Hypertension is the most prevalent treatable cardiovascular disease affecting approximately one in four adults or 140 million USA residents. It affects men and women in all socioeconomic groups equally. If untreated, hypertension is a major cause of stroke, coronary heart disease and renal failure as well as other conditions. Easily diagnosed, and in most instances readily controlled, hypertension is often unsuspected or inadequately treated.
The causes of high blood pressure are a bit of a mystery. According to the National Heart, Lung and Blood Institute, as many as 25% of adult Americans suffer from high blood pressure. Results of the Croatian national survey performed in 1997 in a sample of 5840 persons of both sexes, aged 18-65, showed about 28% adults to be hypertensive (BP>140/90 mm Hg), with a significantly greater prevalence recorded in men (32%) than in women (24 %).
7.1 The causes of high blood pressure
In most people, no specific cause of high blood pressure can be identified. It appears to be a distinct entity, due in part to a genetic predisposition (essential hypertension). As much as 95% of the people with high blood pressure have essential hypertension. The probability of developing hypertension increases with age. More than half of all persons aged 65 are hypertensive. Treating high blood pressure significantly decreases the risk of stroke, myocardial infarction and cardiovascular death. Another type of high blood pressure called secondary hypertension is more common in younger individuals, usually due to some other problem (for example, persons taking birth control pills, renovascular patients, etc.).
About 5% of patients requiring hypertension treatment can trace their high blood pressure to a physical cause such as kidney disease, however for 95% of patients who undergo hypertension treatment the causes of high blood pressure are unknown.
High risk groups. African Americans have a greater risk of developing hypertension than Caucasian Americans. Men are more likely to develop high blood pressure than women, and to develop hypertension at an earlier age. After the menopause, women become more susceptible to high blood pressure.
Hypertension is a major contributor to coronary heart disease and stroke, the two leading causes of death among adults worldwide. It is a silent epidemic affecting both sexes and rising with age. Hypertension, which affects approximately one in four adults in the USA, has an important role as an aetiological factor in the most prevalent treatable conditions such as cardiovascular disease. Untreated hypertension is a major cause of stroke, coronary heart disease (myocardial infarction), congestive heart failure and renal failure, as well as other conditions. Hypertension as a potentially serious condition produces various symptoms like sweating, palpitation, headache, and dizziness. Numerous scientific studies have estimated that between 55 and 70 million of the 140 million adults suffering from hypertension are unaware of it, and of those who know, fewer than half may be appropriately treated. Only 27% of all hypertensive patients in the USA are being treated appropriately. It is well known that the treatment of high blood pressure significantly decreases the risk of developing potentially fatal conditions.
In general, high blood pressure, or hypertension is defined as a systolic pressure of 140 mm Hg or greater and/or diastolic pressure of 90 mm Hg or greater, considered to be above the normal range. Definition of hypertension according to the guidelines of World Health Organization - International Society of Hypertension (1999) is presented in Table 2 and classification of blood pressure for adults according to Joint National Committee in Table 3.
Table 2.
Definition of hypertension according to the World Health Organization and the International Society of Hypertension (WHO/ISH) 1999
| Category | Systolic | Diastolic |
|---|---|---|
| Optimal | <120 | <80 |
| Normal | <130 | <85 |
| High-normal | 130-139 | 85-89 |
| Grade 1 hypertension (mild) | 140-159 | 90-99 |
| Subgroup: borderline | 140-149 | 90-94 |
| Grade 2 hypertension (moderate) | 160-179 | 100-109 |
| Grade 3 hypertension (severe) | ?180 | ?110 |
| Isolated systolic hypertension | ?140 | <90 |
| Subgroup: borderline | 140-149 |
Table 3.
Classification of blood pressure for adults aged 3 18 according to Joint National Committee (JNC VI)
| Category | Systolic (mm Hg) | Diastolic (mm Hg) |
|---|---|---|
| Optimal | <120 and | <80 |
| Normal | <130 and | <85 |
| High-normal | 130-139 or | <85-89 |
| Hypertension | ||
| Stage 1 | 140-159 or | 90-99 |
| Stage 2 | 160-179 or | 100-109 |
| Stage 3 | ?180 or | ?110 |
7.2 Diagnosis
Hypertension is often referred to as a silent killer because the symptoms are often unnoticeable until complications occur. High blood pressure has a long asymptomatic period despite existing cardiovascular damage or kidney failure. The diagnosis of hypertension depends on careful blood pressure measurements and evaluation of the major risk factors. Two readings have to be taken together and averaged. Laboratory testing includes blood tests (haemoglobin and packed red cell volume, electrolytes, fasting blood glucose, serum lipids, serum creatinine levels, and serum uric acid), urine analyses (glycosuria, albuminuria), as well as evidence of the heart muscle thickening seen on electrocardiogram (cardiac rhythm, signs of myocardial ischemia or myocardial infarction) and left ventricular hypertrophy or echocardiogram. Thorough history, physical examination and baseline laboratory data should be obtained in the patient whose blood pressure is usually above 140/90 mm Hg to assess the overall cardiovascular risk and to exclude identifiable causes of hypertension.
7.3 Risk stratification
In addition to blood pressure, JNC-VI recognizes the need to take into consideration other cardiovascular risk factors, target organ damage and coexistent cardiovascular disease to determine the overall risk profile of each patient and the need for drug therapy. In patients who have a low overall cardiovascular risk, even with a blood pressure as high as 160/100 mm Hg, lifestyle modifications alone are recommended initially. On the other hand, in patients at a high overall risk, such as those with diabetes, antihypertensive drug therapy is recommended even when the blood pressure is below 140/90 mm Hg. The treatment goal in these patients is a blood pressure of less than 130/85 mm Hg. In patients at risk, immediate drug therapy may be necessary.
7.4 Hypertension treatments
Today, there is a general agreement that not only severe but also mild-moderate hypertension should be treated. There is no full consensus on when to start antihypertensive treatment, and what is the first line drug treatment. The goal of antihypertensive therapy has to be individual in order to optimize the benefits and minimize the risk for each patient.
Antihypertensive drugs should be given initially in a relatively low dosage to avoid blood pressure lowering. The need to “start low and go slow” is even greater in the elderly, whose blood pressure should be reduced by gradual titration
The list of the more common approaches:
Antihypertensive drugs
Exercise
Quitting smoking
Regular blood pressure monitoring
Stress reduction
Dietary changes
Weight loss
Controlling cholesterol levels
Reducing alcohol consumption
Lifestyle modifications for hypertension prevention and management:
Lose weight if overweight
Limit alcohol intake to no more than 30 ml of ethanol (720 ml of beer, 300 ml of wine, or 60 ml of 100-proof whiskey) per day or 15 ml of ethanol per day
Increase aerobic physical activity (30-45 min most days of the week)
Reduce sodium intake to no more than 100 mmol/d (2.4 g of sodium or 6 g of sodium chloride)
Maintain adequate intake of dietary potassium (approximately 90 mmol/d)
Maintain adequate intake of dietary calcium and magnesium for general health
Stop smoking and reduce intake of dietary saturated fat and cholesterol for overall cardiovascular health
Antihypertensive treatment now include six classes of antihypertensive agents according to WHO-ISH guidelines (1999):
Diuretics
Beta-blockers
ACE inhibitors
Calcium antagonists
Alfa-blockers
AT1-receptor blockers
Strong clinical evidence supports the “compelling indications,” as designated in the JNC-VI report, of certain drugs in four conditions that may accompany hypertension: diabetes with nephropathy (angiotensin converting enzyme [ACE] inhibitors); congestive heart failure (ACE inhibitors and diuretics); systolic hypertension in the elderly (diuretics and long-acting dihydropyridine calcium antagonists) and postmyocardial infarction (beta blockers with nonintrinsic sympathomimetic activity and with systolic dysfunction, ACE inhibitors).
The combinations of different antihypertensive drugs should be added until the goal blood pressure below 140/90 mmHg is reached, and even lower in those patients with renal insufficiency, diabetes or congestive heart failure
7.5 Coronary heart disease
Some 7 million Americans suffer from coronary heart disease (CHD), the most common form of heart disease. CHD is the number one killer of both men and women in the U.S. Each year, more than 500,000 Americans die of heart attacks caused by CHD.
Many of these deaths could be prevented because CHD is related to certain aspects of lifestyle. Risk factors for CHD include hypertension, high blood cholesterol, smoking, obesity, and physical inactivity - all of which can be controlled. Although medical treatments for heart disease have come a long way, the control of risk factors remains the key to preventing illness and death from CHD.
Risk factors that increase the risk of developing coronary heart disease:
Controllable:
Hypertension
High blood cholesterol
Smoking
Obesity
Physical inactivity
Diabetes
Stress
Uncontrollable:
Gender
Heredity (family history of CHD)
Age
Approximately 4 to 5 million patients will be evaluated in US emergency departments for chest pain. Of these patients 2 million will be diagnosed as having an acute ischemic syndrome. More than half a million of these patients will be hospitalized with a diagnosis of unstable angina, and 1.5 million will experience an acute myocardial infarction (AMI). Of the 1.5 million AMI patients, approximately half a million will die, and 50% of these deaths will occur within the first hour. Including prehospital mortality, the first prolonged attack of ischemic pain has a 34% fatality rate.
1.5.1 Symptoms of coronary heart disease
The term “acute coronary syndrome” has become commonly used to refer to patients presenting with ischemic chest pain. Chest pain (angina) or shortness of breath may be the earliest sign of CHD. The other clinical manifestations of CHD are: heaviness, tightness, pain, burning, pressure, or squeezing, usually behind the breastbone but sometimes also in the arms, neck, or jaws. Nevertheless, some people have heart attacks without ever having any of these symptoms.
Nomenclature of acute coronary syndromes (ACS):
Unstable angina
Non-Q-wave myocardial infarction
Q-wave myocardial infarction
Discriminating among the acute coronary syndromes requires integration of clinical information, the amount and timing of cellular necrosis, examination of the cardiac markers (troponin I and T), and serial records of the 12-lead electrocardiogram (ECG).
(Modified from AHCPR. Clinical Practice Guideline - Unstable Angina.)
All of the coronary syndromes are initiated by the same event - rupture of an unstable, lipid-rich atheromatous plaque in an epicardial artery. Plaque disruption and fissuring activates platelet adhesion, fibrin clot formation, and coronary thrombosis. Without flow restriction these plaques do not cause clinical angina. Such plaques, however, have a lipid-rich core that makes them soft and prone to rupture. Inflammatory cells have been found in areas of plaque rupture. Stable plaques have less lipid and a thick cap that makes them more resistant to fissuring and formation of thrombi.
1.5.2 Diagnosis and tests for coronary heart disease
There is no single simple test for the diagnosis of CHD. Various diagnostic procedures have been used to establish CHD, after taking careful medical history and physical examination to determine its extent and severity, and to rule out other possible causes of symptoms.
An examination for CHD may include the following tests:
New blood tests, which measure the level of particular enzyme markers (CK isoforms, troponin T and I, myoglobin) that rise with heart tissue damage, also help quickly diagnose a heart attack.
Electrocardiogram (ECG) is a graphic record of the electrical activity of the heart. Abnormal heartbeats and some areas of damage, inadequate blood flow, and heart enlargement can be detected on the records.
Exercise stress test (also called a treadmill test or exercise ECG) is used to record the heartbeat during exercise and blood pressure. In the test, an ECG is done before, during, and after exercising on a treadmill. ECG identifies any exercise stress-related abnormalities. Breathing rate may be measured as well. Exercise tests are useful but are not completely reliable; false positives (showing a problem where none exists) and false negatives (showing no problem when something is wrong) are fairly common.
Nuclear scanning is sometimes used to show damaged areas of the heart and expose problems with the heart’s pumping action. A small amount of radioactive material is injected into a vein, usually in the arm. A scanning camera records the nuclear material that is taken up by heart muscle (healthy areas) or not taken up (damaged areas).
Coronary angiography (or arteriography) is a test used to explore coronary arteries by a series of x- rays. During an angiogram a fine, long flexible tube (catheter) is inserted into the artery of an arm or leg and passed through the tube into the arteries of the heart. The heart and blood vessels are then filmed while the heart pumps. Angiogram shows the flow within the coronary arteries and identifies any areas of narrowing or blockage caused by atherosclerosis.
7.6 Concepts of treatment and assessment
One of the major insights from the reperfusion era is that significant myocardial salvage is achieved not just from thrombolytic agents. Important benefits in long-term mortality and morbidity emerge from proper and early use of oxygen, ß-blockers, nitroglycerin, aspirin, heparin, and angiotensin-converting enzyme (ACE) inhibitors. From these insights has come the concept of three types of therapy:
Reperfusion therapy - either thrombolytics or primary PTCA
Adjunctive therapy - agents given instead of or in addition to thrombolytics
Conjunctive therapy -agents given to enhance the benefits of thrombolytics
Modifying lifestyles in populations can have major protective effects against high blood pressure and various cardiovascular diseases. Lowering high blood pressure decreases death from stroke, coronary events and heart failure, slows progression of renal failure, prevents progression to severe complications of hypertension, and reduces all-cause mortality.
The goal of various international actions is to reduce morbidity, disability and premature mortality due to cardiovascular diseases with special attention to the prevention and control of hypertension by sharing knowledge, experience and technology in hypertension prevention among interested parties. Although medical treatments for heart disease have come a long way, the control of risk factors remains the key to preventing illness and death from coronary heart disease.
Figure 1.
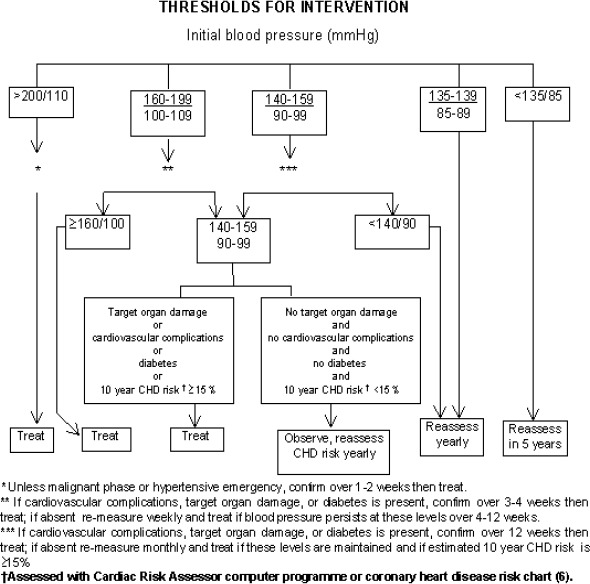
Algorithm for intervention according to blood pressure findings
Table 1.
Components of coronary risk stratification in patients with hypertension
| Major risk factors |
| Smoking Dyslipidemia Diabetes mellitus Age >60 y Sex (men and postmenopausal women) Family history of cardiovascular disease: women <65 y or men <55 y |
| Target organ damage/Clinical cardiovascular disease |
| Heart diseases Left ventricular hypertrophy Angina or prior myocardial infarction Prior coronary revascularization Heart failure Stroke or transient ischemic attack Nephropathy Peripheral arterial disease Retinopathy |
Table 4.
Compelling and possible indications and contraindications for the major classes of antihypertensive drugs (British Hypertension Society – Guidelines for Hypertension Management 1999)
| Class of drug | Indication | Contraindications | ||
|---|---|---|---|---|
| Compelling | Possible | Possible | Compelling | |
| a-blockers | Prostatism | Dyslipidemia | Postural hypotension | Urinary incontinence |
| ACE inhibitors | Heart failure Left ventricular dysfunction Type I diabetic nephropathy | Chronic renal disease* Type II diabetic nephropathy | Renal impairment* Peripheral vascular disease† | Pregnancy Renovascular disease |
| Angiotensin II receptor antagonists | Cough induced by ACE inhibitor‡ | Heart failure Intolerance of other antihypertensive drugs | Peripheral vascular disease† | Pregnancy Renovascular disease |
| ß-blockers | Myocardial infarction Angina | Heart failure§ | Heart failure§ Dyslipidemia Peripheral vascular disease | Asthma or chronic obstructive pulmonary disease Heart block |
| Calcium antagonists (dihydropyridine) | Isolated systolic hypertension in elderly patients | Angina Elderly patients | - | - |
| Calcium antagonists (rate limiting) | Angina | Myocardial infraction | Combination with ß blockade | Heart block Heart failure |
| Thiazides | Elderly patients | - | Dyslipidemia | Gout |
*Angiotensin converting enzyme (ACE) inhibitors may be beneficial in chronic renal failure but should be used with caution. Close supervision and specialist advice are needed when there is established and significant renal impairment.
†Caution with ACE inhibitors and angiotensin II receptor antagonists in peripheral vascular disease because of association with renovascular disease.
‡If ACE inhibitor indicated.
§â-blockers may worsen heart failure, but in specialist hands may be used to treat heart failure.
Table 5.
Patients presenting with chest pain suggestive of ischemia: short-term risk of death. Based on clinical features and presenting electrocardiogram
| HIGH RISK of death or nonfatal AMI. At least one of the following | INTERMEDIATE RISK of death or nonfatal AMI. No high-risk features plus one of the following | LOW RISK of death or nonfatal AMI. No high or intermediate features plus one of the following: |
|---|---|---|
|
|
|
(Modified from AHCPR. Clinical Practice Guideline - Unstable Angina.)
Table 6.
Assessment and treatments of acute coronary syndrome
| Initial assessment | Specific treatments |
|---|---|
|
Reperfusion therapy: goals
Conjunctive therapy (combined with thrombolytic agents)
Adjunctive therapies
|
| Initial general treatment (memory aid: MONA) | |
|
SBP indicates systolic blood pressure.
Recommended literature:
- 1.The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI). Arch Intern Med 1997;157:2413-2446. Copyright 1997, American Medical Association. [DOI] [PubMed] [Google Scholar]
- 2.1999 World Health Organization - International Society of Hypertension.
- 3.Guidelines for the Management of Hypertension. J Hypertens 1999;17:151-183. [PubMed] [Google Scholar]
- 4.Blood Pressure 1999; 8 (Suppl 1):1-35 [Google Scholar]
- 5.Turek S, Rudan I, Smolej-Narancic N, Szirovicza L, Cubrilo-Turek M, Žerjavic-Hrabak V, Rak-Kaic A, Vrhovski-Hebrang D, Prebeg Ž, Ljubicic M, Jancijevic B, Rudan P. A large cross-sectional study of health attitudes, knowledge, behaviour and risks in the postwar Croatian population. The First Croatian Health Project. Coll Antropol 2001; 25:77-96. [PubMed] [Google Scholar]
- 6.http://bmj.com/cgi/content/full/319/7210/630/T2
- 7.The Joint British Societies’ Cardiac Risk Assessor computer programme and copies of the Joint British Societies’ coronary heart disease risk assessment chart can be downloaded from the British Hypertension Society website (www.hyp.ac.uk/bhs).
- 8.Oparil S. Arterial hypertension. In: Cecil Textbook of Medicine 21st ed. Goldman L, Bennett JC. Philadelphia: W.B. Saunders Co., 2000; 258-273. [Google Scholar]


