a vulnerable period for the development of depressive disorders. Recent research has demonstrated the importance of distress tolerance in the onset and maintenance of depression during adulthood; however, little is known about its role in predicting depressive symptoms among adolescents. The current study examines the effect of distress tolerance and co-occurring negative life events on the developmental trajectory of depressive symptoms from middle to late adolescence.
Method:
Our sample included 117 adolescent boys and girls (44.4% female; 54.6% White). Participants were, on average, 16 years old at baseline (SD = 0.90), and completed self-report inventories of negative life events and depressive symptoms; distress tolerance was assessed using a behavioral measure.
Results:
Utilizing a latent growth curve approach, we found a significant interaction between distress tolerance and negative life events in predicting increases in depressive symptoms over time. Follow-up analyses suggest that negative life events were associated with greater increases in depressive symptoms over time for adolescents with lower levels of distress tolerance only.
Conclusion:
The study highlights the moderating role of distress intolerance in the relation between negative life events and depressive symptoms, and underscores the importance of targeting distress tolerance for treating depression among youth.
Keywords: Depression, distress tolerance, adolescents, negative life events
Depression is one of the most common psychiatric disorders in the United States with an estimated lifetime prevalence of 17% (Sadock & Sadock, 2007). Adolescence marks a period of particularly increased risk for depression. Indeed, a review of estimates of incidence of major depression before the age of 18 suggests rates range between 0.2% and 17% (Costello, Mustillo, Keller & Angold, 2004). Longitudinal research suggests that rates of depressive disorders are relatively low during childhood but rise sharply across adolescence (Avenevoli, Swendsen, He, Burstein, & Merikangas, 2015; Kessler et al., 2005). Moreover, studies have demonstrated links between early onset of symptoms in adolescence and recurrent episodes of depression in adulthood (Burcusa & Iacono, 2007; Spijker et al., 2002).
Diathesis-stress models of depression
Many of the leading theories of the development and maintenance of depression suggest that the disorder stems from the interaction between environmental stressors and pre-existing vulnerabilities, commonly known as diathesis-stress models (Padilla Paredes & Calvete Zumalde, 2015; Woody, Burkhouse, Birk, & Gibb, 2015). While the role of negative life events has been consistently linked to the onset of depressive disorders (Hankin, 2006; Hankin, Mermelstein & Roesch, 2007), a number of possible diatheses have been proposed to explain the emergence of depressive symptoms (Lakdawalla, Hankin, & Mermelstein, 2007). Distress tolerance (DT) has recently received considerable attention as a specific vulnerability factor underlying the development and maintenance of depression (Leyro, Zvolensky, & Bernstein, 2010). DT is defined as the ability to experience and endure negative emotional states (Simons & Gaher, 2005). Individuals with low DT evidence an inability to persist in goal-directed behavior in the face of distressing feelings (Leyro et al., 2010). DT is believed to develop across childhood and become stable during early adolescence (Cummings et al., 2013).
Consistent with negative reinforcement models of the development of mental health disorders, distress intolerant individuals are likely to engage in escape or avoidance behaviors when faced with emotional discomfort. In the absence of more adaptive coping skills, people low in DT may fail to learn effective ways to habituate to distress and may engage in maladaptive behaviors meant to avoid further negative feelings. Indeed, DT has been linked to a variety of psychopathologies and risky behaviors, including substance use, gambling, and suicidal behavior) in adult (Anestis, Knorr, Tull, Lavender, & Gratz, 2013; Brown, Lejuez, Kahler, Strong, & Zvolensky, 2005; Buckner, Keough, & Schmidt, 2007; Daughters, Lejuez, Kahler, Strong & Brown, 2005) and adolescent samples (Cohen, Danielson, Adams, & Ruggiero, 2016; Juarascio, Felton, Borges, Manasse, Murray, & Lejuez, 2016). Moreover, recent evidence demonstrates its significant association with depressive symptoms (see Leyro et al., 2010 for review). It may be that the relation between initial levels of negative affect and the onset of depressive symptoms is exacerbated by low levels of DT (see Hankin & Abramson, 2001). In line with this model, several studies have shown cross-sectional correlations between low DT and depressive symptoms in both adult and adolescent clinical (Anestis, Gratz, Bagge, & Tull, 2012; Ellis, Fischer, & Beevers, 2010; Gorka, Ali, & Daughters, 2012; Nock & Mendes, 2008; Williams, Thompson, & Andrews, 2013) and non-clinical samples (Daughters et al., 2009; Peterson, Davis-Becker, & Fischer, 2014). However, other studies have failed to find a prospective relation between DT and depressive symptoms among adolescent populations (e.g. Cummings et al., 2013), suggesting a more complicated pattern of relations between DT and consequent emotional distress (e.g. McHugh et al., 2011), specifically during this developmental period.
One explanation for the noted inconsistencies in these findings may be the critical role that negative life events plays in the relation between DT and depressive symptomology. Individuals low in DT may be less able to tolerate difficult sensations and emotional states associated with potentially stressful experiences (Bardeen, Fergus, & Orcutt, 2017; Felton et al., 2017) and DT may, in turn, exacerbate existing vulnerabilities to psychopathology in the face of negative events. Indeed, a number of studies have implicated the interaction between DT and negative life events in predicting a variety of maladaptive behaviors and negative emotions, including obsessions (Macatee, Capron, Schmidt, & Cougle, 2013), hoarding tendencies (Shaw & Timpano, 2016), cigarette craving (Volz et al., 2014), and anger (Hawkins, Macatee, Guthrie, & Cougle, 2013) in adult populations. Only one study, to our knowledge, has examined the interaction between DT and negative life events in the prediction of depression. The authors found that endorsing a greater number of life events moderated the relation between DT and depression in a cross-sectional study of HIV-positive adults (O’Cleirigh, Ironson, & Smits, 2007). However the prospective relations between negative life events and DT in predicting depressive symptoms among adolescents has, notably, not yet been examined.
Measurement concerns in conceptualizing DT
The manner in which DT is assessed is of particular concern for studies testing models of the emergence of depression. Importantly, self-report and behavioral indicators of DT may be capturing conceptually distinct constructs that may evidence different patterns of relations with outcome variables (Ameral, Palm Reed, Cameron, & Armstrong, 2014; Leyro et al., 2010). Self-report measures of DT ask youth to disclose what they think, feel, and do when distressed. This level of metacognition may be difficult for adolescents, resulting in potentially unreliable or invalid responses. Behavioral tasks, on the other hand, may more accurately gauge an adolescent’s ability to persist in the face of distress. Measures such as the Behavioral Indicator of Resiliency to Distress (BIRD; Lejuez, Daughters, Danielson & Ruggiero, 2006) assess actual attempts to escape from distressing situations, and avoidance behavior during the task is unrelated to performance or skill in completing the task (Daughters et al., 2009; Felton et al., 2017). Given the importance of understanding behavioral tendencies to persist or not in the face of negative life events, behavioral tools for assessing DT may be particularly useful in understanding these relations.
Current study
Despite emerging evidence of the relation between DT, negative life events, and depressive symptoms, there is a need to extend current research by examining the utility of this diathesis-stress model in explaining the emergence of depression across adolescence. Understanding the interaction between specific vulnerabilities and environmentally-based stressors has the potential to inform our understanding of how depressive symptoms develop over time. Thus, the current study examines the interaction between DT (measured using a behavioral task) and negative life events and their prediction of depressive symptoms across a three-year period from middle to late adolescence. We hypothesized that rates of depressive symptoms would increase over this period of time, and that DT would significantly interact with negative life events to predict changes in depressive symptoms over time. Specifically, we theorized that low DT would predict a steeper increase in depressive symptoms over time, and that the presence of negative life events would further exacerbate the relation between DT and depressive symptoms during this critical developmental period of adolescence.
Method
Participants and Procedures
Participants for this study were recruited from a large metropolitan area as part of an ongoing larger, nine-year longitudinal study investigating the predictors of risk-taking behavior in adolescents (although the ninth year was not collected in time for inclusion in the current study). Recruitment took place through media outreach and through fliers at schools, community centers, libraries, and Boys and Girls clubs. Families who were interested were screened for inclusion criteria, including their ability to participate in annual assessments and for their English proficiency. Participants and their parents came into the lab to complete all measures and tasks on an annual basis. Youth received up to $40 for each wave that they took part in.
Because key study measures were not introduced until the sixth year of the data collection, the current study uses data from waves 6 through 8 (relabeled waves 1 through 3, below, for clarity). Of the original sample of 277 adolescents who took part in the initial data collection, the current study includes data from 117 youth (44.4% female) who were still participating at the sixth wave. Adolescents at this wave ranged in age from 14 to 17 (Mage = 16.10, SDage = 0.90) with 54.6% identifying as White, 40.2% identifying as Black, and 5.2% identifying as “other race/ethnicity.” Race/ethnicity was reflective of the urban environment from which the sample was drawn. Mothers’ reported annual family income which ranged from $0 to $375,000 (Mincome = $106,620, SDincome = $70,079), and was grouped into four categories. (1) $0 - $46,999; (2) $47,000 - $99,999; (3) $100,000 - $149,999; and (4) $150,000+. All youth who participated at any wave of the study were recruited to return at each annual point, resulting in an n = 87 at the second wave and n = 88 at the third wave.
Measures
Depressive Symptoms.
Depressive symptoms were assessed annually at waves 1–3. We used the major depression subscale (consisting of 10 items) from the Revised Children’s Anxiety and Depression Scale (RCADS; Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000), which is a youth self-report measure of anxiety and depression symptoms. Participants were asked to rate how often each item applies to them on a 4-point Likert scale, where 0 = never, 1 = sometimes, 2 = often, and 3 = always. Sample items include: “I feel sad or empty,” and “Nothing is much fun anymore.” The total score was computed by adding the scores for each individual item. Higher scores indicate greater levels of depression. The RCADS has demonstrated good factor structure, reliability, and validity in school-based and clinical samples (Chorpita et al., 2000; Chorpita, Moffitt, & Gray, 2005). The coefficient alphas for the depression subscale in our study were .83, .82, and .87 for waves 1 −3, respectively.
Negative Life Events.
Negative life events were measured at wave 1. We used a modified version of the Coddington’s Life Events Questionnaire (LEQ; Coddington, 1972), which is a 72-item measure that assesses the experience of different life events. Adaptations of the scale are widely used to measure negative events associated with the onset of pathology (Bailey & Garralda, 1990; Coddington, 1972; Garrison, Kannel, Stokes, & Castelli, 1987). Participants indicated whether or not each number of life events happened to them, including having a new adult move into the home or being suspended from school. For the present study, we selected 35 items that are most pertinent to adolescents in an urban setting (items eliminated from the current study that were deemed less applicable for the sample included “getting married” and “becoming a member of a church”). Items were then summed to create an index of experienced negative life events.
Distress Tolerance.
The Behavioral Indicator of Resiliency to Distress (BIRD: Lejuez, et al., 2006), a computerized behavioral task, was used to measure distress tolerance at wave 1. During the task, ten numbered boxes are presented on the computer screen. Participants are asked to click a green dot that appears on top of a numbered box before it moves to another box. If the participant is able to click on the green dot before it moves away, a cartoon bird flies out of its cage and makes a pleasant chirping sound and the participant earns a point that can be cashed in for prizes. However, if the participant is unable to click the green dot before it moves, or if the participant clicks an incorrect numbered box, the bird stays in its cage and makes a loud, unpleasant noise and no points are earned.
The BIRD has three levels, each of which is more difficult than the previous one. The first level lasts for 3 minutes, and begins with a 5-second latency in between dot presentations and increases or decreases based on the youth’s performance. If the participant correctly hits the box, the latency is reduced by 0.5 seconds, whereas the latency is increased by 0.5 seconds for each incorrect answer or non-response. Based on the adolescent’s performance on this level, an average latency is calculated to index the skill level of each participant. The second level is more difficult; it lasts for a total of 5 minutes wherein the first four minutes are played using the average latency from the previous level, and then the latency is reduced in half for the last one minute, making the task very difficult to accurately complete (this stage is knows as the challenge latency). After a brief period of rest, the third and final level consists of the challenge latency for up to 5 minutes. Participants are informed in advance that they have the option to quit at anytime during this level, but their final reward will depend upon their total points at the time at which they quit the game. Participants are also told about the different rewards they could win (e.g. games, sporting goods, etc.), but information on the number of points required for these specific rewards is not given. Distress tolerance was calculated as the number of seconds the participants persisted in the task in the final (challenge) level, with a maximum of 300 seconds for those who did not quit the task. Scores on the first two levels were recorded to control for the effects of skill on persistence (Daughters, et. al, 2009).
The BIRD has sound psychometric qualities, with support for test re-test reliability (Cummings et al., 2013) and concurrent validity (Daughters et al., 2009). Specifically, previous studies have utilized a self-report affect schedule (the Positive and Negative Affect Schedule – Children; Laurent et al., 1999) to examine changes in pre- to post-task negative affect, finding significant increases in negative affect over the course of the trial (e.g. Daughters et al., 2009; MacPherson et al., 2010). Moreover, changes in affect have been found to be unrelated to success on the task, suggesting that the BIRD elicits distress above and beyond performance concerns (Amstadter et al., 2012; Cummings et al., 2013; Daughters et al., 2009; MacPherson et al., 2010). Further, youth who quit the task did not differ in the amount of self-reported distress on self-report affect measures as compared to youth who did not quit the task (Daughters et al., 2009; Danielson, Ruggiero, Daughters, & Lejuez, 2010; MacPherson et al., 2010). This indicates that the BIRD does not simply measure success on the task, or distress in response to the task, but the ability to tolerate distress in general. The task has also demonstrated good construct validity and external validity, and performance on the BIRD was related to internalizing and externalizing symptoms (Cummings et al., 2013; MacPherson et al., 2010).
Data Analytic Plan
Latent growth modeling (LGM) is a special case of structural equation modeling whereby multiple waves of data are used to estimate initial levels and change over time. In the current study, we derived a latent intercept and slope for depressive symptoms over the course of three waves. Means and variances for baseline (initial levels) and slope (trajectory) factors are estimated using all available data points. Thus, even though some participants dropped out of the study from the first to the second wave (and from the second to third wave), their data were still used to estimate the latent factors, allowing for increased power to detect growth trajectories. Significant intercept and slope estimates indicate that the latent depressive symptoms trajectory is both statistically different from zero at baseline (intercept) and changes significantly over time (slope). Significant variances in these estimates indicate individual differences around these factors and supports the inclusion of predictors of these differences. Utilizing established power curves (e.g. Muthén & Curran, 1997; Zhang & Wang, 2009), we estimate a sample size of approximately 120 individuals has sufficient power (est. = 0.80) to detect a medium effect size.
Model fit was determined by examining four indices, including: the χ2 statistic, the Comparative Fit Index (CFI; Bentler, 1990), Tucker-Lewis Index (TLI; Tucker & Lewis, 1973), and the Root Mean Square Error of Approximation (RMSEA; Steiger, 1990). Nonsignificant χ2 values indicate good fit; however, the χ2 can be influenced by large sample size and is thus not always a reliable indicator of good fit. CFI and TLI values greater than .90 and RMSEA values less than .08 suggest acceptable fit of the model to the data (Schweizer, 2010). All analyses were completed using Mplus 6.0 (Muthén & Muthén, 2010), which utilizes full information maximum likelihood (ML) estimation methods to handle missing data, providing less biased parameter estimates than procedures such as listwise or pairwise deletion under the missing at random assumption (Little & Rubin, 1989). Thus, we were able to conduct all analyses on the full sample.
We first estimated an unconditional model to determine the trajectory of depression symptoms over time. In order to fit the unconditional model, regression weights from the latent intercept factor to each manifest measure of depressive symptoms (at waves 1 through 3) were constrained to be 1.0. Paths from the latent slope factor to the manifest measures dictate the shape of change in depressive symptoms over time. First, the paths from the latent slope factor to the repeated measures of the manifest variable were set to 1.0, 2.0 and 3.0, respectively, to represent linear change over time. Next, we constrained the residuals to be equal across repeated measures (i.e. homoscedasticity) and compared this more parsimonious model to one in which the errors were freely estimated, using the change in χ2 statistic and accompanying degrees of freedom to determine which is the more parsimonious model. If this constrained model did not result in a significant perturbation of fit, it was retained throughout the rest of the analyses.
We then estimated a conditional model in which we added our covariates (age, sex, race/ethnicity, and family income) and main effects (DT and negative life events). Exogenous variables were entered as predictors of the latent intercept and slope factors, and the fit of this new model was examined. In line with model-building procedures, non-significant covariates were then removed to create a more parsimonious model. Finally, we added the interaction term between DT and negative life events as a predictor in the model and examined its effect on the latent intercept and slope (see Figure 1).
Figure 1.
Final latent growth curve model with standardized (and unstandardized) estimates.
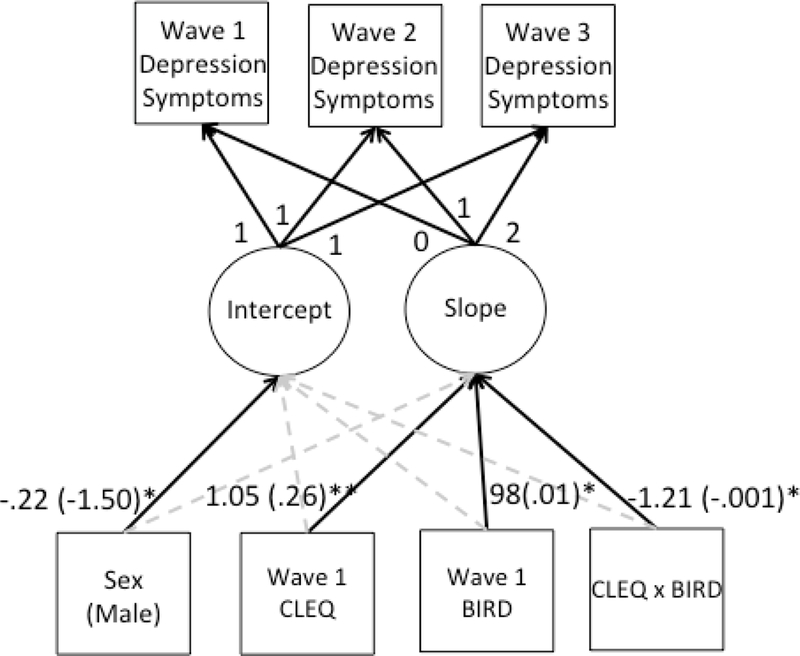
Note. Solid lines represent significant paths, grey dashed lines represent non-significant paths. CLEQ = Children’s Life Events Questionnaire; BIRD = Behavioral Indicator of Resilience to Distress. *p < .05, **p < .01.
Results
Preliminary Analyses
First, we examined patterns of missing data. Little’s MCAR analyses supported the assumption that data were missing completely at random: χ2 (88) = 70.50, p = 0.914. We then examined correlations between baseline variables and participation in future waves of data. We found no significant relations (ps > .39), with the exception of a small correlation (r = .15) between sex and participation at the final wave, indicating that boys were more likely to participate at wave 3 than girls. Data were also examined for univariate and multivariate normality and all variables were found to be within acceptable ranges for skew and kurtosis (≤ 3.0). Utilizing RCADS clinical cut-offs recommended by Chorpita, Moffitt, & Gray (2005), we found that 4%, 4%, and 3% of the sample met criteria for clinically significant levels of depressive symptoms at waves 1 through 3, respectively. Means and standard deviations as well as correlations between variables are reported in Table 1. Of note, girls reported higher levels of depressive symptoms at waves 1 and 3, while children with higher distress tolerance evidenced lower levels of depressive symptoms at wave 2. Children who reported more negative life events at baseline also reported higher levels of depressive symptoms at all waves.
Table 1.
Summary of Intercorrelations, Means and Standard Deviations on key study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
|---|---|---|---|---|---|---|---|---|---|
| 1. | Sex (male) | – | |||||||
| 2. | Age | .23* | – | ||||||
| 3. | Ethnicity (white) | −.03 | .05 | – | |||||
| 4. | BIRD Wave 1 | .03 | .10 | −.06 | – | ||||
| 5. | CLEQ Wave 1 | −.10 | −.07 | .23* | −.16 | – | |||
| 6. | RCADS: MDD Wave1 | −.22* | −.08 | .06 | −.16 | .23* | – | ||
| 7. | RCADS: MDD Wave2 | −.13 | −.09 | .03 | −.15 | −.30** | .65** | – | |
| 8. | RCADS: MDD Wave3 | −.11 | .03 | .01 | −.16 | .37** | .48** | .61** | – |
| M | .56 | 16.10 | .51 | 209.45 | 13.90 | 6.25 | 5.95 | 6.38 | |
| SD | .50 | .90 | .50 | 108.14 | 6.05 | 4.09 | 4.19 | 4.83 |
Note. BIRD = Behavioral Indicator of Resilience to Distress; CLEQ = Children’s Life Events Questionnaire; RCADS: MDD = Revised Children’s Anxiety and Depression Scale: Major Depressive Disorder Subscale.
p < .05
p < .01.
Unconditional Latent Growth Curve
Next, we examined a univariate latent growth curve of depressive symptoms over time in which we included fixed paths for a linear slope. The unconditional model fit the data well: χ2(df=1) = 0.16, p = 0.69; CFI = 1.00; TLI = 1.00; RMSEA = 0.00 (90% CI = 0.00 – 0.14). We then constrained the residuals of each manifest term to be homoscedastic. This constraint resulted in a non-significant change in model fit (Δχ2=6.5, Δdf = 2) and thus was retained. Examination of the means of the intercept (M = 6.05, SE = 0.29, p < .001) and slope (M = 0.21, SE = 0.17, p = .240) suggest that baseline levels of depressive symptoms are significantly different from zero, but that depressive symptoms do not significantly change over time, on average. The variances of the intercept (Var. = 11.05, SE = 1.84, p < .001) and the slope (Var. = 1.87, SE = 0.69, p = .007) were both significant, indicating individual differences around these parameters. The intercept and slope, however, were not significantly correlated with one another (r = −.17).
Conditional Latent Growth Curve
Using a model building approach, we next added our control variables (sex, race/ethnicity, family income and age at baseline) as well as our main effects (negative life events and distress tolerance at baseline) as predictors of the latent intercept and slope. This model provided an adequate fit to the data: χ2(df=17) = 33.25, p = 0.011; CFI = 0.88; TLI = 0.85; RMSEA = 0.09 (90% CI = 0.04 – 0.14). Of the included covariates, only sex was a significant predictor of baseline levels (std. est. = −.23, p = .032). We removed the non-significant covariates and re-ran the model, resulting in significantly improved model fit: χ2(df=8) = 7.77, p = 0.456; CFI = 1.00; TLI = 1.00; RMSEA = 0.00 (90% CI = 0.00 – 0.10). Results from this model suggest that negative life events (std. est. = .24, p = .027) and sex (std. est. = −.23, p = .021) predicted depressive symptoms at baseline, suggesting that girls and youth who report experiencing more negative life events evidenced significantly greater baseline levels of depressive symptoms. None of the predictors were significantly associated with change in depressive symptoms over time.
Finally, we added an interaction term between negative life events and distress tolerance to the model. Again, the model fit the data well: χ2(df=7) = 4.97, p = 0.663; CFI = 1.00; TLI = 1.00; RMSEA = 0.00 (90% CI = 0.00 – 0.09). The interaction term significantly predicted the slope (std. est. = −1.21, p = .011) only. In order to better understand the nature of this relation, we ran another model in which we utilized a multigroup approach, including a group of youth with high DT (classified as scoring +1 SD from the mean on the BIRD) and a group of youth with low DT (classified as scoring −1 SD from the mean on the BIRD). We then examined the effect of negative life events on the slope of depressive symptoms, controlling for sex, in both groups. This model also fit the data well: χ2(df=11) = 11.67, p = 0.389; CFI = .99; TLI = .98; RMSEA = 0.04 (90% CI = 0.00 – 0.17). Negative life events were a significant predictor of the intercept for the low distress tolerance group only (std. est. = .51, p = .028) but not the high distress tolerance group (std. est. = .03, p = .910). In other words, negative life events is associated with greater increases in depressive symptoms over time for distress intolerant adolescents only (see Figure 2).
Figure 2.
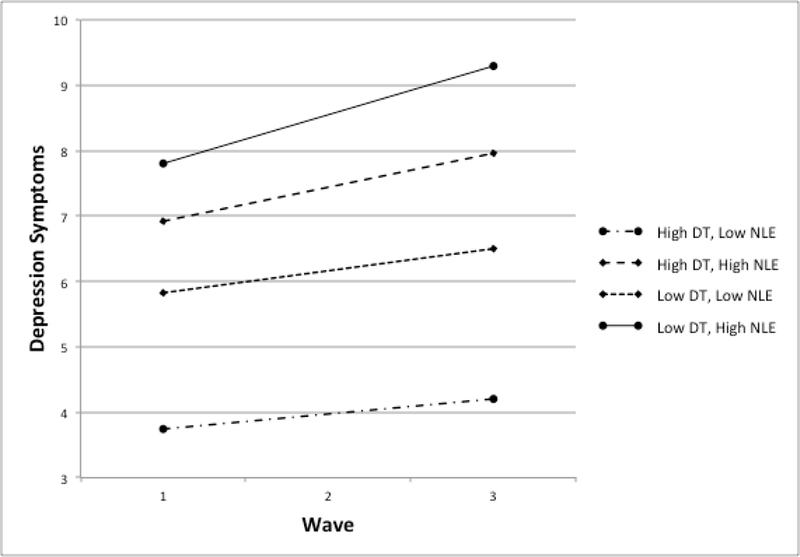
Graph of the linear trajectories of +/− 1 SD of mean distress tolerance and negative life events on depressive symptoms over time.
DT = Distress Tolerance (as measured by the Behavioral Indicator of Resilience to Distress at Wave 1); NLE = Negative Life Events (as measured by the Children’s Life Events Questionnaire at Wave 1).
Discussion
Diathesis-stress models of the development of depression are well-established in the literature, yet less is known about which specific vulnerabilities are associated with increases in depressive symptoms during adolescence. Identifying these vulnerability factors constitutes an important research agenda given that not all youth who experience negative life events proceed to develop depression. Therefore, the primary aim of the current investigation was to examine whether distress tolerance, an individual difference factor that refers to one’s ability to persist in goal-directed behavior in the face of aversive emotionality, moderated the association between negative life events at baseline and adolescent depressive symptoms over time. The findings were consistent with a diathesis-stress model, such that negative life events at wave 1 were associated with increases in depressive symptoms among adolescents with low levels of DT, but not for adolescents with high levels of DT.
Our results expand the research literature on adolescent depressive symptomatology in several key ways. Specifically, a substantial number of investigations have focused solely on the independent relation between negative life events and depressive symptoms, and a growing yet limited line of research has examined the relation between DT and depressive symptoms primarily within adult populations (Abrantes et al., 2008; Harrington, 2006). However, our results reveal the importance of the interaction between baseline negative life events and DT, and indicate that when viewed independently, baseline negative life events and DT may be insufficient indicators of emotional well-being. This finding helps to elucidate why there are notable inconsistencies in the existing literature examining the relation between DT and depressive symptoms (e.g. Anestis et al. 2012; Cummings et al., 2013). In fact, correlational studies may tell an incomplete story; in the current research, DT at wave 1 was only associated with depressive symptoms at the second assessment wave, and negative life events at wave 1 was related to depressive symptoms across the three assessment waves, which may have led to the erroneous conclusion that depression and DT were unrelated. Therefore, future research may benefit from also using longitudinal approaches and examining the interplay between the effects of DT and negative life events as vulnerability factors for depressive disorders.
Our results with an adolescent sample, coupled with prior research showing that self-reported distress tolerance moderates the association between number of negative life events and depressive symptoms among HIV-positive patients (O’Cleirigh et al., 2007), may be taken as preliminary evidence that the joint contribution and interplay of these two variables may hold across various populations and age groups. Future work is warranted to examine the extent to which our results can be generalized to clinical and other non-clinical samples.
This research has several important clinical implications. Those who experience negative life events and who are low in DT may be a particularly important target for clinical interventions and prevention efforts for depression. As such, mental health prevention and intervention efforts should focus on promoting healthy levels of distress tolerance, especially because without intervention, distress tolerance shows relative stability over time (Cummings et al., 2013). Our finding that low DT exacerbates negative life events and impacts depressive symptoms is not entirely surprising. Indeed, individuals with low distress tolerance try to avoid distressing situations and emotions (McHugh & Otto, 2011; Leyro et al., 2010), which can lead to maladaptive coping strategies, which in turn may further increase the propensity to experience depression (Campbell-Sills & Barlow, 2007; Gross & Munoz, 1995). Therefore, interventions that focus on increasing exposure to and acceptance of emotional experiences, such as Acceptance and Commitment Therapy (Hayes & Lillis, 2014) and Dialectical Behavior Therapy (Linehan, 1993), may help buffer individuals who experience negative life events by increasing their perception that their emotions are bearable, acceptable, and temporary. Individual-level intervention and prevention efforts may also benefit from approaches that offer specific strategies for coping with negative life events and which support development of effective emotion regulation strategies (e.g., Cognitive Behavioral Therapy and Dialectical Behavior Therapy; Linehan, 1993). The current study also suggests that when assessing risk for depressive symptoms clinically, it is important to also assess the impact of negative life events for clients with low distress tolerance.
Limitations and future directions
The current study must be interpreted in light of its limitations. First, the generalizability of the results is limited given that adolescents were recruited via local newspapers and letters to parents which limits the representativeness of the sample. Indeed, this sampling strategy resulted in recruiting a sample with low levels of clinically-significant depression. Moreover, our sample size did not allow for sufficient power to examine sex and race/ethnicity effects more fully. Future research should attempt to explore and clarify the effects of demographic factors and a broader range of symptom severity on these relations. Second, we assessed symptoms of major depression but did not assess for actual clinical diagnoses of depression (e.g., Major Depressive Disorder) or functional impairment, which limits our ability to make inferences regarding relations between these constructs and treatment implications for this population. Although research suggests similar correlations between (a) symptoms and dimensional depression and (b) symptoms and depressive disorders (Georgiades, Lewinsohn, Monroe, & Seeley, 2006; Kessler, Zhao, Blazer, & Swartz, 1997), future research will benefit from assessing how negative life events interact with distress tolerance to predict clinical depression. It is also not clear whether the interaction between distress tolerance and stressful life events is specific to depressive symptoms. Although not presented as part of the current study, we conducted exploratory analyses following the request of one of the reviewers of the present manuscript. The results were similar to those of the current investigation: the interaction between distress tolerance and stressful life events was predictive of a broader range of internalizing symptoms, including those related to anxiety. Therefore, an important research avenue is to ascertain the applicability of this interaction to other clinical disorders and/or symptoms. Third, the study was limited to only one behavioral task for assessing distress tolerance. Despite the noted advantages to using behavioral tasks with adolescents, pairing this task with a self-report scale may more effectively tap into both the perceived and real-time experience of DT for youth. Fourth, due to changes in assessment protocols over the course of the study, we were only able to include three waves of data. Future research should examine the longitudinal trajectories of negative life events and distress tolerance from a developmental perspective beginning in early childhood and across adolescence. Finally, future research would benefit from expanding on the current measure of negative life events in several ways. For instance, future research should consider specific types of stressful experiences (such as independent vs. dependent or interpersonal vs. achievement-oriented negative life events) and their differential role in moderating the relation between distress tolerance and depressive symptoms. Additionally, given that distress intolerant individuals may be more likely to perceive a greater number of events as stressful and may, consequently, identify more negative life events than their distress tolerant peers, future research should utilize different measurement approaches (such as interview techniques) to address these concerns. Finally, including measures of negative life events and distress tolerance at each wave would allow for us to understand more nuanced changes in their relations over time.
Notwithstanding these limitations, the study has several strengths. To our knowledge, this is one of the few studies to examine the interaction between negative life events and DT in predicting depressive symptoms, and is the first to do so in a sample of adolescents. Our study also utilized a behavioral assessment of DT which largely removes limitations that are more characteristic of self-report assessments, including retrospective bias, subjectivity, and social desirability. Finally, these findings highlight the importance of assessing the joint contribution of DT and negative life events in both clinical and research settings, and this work underscores the potential benefit of targeting distress intolerance in the context of depression prevention efforts.
Acknowledgments
This research was supported in part by a grant from the National Institute of Drug Abuse Grant R01DA018647 (primary investigator, C.W. Lejuez).
References
- Abrantes AM, Strong DR, Lejuez CW, Kahler C, Carpenter LL, Price LH, … & Brown RA (2008). The role of negative affect in risk for early lapse among low distress tolerance smokers. Addictive Behaviors, 33(11), 1394–1401. doi: 10.1016/j.addbeh.2008.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ameral V, Palm Reed KM, Cameron A, & Armstrong JL (2014). What are measures of distress tolerance really capturing? A mixed methods analysis. Psychology Of Consciousness: Theory, Research, And Practice, 1(4), 357–369. doi: 10.1037/cns0000024 [DOI] [Google Scholar]
- Amstadter AB, Daughters SB, MacPherson L, Reynolds EK, Danielson CK, Wang F, & … Lejuez CW (2012). Genetic associations with performance on a behavioral measure of distress intolerance. Journal Of Psychiatric Research, 46(1), 87–94. doi: 10.1016/j.jpsychires.2011.09.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anestis MD, Gratz KL, Bagge CL, & Tull MT (2012). The interactive role of distress tolerance and borderline personality disorder in suicide attempts among substance users in residential treatment. Comprehensive Psychiatry, 53(8), 1208–1216. doi: 10.1016/j.comppsych.2012.04.004 [DOI] [PubMed] [Google Scholar]
- Anestis MD, Knorr AC, Tull MT, Lavender JM, & Gratz KL (2013). The importance of high distress tolerance in the relationship between nonsuicidal self‐injury and suicide potential. Suicide And Life-Threatening Behavior, 43(6), 663–675. doi: 10.1111/sltb.12048 [DOI] [PubMed] [Google Scholar]
- Avenevoli S, Swendsen J, He J, Burstein M, & Merikangas KR (2015). Major depression in the national comorbidity survey–adolescent supplement: Prevalence, correlates, and treatment. Journal Of The American Academy Of Child & Adolescent Psychiatry, 54(1), 37–44. doi: 10.1016/j.jaac.2014.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey D, & Garralda ME (1990). Life events: Children’s reports. Social Psychiatry And Psychiatric Epidemiology, 25(6), 283–288. doi: 10.1007/BF00782882 [DOI] [PubMed] [Google Scholar]
- Bardeen JR, Fergus TA, & Orcutt HK (2017). Examining the specific dimensions of distress tolerance that prospectively predict perceived stress. Cognitive Behaviour Therapy, 46(3), 211–223. [DOI] [PubMed] [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR, & Zvolensky MJ (2005). Distress tolerance and early smoking lapse. Clinical Psychology Review, 25(6), 713–733. doi: 10.1016/j.cpr.2005.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Keough ME, & Schmidt NB (2007). Problematic alcohol and cannabis use among young adults: The roles of depression and discomfort and distress tolerance. Addictive Behaviors, 32(9), 1957–1963. doi: 10.1016/j.addbeh.2006.12.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burcusa SL, & Iacono WG (2007). Risk for recurrence in depression. Clinical Psychological Review, 27(8), 959–985. doi: 10.1016/j.cpr.2007.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell-Sills L, & Barlow DH (2007). Incorporating Emotion Regulation into Conceptualizations and Treatments of Anxiety and Mood Disorders. In Gross JJ (Ed.), Handbook of Emotion Regulation (pp. 542–559). New York: Guilford Press. [Google Scholar]
- Chorpita BF, Moffitt CE, & Gray J (2005). Psychometric properties of the Revised Child Anxiety and Depression Scale in a clinical sample. Behaviour Research And Therapy, 43(3), 309–322. doi: 10.1016/j.brat.2004.02.004 [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, & Francis SE (2000). Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behaviour Research and Therapy, 38(8), 835–855. doi: 10.1016/S0005-7967(99)00130-8 [DOI] [PubMed] [Google Scholar]
- Coddington RD (1972). The significance of life events as etiologic factors in the diseases of children–II: A study of a normal population. Journal of Psychosomatic Research, 16, 205–213. [DOI] [PubMed] [Google Scholar]
- Cohen JR, Danielson CK, Adams ZW, & Ruggiero KJ (2016). Distress tolerance and social support in adolescence: Predicting risk for internalizing and externalizing symptoms following a natural disaster. Journal Of Psychopathology And Behavioral Assessment, 38(4), 538–546. doi: 10.1007/s10862-016-9545-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Keller G, Angold A (2004). Prevalence of psychiatric disorders in childhood and adolescence. In: Levin BL, Petrila J, Hennessy KD, eds. Mental Health Services: a Public Health Perspective, Second Edition. Oxford, UK: Oxford University Press; 2004:111–128. [Google Scholar]
- Cummings JR, Bornovalova MA, Ojanen T, Hunt E, MacPherson L, & Lejuez C (2013). Time doesn’t change everything: The longitudinal course of distress toleranceand its relationship with externalizing and internalizing symptoms during earlyadolescence. Journal of Abnormal Child Psychology, 41(5), 735–748.doi: 10.1007/s10802-012-9704-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielson CK, Ruggiero KJ, Daughters SB, & Lejuez CW (2010). Distress tolerance, risk-taking propensity, and PTSD symptoms in trauma-exposed youth: Pilot study. The Behavior Therapist, 33(2), 28–34. [Google Scholar]
- Daughters SB, Lejuez CW, Kahler CW, Strong DR, & Brown RA (2005). Psychological Distress Tolerance and Duration of Most Recent Abstinence Attempt Among Residential Treatment-Seeking Substance Abusers. Psychology Of Addictive Behaviors, 19(2), 208–211. doi: 10.1037/0893-164X.19.2.208 [DOI] [PubMed] [Google Scholar]
- Daughters SB, Reynolds EK, MacPherson L, Kahler CW, Danielson CK, Zvolensky M, & Lejuez CW (2009). Distress tolerance and early adolescent externalizing and internalizing symptoms: The moderating role of gender and ethnicity. Behaviour Research and Therapy, 47(3), 198–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis AJ, Fischer KM, & Beevers CG (2010). Is dysphoria about being red and blue? Potentiation of anger and reduced distress tolerance among dysphoric individuals. Cognition and Emotion, 24(4), 596–608. [Google Scholar]
- Felton JW, Banducci AN, Shadur JM, Stadnik R, MacPherson L, & Lejuez CW (2017). The developmental trajectory of perceived stress mediates the relations between distress tolerance and internalizing symptoms among youth. Development And Psychopathology, doi: 10.1017/S0954579417000335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrison RJ, Kannel WB, Stokes J III, & Castelli WP (1987). Incidence and precursors of hypertension in young adults: The Framingham offspring study. Preventive Medicine, 16 (2), 235–251. [DOI] [PubMed] [Google Scholar]
- Georgiades K, Lewinsohn PM, Monroe SM, & Seeley JR (2006). Major Depressive Disorder in Adolescence: The Role of Subthreshold Symptoms. Journal Of The American Academy Of Child & Adolescent Psychiatry, 45(8), 936–944. doi: 10.1097/01.chi.0000223313.25536.47 [DOI] [PubMed] [Google Scholar]
- Gorka SM, Ali B, & Daughters SB (2012). The role of distress tolerance in the relationship between depressive symptoms and problematic alcohol use. Psychology Of Addictive Behaviors, 26(3), 621–626. doi: 10.1037/a0026386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ, & Muñoz RF (1995). Emotion Regulation and Mental Health. Clinical Psychology: Science and Practice, 2(2), 151–164. doi: 10.1111/j.1468-2850.1995.tb00036.x [DOI] [Google Scholar]
- Harrington N (2006). Frustration intolerance beliefs: Their relationship with depression, anxiety, and anger in a clinical population. Cognitive Therapy and Research, 30(6), 699– 709. doi: 10.1007/s10608-006-9061-6. [DOI] [Google Scholar]
- Hankin BL (2006). Adolescent depression: Description, causes, and interventions. Epilepsy & Behavior, 8(1), 102–114. doi: 10.1016/j.yebeh.2005.10.012 [DOI] [PubMed] [Google Scholar]
- Hankin BL, & Abramson LY (2001). Development of gender differences in depression: An elaborated cognitive vulnerability–transactional stress theory. Psychological Bulletin, 127(6), 773–796. doi: 10.1037/0033-2909.127.6.773 [DOI] [PubMed] [Google Scholar]
- Hankin BL, Mermelstein R, Roesch L (2007). Sex differences in adolescent depression: Stress exposure and reactivity models. Child Development, 78(1), 279–295. doi: 10.1111/j.1467-8624.2007.00997.x [DOI] [PubMed] [Google Scholar]
- Hawkins KA, Macatee RJ, Guthrie W, & Cougle JR (2013). Concurrent and prospective relations between distress tolerance, life stressors, and anger. Cognitive Therapy And Research, 37(3), 434–445. doi: 10.1007/s10608-012-9487-y [DOI] [Google Scholar]
- Hayes SC & Lillis J (2014). Acceptance and commitment therapy. In VandenBos G, Meidenbauer E, & Frank-McNeil J (Eds.) Psychotherapy theories and techniques: A reader (pp. 3–8). Washington, DC: American Psychological Association. [Google Scholar]
- Juarascio AS, Felton JW, Borges AM, Manasse SM, Murray HB, & Lejuez CW (2016). An investigation of negative affect, reactivity, and distress tolerance as predictors of disordered eating attitudes across adolescence. Journal Of Adolescence, 4991–98. doi: 10.1016/j.adolescence.2016.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, & … Zaslavsky AM (2005). Prevalence and Treatment of Mental Disorders, 1990 to 2003. The New England Journal Of Medicine, 352(24), 2515–2523. doi: 10.1056/NEJMsa043266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Zhao S, Blazer DG, & Swartz M (1997). Prevalence, correlates, and course of minor depression and major depression in the national comorbidity survey. Journal Of Affective Disorders, 45(1–2), 19–30. doi: 10.1016/S0165-0327(97)00056-6 [DOI] [PubMed] [Google Scholar]
- Lakdawalla Z, Hankin BL, & Mermelstein R (2007). Cognitive theories of depression in children and adolescents: A conceptual and quantitative review. Clinical Child And Family Psychology Review, 10(1), 1–24. doi: 10.1007/s10567-006-0013-1 [DOI] [PubMed] [Google Scholar]
- Laurent J, Catanzaro SJ, Joiner TJ, Rudolph KD, Potter KI, Lambert S, & … Gathright T (1999). A measure of positive and negative affect for children: Scale development and preliminary validation. Psychological Assessment, 11(3), 326–338. doi: 10.1037/1040-3590.11.3.326 [DOI] [Google Scholar]
- Lejuez CW, Daughters SB, Danielson CW, & Ruggiero K (2006). The behavioral indicator of resiliency to distress (BIRD), Unpublished manual.
- Leyro TM, Zvolensky MJ, & Bernstein A (2010). Distress tolerance and psychopathological symptoms and disorders: A review of the empirical literature among adults. Psychological Bulletin, 136(4), 576–600. doi: 10.1037/a0019712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan M (1993). Cognitive–behavioral treatment of borderline personality disorder New York, NY: Guilford Press. [Google Scholar]
- Little RJ & Rubin DB (1989). Statistical analysis with missing data New York, NY: John Wiley and Sons. [Google Scholar]
- Macatee RJ, Capron DW, Schmidt NB, & Cougle JR (2013). An examination of low distress tolerance and life stressors as factors underlying obsessions. Journal Of Psychiatric Research, 47(10), 1462–1468. doi: 10.1016/j.jpsychires.2013.06.019 [DOI] [PubMed] [Google Scholar]
- MacPherson L, Reynolds EK, Daughters SB, Wang F, Cassidy J, Mayes LC, & Lejuez CW (2010). Positive and negative reinforcement underlying risk behavior in early adolescents. Prevention Science, 11(3), 331–342. doi: 10.1007/s11121-010-0172-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, Daughters SB, Lejuez CW, Murray HW, Hearon BA, Gorka SM, Otto MW (2011). Shared variance among self-report and behavioral measures of distress intolerance. Cognitive Therapy and Research, 35(3), 266–275. doi: 10.1007/s10608-010-9295-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, & Otto MW (2011). Domain-general and domain-specific strategies for the assessment of distress intolerance. Psychology Of Addictive Behaviors, 25(4), 745–749. doi: 10.1037/a0025094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén BO, & Curran PJ (1997). General longitudinal modeling of individual differences in experimental designs: A latent variable framework for analysis and power estimation. Psychological Methods, 2(4), 371–402. doi: 10.1037/1082-989X.2.4.371 [DOI] [Google Scholar]
- Muthen LK, & Muthen BO (2010). MPLUS user’s guide (6th ed.) Los Angeles,CA: Muthen & Muthen. [Google Scholar]
- Nock MK, & Mendes WB (2008). Physiological arousal, distress tolerance, and social problem-solving deficits among adolescent self-injurers. Journal Of Consulting And Clinical Psychology, 76(1), 28–38. doi: 10.1037/0022-006X.76.1.28 [DOI] [PubMed] [Google Scholar]
- O’Cleirigh C, Ironson G, & Smits JJ (2007). Does distress tolerance moderate the impact of major life events on psychosocial variables and behaviors important in the management of HIV?. Behavior Therapy, 38(3), 314–323. doi: 10.1016/j.beth.2006.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padilla Paredes P, & Calvete Zumalde E (2015). A test of the vulnerability–stress model with brooding and reflection to explain depressive symptoms in adolescence. Journal Of Youth And Adolescence, 44(4), 860–869. doi: 10.1007/s10964-014-0148-1 [DOI] [PubMed] [Google Scholar]
- Peterson CM, Davis‐Becker K, & Fischer S (2014). Interactive role of depression, distress tolerance and negative urgency on non‐suicidal self‐injury. Personality And Mental Health, 8(2), 151–160. doi: 10.1002/pmh.1256 [DOI] [PubMed] [Google Scholar]
- Sadock BJ, & Sadock VA(2007). Kaplan & Sadock’s synopsis of psychiatry: Behavioral sciences/clinical psychiatry (Tenth edition). Philadelphia: Wolters Kluwer. [Google Scholar]
- Schweizer K (2010). Improving the interpretability of the variances of latent variables by uniform and factor-specific standardizations of loadings. Methodology: European Journal of Research Methods for the Behavioral and Social Sciences, 6(4), 152–159. doi: 10.1027/1614-2241/a000017 [DOI] [Google Scholar]
- Shaw AM, & Timpano KR (2016). An experimental investigation of the effect of stress on saving and acquiring behavioral tendencies: The role of distress tolerance and negative urgency. Behavior Therapy, 47(1), 116–129. doi: 10.1016/j.beth.2015.10.003 [DOI] [PubMed] [Google Scholar]
- Simons JS, & Gaher RM (2005). The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation And Emotion, 29(2), 83–102. doi: 10.1007/s11031-005-7955-3 [DOI] [Google Scholar]
- Spijker J, De Graaf R, Bijl RV, Beekman AF, Ormel J, & Nolen WA (2002). Duration of major depressive episodes in the general population: Results from the Netherlands Mental Health Survey and Incidence Study (NEMESIS). The British Journal Of Psychiatry, 181(3), 208–213. doi: 10.1192/bjp.181.3.208 [DOI] [PubMed] [Google Scholar]
- Steiger JH (1990). Structural model evaluation and modification: an interval estimation approach. Multivariate Behavioral Research, 25, 173–180. [DOI] [PubMed] [Google Scholar]
- Tucker LR, & Lewis C (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38(1), 1–10. doi: 10.1007/BF02291170. [DOI] [Google Scholar]
- Volz AR, Dennis PA, Dennis MF, Calhoun PS, Wilson SM, & Beckham JC (2014). The role of daily hassles and distress tolerance in predicting cigarette craving during a quit attempt. Nicotine & Tobacco Research, 16(6), 872–875. doi: 10.1093/ntr/ntt286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams AD, Thompson J, & Andrews G (2013). The impact of psychological distress tolerance in the treatment of depression. Behaviour Research and Therapy, 51(8), 469–475. doi: 10.1016/j.brat.2013.05.005 [DOI] [PubMed] [Google Scholar]
- Woody ML, Burkhouse KL, Birk SL, & Gibb BE (2015). Brooding rumination and cardiovascular reactivity to a laboratory‐based interpersonal stressor. Psychophysiology, 52(5), 722–725. doi: 10.1111/psyp.12397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, & Wang L (2009). Statistical power analysis for growth curve models using SAS. Behavior Research Methods, Instruments & Computers, 41(4), 1083–1094. doi: 10.3758/BRM.41.4.1083 [DOI] [PubMed] [Google Scholar]


