Abstract
Objectives
It has been hypothesized that patellofemoral pain, a common knee condition in adolescents and young adults, may be a precursor of degenerative joint changes and may ultimately lead to patellofemoral osteoarthritis. Since both conditions share several mechanical disease characteristics, such as altered contact area between the femur and patella and increased joint stress, we investigated whether these conditions share similar and different shape characteristics of the patella compared with normal controls.
Methods
This cross-sectional study compared three different study populations: 32 patellofemoral pain subjects (mean age, 32 years (22 to 45); 72% female); 56 isolated radiological patellofemoral osteoarthritis subjects (mean age, 54 years (44 to 58); 89% female); and 80 healthy control subjects (mean age, 52 years (44 to 58); 74% female). Measurements included questionnaires, and lateral and skyline radiographs of the knee. Two separate 30-point 2D statistical shape models of the patella were created from the lateral and skyline radiographs. A general linear model was used to test for differences in standardized shape modes (a specific shape variant of the patella) between patellofemoral osteoarthritis, patellofemoral pain, and controls, using Bonferroni correction and adjustment for body mass index and gender.
Results
Five shape modes showed statistically significant differences between groups: skyline modes 1 (p < 0.001), 8 (p = 0.004), and 10 (p < 0.001); and lateral modes 5 (p = 0.002) and 7 (p = 0.002). Skyline mode 8 and lateral mode 5 were similar for patellofemoral osteoarthritis and patellofemoral pain populations, while being statistically significant different from the control group.
Conclusion
Our results indicate that patellofemoral pain and patellofemoral osteoarthritis share similar shape characteristics, which are different from control subjects. These findings support the proposed continuum disease model of patellofemoral pain predisposing to the development of patellofemoral osteoarthritis.
Cite this article: J. F. A. Eijkenboom, J. H. Waarsing, E. H. G. Oei, S. M. A. Bierma-Zeinstra, M. van Middelkoop. Is patellofemoral pain a precursor to osteoarthritis? Patellofemoral osteoarthritis and patellofemoral pain patients share aberrant patellar shape compared with healthy controls. Bone Joint Res 2018;7:541–547. DOI: 10.1302/2046-3758.79.BJR-2018-0112.R1.
Keywords: Osteoarthritis, Knee, Radiograph, Statistical shape modelling, Patellofemoral
Article focus
It has been hypothesized that patellofemoral pain (PFP) may precede degenerative joint changes, which may ultimately lead to patellofemoral osteoarthritis (PFOA).
This study investigates the similarity of patella shape between PFP and PFOA patients using statistical shape modelling compared with healthy control subjects.
Key messages
Previous research has shown associations between bone shape and PFP and PFOA independently.
Our study shows similarities in patellar shape between PFP and PFOA patients.
The results provide further evidence of the link between PFP and PFOA, and highlights the non-self-limiting nature of PFP.
Strengths and limitations
The data from two different studies were used in our analysis. However, there were differences in both subject demographics and radiology protocols between each study.
Our study group consisted mostly of women, thus limiting the broader interpretation of our results to the population in general.
However, both PFP and PFOA are significantly more prevalent in women, thus our study appears to reflect and be representative of the patient population.
Introduction
Patellofemoral pain (PFP) or anterior knee pain is a very common problem in young adults, particularly in women, characterized by pain behind and around the patella, often without clear aetiology.1 Recent studies have suggested that PFP might predispose an individual to patellofemoral osteoarthritis (PFOA) later in life.2,3 Patellofemoral osteoarthritis has not been investigated as frequently as tibiofemoral osteoarthritis (TFOA). However, the PFJ may be the first compartment affected in early knee osteoarthritis, which later affects both the patellofemoral and tibiofemoral compartments.4-6 Moreover, a stronger association between pain and loss of function is seen in patients with isolated PFOA compared with those with isolated TFOA.4,7-9 While no evidence of a causal relationship between PFP and PFOA has been shown,3,10 there are many overlapping disease characteristics that are associated with both PFP and PFOA, including patellar malalignment, quadriceps dysfunction, hip abductor dysfunction, painful crepitus with stair-climbing, and female gender.3,11-14
One probable association that likely links PFP and PFOA is biomechanical dysfunction, since both PFP and PFOA are thought to be caused by alterations in patellofemoral joint mechanics.15,16 Alterations in patellofemoral joint mechanics, such as malalignment, joint laxity, and muscular dysfunction, lead to pain and ultimately joint degeneration.11,17 These changes may be produced by alterations in the contact area between patella and femur, resulting in increased joint contact stress and subsequent cartilage degeneration.16,18-21 Thus, joint surface shape might influence contact areas and be associated with PFP and PFOA. The influence of joint shape on knee OA and PFP has been described individually, but similar shape patterns between these conditions have never been compared or investigated.22-26
The influence of joint shape on knee OA has been described by Bredbenner et al,23 who found a greater width of the tibial plateau in anteroposterior (AP) and mediolateral (ML) direction in patients at risk of developing OA. This may be characterized as bone remodelling, one of the first signs of OA.27 An increased ML width of both the femur and tibia is also seen in AP radiographs of patients with OA.24 A recent study was able to predict the onset of knee OA, using a 3D bone shape model as the predictor.25 Several bone shape variants have been described in PFP patients, as well as OA patients. Connolly et al22 found, in a small study, that PFP patients had different contact areas with a higher prevalence of increased sagittal plane morphology ratios (patellar length/articular surface length) compared with healthy controls. Given the shared mechanical characteristics and the suggested link with joint shape, the aim of this study is to investigate possible similarities between the shape of the patella in PFOA and PFP patients using statistical shape modelling (SSM). Additionally, similarities in PFOA and PFP bone shape are compared with those of healthy control subjects. We hypothesize that there will be shape modes that show similarities between patients with PFP and PFOA, and differences compared with control subjects.
Patients and Methods
We undertook a retrospective case control study (level of evidence: III). We compared three groups: one group with a history of PFP (n = 32); one group with radiological PFOA (n = 56); and a healthy control group (n = 80). Subjects were selected from two different data sets: the baseline data from the Cohort Hip and Cohort Knee (CHECK) cohort;28 and the five- to eight-year follow-up data of a randomized clinical trial (RCT) on the effectiveness of exercise therapy for PFP.29 Informed consent was given by all subjects, and both studies were approved by the medical ethics committees of all participating centres; detailed descriptions of both study protocols can be found elsewhere.28,29 From the CHECK study, the youngest subjects (up to 58 years at baseline) diagnosed with isolated radiological PFOA were selected. Additionally, we selected 80 control subjects in the same age range from the CHECK cohort without radiological knee OA, knee pain, or stiffness. Finally, we selected all PFP subjects with skyline and AP radiographs, aged between 22 and 47 years, from the follow-up data of the RCT. This group of PFP patients could be further subdivided into patients with a favourable recovery at follow-up (‘completely recovered’ or ‘strongly recovered’) and patients with an unfavourable recovery at follow-up (‘slight improvement’ to ‘worse than ever’), measured on a seven-point Likert scale.29 From both PFOA and PFP subjects, the most painful knee was selected for the analyses; from the control subjects, a knee was selected at random.
Measurements in both studies included questionnaires and radiographs. The questionnaires in both studies recorded demographics including: age; gender; education level (dichotomized into: high, “upper level high school, university”; and low, “elementary school, lower level high school, vocational college”); weight and height, from which body mass index (BMI) was calculated; bilateral symptoms (yes/no); and side of the most painful knee. Pain was assessed in both studies using pain at rest (11-point numerical rating scale (NRS)).30 Also, pain, stiffness, and function were assessed with the Western Ontario and McMaster Universities Arthritis Index (WOMAC)31 in the CHECK study, while WOMAC scores for the RCT study were calculated using the Knee Injury and Osteoarthritis Outcome Score (KOOS).32
The study population consisted of 56 subjects with PFOA (mean age, 54 years (44 to 58, sd 2.7); mean BMI, 29 (sd 5.1); 89% female), 32 PFP patients (mean age, 32 years (22 to 45, sd 8.5); mean BMI, 25 (sd 3.8); 72% female), and 80 control subjects (mean age, 52 years (44 to 58, sd 3.5); mean BMI, 25 (sd 3.6); 74% female). Characteristics are presented in Table I.
Table I.
Descriptive characteristics and radiographic findings of patients and controls
| Control (n = 80) | PFOA (n = 56) | PFP (n = 32) | p-value | |
|---|---|---|---|---|
| Mean age, yrs (sd) | 52.3 (3.5) | 53.6 (2.7) | 32.1 (8.5) | < 0.001*†‡ |
| Female gender, n (%) | 59 (73.8) | 50 (89.3) | 23 (71.9) | 0.056* |
| Highly educated, n (%) | 28 (35) | 18 (32.1) | 14 (43.8) | < 0.001*†‡ |
| Mean body mass index, kg/m2 (sd) | 25.2 (3.6) | 28.5 (5.1) | 24.7 (3.8) | < 0.001*†§ |
| Bilateral complaints, n (%) | N/A | 25 (44.6) | 14 (43.8) | 0.740¶ |
| Right knee most affected knee, n (%) | N/A | 33 (58.9) | 12 (37.5) | 0.071¶ |
| Mean NRS pain score (0 to 10) (sd) | N/A | 3.7 (2.1) | 1.6 (2.3) | < 0.001†** |
| Mean normalized WOMAC pain score (0 to 100) (sd) | 20.4 (15.6) | 25.6 (15.9) | 45.8 (19.7) | < 0.001†** |
| Mean normalized WOMAC stiffness score (0 to 100) (sd) | 28.9 (21.2) | 35.9 (18.8) | 21.5 (21.8) | 0.002†** |
| Mean normalized WOMAC physical functioning score (0 to 100) (sd) | 17.7 (13.8) | 26.8 (17.4) | 37.7 (17.3) | 0.006†** |
| Kellgren and Lawrence score, n (%) | < 0.001*†§ | |||
| 0: None | 57 (71.3) | 13 (23.2) | 29 (90.6) | |
| 1: Doubtful | 23 (28.7) | 43 (76.8) | 3 (9.4) | |
| > 1: Minimal to severe | 0 (0) | 0 (0) | 0 (0) | |
| Osteophytes (lateral radiograph), n (%) | < 0.001*†§ | |||
| None | 63 (78.8) | 5 (8.9) | 28 (87.5) | |
| Doubtful | 16 (20) | 26 (46.4) | 4 (12.5) | |
| Minimal | 1 (1.3) | 24 (42.9) | 0 (0) | |
| Moderate | 0 (0) | 1 (1.8) | 0 (0) | |
| Osteophytes (skyline radiograph), n (%) | < 0.001*†§ | |||
| None | 48 (60) | 4 (7.1) | 26 (81.3) | |
| Doubtful | 25 (31.3) | 11 (19.6) | 6 (18.8) | |
| Minimal | 4 (5) | 37 (66.1) | 0 (0) | |
| Moderate | 0 (0) | 2 (3.6) | 0 (0) | |
| Joint space narrowing (skyline radiograph), n (%) | < 0.001*†§ | |||
| None | 73 (91.3) | 35 (62.5) | 30 (93.8) | |
| Doubtful | 3 (3.8) | 12 (21.4) | 2 (6.3) | |
| Minimal | 1 (1.3) | 7 (12.5) | 0 (0) | |
| Moderate | 0 (0) | 2 (3.6) | 0 (0) | |
| Sclerosis (skyline radiograph), n (%) | 0.006*§ | |||
| None | 77 (85.6) | 51 (91.1) | 32 (100) | |
| Doubtful | 0 (0) | 5 (8.9) | 0 (0) | |
| Minimal | 0 (0) | 0 (0) | 0 (0) | |
| Moderate | 0 (0) | 0 (0) | 0 (0) |
One-way analysis of variance
Statistically significant difference between PFOA and PFP group
Statistically significant difference between control and PFP group
Statistically significant difference between control and PFOA group
Chi-squared test
Unpaired Student’s t-test
PFOA, patellofemoral osteoarthritis; PFP, patellofemoral pain; N/A, not available; NRS, numerical rating scale; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index
The radiological measurements for both studies consisted of semi-flexed weight-bearing AP radiographs, weight-bearing lateral radiographs, and skyline radiographs (30° and 45° knee flexion for CHECK and RCT study, respectively). Individual features of OA were scored according to the method of Altman et al.33 The Kellgren and Lawrence (K&L) scores were recorded from the AP radiographs and used to exclude TFOA patients from all subject groups.34
All individual features were scored by four different observers in the CHECK cohort. The interobserver reliability of K&L scoring in the CHECK cohort has been described previously, indicating fair to near perfect reliability (interobserver with trained reader prevalence bias adjusted κ score: 0.28 to 0.79).35 The radiographs of the PFP patients were scored by a trained medical student who was unaware of the context of the study and had established reliability (inter-observer with trained reader prevalence bias adjusted κ score: 0.61 to 0.75).
Radiological PFOA was defined according to the methods of Duncan et al36 and Baker et al.37 The presence of isolated PFOA was defined as a K&L score < 2 combined with: 1) an osteophytes grade ⩾ 2 on skyline radiographs; 2) an osteophytes grade ⩾ 2 on lateral radiographs; or 3) grade ⩾ 2 joint space narrowing and grade ⩾ 1 osteophytes on skyline radiographs.
Statistical shape models (SSM) were used to analyze the shape of the patella. A SSM quantitatively describes the complete variation in shape within a population by a set of statistically independent measures called modes. Each mode describes a specific shape variant of, in this case, the patella. The value of a mode for a specific patient indicates how strongly the shape variant, represented by the mode, is present in that patient. Therefore, if two patients had similar values for all the modes of variance, their patellae would be nearly identical. Two patients with vastly different values for all modes would have patellae, which look completely different. Even one different mode of variance can completely change the shape of a patella. Two separate SSMs were constructed from both the lateral and skyline radiographs. We limited the number of modes by restricting the SSMs to describe no more than 95% of the shape variation in our data set, as is customary in statistical shape modelling. Freely available active shape model software tools, described by Cootes et al,38 were used to construct our SSMs. We used a 30-contour-point model to describe the patella in both models. These models were constructed by placing two points on distinct landmarks of the patella (the most lateral and medial corners on the skyline view, and the most superior and inferior corners for the lateral view) and semi-automatically placing the other points, at equal distance between these landmarks, using the active shape model within the software. After all points were applied to all subjects, the software used principal component analysis to transform the coordinates of the contour points into a smaller set of independent variables, the shape modes.
Statistical analysis
Descriptive statistics were used to describe the demographics, pain, and function of the subjects. Differences between the three study groups were tested using unpaired Student’s t-tests (NRS, WOMAC scores), chi-squared tests (bilateral complaints, side of most affected knee), and one-way analysis of variance (ANOVA) (age, gender, education level, BMI, K&L scores, osteophytes, joint space narrowing, sclerosis), after confirming normal distributions. A general linear model with post hoc analysis, using Bonferroni correction for multiple testing, was used to assess the association between independent shape modes and group status (PFOA, PFP, or control), both with and without adjusting for gender and BMI.39 Residuals followed a normal distribution (Shapiro–Wilk and QQ plots) and had homogeneous variance (Levene’s test). Mean values for each group and mean differences between groups of standardized shape modes were reported for all statistically significant modes. Statistical significance was set at p < 0.05. Differences in modes associated with PFP between the PFP subgroups with a favourable recovery and unfavourable recovery at follow-up were tested using Student’s t-test, also using a Bonferroni correction for multiple comparisons. Missing values were handled by performing complete case analysis, only using subjects who have no missing values in the analysis.
Results
Compared with PFOA patients, PFP patients were significantly younger (p < 0.001, one-way ANOVA), higher educated (p < 0.001, one-way ANOVA), had a lower BMI (p < 0.001, one-way ANOVA), less pain (NRS) (p < 0.001, unpaired Student’s t-test) and higher WOMAC pain (p < 0.001, unpaired Student’s t-test), stiffness (p = 0.002, unpaired Student’s t-test), and function scores (p = 0.006, unpaired Student’s t-test). A K&L score of 1 was seen in 28.7% of the control patients compared with 76.8% in the PFOA group and only 9.4% in the PFP group.
The skyline shape analysis consisted of 150 subjects (12 control and six PFOA cases from the CHECK data, 18 in total, were excluded due to poor quality of the radiograph) while the lateral shape analysis consisted of 156 subjects (ten control and two PFOA cases from the CHECK data, 12 in total, were excluded due to poor quality of the radiograph). The skyline model produced 12 modes of variance (Supplementary figure a), while the lateral model produced 17 modes of variance (Supplementary figure b). This resulted in a Bonferroni adjusted threshold for significance of 0.004 and 0.003, respectively.
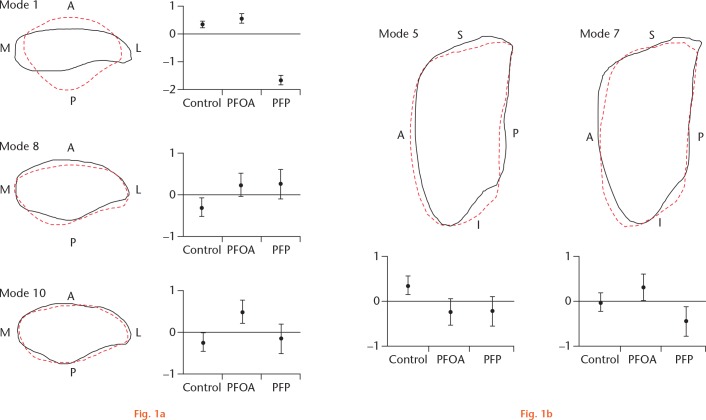
The skyline shape model showed statistically significant associations between group status and modes 1, 8, and 10 (Table II, Fig. 1a). Post hoc analyses revealed statistically significant differences in skyline shape between all three subject groups within mode 1 (Table III). In addition, statistically significant differences were found between the control subjects and both PFOA and PFP subjects in mode 8. Mode 10 showed a statistical significant difference between the PFOA subjects compared with both control and PFP subjects. Adjustment for gender and BMI did not influence the strength of the three associations. Modes 1, 8, and 10 described a variance within the population of 43%, 1.9%, and 1.1%, respectively.
Table II.
Mean values (and standard deviations) of standardized modes and p-values of group associations
| Control | PFOA | PFP | p-value* | Adjusted p-value* | |
|---|---|---|---|---|---|
| Skyline mode 1 | 0.33 (0.51) | 0.54 (0.58) | -1.68 (0.47) | < 0.001 | < 0.001 |
| Skyline mode 2 | 0.18 (0.94) | -0.28 (1.14) | -0.15 (0.72) | 0.031† | 0.040† |
| Skyline mode 8 | -0.30 (0.96) | 0.24 (0.98) | 0.26 (1.02) | 0.004 | 0.006 |
| Skyline mode 10 | -0.24 (0.89) | 0.48 (0.99) | -0.16 (0.98) | < 0.001 | < 0.001 |
| Lateral mode 4 | 0.09 (1.03) | -0.29 (0.90) | 0.15 (0.91) | 0.048† | 0.053† |
| Lateral mode 5 | 0.33 (0.89) | -0.25 (1.09) | -0.22 (0.94) | 0.002 | 0.003 |
| Lateral mode 7 | -0.02 (0.95) | 0.32 (0.99) | -0.45 (0.98) | 0.002 | 0.005 |
A general linear model with Bonferroni correction was used to assess the association between independent shape modes and group status, both with and without adjusting for gender and body mass index
Considered as non-significant following Bonferroni correction
a) Skyline and b) lateral modes displayed as -2.5 (dashed red line) and +2.5 (solid black line) standard deviations for visualization purposes. Error bars show mean values of groups (2× standard error) for corresponding modes. Anterior (A), medial (M), lateral (L), posterior (P), superior (S), and inferior (I) locations are defined. PFOA, patellofemoral osteoarthritis; PFP, patellofemoral pain.
Table III.
Post hoc analysis between groups (general linear models using pairwise comparisons)
| Variance explained, % | p-value, control vs PFP | p-value, control vs PFOA | p-value, PFP vs PFOA | |
|---|---|---|---|---|
| Skyline mode 1 | 43 | < 0.001* | 0.047* | < 0.001* |
| Skyline mode 8 | 1.9 | 0.020* | 0.044* | 1.000 |
| Skyline mode 10 | 1.1 | 1.000 | < 0.001* | 0.008* |
| Lateral mode 5 | 8.5 | 0.022* | 0.012* | 1.000 |
| Lateral mode 7 | 4.0 | 0.096 | 0.302 | 0.004* |
Statistically significant
The lateral shape model showed statistically significant associations for group status and mode 5 and 7 (Fig. 1b). Post hoc analysis showed statistically significant differences in lateral patellar shape between control subjects and both PFOA and PFP subjects in mode 5 (Table III). In addition, post hoc analysis showed statistically significant differences in lateral patellar shape between PFOA and PFP subjects in mode 7. Adjustment for gender and BMI did not influence the strength of these associations. Mode 5 and 7 described a variance within the population of 8.5% and 4.0%, respectively. No significant differences (p < 0.05) were seen on any of the five statistically significant modes of the shape models between the subgroups of PFP patients with and without a favourable recovery.
Discussion
Our study gave us the unique opportunity to study patellar bone shape in three distinct populations. Two shape variants were similar for both the PFOA and PFP groups and statistically different from the control group. The first shape variant indicates that both PFOA and PFP subjects have a more lateral positioned vertical ledge on the posterior side of the patella (Fig. 1, skyline mode 8, solid black line) compared with the healthy control group. Additionally, both PFOA and PFP subjects seem to have a rounder inferior-posterior articular area on their patella, increasing the articular surface area (Fig. 1, lateral mode 5, dashed red line) when compared with the control subjects. It has been suggested that this longer inferior-posterior area negatively affects the fit of the patella within the trochlear groove, consequently leading to increased shear forces and joint stresses and finally leading to cartilage degeneration,11 while an increased articular surface area on the patella has been positively correlated with maltracking.26 Therefore, the results seem to support the hypothesis that the initial onset of PFOA commences early in PFP patients, which might be a result of aberrant patellofemoral joint (PFJ) kinematics that are already present in younger PFP knees.
The associations found in skyline mode 1 and 10 are only correlated with either PFP or PFOA. Mode 1 suggests a large difference in bone shape, indicating that PFP patients have a more circular patella in the frontal plane, compared with control and PFOA subjects. However, this large difference may be a consequence of differences in knee flexion angle in the radiography protocol between the CHECK cohort and long-term RCT follow-up data. Skyline mode 10 suggests changes in vertical ledge depth and positioning similar to mode 8, but here only the PFOA subjects were different from the control group. The vertical ledge on the patella again seems to be located more laterally in PFOA subjects compared with control subjects, but also compared with PFP subjects. Lateral mode 7 suggests that subjects with PFP have a wider inferior patella compared with PFOA subjects, while at the same time being smaller and rounder on the superior side.
While our findings suggest that PFP and PFOA share similar patella shape variants, certain limitations should be acknowledged. First, we used data from two different studies and, consequently, slightly different radiography protocols. In particular, the difference in knee flexion angle between the cohort and RCT for the skyline radiographs might have had an effect on the projected 2D bone shape. This difference in projection angle appears to be captured in skyline mode 1. The other modes are unaffected by differences in projection angle since all modes are statistically independent as a result of their construction through Principal Component Analysis, which is part of the SSM.
Some of the shape differences found between our study populations might be explained by age differences. This is, however, inherent to our study, as we compared a condition that is more prevalent in a younger population (i.e. PFP) to a condition that affects a relatively older population (i.e. PFOA). Additionally, a disadvantage of shape modes is that it is not intuitively understood what these modes truly represent, since each mode is a composite of different correlated shape aspects. However, a mode might be used to derive a more intuitive geometrical marker, which can be measured directly and could be used in future studies as a prognostic or diagnostic biomarker. However, such a measure will only partly represent a shape mode and thus might not have the same associative strength of a shape mode.
Our study groups consisted largely of female patients, limiting the generalizability of our study in male populations. However, both OA40 and PFP41 are significantly more prevalent in women, and therefore our population seems to be a good representation of the patient population as a whole.
Finally, we only modelled the shape of the patella, without considering the surface and effects of the femur. This limits generalizability of the results of our study to the patella only, and we are therefore not able to draw any conclusions as to the fit between the patella and the femoral trochlea. The fit between patella and trochlea is impossible to study in 2D radiographs, and the trochlear groove is not completely visible in the skyline radiographs. By only modelling the patella, we were able to detect very sensitive local or regional differences within the patella shape, which may be associated the PFP and PFOA.
In summary, we have demonstrated that some shape aspects, derived from radiograph-based 2D patellar bone shape modeling, are similar in subjects with PFP and PFOA, and differ from normal controls. These findings give support to the hypothesis that suggests altered patellofemoral joint kinematics leads to increase peak joint stress and pain in the young patient and may predispose to patellofemoral OA at a later life.
Footnotes
Author Contributions: J. F. A. Eijkenboom: Designing the study, Analyzing and interpreting the data, Drafting and revising the manuscript.
J. H. Waarsing: Designing the study, Analyzing and interpreting the data, Revising the manuscript.
E. H. G. Oei: Designing the study, Interpreting the data, Revising the article.
S. M. A. Bierma-Zeinstra: Designing the study, Interpreting the data, Revising the article.
M. van Middelkoop: Designing the study, Analyzing and interpreting the data, Revising the manuscript.
Conflict of Interest Statement: None declared
Follow us @BoneJointRes
Supplementary material
Images showing modes of variance for the skyline and lateral models.
Funding Statement
The Cohort Hip and Cohort Knee (CHECK) study was funded by the Dutch Arthritis Foundation. The randomized clinical trial long-term follow-up was funded by The Royal Dutch Society for Physical Therapy (KNGF/WCF) and The Netherlands Organisation for Health Research and Development (ZON-MW), and partly funded by a programme grant of the Dutch Arthritis Foundation. The present study was financially supported by the Dutch Arthritis Foundation.
References
- 1. Rathleff MS, Skuldbøl SK, Rasch MNB, et al. Care-seeking behaviour of adolescents with knee pain: a poplation-based study among 504 adolescents. BMC Musculoskelet Disord 2013;14:225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Thomeé R, Augustsson J, Karlsson J. Patellofemoral pain syndrome: a review of current issues. Sport Med 1999;28:245–262. [DOI] [PubMed] [Google Scholar]
- 3. Crossley KM. Is patellofemoral osteoarthritis a common sequela of patellofemoral pain? Br J Sports Med 2014;48:409–410. [DOI] [PubMed] [Google Scholar]
- 4. Duncan R, Peat G, Thomas E, Hay EM, Croft P. Incidence, progression and sequence of development of radiographic knee osteoarthritis in a symptomatic population. Ann Rheum Dis 2011;70:1944–1948. [DOI] [PubMed] [Google Scholar]
- 5. Stefanik JJ, Guermazi A, Roemer FW, et al. Changes in patellofemoral and tibiofemoral joint cartilage damage and bone marrow lesions over 7 years: The Multicenter Osteoarthritis Study. Osteoarthritis Cartilage 2016;24:1160-1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. van Middelkoop M, Bennell KL, Callaghan MJ, et al. International patellofemoral osteoarthritis consortium: consensus statement on the diagnosis, burden, outcome measures, prognosis, risk factors and treatment. Semin Arthritis Rheum 2018;47:666-675. [DOI] [PubMed] [Google Scholar]
- 7. Duncan R, Peat G, Thomas E, et al. Does isolated patellofemoral osteoarthritis matter? Osteoarthritis Cartilage 2009;17:1151–1155. [DOI] [PubMed] [Google Scholar]
- 8. Stefanik JJ, Niu J, Gross KD, et al. Using magnetic resonance imaging to determine the compartmental prevalence of knee joint structural damage. Osteoarthritis Cartilage 2013;21:695–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hinman RS, Crossley KM. Patellofemoral joint osteoarthritis: an important subgroup of knee osteoarthritis. Rheumatology 2007;46:1057–1062. [DOI] [PubMed] [Google Scholar]
- 10. Thomas MJ, Wood L, Selfe J, Peat G. Anterior knee pain in younger adults as a precursor to subsequent patellofemoral osteoarthritis: a systematic review. BMC Musculoskelet Disord 2010;11:201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mills K, Hunter DJ. Patellofemoral joint osteoarthritis: an individualised pathomechanical approach to management. Best Pract Res Clin Rheumatol 2014;28:73–91. [DOI] [PubMed] [Google Scholar]
- 12. Lankhorst NE, Bierma-Zeinstra SMA, van Middelkoop M. Risk factors for patellofemoral pain syndrome: a systematic review. J Orthop Sports Phys Ther 2012;42:81-94. [DOI] [PubMed] [Google Scholar]
- 13. Peat G, Duncan RC, Wood LR, Thomas E, Muller S. Clinical features of symptomatic patellofemoral joint osteoarthritis. Arthritis Res Ther 2012;14:R63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kobayashi S, Pappas E, Fransen M, Refshauge K, Simic M. The prevalence of patellofemoral osteoarthritis: a systematic review and meta-analysis. Osteoarthritis Cartilage 2016;24:1697-1707. [DOI] [PubMed] [Google Scholar]
- 15. Hunter DJ, Zhang YQ, Niu JB, et al. Patella malalignment, pain and patellofemoral progression: the Health ABC Study. Osteoarthritis Cartilage 2007;15:1120-1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sheehan FT, Derasari A, Brindle TJ, Alter KE. Understanding patellofemoral pain with maltracking in the presence of joint laxity: complete 3D in vivo patellofemoral and tibiofemoral kinematics. J Orthop Res 2009;27:561–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fulkerson JP, Shea KP. Current concepts review: disorder of patellofemoral alignment. J Bone Joint Surg [Am] 1990;72-A:1424–1429. [PubMed] [Google Scholar]
- 18. Teng H-L, MacLeod TD, Kumar D, et al. Individuals with isolated patellofemoral joint osteoarthritis exhibit higher mechanical loading at the knee during the second half of the stance phase. Clin Biomech 2015;30:383-390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Herzog W, Diet S, Suter E, et al. Material and functional properties of articular cartilage and patellofemoral contact mechanics in an experimental model of osteoarthritis. J Biomech 1998;31:1137–1145. [DOI] [PubMed] [Google Scholar]
- 20. Salsich GB, Perman WH. Patellofemoral joint contact area is influenced by tibiofemoral rotation alignment in individuals who have patellofemoral pain. J Orthop Sports Phys Ther 2007;37:521–528. [DOI] [PubMed] [Google Scholar]
- 21. Fitzpatrick CK, Baldwin MA, Laz PJ, et al. Development of a statistical shape model of the patellofemoral joint for investigating relationships between shape and function. J Biomech 2011;44:2446–2452. [DOI] [PubMed] [Google Scholar]
- 22. Connolly KD, Ronsky JL, Westover LM, Küpper JC, Frayne R. Differences in patellofemoral contact mechanics associated with patellofemoral pain syndrome. J Biomech 2009;42:2802–2807. [DOI] [PubMed] [Google Scholar]
- 23. Bredbenner TL, Eliason TD, Potter RS, et al. Statistical shape modeling describes variation in tibia and femur surface geometry between Control and Incidence groups from the osteoarthritis initiative database. J Biomech 2010;43:1780–1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Haverkamp DJ, Schiphof D, Bierma-Zeinstra SM, Weinans H, Waarsing JH. Variation in joint shape of osteoarthritic knees. Arthritis Rheum 2011;63:3401–3407. [DOI] [PubMed] [Google Scholar]
- 25. Neogi T, Bowes MA, Niu J, et al. Magnetic resonance imaging-based three-dimensional bone shape of the knee predicts onset of knee osteoarthritis: data from the osteoarthritis initiative. Arthritis Rheum 2013;65:2048–2058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Harbaugh CM, Wilson NA, Sheehan FT. Correlating femoral shape with patellar kinematics in patients with patellofemoral pain. J Orthop Res 2010;28:865–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Burr DB, Gallant MA. Bone remodelling in osteoarthritis. Nat Rev Rheumatol 2012;8:665–673. [DOI] [PubMed] [Google Scholar]
- 28. Wesseling J, Boers M, Viergever MA, et al. Cohort Profile : Cohort Hip and Cohort Knee ( CHECK ) study. Int J Epidemiol 2016;45:36-44. [DOI] [PubMed] [Google Scholar]
- 29. Lankhorst NE, van Middelkoop M, Crossley KM, et al. Factors that predict a poor outcome 5–8 years after the diagnosis of patellofemoral pain: a multicentre observational analysis. Br J Sports Med 2016;50:881–886. [DOI] [PubMed] [Google Scholar]
- 30. Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken) 2011;63 Suppl 11:S240-52. [DOI] [PubMed] [Google Scholar]
- 31. Jinks C, Jordan K, Croft P. Measuring the population impact of knee pain and disability with the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC). Pain 2002;100:55-64. [DOI] [PubMed] [Google Scholar]
- 32. Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 2003;1:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage 2007;15(Suppl A):A1-A56. [DOI] [PubMed] [Google Scholar]
- 34. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957;16:494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Damen J, Schiphof D, Wolde ST, et al. Inter-observer reliability for radiographic assessment of early osteoarthritis features: the CHECK (cohort hip and cohort knee) study. Osteoarthritis Cartilage 2014;22:969–974. [DOI] [PubMed] [Google Scholar]
- 36. Duncan RC, Hay EM, Saklatvala J, Croft PR. Prevalence of radiographic osteoarthritis-it all depends on your point of view. Rheumatology 2006;45:757–760. [DOI] [PubMed] [Google Scholar]
- 37. Baker KR, Xu L, Zhang Y, et al. Quadriceps weakness and its relationship to tibiofemoral and patellofemoral knee osteoarthritis in Chinese: the Beijing osteoarthritis study. Arthritis Rheum 2004;50:1815–1821. [DOI] [PubMed] [Google Scholar]
- 38. Cootes TF, Taylor CJ. Statistical Models of Appearance for Computer Vision. 2004. http://www.face-rec.org/algorithms/aam/app_models.pdf (date last accessed 31 August 2018).
- 39. Bland JM, Altman DG. Multiple significance tests: the Bonferroni method. BMJ 1995;310:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. O’Connor MI. Osteoarthritis of the hip and knee: sex and gender differences. Orthop Clin North Am 2006;37:559–568. [DOI] [PubMed] [Google Scholar]
- 41. Boling M, Padua D, Marshall K, et al. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports 2010;20:725–730. [DOI] [PMC free article] [PubMed] [Google Scholar]