Abstract
Objective
Fasting Ramadan is associated with changes in lifestyle patterns of patients with diabetes who choose to perform fasting. We aimed to determine the attitude and habits of patients with type 1 diabetes during fasting Ramadan.
Methods
The study comprised a prospective cohort of patients with type 1 diabetes who were on insulin pump or multiple daily insulin injections (MDI) regimen. Patient questionnaires included the frequency of self-monitoring of blood glucose (SMBG), the need to make changes in insulin regimen by patients, timings of insulin administration, performing carbohydrate counting and levels of physical activity.
Results
A total of 156 patients were studied (61 patients on insulin pump and 95 patients on MDI). Patients on pump therapy performed SMBG more frequently than those on MDI regimen (4.8 ± 1.4 and 3.7 ± 1.7 times per day, respectively, P = 0.001) and were more likely to perform carbohydrate counting (32.7% and 8.4% of pump and MDI patients, respectively, P < 0.001). There was no difference in the percentage of patients who made changes in insulin doses (74.5% of the pump group and 77.3% of MDI patients) or those who had any level of physical activity (12.5% of the pump group and 21.1% of the MDI group). The timing of administering meal insulin in relation to sunset meal was variable with a preference to taking the injection immediately at sunset. There was no difference in glucose control between both groups as measured by frucotsamine levels or the number of days that patients have to stop fasting.
Conclusion
Fasting Ramadan is associated with significant and variable changes in the attitude and behaviors of patients with type 1 diabetes with no difference in glucose control between patients on insulin pump or MDI regimen. Further studies are needed to define the role of education and its effect on these attitudes and patient care in this population.
ClinicalTrials.gov Identifier: NCT01941238.
Fasting the month of Ramadan is a fundamental religious practice performed by millions of Muslims every year. Fasting Ramadan has been shown to be associated with an increased risk of hypoglycemia and glycemic deterioration in some patients with diabetes, particularly type1 diabetes [1], [2]. During this month and depending on culture patients adapt many changes that affect eating habits, physical activity and sleep patterns. Food intake becomes exclusively nocturnal and is characterized by a large fast-breaking meal at sunset commonly with large portions of carbohydrate-rich food. In the majority of Muslim countries, the working hours are reduced and patients’ daily activity pattern changes where the main activity occurs at night and much less activity prevails during daytime. Patients with type 1 diabetes are considered high risk for acute complications during Ramadan and expert professional guidelines advice that these patients should not fast [2], [3]. Despite that it was reported that about 43% of those patients fast during Ramadan [4]. Often these patients would fast without medical guidance which may lead to the development of acute complications [1]. Therefore, managing patients with type 1 diabetes during fasting Ramadan can be challenging. Assessment of lifestyle aspects of those patients is important in order to address required changes in insulin doses and timing of insulin administration to assure safe fasting. Clinical studies addressing fasting in patients with type 1 diabetes are limited. We aimed to examine the attitude and daily habits of patients with type 1 diabetes who fast Ramadan, comparing patients on insulin pump with those on multiple daily insulin injections (MDI).
Methods
The study comprised of a prospective cohort of patients with type 1 diabetes who were either on insulin pump or MDI regimen attending diabetes clinics in Ministry of National Guard hospitals in three cities in Saudi Arabia. All patients planning fasting Ramadan were offered to participate. Patients were included if they were ≥14 years of age and were diagnosed with type 1 diabetes for at least 6 months and on either insulin pump (for at least 3 months) or MDI regimen which included a basal insulin (Glargine or Detemir) with a rapid-acting insulin (Aspart, Glulisine or Lispro). Patients were required to have two study visits, one at 1–2 months before the start of Ramadan and the other visit after the end of the month. Demographic data and data on the frequency of performing self-monitoring of blood glucose (SMBG), eating habits, performing carbohydrate counting, presence of physical activity, self-management of insulin doses, timing of meal (or bolus) insulin in relation to meals were collected using self-administrable questionnaires. The questionnaire was validated on a pilot of patients before starting the study. Eating habits at the time of breaking of fasting at sunset “Iftar” was assessed as there are different practices including taking the mean meal immediately at sunset, after sunset prayer or late evening. Timing of taking meal insulin in relation to iftar meal, using insulin at predawn meal “Suhur” and taking an extra meal at midnight with or without insulin were assessed. Levels of physical activities were categorized into active, not active enough and inactive. Active was defined as more than 15 minutes of medium exercise or 60 minutes of heavy exercise per week. Not active enough was defined as 30 to less than 150 minutes of medium exercise per week. Inactive was defined as less than 30 minutes of medium exercise per week. The intensity of physical activity was defined as medium exercise which included only walking and heavy exercise which included jogging or running. All patients received standardized diabetes education according to the curriculum of the international diabetes federation. The aspects of diabetes care including adjustment of insulin doses were left to be managed at the discretion of the treating physician. Patients accustomed to making adjustments to their insulin doses based on results of SMBG and carbohydrate counting were allowed to continue to do so. The number of days that patients had to break their fast along with accompanied reasons – usually hypoglycemia or significant hyperglycemia- was assessed. Due to the risk of fasting in patients with type 1 diabetes and following professional guidelines of target fasting and premeal glucose levels of 4.4–7.2 mmol/L [5], a capillary glucose value of <4.4 mmol/L was defined as hypoglycemia. Patients were advised to stop their fast if they had hypoglycemia or significant hyperglycemia-defined as a glucose value of >16.6 mmol at any time of the day [3]. Glucose control was assessed by measuring serum frucotsamine levels before and after the month of Ramadan. This study reports data focused on attitudes and behaviours, data on hypoglycemia using CGM and SMBG have been reported in a separate publication [20].
Statistical analysis
Data was entered and analysed using the Statistical Package of Social Sciences (SPSS). Continuous results were expressed as means and SDs or medians and interquartile ranges according to the data distribution, and categorical data was presented as proportions with 95% confidence intervals. Between-group comparison was done using a student-t-test or Mann-Whitney U test where the data are not normally distributed. For categorical data, chi square test (with Yates’ correction or Fisher’s exact test where appropriate) were used. The level of statistical significance was chosen as P ≤ 0.05 (two-sided).
Results
A total of 156 patients with type 1 diabetes were studied, 61 patients on insulin pump and 95 patients on MDI regimen. The baseline characteristics of patients are shown in Table 1. The mean age, mean duration of diabetes, body mass index and level of education were not different in the insulin pump patients and MDI group while HbA1c levels were significantly lower in the insulin pump group compared to the MDI group [8.5 ± 1.6% (69.4 ± 9.6 mmol/mol) versus 9.3 ± 2.3% (78.1 ± 17.3 mmol/mol, P = 0.045]. Levels of serum fructosamine were not different between both groups before Ramadan (385.6 ± 76.1 µmol/L in the insulin pump group and 409.2 ± 95.5 µmol/L in the MDI group, P = 0.12).
Table 1.
Baseline characteristics of study groups.
| Insulin pump (n = 61) | MDI (n = 95) | P value | |
|---|---|---|---|
| Gender | |||
| Male | 18 (29.5%) | 41 (43.2%) | 0.09 |
| Female | 43 (70.5%) | 54 (56.8%) | |
| Age (years) | 23.4 ± 06.1 | 21.3 ± 06.3 | 0.04 |
| Educational level | |||
| Elementary/Intermediate | 3 (5%) | 13 (13.8%) | 0.23 |
| High school | 25 (41.7%) | 42 (44.7%) | |
| University | 31 (51.7%) | 37 (39.4%) | |
| Duration of diabetes (years) | 10.8 ± 05.4 | 9.3 ± 06.6 | 0.19 |
| BMI | 26.4 | 25.8 | 0.51 |
| HbA1c % (mmol/mol) | 8.5 ± 1.6 (69.4 ± 9.6) | 9.3 ± 2.3 (78.1 ± 17.3) | 0.04 |
| Fructosamine (µmol/L) | 385.6 ± 76.1 | 409.2 ± 95.5 | 0.12 |
| Perform carbohydrate counting | 20 (32.7%) | 8 (8.4%) | <0.001 |
| Performed SMBG^ ≥ 4 times/day | 35 (57.4%) | 23 (24.5%) | 0.001 |
| Physical Activity* | |||
| Active | 15 (25.0%) | 18 (20.2%) | 0.76 |
| Not active enough | 25 (41.7%) | 41 (46.1%) | |
| Inactive | 20 (33.3%) | 30 (33.7%) | |
BMI, Body Mass Index; HbA1c, glycated hemoglobin. *Active:(>150 mins of medium exercise or 60 mins of heavy exercise per week); Not active enough: (30 to <150 mins of medium exercise per week/week); Inactive: (<30 mins of medium exercise per week), ^SMBG: self-monitoring of blood glucose.
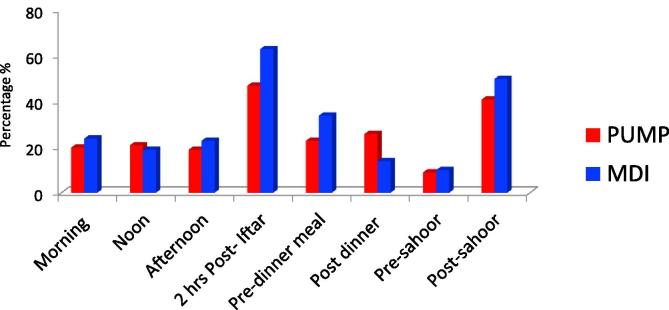
Table 2 shows the behaviors and attitudes of studied patients during Ramadan. Carbohydrate counting was performed by more patients in the insulin pump group compared to the MDI group, 36.1% and 26.1%, respectively, P < 0.001. SMBG was performed 4 times or more daily by 57.4% of the pump group compared to 24.5% of the MDI group, P < 0.001. A higher number of patients in both groups performed SMBG 2 times or more daily, with more patients doing so in the insulin pump group (95% of the pump group and 77.6% of the MDI group, p < 001). Fig. 1 shows the difference between the two groups in favored time of day performing SMBG. There was a significant difference in patients who reported omitting at least one daily insulin dose between both groups: 27.6% of the pump group (not taking bolus insulin doses) compared to 57.6% of the MDI group, p = 0.005. Planning to change insulin doses in Ramadan was reported by 54.1% of the pump group versus 36.8% of the MDI group, P = 0.037. However, during Ramadan more patients in both groups made adjustments to their insulin doses with an end result of no difference between both groups (74.5% of the pump group and 77.3% of the MDI group, P = 0.751. The timing of taking the main meal in relation to sunset (Iftar) along with timing of taking meal insulin varied significantly among patients, but did not vary between the insulin pump and MDI groups. The favored time for taking the main meal was at sunset call for prayer (54.3% of patients) followed by taking a small meal at sunset then consuming the main meal immediately after sunset prayer (34.5% of patients). Meal insulin at Iftar was administered in the majority of patients at sunset call (60.6% of patients).
Table 2.
Patients’ attitudes during Ramadan.
| Factors | Pump (n = 61) | MDI (n = 95) | P value |
|---|---|---|---|
| Patients plan to change insulin doses in Ramadan | 33 (54.1%) | 32 (33.7%) | 0.03 |
| Patients changed insulin doses in Ramadan | 45 (74.5%) | 73 (77.3%) | 0.75 |
| Iftar#attitudes | |||
| Main meal immediately at sunset call for prayer | 25 (49%) | 23 (59.7%) | 0.48 |
| Small meal at sunset call followed by main meal immediately after sunset prayer | 20 (39.2%) | 23 (29.9%) | |
| Small meal at sunset call followed by main meal after late evening “Isha” prayer | 6 (11.8%) | 8 (10.4%) | |
| Timing of Iftar#meal insulin | |||
| Before sunset call | 6 (12%) | 19 (24.7%) | 0.15 |
| At sunset call | 34 (68%) | 41 (53.2%) | |
| After sunset prayer call with the main meal | 9 (18%) | 16 (20.8%) | |
| After late evening “Isha” prayer with the main meal | 1 (2%) | 0 | |
| Regularly take a midnight meal | 31 (63.3%) | 51 (68%) | 0.73 |
| Take insulin with midnight meal | 28 (93.3%) | 32 (62.7%) | 0.004 |
| Take insulin with pre-dawn “Sahoor “ meal | 54 (88.4%) | 83 (87.4%) | 0.44 |
| Sleep pattern | |||
| During the daytime | 47 (92.2%) | 72 (93.5%) | 0.99 |
| At night | 4 (7.8%) | 5 (6.5%) | |
| Perform any level physical activity (after ishaa-dawn) | 39 (81.3%) | 55 (77.5%) | 0.21 |
| Number of daily SMBG performed | 4.8 ± 1.4 | 3.7 ± 1.7 | 0.001 |
Iftar: meal consumed at sunset, “Sahoor ”: predawn meal, “Isha”: late evening.
Fig. 1.
Timing of doing SMBG during Ramadan.
There was no difference in the percentage of patients who performed any type of physical activity during Ramadan (81.3% of the pump group and 77.5% of the MDI group). Most patients (78.7% of the pump group and 71.5% of the MDI group) had their activity after late evening “Isha” prayer. The majority of patients had their sleeping time during day time (92.2% of the pump group and 93.5% of the MDI group) with no difference in the number of sleeping hours (9.1 ± 0.2 h in the pump group and 8.8 ± 2 h in the MDI group, P = 0.4).
There was no difference in the percentage of patients who could fast the whole month of Ramadan without the need to break their fast (31.2% of patients in the insulin pump group and 22.1% of patients in the MDI group, P = 0.41). There was no difference in glycemic control between both groups as measured by fructosamine levels after the end of Ramadan (392.8–60.1 µmol/L in the pump group and 405.9–84.4 µmol/L in MDI group, P = 0.61) or the number of days that patients have to stop fasting between both groups (4.1 ± 5.3 days in the insulin pump group compared to 5.7 ± 5.8 days in MDI group, P = 0.23). The main reasons for stopping fasting was hypoglycemia (81.2% in the insulin pump group and 88.7% in the MDI group), followed by significant hyperglycemia (18.7% and 18.9% respectively). No diabetic ketoacidosis was reported in either group.
Discussion
Fasting Ramadan is not merely abstinence from eating but involves a drastic change in lifestyle aspects and habits. Addressing these lifestyle changes is essential and can become a challenge in the daily management of diabetes. The majority of clinical studies addressing fasting have focused on type 2 diabetes [6], [7], [8], [9], [10], [11], [12], [13] while studies in patients with type 1 diabetes have focused mainly on modes of treatment and risks of complications during fasting [14], [15], [16], [17], [18], [19], [20]. Data on habits and attitudes of patients with diabetes during Ramadan is limited. Deeb and colleagues evaluated the willingness of children and adolescents with type 1 diabetes to fast Ramadan and the frequency of acute complications during fasting [21]. They found that most patients were keen to fast Ramadan with no difference in rates of hypoglycemia or hyperglycemia between patients on insulin pump or MDI.
We found that a large number of patients particularly those on MDI therapy did not perform regular SMBG during fasting. This can have a negative impact on glucose control due to lack of data to make proper adjustments in insulin therapy. Patients on insulin pump therapy were more likely to perform SMBG and more likely to follow carbohydrate counting while patients on MDI therapy were more likely to forget their insulin injections. Even though a significant number of patients in our study had no plans on adjusting insulin doses during fasting, a large percentage did change the doses on their own. A structured education program that included frequent SMBG, plans for adjustment of medications and dietary advice during Ramadan has been shown to help patients fast safely with a reduction in the frequency of hypoglycemia [22]. We have observed a wide range of different habits regarding the timing the main meal at sunset (Iftar) as well as the timing of administering meal insulin. This can have implications on glucose levels during fasting and should prompt physicians and educators to put this in consideration when providing patient education about insulin injection timing and dose adjustment during Ramadan. This was also reflected in the fact that a significant number of patients had to make adjustments in their insulin doses even though this was not initially planned before Ramadan. These findings indicate the need for intensive education to make sure patients with type 1 diabetes master self-management optimally in particular during the fasting month of Ramadan.
Professional guidelines emphasize that educational programs for patients with diabetes intending to fast Ramadan should aim at empowering patients with necessary knowledge to make informed decisions regarding glucose management during fasting [3]. The recommended key components of these programs are risk quantification, self-monitoring of blood glucose, advice on nutrition and physical activity, medication adjustments and understanding when to break the fast.
The wide variability of patients’ habits during fasting in our study emphasizes the need for individualized level of patient education. Patients with type 2 diabetes planning to fast Ramadan who received an individualized educational program were more likely to modify their diabetes treatment, to perform SMBG, to have less episodes of hypoglycemia, to have less weight and to have better glucose control compared with usual care [23]. We propose to add assessment of individual patient habits during Ramadan to patient education programs. This could assist patients to make timely and proper decisions regarding therapy
In conclusion, fasting the month of Ramadan for patients with diabetes is associated with major changes in attitudes and behaviors which can affect glycemic control. This requires that patients planning to fast receive continuous multidisciplinary support along with properly structured educational programs for optimal outcomes.
Acknowledgments
The study was sponsored through a grant from King Abdullah International Medical Research Center (KAIMRC). Our thanks and appreciation to the efforts of our study site coordinators: Ms. Amal Aljaafari, Ms. Fatme Elhabbal, Ms. Suzan Oraibi, and Ms. Shahinaz Bashir, and to our diabetes educators: Ms. Mehad Awad, Ms. Faiza Haider, Ms. Sultana Alenazi, Ms. Rasha Alwehaib, Ms. Sabah Alshuwish, and Ms. Rahab Hamad. Parts of this study were presented as poster presentation at the Endocrine Society’s 98th Annual Meeting and Expo, April 1–4, 2016, Boston—SAT-700 on April 2, 2016.
Footnotes
Sources of Research Support: Grant from King Abdullah International Medical Research Center.
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.jcte.2018.09.001.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Ali G., Car N., Muacevic D. Fasting of persons with diabetes mellitus during Ramadan. Diabetologia Croatica. 2002;31:75–84. [Google Scholar]
- 2.Al-Arouj M., Khalil S., Buse J., Fahdil I., Fahmy M., Hafez S. Recommendations for management of diabetes during Ramadan. Diabet Care. 2010;33:1895–1902. doi: 10.2337/dc10-0896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hassanein M, Al-Arouj M, Ben-Nakhi A, Jabbar A, Hanif W, Al-Madani A, et al. Diabetes and Ramadan: practical guidelines International Diabetes Federation (IDF) in collaboration with the Diabetes and Ramadan (DAR) International Alliance. http://www.idf.org/sites/default/files/IDF-DAR-Practical-Guidelines-Final-Low.pdf [accessed 12 August 2017].
- 4.Salti I., Benard E., Detournay B., Bianchi M., Brigand C., Voinet C. A population-based study of diabetes and its characteristics during the fasting month of Ramadan in 13 countries: results of the epidemiology of diabetes and Ramadan 1422/2001 (EPIDIAR) study. Diabet Care. 2004;27:2306–2311. doi: 10.2337/diacare.27.10.2306. [DOI] [PubMed] [Google Scholar]
- 5.American Diabetes Association Standards of medical care in diabetes-2018. Diabet Care. 2018;41(Suppl. 1):S55–S64. doi: 10.2337/dc18-S006. [DOI] [PubMed] [Google Scholar]
- 6.Babineaux S.M., Toaima D., Boye K.S., Zagar A., Tahbaz A., Jabbar A. Multi-country retrospective observational study of the management and outcomes of patients with Type 2 diabetes during Ramadan in 2010 (CREED) Diabet Med. 2015;32:819–828. doi: 10.1111/dme.12685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Uysal A.R., Erdoğan M.F., Sahin G., Kamel N., Erdoğan G. Clinical and metabolic effects of fasting in 41 type 2 diabetic patients during Ramadan. Diabet Care. 1998;21:2033–2034. doi: 10.2337/diacare.21.11.2033. [DOI] [PubMed] [Google Scholar]
- 8.Laajam M.A. Ramadan fasting and non-insulin-dependent diabetes: effect on metabolic control. East Afr Med J. 1990;67:732–736. [PubMed] [Google Scholar]
- 9.Mafauzy M., Mohammed W.B., Anum M.Y., Zulkifli A., Ruhani A.H. A study of the fasting diabetic patient during the month of Ramadan. Med J Malaysia. 1990;45:14–17. [PubMed] [Google Scholar]
- 10.Belkhadir J., el Ghomari H., Klöcker N., Mikou A., Nasciri M., Sabri M. Muslims with non-insulin dependent diabetes fasting during Ramadan: treatment with glibenclamide. BMJ. 1993;307:292–295. doi: 10.1136/bmj.307.6899.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Katibi I.A., Akande A.A., Bojuwoye B.J., Okesina A.B. Blood sugar control among fasting Muslims with type 2 diabetes mellitus in Ilorin. Niger J Med. 2001;10:132–134. [PubMed] [Google Scholar]
- 12.Omar M., Motala A. Fasting in Ramadan and the diabetic patient. Diabet Care. 1997;20:1925–1926. doi: 10.2337/diacare.20.12.1925. [DOI] [PubMed] [Google Scholar]
- 13.Azizi F., Siahkolah B. Ramadan fasting and diabetes mellitus. Int J Ramadan Fasting Res. 1998;28:8–17. [Google Scholar]
- 14.Kadiri A., Al-Nakhi A., El-Ghazali S., Jabbar A., Al Arouj M., Akram J. Treatment of type 1 diabetes with insulin lispro during Ramadan. Diabet Metab. 2001;27:482–486. [PubMed] [Google Scholar]
- 15.Mucha G.T., Merkel S., Thomas W., Bantle J.P. Fasting and insulin glargine in individuals with type 1 diabetes. Diabet Care. 2004;27:1209–1210. doi: 10.2337/diacare.27.5.1209. [DOI] [PubMed] [Google Scholar]
- 16.Hawli Y., Zantout M.S., Azar S.T. Adjusting the basal insulin regimen of patients with type 1 diabetes mellitus receiving insulin pump therapy during the Ramadan fast: a case series in adolescents and adults. Curr Ther Res Clin Exp. 2009;70:29–34. doi: 10.1016/j.curtheres.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Benbarka M., Khalil A., Beshyah S., Marjei S., Abu Awad S. Insulin pump therapy in Moslem patients with type 1 diabetes during Ramadan fasting: an observational report. Diabet Ther. 2010;12:287–290. doi: 10.1089/dia.2009.0130. [DOI] [PubMed] [Google Scholar]
- 18.Vigeral C., Sola-Gazagnes A., Nejjar S., M'Bemba J., Boitard C., Slama G. Ambulatory 24-hour fast using flexible insulin therapy in patients with type 1 diabetes. Diabet Metab. 2011;37:553–559. doi: 10.1016/j.diabet.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 19.Khalil A.B., Beshyah S.A., Abu Awad S.M., Benbarka M.M., Haddad M., Al-Hassan D. Ramadan fasting in diabetes patients on insulin pump therapy augmented by continuous glucose monitoring: an observational real-life study. Diabet Technol Ther. 2012;14:813–818. doi: 10.1089/dia.2012.0061. [DOI] [PubMed] [Google Scholar]
- 20.Alamoudi R., Alsubaiee M., Alqarni A., Saleh Y., Aljaser S., Salam A. Comparison of insulin pump therapy and multiple daily injections insulin regimen in patients with type 1 diabetes during Ramadan fasting. Diabet Technol Ther. 2017;19:349–354. doi: 10.1089/dia.2016.0418. [DOI] [PubMed] [Google Scholar]
- 21.Deeb A., Al Qahtani N., Akle M., Singh H., Assadi R., Attia S. Attitude, complications, ability of fasting and glycemic control in fasting Ramadan by children and adolescents with type 1 diabetes mellitus. Diabet Res Clin Pract. 2017;126:10–15. doi: 10.1016/j.diabres.2017.01.015. [DOI] [PubMed] [Google Scholar]
- 22.Ahmedani M.Y., Haque M.S., Basit A., Fawwad A., Alvi S.F. Ramadan Prospective Diabetes Study: the role of drug dosage and timing alteration, active glucose monitoring and patient education. Diabet Med. 2012;29:709–715. doi: 10.1111/j.1464-5491.2011.03563.x. [DOI] [PubMed] [Google Scholar]
- 23.McEwen L.N., Ibrahim M., Ali N.M., Assaad-Khalil S.H., Tantawi H.R., Nasr G. Impact of an individualized type 2 diabetes education program on clinical outcomes during Ramadan. BMJ Open Diabet Res Care. 2015;3:e000111. doi: 10.1136/bmjdrc-2015-000111. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.