Abstract
Despite years' research, the radiographic criteria for osteoporotic vertebral fracture and its grading remain debated. The importance of identifying vertebral endplate/cortex fracture (ECF) is being recognised; however, evaluation of osteoporotic ECF requires training and experience. This article aims to serve as a teaching material for radiologists/physicians or researchers to evaluate osteoporotic ECF. Emphasis is particularly dedicated to identifying ECF that may not be associated with apparent vertebral body collapse. We suggest a combined approach based on standardised radiologic evaluation by experts and morphometry measurement is the most appropriate approach to detect and classify osteoporotic vertebral fractures.
The translational potential
A good understanding of radiologic anatomy of vertebrae and fracture signs of endplate/cortex are essential for spine fragility fracture assessment.
Keywords: Endplate, Normal variants, Osteoporosis, Osteoporotic fractures, Radiograph
Introduction
Osteoporosis is characterised by low bone mass and microarchitectural deterioration, which leads to bone fragility and consequent increase in fracture risk. Often bone loss becomes apparent only after a typical osteoporotic fracture has occurred. Vertebral fractures (VFs) are the most common osteoporotic fracture. A VF, after minor trauma, is a hallmark of osteoporosis. Thirty to fifty percent of women and 20–30% of men experience a VF at some points in their life (2). Prevalent VFs increase the risk of future vertebral and nonvertebral osteoporotic fracture independent of bone mineral density [1]. VFs may be associated with poor life quality, impaired bending and rising, difficulties in the activities of daily living, frailty, higher risk of institutionalisation and higher mortality (irrespective of those related to fractures) [2], [3], [4], [5], [6], [7]. Appropriate management of osteoporosis can reduce future fracture risk, and therefore, it is important to identify and report VFs accurately and clearly, so that appropriate investigation and treatment can be instigated [8].
Despite years' research, the radiographic criteria for osteoporotic VF and its grading remain hotly debated [8], [9], [10], [11], [12], [13], [14], [15], [16], [17]. The semiquantitative (SQ) criteria proposed by Genant et al. are commonly used for identifying VF [18]. According to this criteria, a “normal” vertebra, i.e., vertebra that does not meet the following defined vertebral deformity (VD), is defined as Grade 0; 20–25% reduction in anterior, middle and/or posterior vertebral height and 10–20% reduction in area is defined as Grade 1 VD; a 26–40% reduction in any height and 20–40% in area is defined as Grade 2 VD and a >40% reduction in any height and area is regarded as Grade 3 VD. On spine radiograph, Genant et al.'s SQ approach is commonly applied to vertebrae T4 to L4. Visualising T1–T3 is often hampered due to overlying of the shoulders, and visualising L5 can be hampered by the overlying pelvis. Osteoporotic VF above T4 is also rare. L5 is also usually not affected by osteoporotic fractures. Genant et al. described the importance of loss of endplate integrity as a characteristic of fractures but did not make diagnosis contingent on this observation [19].
However, there are some practical difficulties in applying Genant et al.'s SQ approach. An experienced reader may estimate the severity of fracture according to the apparent vertebral height reduction, but without the aid of measurement, the reduction in vertebral height cannot be determined with high accuracy and consistency [16], [20], [21]. Quantitative measurement is often necessary to ensure necessary accuracy and consistency [16], [21]. In addition, incident endplate fracture may be evident when the height reduction does not reach the grade semiquantitative vertebral deformity (SQ-VD) threshold of 15% or 20%. On the other hand, it is generally considered that at least some Grade 1 SQ-VDs may not be true fractures. Szulc et al. [22] suggested that a cut-off of 30% for wedge deformities from T6 to T9 (thoracic kyphosis site) and that 25% for deformities at other levels may have a high specificity and a moderate sensitivity for identifying VDs related to low bone mineral density (BMD) in men. A recent analysis shows that for both women and men, vertebrae with >34% height loss are always associated with radiographically identifiable endplate/cortex fracture (ECF), whereas in women, vertebrae with <34% height loss may or may not be associated with ECF [23]. In men, vertebrae with less than 34% height loss tended to be without ECF. Grade 2 VD with height loss >34% may constitute a distinct subcategory and always reflect true VF [23].
The algorithm-based qualitative approach assumes that the endplate is always deformed in VFs and is 100% sensitive in case of VF, whereas vertebral height reduction is not an indispensable finding of VF [24]. According to Jiang et al.'s initial description, osteoporotic endplate collapse occurs primarily at, or close to, the centre of the endplate (this represents the weakest part of the vertebral body as it is not protected by the strong outer vertebral ring), indicated by depression of the line that represents the endplate within the vertebral ring [24]. However, without endplate disruption, fracture can also deform the anterior vertebral cortex that is usually termed by radiologists as buckling, dented, swollen and projecting types of fracture [8], [9], [10], [16]. In the case of chronic VF, the endplate may remodel over time, and its discontinuity or depression may no longer be apparently identifiable [8]. It is also possible that a VF actually occurred without identifiable ECF, which is related to the resolution limitation of the radiograph. The current evidence favours the approaches incorporating ECF identification for VF assessment [8], [9], [13], [14], [15], [16], [25].
We suggest that the points mentioned in the following are the current understanding of osteoporotic VF:
-
1.
Microscopic fractures as shown by histology are common in radiographically normal vertebrae [26], [27], [28].
-
2.
An osteoporotic ECF can occur without apparent SQ-VD [10], [13], [14], [16]. VF and its repair/healing can occur even in the absence of any appreciable radiographic change in vertebral shape [8].
-
2
An osteoporotic VF can occur without radiographically identifiable ECF. The endplate depression is not an indispensable sign of a vertebral fracture [8], [10], [13], [16].
-
3
An osteoporotic VF can actually occur without radiographically identifiable ECF and without SQ-VD [8]. It has often been noted that acute VF can appear normal in a radiograph [29], [30], although such reports might have missed ECF during their studies.
-
4
Clearly identified ECF, regardless of whether there is associated VD, indicates VF [8]. Therefore, a new incident ECF, even without meeting the usual criteria of 15% or 20% further height loss (19), should be regarded as incident fracture.
-
5
Grade 2 SQ-VD with vertebral height loss >34% and Grade 3 SQ-VD always indicate VF [23].
-
6
Some Grade 1 SQ-VD and even a small portion of mild Grade 2 SQ-VD may be physiological or degenerative wedging [23]. A mild (<34% height loss) Grade 2 SQ-VD without ECF may also be an old fracture with remodelled endplate or cortex [8].
Definite identification of ECF may not be possible in all VF cases due to the inherent limitation of projectional radiograph. Although many fractures of moderate and severe grades can be consistently diagnosed, inevitably, there will be findings that are not ambiguous. If clinical decision-making depends on the diagnosis of a fracture, then comparison with previous images, a radionuclide scan, computed tomography scan with sagittal reformation and/or magnetic resonance imaging (MRI) may provide more conclusive evidence.
When interpreting radiographs, a vertebra should be carefully compared with its neighbours. An isolated anterior wedging of vertebral body between vertebrae of normal shape is suggestive of VF. A Grade 1 or Grade 2 SQ-VD even without clear ECF which is distinctly different from its neighbours may be more indicative of higher fracture risk than if wedged or biconcave vertebrae are evident throughout much of the thoracic or lumbar spine [8]. According to our experience, upper endplate is more likely fractured than the lower endplate, which concurs with the published theory that the cranial endplate is thinner and supported by less-dense trabecular bone [31].
Owing to the subjectivity of diagnosing vertebral ECF, for epidemiological studies and clinical trials, we advocate central reading by experienced readers. Interstudy comparison of epidemiological results is only possible when the methodology of the epidemiological studies is similar/the same (for example, table 6 of reference 32). For ambiguous cases in daily clinical care, in addition to necessary additional investigations such as computed tomography/MRI, radiograph follow-up is also a reasonable choice [8], [10], [19], [29], [33].
Although the importance of identifying vertebral ECF is being recognised, evaluation of osteoporotic ECF can be difficult and requires training and experience [12], [34], [35]. This article aims to serve as a teaching material for the radiographic identification of ECF. The radiograph materials in this article were selected from the baseline (year-0) and year-4 follow-up of MrOS (Hong Kong) and MsOS (Hong Kong) studies [16], [32], [36], [37]. This article can be read together with another recent pictorial article on this topic [10]. Most of the time, the golden standard for a VF diagnosis cannot be obtained, and the radiographic diagnosis of mild VF is inherently subjective. The examples given in this document represent the consensus reading of all the authors of this article, and the follow-up and baseline radiographs were available for comparison to assist the diagnosis. Furthermore, during the course of the follow-up to year-14, 784 MRIs were performed on these MrOS (Hong Kong) and MsOS (Hong Kong) study participants. However, we cannot exclude the possibility that there are errors remaining; if this is the case, we hope that, when identified, we can correct them by additional publication in the future.
Atlas of osteoporotic vertebral endplate and cortex fractures
See Figure 1, Figure 2, Figure 3, Figure 4, Figure 5, Figure 6, Figure 7, Figure 8, Figure 9, Figure 10, Figure 11, Figure 12, Figure 13, Figure 14, Figure 15, Figure 16, Figure 17, Figure 18, Figure 19, Figure 20, Figure 21, Figure 22, Figure 23, Figure 24, Figure 25.
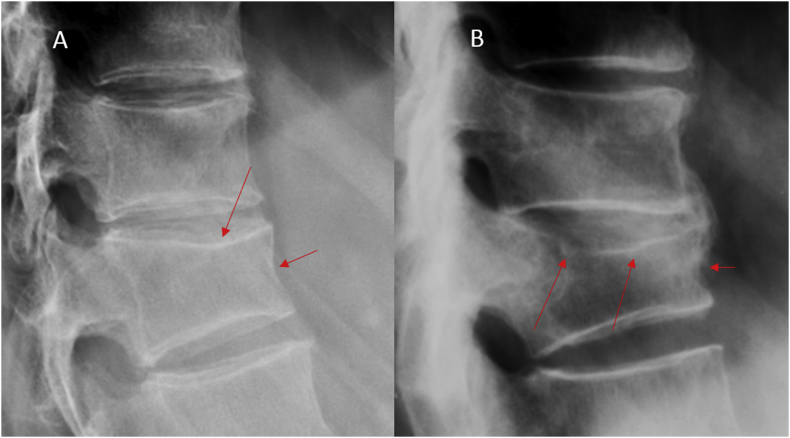
Figure 1.
(A) T12 upper endplate fracture (long arrow) and anterior cortex mild buckling (short arrow), with SQ-VD Grade 2; (B) T12 vertebra Grade 3 SQ-VD (wedge fracture) with buckling of the anterior cortex (short arrow) and upper endplate fracture (long arrow). Note that there is no fracture for T12 lower endplate.
SQ-VD = semiquantitative vertebral deformity.
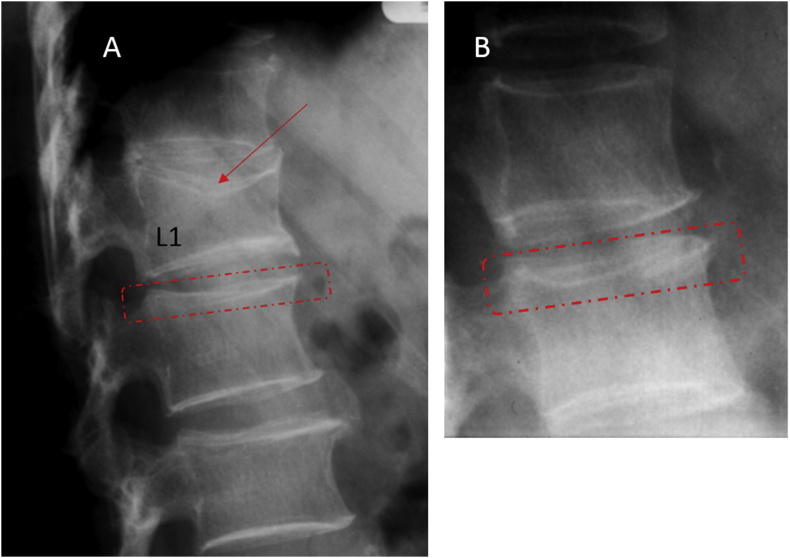
Figure 2.
(A) L1 upper concave endplate fracture (long arrow) and Grade 2 SQ-VD. L2 upper endplate is normal (dotted square) which may be misdiagnosed as endplate fracture. This is due to the projection of endplate ring; note the parallel multilayered endplate lines and that there is no depression; (B) Radiograph from another subject demonstrates a similar appearance of upper endplate (without fracture).
SQ-VD = semiquantitative vertebral deformity.
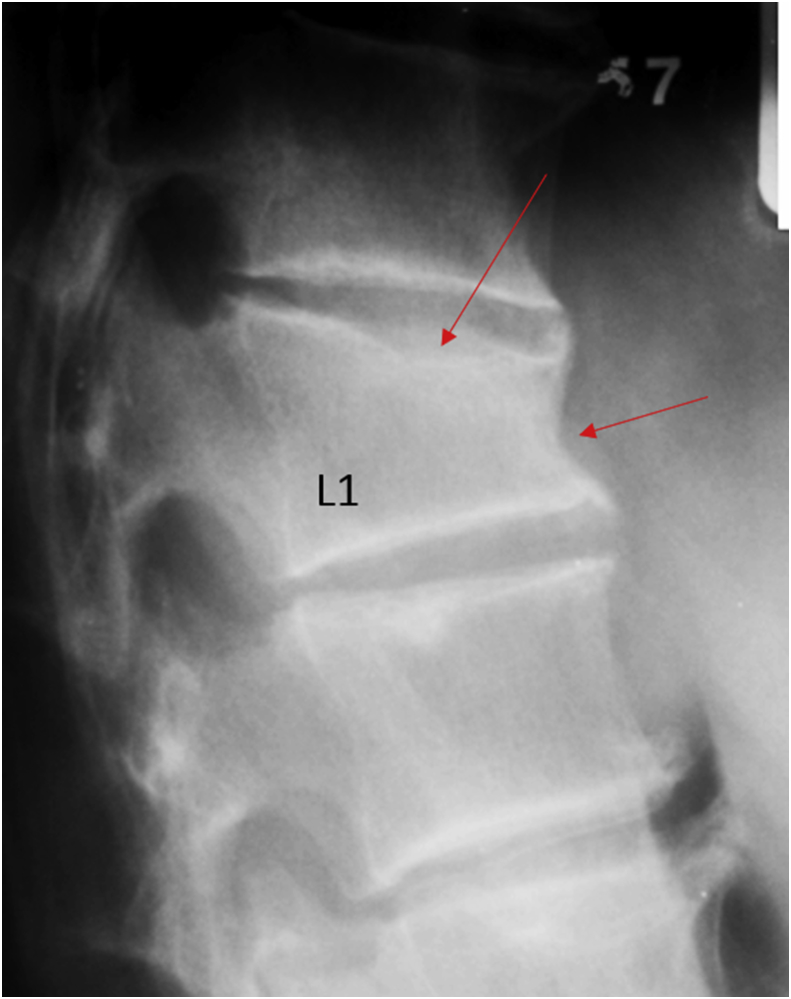
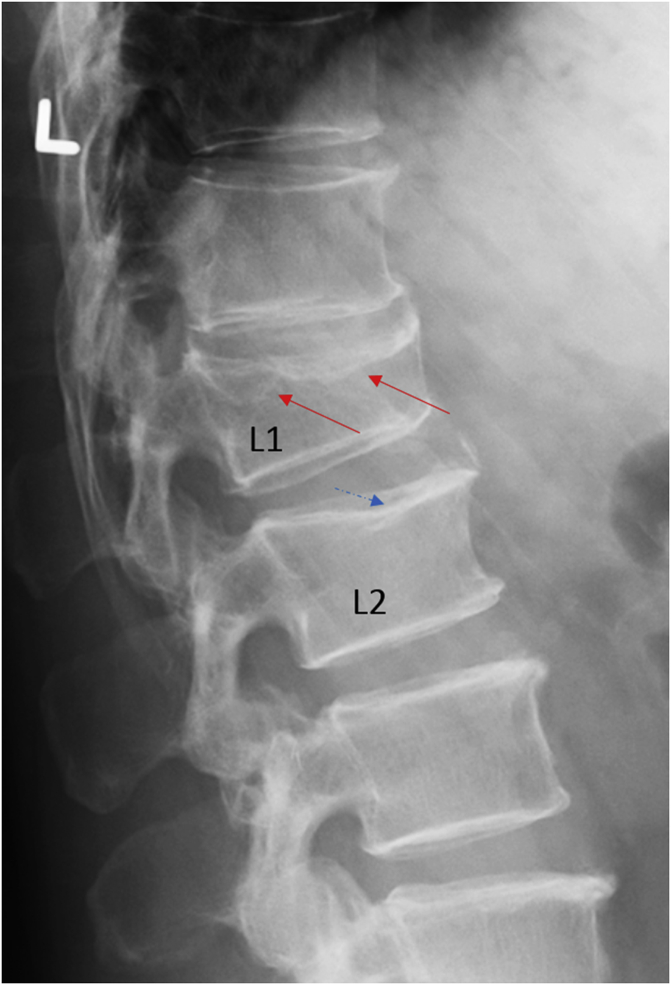
Figure 3.
L1 vertebra Grade 3 SQ-VD and upper endplate fracture (long arrow) and anterior cortex mild buckling (short arrow).
SQ-VD = semiquantitative vertebral deformity.
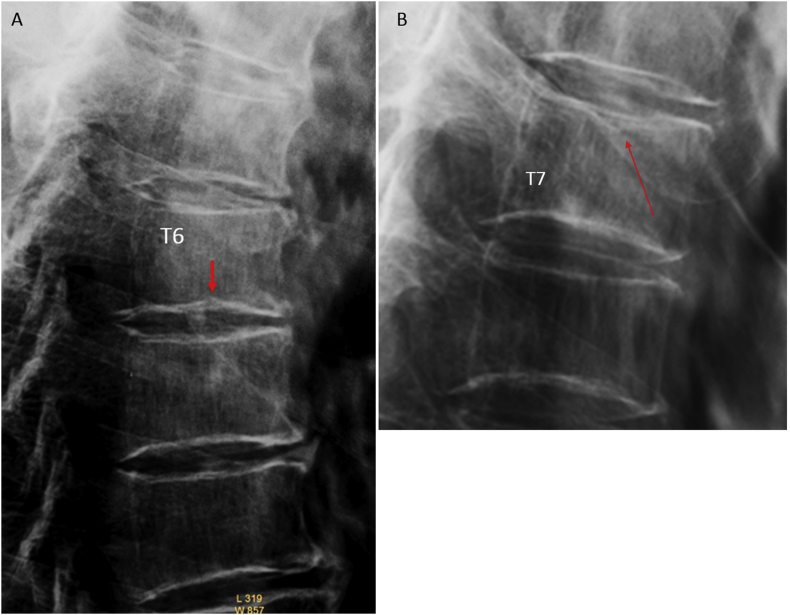
Figure 4.
(A) T6 lower endplate fracture with broken endplate line and slight depression at its centre. There is no SQ-VD; (B) T7 upper endplate fracture and slight depression at its centre. There is no SQ-VD.
SQ-VD = semiquantitative vertebral deformity.
Figure 5.
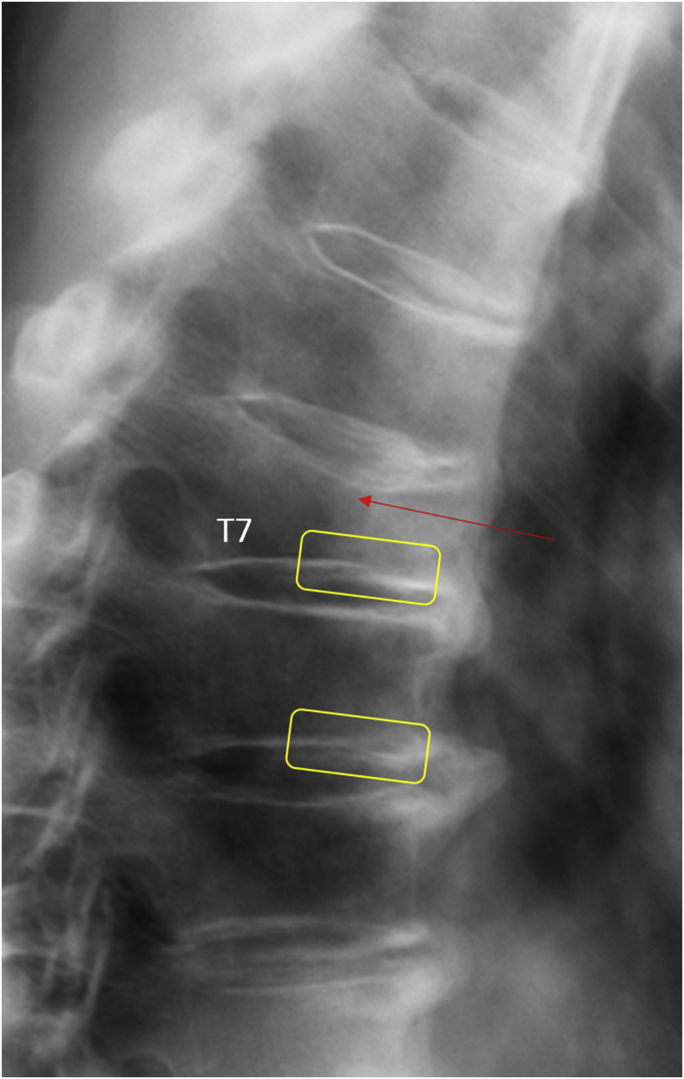
T7 vertebra Grade 2 SQ-VD with upper endplate fracture (long arrow). The T7 lower endplate is without endplate fracture (the same appearance is also seen at T8 lower endplate).
SQ-VD = semiquantitative vertebral deformity.
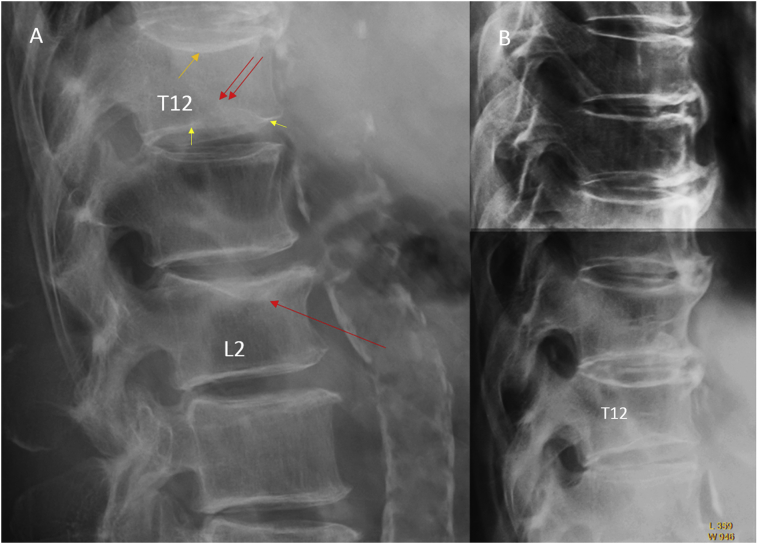
Figure 6.
(A) L2 upper endplate fracture (red long arrow); A depression of T12 lower endplate is seen (double red arrow). The T12 lower endplate depression is symmetrically looking; the depressed endplate is of low density and there are angles (short yellow arrows) between the depressed endplate and nondepressed endplate. Our reading is that it could be a Schmorl's node (preferred diagnosis) or an endplate fracture. T12 upper endplate shows arc-shaped endplates (orange short arrow, commonly called “bean-can” appearance). This can usually be confirmed with comparing the endplates of upper adjacent vertebrae as shown in (B).
Figure 7.
(A) L3 upper endplate fracture with depression (red arrows), and borderline Grade 0 SQ-VD (19% height reduction); (B) magnified image of the involved vertebra.
SQ-VD = semiquantitative vertebral deformity.
Figure 8.
L1 vertebra with Grade 2 SQ-VD. The arrow indicates anterior cortex fracture, and the triangle indicates ambiguous upper endplate fracture.
SQ-VD = semiquantitative vertebral deformity.
Figure 9.
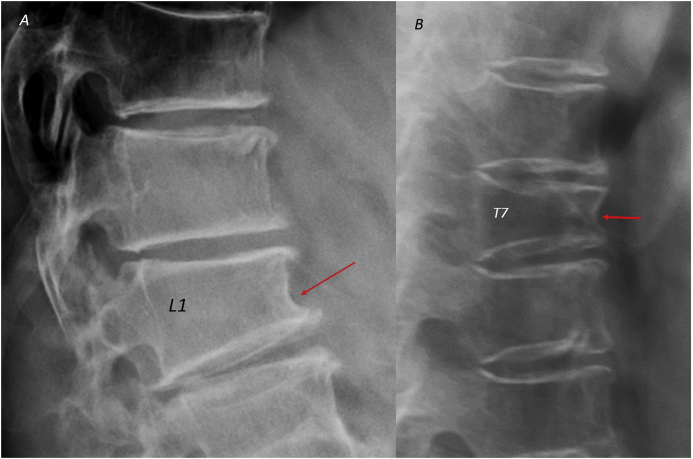
(A) L1 vertebra anterior cortex buckling (arrow) and Grade 2 SQ-VD (anterior height loss approximately 38%). There is no endplate fracture observed for this vertebra; (B) T7 vertebra Grade 2 SQ-VD with upper endplate fracture and anterior cortex buckling (arrow). Note that the layered appearance of T8 upper endplate does not suggest fracture (see Figure 2).
SQ-VD = semiquantitative vertebral deformity.
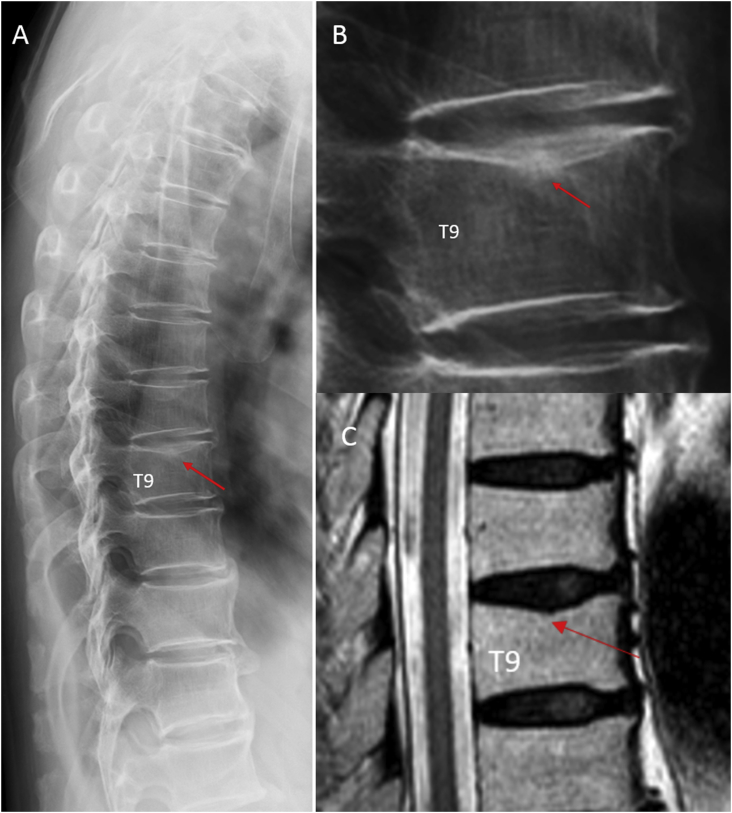
Figure 10.
(A) T9 upper endplate fracture with slight depression at its centre; (B) magnified image of the involved vertebra. (C) A follow-up T2-weighted MR image 10 years later shows upper endplate central depression, with vertebral body homogenous fatty bone marrow signal.
MR = magnetic resonance; SQ-VD = semiquantitative vertebral deformity.
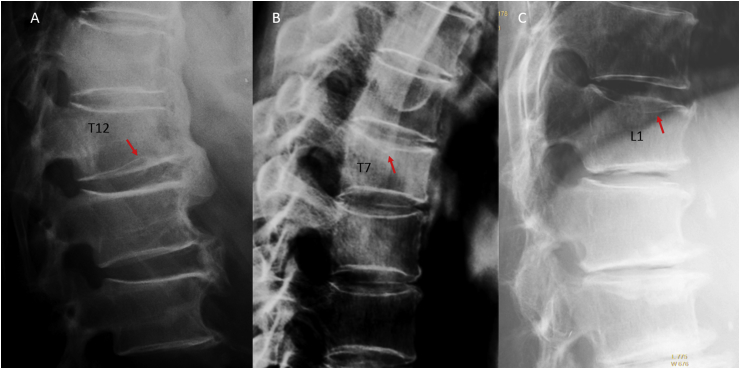
Figure 11.
(A) T12 vertebra Grade 2 SQ-VD and lower endplate fracture; (B) T7 vertebra Grade 1 SQ-VD and upper endplate fracture; (C) L1 vertebra Grade 2 SQ-VD and upper endplate fracture.
SQ-VD = semiquantitative vertebral deformity.
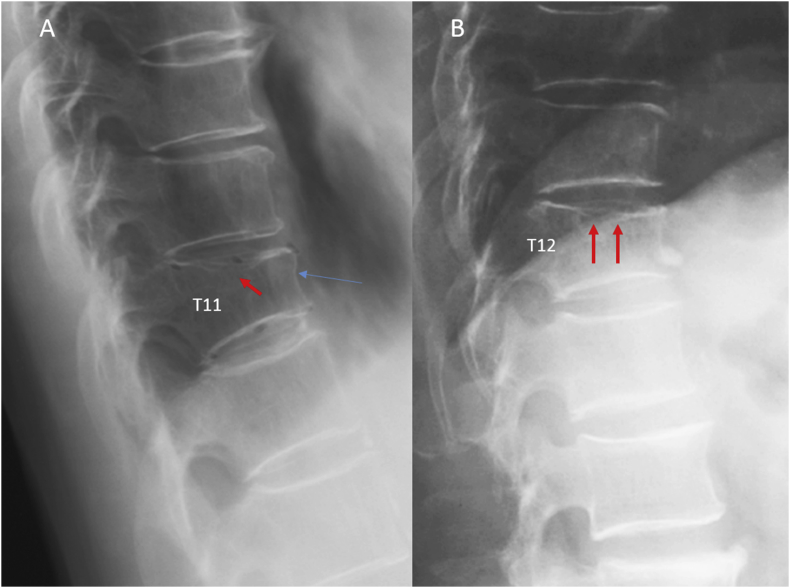
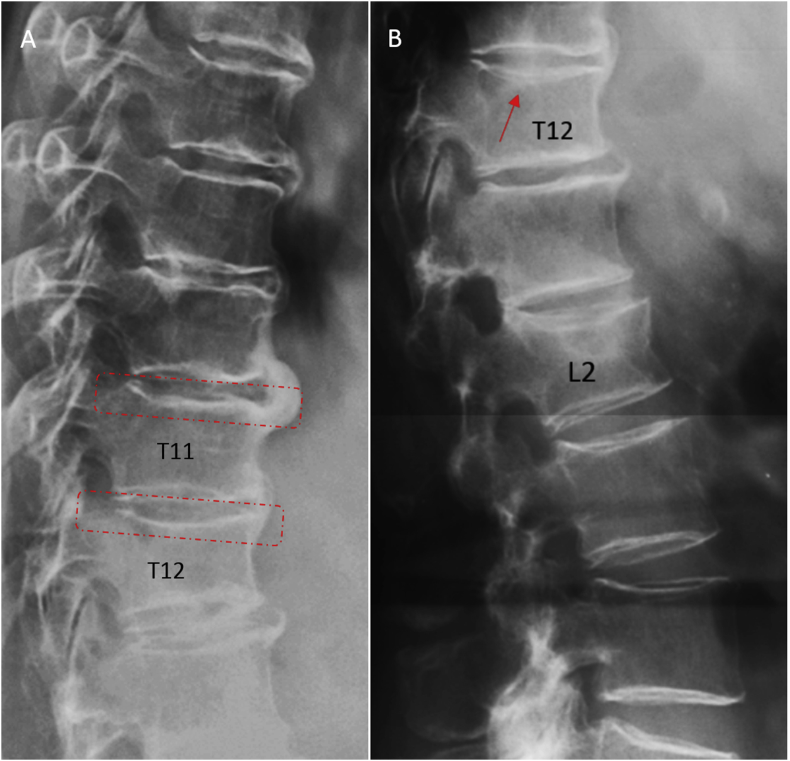
Figure 12.
(A) T11 vertebra Grade 2 SQ-VD with upper endplate depression (red arrow) and mild buckling of the anterior cortex (blue arrow, note that the vertebral borders have been marked with pen); (B) T12 vertebra Grade 2 SQ-VD and upper endplate fracture with depression and broken endplate line (double red arrows).
SQ-VD = semiquantitative vertebral deformity.
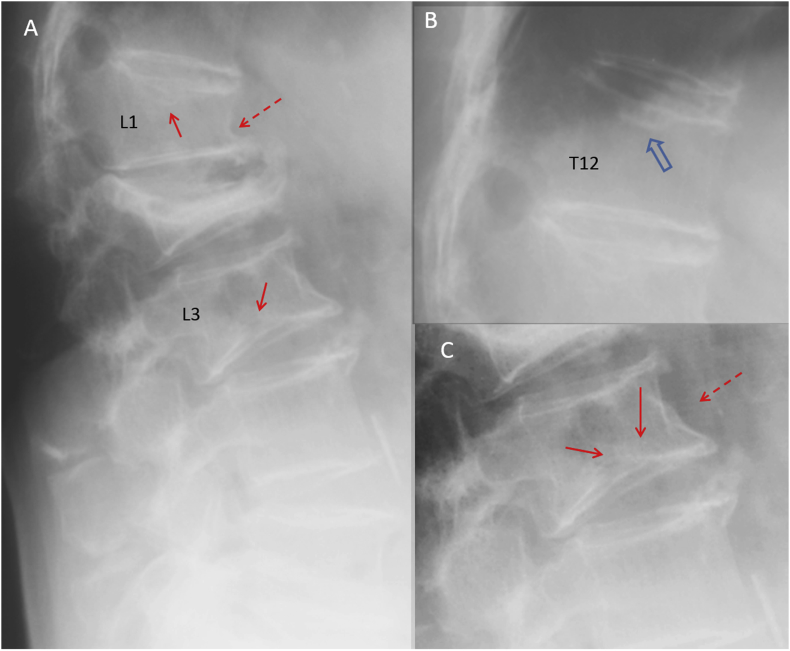
Figure 13.
Radiographs in (A), (B) and (C) are from the same patient. (A) L1 shows upper endplate fracture (red arrow) and anterior cortex buckling (red dotted arrow). L2 vertebra is collapsed (Grade 3 SQ-VD); (B) T12 Schmorl's node (blue arrow); (C) zoomed-in image of L3. There is lower endplate fracture (red arrows); however, L3 anterior cortex should not be read as buckling (red dotted arrow).
SQ-VD = semiquantitative vertebral deformity.
Figure 14.
L1 vertebra Grade 3 SQ-VD and upper endplate wavy fracture. L2 upper endplate ambiguous fracture (differential diagnosis of Schmorl's node cannot be excluded, or endplate fracture and Schmorl's node may coexist).
SQ-VD = semiquantitative vertebral deformity.
Figure 15.
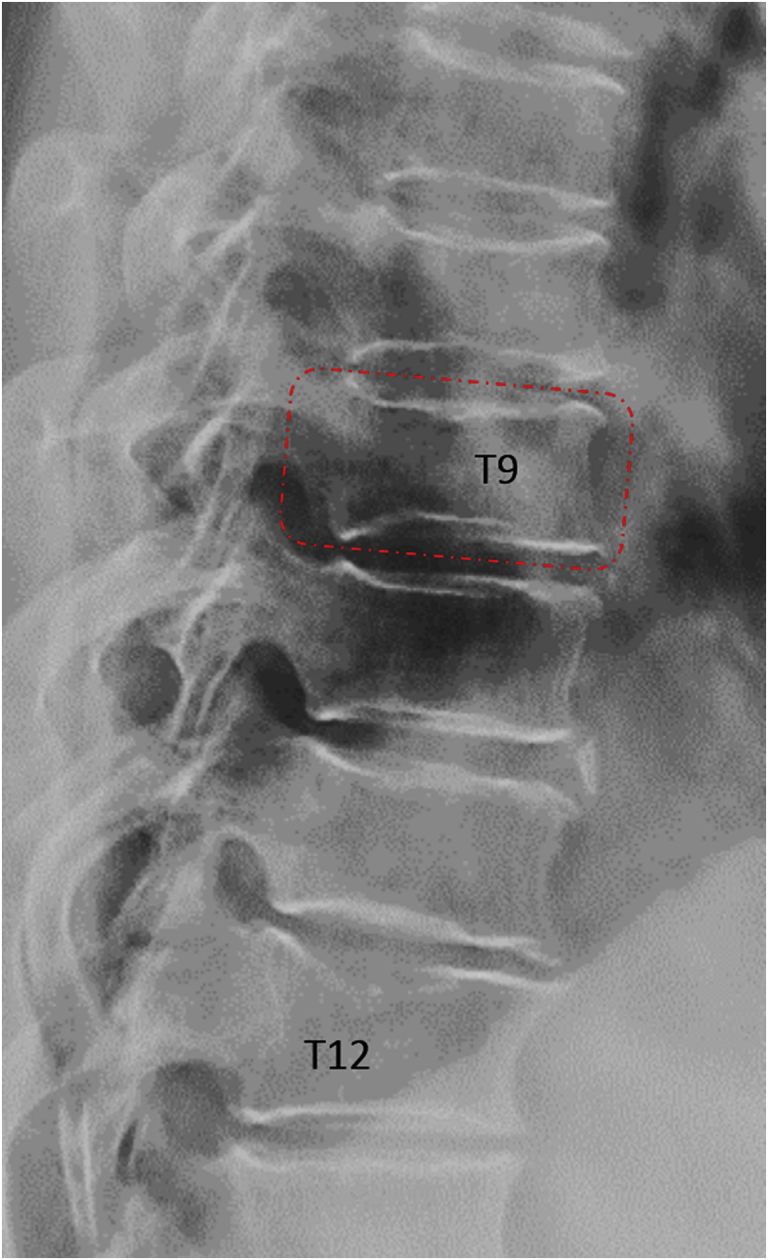
T12 vertebra wedge deformity (Grade 2 SQ-VD) and upper endplate fracture. Note that both upper and lower endplates of T9 vertebra are without fracture (dotted square).
SQ-VD = semiquantitative vertebral deformity.
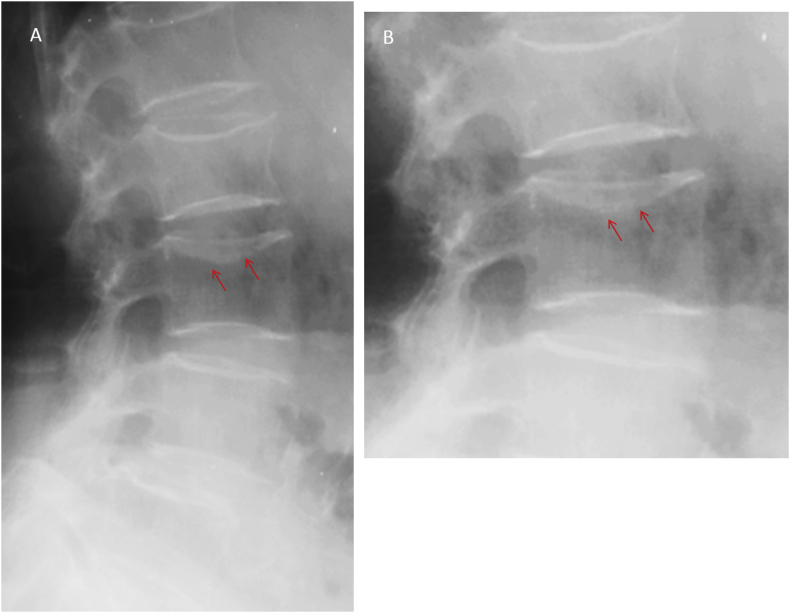
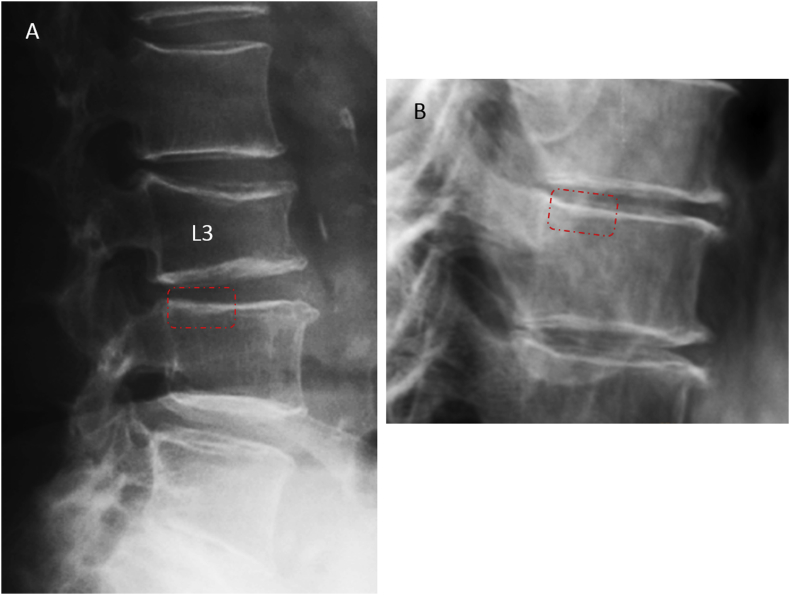
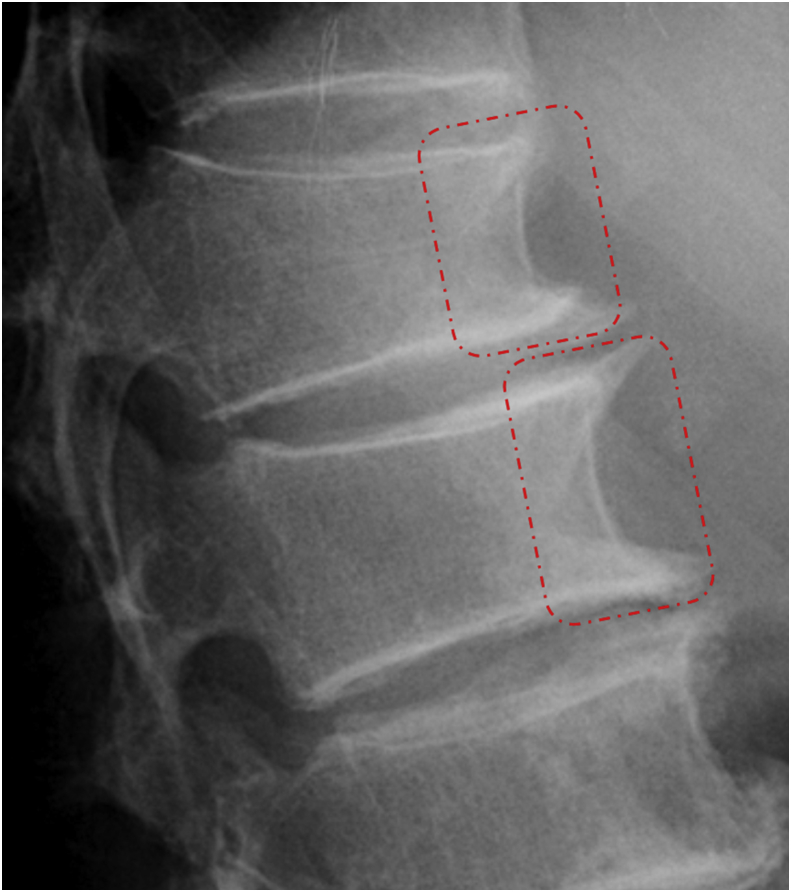
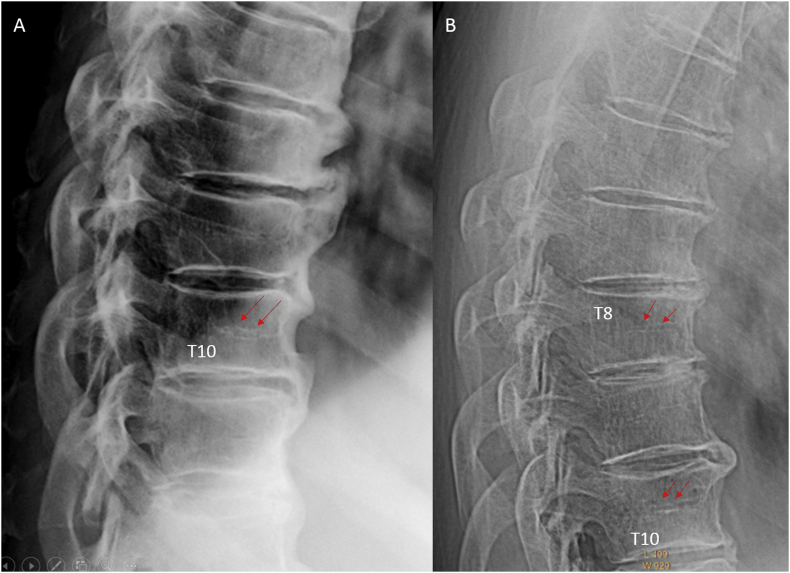
Figure 16.
(A) L3 upper and lower endplates fracture and SQ-VD grade 2. Radiographs (A) and (B) are from two subjects. The upper endplates in (A) and (B) marked by the red dotted rectangles are without fracture (a potential pitfall).
SQ-VD = semiquantitative vertebral deformity.
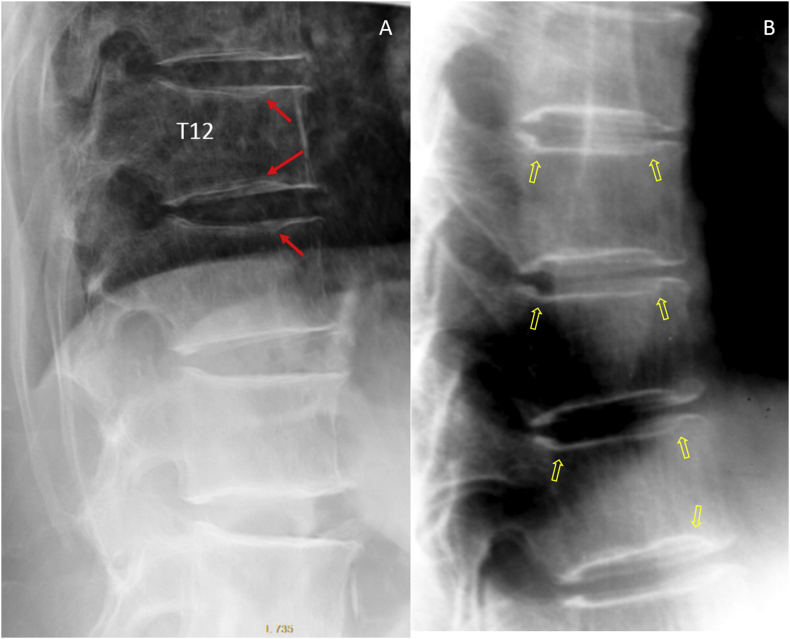
Figure 17.
(A) Red arrows indicate parts of endplate without fracture (potential pitfalls); (B) more typical type of these appearances (yellow arrows).
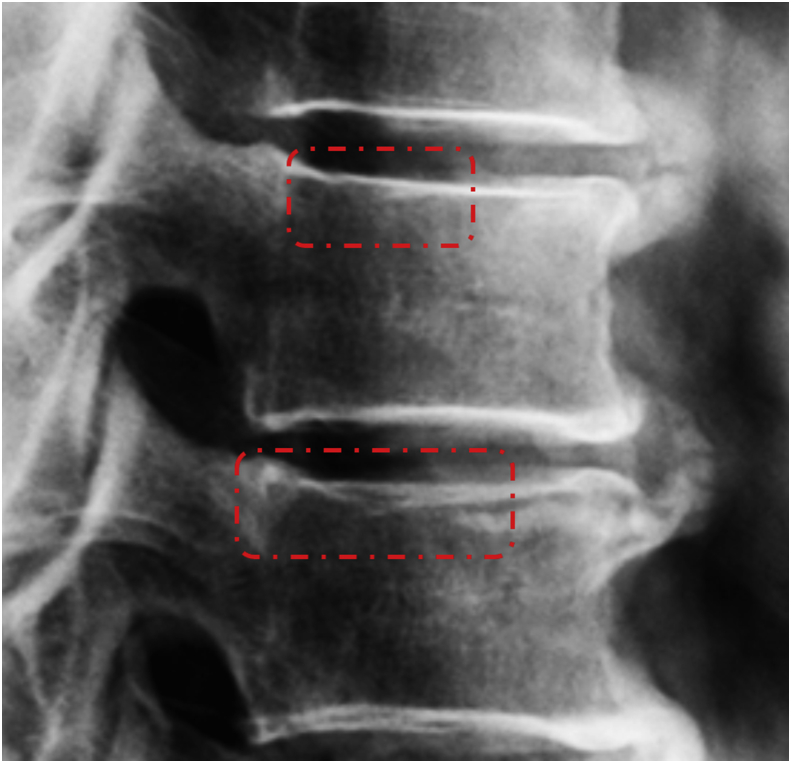
Figure 18.
Dotted squares indicate normal appearance of upper endplate which may be misread as a fracture (potential pitfall).
Figure 19.
Anterior upper part of L1 vertebra shows anterior marginal cartilage node (congenital anomaly, red arrow). L2 upper endplate is without fracture (yellow square); also see Figure 17B.
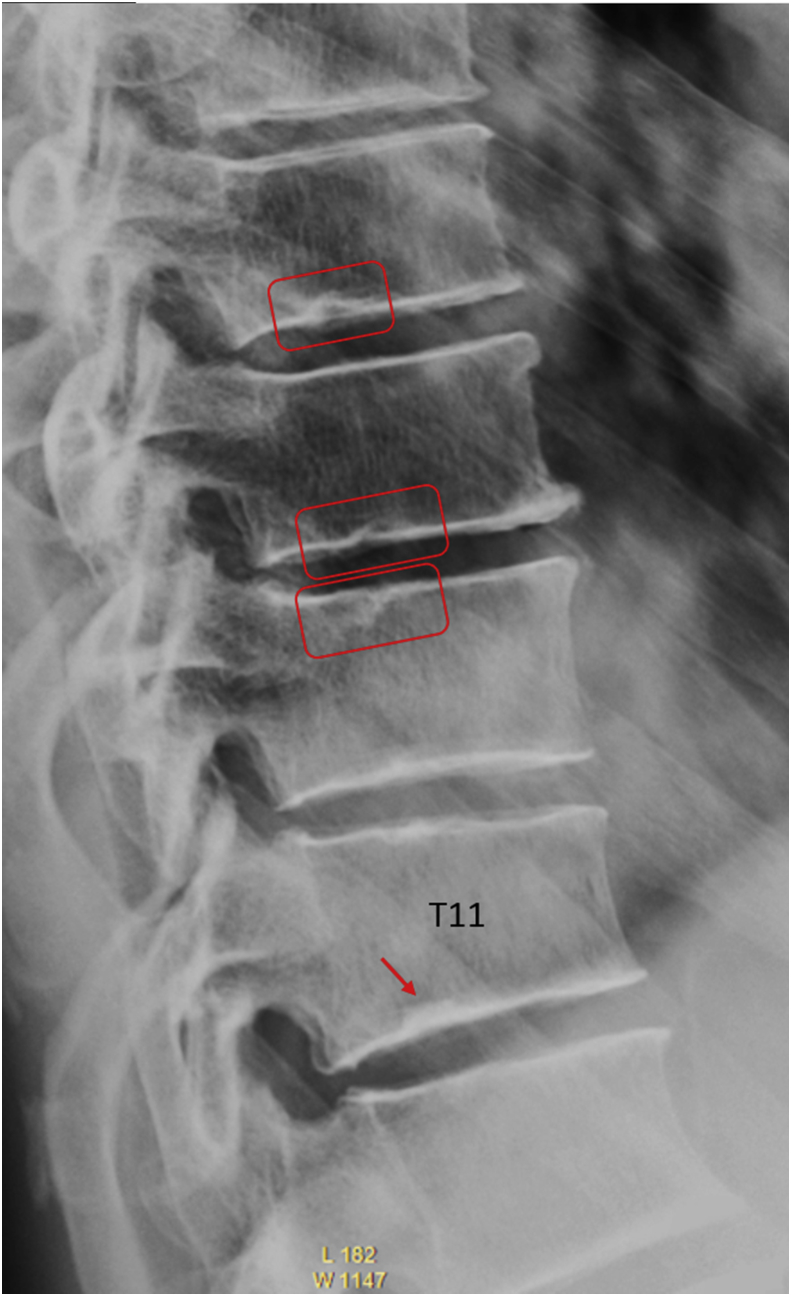
Figure 20.
Vertebral T11 physiological (developmental) wedging and Schmorl's node (red arrow) at the lower endplate. Red rectangles indicate multiple Schmorl's nodes.
Figure 21.
Dotted squares indicate intact anterior cortex (a potential pitfall). T12 (associated with upper dotted square) has Grade 2 SQ-VD with anterior height loss of 33%. Osteophytes are noted.
SQ-VD = semiquantitative vertebral deformity.
Figure 22.
T12 upper endplate shows fracture (lower square in A); this is better shown in B (arrow) and confirmed by comparing the upper endplates of T11 (upper square in A), T12 and L1. L2 Grade 2 SQ-VD upper endplate fracture and anterior cortex buckling.
SQ-VD = semiquantitative vertebral deformity.
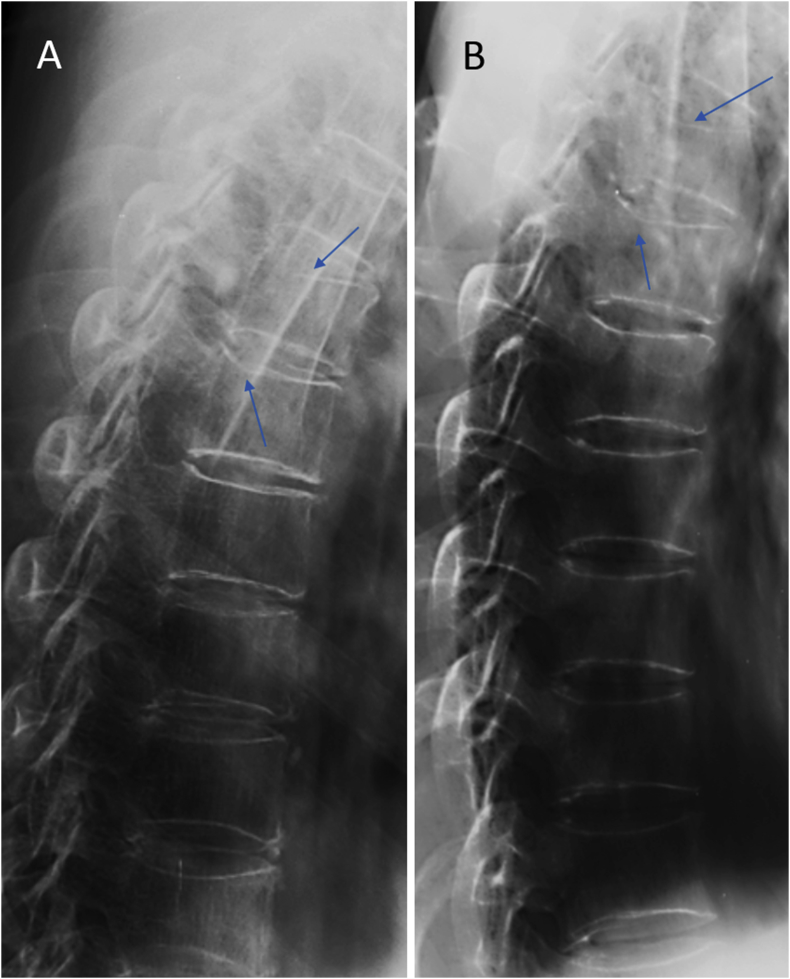
Figure 23.
Arrows indicate normal appearance of endplate in upper thoracic spine. Potential pitfall (due to X-ray projection) reading of endplate depression.
Figure 24.
Arrows indicate anterior vascular grooves. Radiographs (A) and (B) are from two subjects.
Figure 25.
Red long arrows indicate slight irregularity of vertebral anterior cortex, which should not be interpreted as cortex buckling. Black double-headed arrow indicates “bean-can” appearance due to X-ray projection.
Conflict of interest
The authors have no conflicts of interest to disclose in relation to this article.
Footnotes
We thanks Professor Ping Chung Leung, Professor Timothy CY Kwok, Mr Jason CS Leung, and Professor James Griffith, all at the Chinese University of Hong Kong, for the supports of this study.
References
- 1.Ross P.D. Clinical consequences of vertebral fractures. Am J Med. 1997;103:30S–42S. doi: 10.1016/s0002-9343(97)90025-5. [DOI] [PubMed] [Google Scholar]
- 2.Kado D.M., Browner W.S., Palermo L., Nevitt M.C., Genant H.K., Cummings S.R. Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1999;159:1215–1220. doi: 10.1001/archinte.159.11.1215. [DOI] [PubMed] [Google Scholar]
- 3.Morin S., Lix L.M., Azimaee M., Metge C., Majumdar S.R., Leslie W.D. Institutionalization following incident non-traumatic fractures in community-dwelling men and women. Osteoporos Int. 2012;23:2381–2386. doi: 10.1007/s00198-011-1815-7. [DOI] [PubMed] [Google Scholar]
- 4.Cooper C., Atkinson E.J., Jacobsen S.J., O'Fallon W.M., Melton L.J., 3rd Population-based study of survival after osteoporotic fractures. Am J Epidemiol. 1993;137:1001–1005. doi: 10.1093/oxfordjournals.aje.a116756. [DOI] [PubMed] [Google Scholar]
- 5.Nevitt M.C., Ettinger B., Black D.M. The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med. 1998;128(10):793–800. doi: 10.7326/0003-4819-128-10-199805150-00001. [DOI] [PubMed] [Google Scholar]
- 6.Bliuc D., Nguyen N.D., Milch V.E., Nguyen T.V., Eisman J.A., Center J.R. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301(5):513–521. doi: 10.1001/jama.2009.50. [DOI] [PubMed] [Google Scholar]
- 7.Kado D.M., Browner W.S., Palermo L., Nevitt M.C., Genant H.K., Cummings S.R. Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1999;159:1215–1220. doi: 10.1001/archinte.159.11.1215. [DOI] [PubMed] [Google Scholar]
- 8.Szulc P. Vertebral fracture: diagnostic difficulties of a major medical problem. J Bone Miner Res. 2018;33(4):553–559. doi: 10.1002/jbmr.3404. [DOI] [PubMed] [Google Scholar]
- 9.Lentle B.C., Oei E., Goltzman D. Vertebral fractures and morphometric deformities. J Bone Miner Res. 2018;33:1544–1545. doi: 10.1002/jbmr.3470. [DOI] [PubMed] [Google Scholar]
- 10.Wáng Y.X., Ruiz Santiago F., Deng M., Nogueira-Barbosa M.H. Identifying osteoporotic vertebral endplate and cortex fractures. Quant Imaging Med Surg. 2017;7:555–591. doi: 10.21037/qims.2017.10.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oei L., Koromani F., Rivadeneira F. Quantitative imaging methods in osteoporosis. Quant Imaging Med Surg. 2016;6:680–698. doi: 10.21037/qims.2016.12.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Diacinti D., Vitali C., Gussoni G. Misdiagnosis of vertebral fractures on local radiographic readings of the multicentre POINT (Prevalence of Osteoporosis in INTernal medicine) study. Bone. 2017;101:230–235. doi: 10.1016/j.bone.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 13.Lentle B.C., Berger C., Probyn L., For the CaMos Research Group Comparative Analysis of the radiology of osteoporotic vertebral fractures in women and men: cross-sectional and longitudinal observations from the Canadian Multicentre Osteoporosis Study (CaMos) J Bone Miner Res. 2018;33:569–579. doi: 10.1002/jbmr.3222. [DOI] [PubMed] [Google Scholar]
- 14.Oei L., Koromani F., Breda S.J. Osteoporotic vertebral fracture prevalence varies widely between qualitative and quantitative radiological assessment methods: the Rotterdam Study. J Bone Miner Res. 2018;33:560–568. doi: 10.1002/jbmr.3220. [DOI] [PubMed] [Google Scholar]
- 15.Fink H.A., Litwack-Harrison S., Ensrud K.E. For osteoporotic fractures in men (MrOS) study Group. Association of incident, clinically undiagnosed radiographic vertebral fractures with follow-up back pain symptoms in older men: the osteoporotic fractures in men (MrOS) study. J Bone Miner Res. 2017;32(11):2263–2268. doi: 10.1002/jbmr.3215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deng M., Zeng X.J., He L.C. Osteoporotic vertebral fracture prevalence in elderly Chinese men and women: a comparison of endplate/cortex fracture-based and morphometrical deformity-based methods. J Clin Densitom. 2017 Dec 2 doi: 10.1016/j.jocd.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Szulc P., Munoz F., Marchand F., Delmas P.D. Semiquantitative evaluation of prevalent vertebral deformities in men and their relationship with osteoporosis: the MINOS study. Osteoporos Int. 2001;12:302–310. doi: 10.1007/s001980170120. [DOI] [PubMed] [Google Scholar]
- 18.Genant H.K., Wu C.Y., van Kuijk C., Nevitt M.C. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res. 1993;8:1137–1148. doi: 10.1002/jbmr.5650080915. [DOI] [PubMed] [Google Scholar]
- 19.Schwartz E.N., Steinberg D. Detection of vertebral fractures. Curr Osteoporos Rep. 2005;3:126–135. doi: 10.1007/s11914-996-0015-4. [DOI] [PubMed] [Google Scholar]
- 20.Ruiz Santiago F., Tomás Muñoz P., Moya Sánchez E., Revelles Paniza M., Martínez Martínez A., Pérez Abela A.L. Classifying thoracolumbar fractures: role of quantitative imaging. Quant Imaging Med Surg. 2016;6:772–784. doi: 10.21037/qims.2016.12.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu W., Perera S., Medich D. Height loss, vertebral fractures, and the misclassification of osteoporosis. Bone. 2011;48:307–311. doi: 10.1016/j.bone.2010.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Szulc P., Munoz F., Marchand F., Delmas P.D. Semiquantitative evaluation of prevalent vertebral deformities in men and their relationship with osteoporosis: the MINOS study. Osteoporos Int. 2001;12:302–310. doi: 10.1007/s001980170120. [DOI] [PubMed] [Google Scholar]
- 23.Deng M., Kwok T.C.Y., Leung J.C.S., Leung P.C., Wang Y.X. All osteoporotically deformed vertebrae with >34% height loss have radiographically identifiable endplate/cortex fracture. J Orthop Translat. 2018;14:63–66. doi: 10.1016/j.jot.2018.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jiang G., Eastell R., Barrington N.A., Ferrar L. Comparison of methods for the visual identification of prevalent vertebral fracture in osteoporosis. Osteoporos Int. 2004;15:887–896. doi: 10.1007/s00198-004-1626-1. [DOI] [PubMed] [Google Scholar]
- 25.Ferrar L., Jiang G., Clowes J.A., Peel N.F., Eastell R. Comparison of densitometric and radiographic vertebral fracture assessment using the algorithm-based qualitative (ABQ) method in postmenopausal women at low and high risk of fracture. J Bone Miner Res. 2008;23:103–111. doi: 10.1359/jbmr.070902. [DOI] [PubMed] [Google Scholar]
- 26.Amling M., Pösl M., Ritzel H., Hahn M., Vogel M., Wening V.J. Architecture and distribution of cancellous bone yield vertebral fracture clues. A histomorphometric analysis of the complete spinal column from 40 autopsy specimens. Arch Orthop Trauma Surg. 1996;115:262–269. doi: 10.1007/BF00439050. [DOI] [PubMed] [Google Scholar]
- 27.Antonacci M.D., Mody D.R., Rutz K., Weilbaecher D., Heggeness M.H. A histologic study of fractured human vertebral bodies. J Spinal Disord Tech. 2002;15:118–126. doi: 10.1097/00024720-200204000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Imai K. Analysis of vertebral bone strength, fracture pattern, and fracture location: a validation study using a computed tomography-based nonlinear finite element analysis. Aging Dis. 2015;6:180–187. doi: 10.14336/AD.2014.0621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pham T., Azulay-Parrado J., Champsaur P., Chagnaud C., Legré V., Lafforgue P. "Occult" osteoporotic vertebral fractures: vertebral body fractures without radiologic collapse. Spine (Phila Pa 1976) 2005;30(21):2430–2435. doi: 10.1097/01.brs.0000184303.86932.77. [DOI] [PubMed] [Google Scholar]
- 30.Takahara K., Kamimura M., Nakagawa H., Hashidate H., Uchiyama S. Radiographic evaluation of vertebral fractures in osteoporotic patients. J Clin Neurosci. 2007;14:122–126. doi: 10.1016/j.jocn.2005.11.050. [DOI] [PubMed] [Google Scholar]
- 31.Zhao F.D., Pollintine P., Hole B.D., Adams M.A., Dolan P. Vertebral fractures usually affect the cranial endplate because it is thinner and supported by less-dense trabecular bone. Bone. 2009;44:372–379. doi: 10.1016/j.bone.2008.10.048. [DOI] [PubMed] [Google Scholar]
- 32.Kwok A.W., Gong J.S., Wang Y.X., Leung J.C., Kwok T., Griffith J.F. Prevalence and risk factors of radiographic vertebral fractures in elderly Chinese men and women: results of Mr. OS (Hong Kong) and Ms. OS (Hong Kong) studies. Osteoporos Int. 2013;24:877–885. doi: 10.1007/s00198-012-2040-8. [DOI] [PubMed] [Google Scholar]
- 33.Siriwanarangsun P., Statum S., Biswas R., Bae W.C., Chung C.B. Ultrashort time to echo magnetic resonance techniques for the musculoskeletal system. Quant Imaging Med Surg. 2016;6:731–743. doi: 10.21037/qims.2016.12.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fechtenbaum J., Briot K., Paternotte S. Difficulties in the diagnosis of vertebral fracture in men: agreement between doctors. Jt Bone Spine. 2014;81:169–174. doi: 10.1016/j.jbspin.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 35.Delmas P.D., van de Langerijt L., Watts N.B. Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res. 2005;20:557–563. doi: 10.1359/JBMR.041214. [DOI] [PubMed] [Google Scholar]
- 36.Wáng J.Q., Káplár Z., Deng M. Thoracolumbar intervertebral disc area morphometry in elderly Chinese men and women: radiographic quantifications at baseline and changes at year-4 follow-up. Spine (Phila Pa 1976) 2018;43:E607–E614. doi: 10.1097/BRS.0000000000002482. [DOI] [PubMed] [Google Scholar]
- 37.Wáng Y.X., Deng M., Griffith J.F. Lumbar spondylolisthesis progression and de novo spondylolisthesis in elderly Chinese men and women: a Year-4 follow-up study. Spine (Phila Pa 1976) 2016;41:1096–1103. doi: 10.1097/BRS.0000000000001507. [DOI] [PubMed] [Google Scholar]