Abstract.
Protobothrops mucrosquamatus (Trimeresurus mucrosquamatus) is a medically important species of pit viper with a wide geographic distribution in Southeast Asia. Bites by P. mucrosquamatus mostly involve the extremities. Little is known about the toxic effects of P. mucrosquamatus envenoming to the head because of the infrequency of such occurrence. To better delineate the clinical manifestations of envenoming to the head, we report three patients who suffered from P. mucrosquamatus bites to the head and were treated successfully. All three patients developed progressive soft tissue swelling extending from head to neck, with two patients expanding further onto the anterior chest wall. Mild thrombocytopenia was noted in two patients. One patient had transient acute renal impairment and airway obstruction, necessitating emergent intubation. All three patients received high doses of species-specific antivenom with recovery within 1 week. No adverse reactions to antivenom were observed.
INTRODUCTION
The genus Protobothrops of venomous pit vipers (crotalines) contains 14 terrestrial species in Asia.1 Protobothrops mucrosquamatus (Trimeresurus mucrosquamatus) has a wide geographic distribution including India, Bangladesh, Myanmar, Laos, Vietnam, Thailand, southern China, Taiwan, and Okinawa.1–3 Protobothrops mucrosquamatus poses a serious medical threat to humans because of their overlapping habitats with areas of human activities, frequenting human dwellings in pursuit of prey, and inflicting severe envenomation.4,5 The World Health Organization lists P. mucrosquamatus among the venomous snakes of highest medical importance in Asia.6
Recent studies revealed that most of the P. mucrosquamatus bites occurred to the extremities.4,5 Protobothrops mucrosquamatus envenoming can cause local effects such as pain, edema, hemorrhage, necrosis, and rare compartment syndrome (N = 9) that were confirmed with objective tissue compartment pressure measurements > 30 mm of Hg.5 Reported systemic effects included thrombocytopenia, coagulopathy, rhabdomyolysis, and acute renal injuries.5 Death and possibly recurrence phenomena have been reported.7,8 No previous report of P. mucrosquamatus bites involving the head has been published. Herein, we report three patients with P. mucrosquamatus envenoming to the head.
The study hospital is a tertiary facility in northern Taiwan. The patients were identified in the emergency department (ED) and followed through their hospital courses. Identification of the snake species was presumed by the patient, either on site immediately following the bite or later via species-specific snake pictures. The laboratory workup included complete blood count (platelet < 150,000/mm3 for thrombocytopenia), prothrombin time (international normalized ratio [INR] > 1.25 for coagulopathy), creatine kinase (CK > 1,000 U/L for rhabdomyolysis), and creatinine (> 1.4 but ≤ 3.0 mg/dL for renal impairment). In Taiwan, the F(ab’)2 Bivalent Antivenom Pit Viper, Taiwan Centers for Disease Control, for P. mucrosquamatus and Viridovipera stejnegeri (hemorrhagic bivalent [HB]) has been marketed since 1980.5
PATIENT 1
A 65-year-old male with history of hypertension was bitten to the head by P. mucrosquamatus when he opened the bathroom door the snake was resting on. The patient arrived at a local hospital 0.5 hour post-bite. Physical examination (PE) showed two fang marks at the left posterior scalp with pain and swelling over the left scalp and face. He received two vials of HB intravenously 1.5 hours post-bite. Because of the progressive facial swelling, he was transferred to the study hospital.
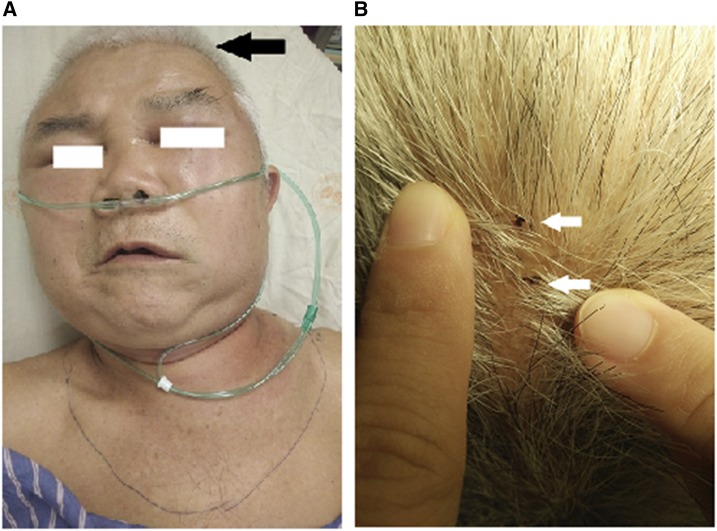
Physical examination in our ED revealed fang marks and marked edema over the scalp, face, neck, and anterior chest wall without bruising or blistering (Figure 1). Laboratory tests showed white blood cell (WBC) 13,000/mm3, platelet 145,000/mm3, and INR 1.19. Two vials of HB were administered separately at 9.5 and 11.5 hours post-bite for the worsening edema.
Figure 1.
(A) The fang marks were at the left parietal–occipital region (black arrow). The picture, taken about 9 hours post-bite and 7 hours after the initial two vials of antivenom, showed marked edema over the scalp, face, neck, and anterior chest wall. (B) The two fang marks were at the left parietal–occipital region (white arrows). The photographs were authorized by the patient. This figure appears in color at www.ajtmh.org.
On the second hospital day, the laboratory tests showed acute renal impairment (creatinine 2.02 mg/dL), INR 1.22, and platelet 132,000/mm3. The patient developed dysarthria and globus sensation 12.5 hours post-bite, but he denied having shortness of breath. Breathing sounds were normal. Epinephrine inhalation and hydrocortisone injection were given with no improvement of symptoms. Two more vials of HB were infused 13.5 hours post-bite in attempt to alleviate the dysarthria and globus sensation.
He complained of asphyxia and became unconscious 17.5 hours post-bite. His peripheral O2 saturation dropped from 95% to 60%. With bag-valve-mask ventilation on 100% oxygen, his O2 saturation increased to 99%. Orotracheal intubation was performed. Two more vials of HB were added 18.5 hours post-bite for the upper airway obstruction. He was transferred to the intensive care unit. CT scan of head and neck with contrast enhancement was performed and showed diffuse soft tissue swelling over oropharynx, scalp, neck, and superior and anterior thoracic regions (Figure 2).
Figure 2.
The computer tomography scan showed diffuse swelling of soft tissue over oropharynx (black arrow), scalp, face, neck, and superior and anterior thoracic regions (white arrows). The photograph was authorized by the patient.
The patient’s swelling decreased gradually and he was extubated on the third hospital day. The head and neck swelling completely resolved on the fifth hospital day. The total amount of HB administered was 10 vials.
PATIENT 2
A 50-year-old healthy male was bitten by P. mucrosquamatus to the head near his domicile. He presented to our ED 1 hour post-bite. Physical examination disclosed two fang marks over the frontal scalp with tenderness, edema, bruising, blistering, and facial swelling. Laboratory tests showed WBC 12,100/mm3, platelet 149,000/mm3, and CK 462 U/L. He received two vials of HB intravenously 2 hours post-bite. Additional six vials were administered in increments of two vials because of the progressive soft tissue swelling on the neck and anterior chest wall over the following 10 hours. With edema and blisters over his head, neck, and anterior chest wall, the patient denied having shortness of breath with normal breathing sounds. The patient’s head and neck swelling completely resolved on the sixth hospital day. The total amount of HB administered was eight vials.
PATIENT 3
A 58-year-old male with history of asthma was bitten to the head by a snake present in a plantain tree. He presented to a local hospital 1 hour post-bite. Physical examination revealed two fang marks at the left posterior scalp with local tenderness only. He received one vial of HB 2 hours post-bite. Because of subsequent left facial swelling, the patient was transferred to the study hospital.
The PE in our ED showed left facial edema extending to the left upper neck without bruising or blistering 18.5 hours post-bite. The patient denied having difficulty breathing with normal respiration. Laboratory tests showed WBC 12,100/mm3 and CK 237 U/L. The snake was identified by the patient to be P. mucrosquamatus using species-specific snake pictures. Two more vials of HB were administered at 19 hours post-bite and two additional vials at 21 hours post-bite because of the continuously progressive edema. The head and neck swelling decreased on the second hospital day and resolved on the fifth day. The total amount of HB administered was five vials.
DISCUSSION
Crotaline snakebites may occur to the head and neck. In the Americas, less than 2% of the Crotalus and Bothrops species bites involve the head.9,10 Crotaline snakebites to the head, in addition to causing local signs such as swelling, bruising, and blistering, are capable of inflicting significant morbidities such as ocular injuries, airway compromise, and mortality.10
In this case series, envenoming by P. mucrosquamatus to the head resulted in local pain and progressive soft tissue swelling. Patient 2 exhibited more severe and extensive soft tissue injuries such as bruising of the scalp and blister formation. All three patients did not have soft tissue necrosis or later scar formation. Regarding systemic effects, mild thrombocytopenia was observed in Patient 1 and 2, and acute renal impairment was observed transiently in Patient 1. No coagulopathy or rhabdomyolysis was detected.
The venom of P. mucrosquamatus is a complex mixture containing snake venom metalloproteinases (SVMPs), phospholipases A2 (PLA2s), serine proteases, and vasoactive peptides.11 The clinical complications following P. mucrosquamatus envenoming are most likely caused by the integrated actions of hemorrhagic SVMPs, myotoxic PLA2s, and vasoactive peptides. The severity of complications in individual setting depends on the interplay among multiple factors such as the amount and location of the venom injected as well as the timing and doses of antivenom administered.
Patient 1 developed respiratory distress resulting from airway obstruction in spite of prompt antivenom treatment. The pathophysiologic change underlying the airway obstruction was the diffuse soft tissue edema over the pharynx and larynx. Possible mechanisms have been suggested for the upper airway edema from Crotalus snakebites: direct extension of local envenoming, direct topical effects of venom, and anaphylaxis.12 In Patient 1, a larger dose of injected venom and direct extension of local envenoming via rich vascularity and lymphatic network in the head and neck are most likely the causes for patient’s obstructive airway edema, given the lack of direct topical effects or anaphylaxis signs such as generalized hives or lip–tongue swelling.
Crotaline envenoming to the cheek, tongue, and mouth has been reported to cause airway compromise,9,10 suggesting that the unusual bite sites in close proximity to the airway may increase the risk of airway obstruction and thus substantiate the necessity of endotracheal intubation. In crotaline snakebites to the scalp, the decision to intubate varies, depending on the clinical signs of impending respiratory distress. In Patient 1, airway compromise occurred 12.5 hours post-bite. Emergent intubation was performed because of hypoxia and imminent respiratory failure. In Patient 2 and Patient 3, swelling of local soft tissues progressed from head to neck and anterior chest wall without respiratory distress.
Species-specific antivenom is the mainstay therapy for snake envenoming. For treatment of P. mucrosquamatus envenoming, the Taiwan Poison Control Center recommends one to four vials of HB.13 In our case series, the total amount of HB administered, as based on clinical assessment, was higher than that of the recommendation. No adverse reactions to the higher doses of antivenom were observed. Therefore, higher doses of antivenom with a loading dose of up to four vials can be considered to alleviate the rapid progression of soft tissue swelling, especially in cases of envenoming to the head, to prevent possible respiratory compromise.
In conclusion, our case series is the first report that describes the clinical manifestations of P. mucrosquamatus envenoming to the head, which ranged from extensive soft tissue edema and transient acute renal impairment to life-threatening airway obstruction. High vigilance and prompt administration of high-dose antivenom are recommended with symptom progression. Early airway protection should be initiated for clinical manifestations suggesting respiratory distress.
Acknowledgment:
The authors thank Susan S. Sheu, MD for her review and editing of the manuscript.
REFERENCES
- 1.Guo P, Liu Q, Wen T, Xiao R, Fang M, Zhong G, Truong NQ, Zhu F, Jadin RC, Li C, 2016. Multilocus phylogeny of the Asian lance-headed pitvipers (Squamata, Viperidae, Protobothrops). Zootaxa 4093: 382–390. [DOI] [PubMed] [Google Scholar]
- 2.Terada K, 2011. The distribution, population density and controls of Protobothrops mucrosquamatus, Protobothrops elegans, Elaphe taeniura friesei, 3 snake species established on Okinawa Island. Bull Herpetol Soc Jpn 2: 161–168. [Google Scholar]
- 3.Vasaruchapong T, Laoungbua P, Tangrattanapibul K, Tawan T, Chanhome L, 2017. Protobothrops mucrosquamatus (Cantor, 1839), a highly venomous species added to the snake fauna of Thailand (Squamata: Viperidae). Trop Nat Hist 17: 111–115. [Google Scholar]
- 4.Hung DZ, 2004. Taiwan’s venomous snakebite: epidemiological, evolution and geographic differences. Trans R Soc Trop Med Hyg 98: 96–101. [DOI] [PubMed] [Google Scholar]
- 5.Chen YW, Chen MH, Chen YC, Hung DZ, Chen CK, Yen DH, Huang CI, Lee CH, Wang LM, Yang CC, 2009. Differences in clinical profiles of patients with Protobothrops mucrosquamatus and Viridovipera stejnegeri envenoming in Taiwan. Am J Trop Med Hyg 80: 28–32. [PubMed] [Google Scholar]
- 6.Warrell D, 2010. WHO Guidelines for the Production, Control and Regulation of Snake Antivenom Immunoglobulins. Geneva, Switzerland: WHO Press. [DOI] [PubMed]
- 7.Liao WB, Lee CW, Tsai YS, Liu BM, Chung KJ, 2000. Influential factors affecting prognosis of snakebite patients management: Kaohsiung Chang Gung Memorial Hospital experience. Chang Gung Med J 23: 577–583. [PubMed] [Google Scholar]
- 8.Luo GP, Yue DY, Xu ZQ, 2012. Clinical analysis of delayed hemorrhage following Trimeresurus mucrosquamatus bite. J Snake 24: 254–257. [Google Scholar]
- 9.Gerkin R, Sergent KC, Curry SC, Vance M, Nielsen DR, Kazan A, 1987. Life-threatening airway obstruction from rattlesnake bite to the tongue. Ann Emerg Med 16: 813–816. [DOI] [PubMed] [Google Scholar]
- 10.Bucaretchi F, Hyslop S, Mello SM, Vieira RJ, 2007. Bothrops snakebite on the head: case report and review of the literature. Ann Trop Med Parasitol 101: 733–743. [DOI] [PubMed] [Google Scholar]
- 11.Villalta M, et al. 2012. Snake venomics and antivenomics of Protobothrops mucrosquamatus and Viridovipera stejnegeri from Taiwan: keys to understand the variable immune response in horses. J Proteomics 75: 5628–5645. [DOI] [PubMed] [Google Scholar]
- 12.Hinze JD, Barker JA, Jones TR, Winn RE, 2001. Life-threatening upper airway edema caused by a distal rattlesnake bite. Ann Emerg Med 38: 79–82. [DOI] [PubMed] [Google Scholar]
- 13.Chen YC, Chen MH, Wang LM, Wu JJ, Huang CI, Lee CH, Yen DH, Yang CC, 2007. Antivenom therapy for crotaline snakebites: has the poison control center provided effective guidelines? J Formos Med Assoc 106: 1057–1062. [DOI] [PubMed] [Google Scholar]