Abstract:
Purpose
Postoperative protocols following surgical management of supracondylar humerus fractures (SCFs) are often based upon surgeon preference rather than clinical merit. The purpose of this study is to determine the utility of early clinical and radiographic follow-up.
Methods
A retrospective review of patients who underwent closed reduction and percutaneous pinning (CRPP) for SCF between 2009 and 2015 was performed using a database of prospectively-collected consecutive patient data. Previously undiagnosed neuropathies documented at the first postoperative visit were identified. Unscheduled visits and postoperative complications were compared between patients who were seen at one week and those with delayed first clinic visits.
Results
Of 873 patients, 823 (94.3%) were seen within ten days of surgery (early follow-up) and 50 (5.7%) had a delayed first clinic appointment. Among patients seen for early follow-up, 12 (1.5%) had a previously undocumented neuropathy diagnosed but only eight (1%) had an alteration of management secondary to clinical findings. Greater than 90% of patients seen for early follow-up had radiographs performed, but only one had an alteration in management due to radiographic findings. Patients seen for early follow-up had the same rate of unscheduled visits (2.9% versus 4%, p = 0.66) and postoperative complications (1.6% versus 0%, p > 0.99) as those with delayed first appointments. Radiographic parameters were comparable at final follow-up (Baumann’s angle 74.5° versus 73.7°, p = 0.40; lateral humeral condylar angle 40.2° versus 41.2°, p = 0.53).
Conclusion
The early follow-up visit after CRPP of SCF rarely leads to alterations in care and does not reduce unscheduled visits or late complications.
Level of Evidence
Level IV
Keywords: supracondylar fracture, postoperative visit, postoperative protocol
Introduction
While there has been a move towards improved clinical decision-making and evidence-based practice in orthopaedic surgery, there is little evidence to support the majority of postoperative clinical and radiographic follow-up protocols. This is especially true for paediatric supracondylar humerus fractures (SCFs). Despite their ubiquity, there is no consensus on appropriate postoperative management.1 Neither the American Academy of Orthopaedic Surgeons clinical practice guidelines or the evidence-based guidelines published in the Journal of Pediatric Orthopaedics regarding the treatment of SCF address optimal timing of postoperative clinical or radiographic follow-up or provide information regarding postoperative care.2–4 Both guidelines report the lack of evidence concerning optimal time to pin removal.2–4
Given the current lack of evidence to support a singular postoperative pathway, we sought to examine the postoperative management protocols at a single level 1 paediatric centre. The goal of this study is to determine the utility of the standard one-week clinical return visit and of early radiographic follow-up after routine closed reduction and percutaneous pinning (CRPP) of paediatric SCF.
Materials and methods
All patients treated for SCF with CRPP between 2009 and 2015 at a single level 1 paediatric trauma centre were prospectively enrolled in a database. Informed consent was obtained for each patient prior to enrolment. Institutional Review Board approval was obtained to review this database for the study. All included patients were between 0 and 12 years of age, had closed fractures and were classified as either flexion-type or extension Gartland type II or III fractures.5 All included patients were treated with CRPP within ten days of injury. Exclusion criteria included pulseless extremity, open fractures and the need for open reduction as these cases are typically more complex and may warrant case-specific changes in postoperative management compared with SCFs that are treated with CRPP.
Information obtained during prospective enrolment included age, gender, weight, date of injury, mechanism of injury, details of preoperative neurologic and vascular examinations, date of fixation, date of first and last follow-up, treating surgeon and complications noted at any time intra- or postoperatively. Records were further reviewed to determine the number of postoperative visits and postoperative radiographs, the date of the first postoperative clinical visit and first postoperative radiographic exam and whether changes were made to patient immobilization postoperatively. Alterations in patient management, unscheduled clinic or emergency department (ED) visits, postoperative complications, payor status and clinical outcomes were also recorded. Postoperative complications included postoperative infection, pin migration or failure, new neurovascular injury and return to surgery.
Pre- and postoperative radiographs were reviewed to determine fracture type, fixation construct, fracture alignment and radiographic healing. Final Baumann’s angle as well as lateral humeral condylar angle (LHCA) were measured by a single observer (ME) who was blinded to the patient’s postoperative clinical visit schedule. Radiographs were measured using iSite picture archiving and communication medical imaging angular measurement tools (Philips Healthcare, Philips North America Corporation, Andover, Massachusetts).
Statistical analysis was performed to compare those patients seen within ten days from date of surgery (early follow-up) and those first visit occurred more than ten days postoperatively (delayed follow-up). These cohorts were compared in regard to incidence of unscheduled clinic/ED visits and rate of postoperative complications. Means and ranges were used to describe continuous variables and percentages were used for categorical variables. Independent two-sample t-tests were used to compare parametric data. Mann-Whitney U and chi-squared tests were used to compare non-parametric data. Fisher’s exact tests were used for categorical variables. Statistical significance was set at p < 0.05.
No external funding was used for this study.
Results
A total of 873 patients met inclusion criteria. There was an even distribution of male to female patients (53%:47%), with a mean age at presentation of 5.08 years sd 2.15 and a mean body mass index (BMI) of 17.7 sd 9.02. Of the included patients, 321 fractures (36.8%) were classified as Gartland type II, 494 (56.6%) as Gartland type III and 47 (5.4%) as flexion type. In all, 68 patients (7.8%) had neuropraxias diagnosed preoperatively and none had vascular compromise requiring direct intervention. An all-lateral pin construct was used in 570 (65.2%) patients and 304 were stabilized with a crossed-pin construct (34.8%). Pin size and the decision to use an all-lateral versus crossed-pin construct were determined at the time of operative fixation by the attending surgeon, with the most common Kirschner-wire ranging from 1.6 mm to 2 mm in diameter. Methodology regarding assessment of fracture stability after fixation was also surgeon specific, although it is common at our institution to gently flex and extend the elbow under live fluoroscopy to confirm that fracture alignment is stable after CRPP and prior to splint/cast application. All patients were initially immobilized with a posterior plaster splint in approximately 70° of flexion.
Nine fellowship-trained pediatric orthopaedic surgeons managed 838 (96%) patients. The remainder were seen by a combination of postoperative providers and/or surgeons who treat a lower volume of trauma patients. This resulted in seven unique postoperative protocols, five of which were used most frequently (greater than 50 patients per protocol; Fig. 1). Each patient’s postoperative protocol was determined based on the preference of the treating surgeon. Patients had a mean of 2.9 postoperative clinic visits (1 to 6) and had 2.5 radiographic series taken postoperatively (1 to 6). Mean postoperative follow-up was ten weeks (2.5 to 54). There was no difference in age (p = 0.694), BMI (p = 0.2012) or mechanism of injury (p = 0.559) between patients seen at one week and those with delayed first visits. Similarly, there was no difference in the distribution of fracture type and no correlation between pin construct (p = 0.238) or pin number (p = 0.344) between patients seen at one week and those with delayed follow-up.
Fig. 1.
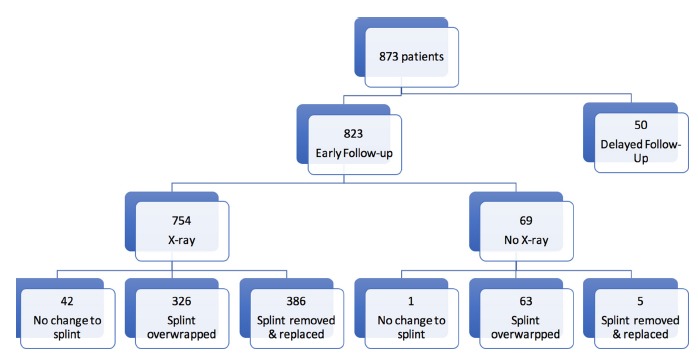
Postoperative protocol variation after closed reduction and percutaneous pinning of supracondylar humerus fractures.
Of the 873 patients who met inclusion criteria, 823 (94.3%) had an early follow-up visit (mean eight days postoperative (sd 2); Fig. 1). More than 90% of early follow-up patients had radiographs obtained at that visit (754/823, 91.5%). More than 90% of early follow-up patients also underwent alterations to their splints, with 39.6% of patients having splints overwrapped and 46.9% of patients have splints removed and replaced with fibreglass long-arm casts. A total of 42 patients (5.1%) had no alterations to their postoperative immobilization (Fig. 1).
Of early follow-up patients, eight (1%) had changes in management based on history or clinical exam alone and only one patient had a change in management based off radiographic findings from the one-week radiographs. One patient returned to the OR for removal of pins that migrated under the skin, two were treated with antibiotics for pin site infection, one was prophylactically treated with antibiotics for an unrelated fever and three patients had cast changes for skin issues (allergic dermatitis, fracture blisters and wet cast). One patient with a crossed-pin fixation construct presented with a previously undocumented ulnar nerve palsy and the medial pin was removed at the first postoperative visit as a result of this new diagnosis. Only one early follow-up patient (0.1%) had changes in management based on radiographs, in which the treating surgeon pulled back an anteriorly-protruding asymptomatic pin (Fig. 2). All nine patients with changes in postoperative management went onto radiographic union and satisfactory clinical function without further complication or alteration in total follow-up time compared with those without alterations in management (8.9 weeks versus 9.9 weeks, p = 0.92). The patient with the new diagnosis of ulnar nerve palsy had complete resolution of symptoms with return of sensory and motor function by the final follow-up visit.
Fig. 2.
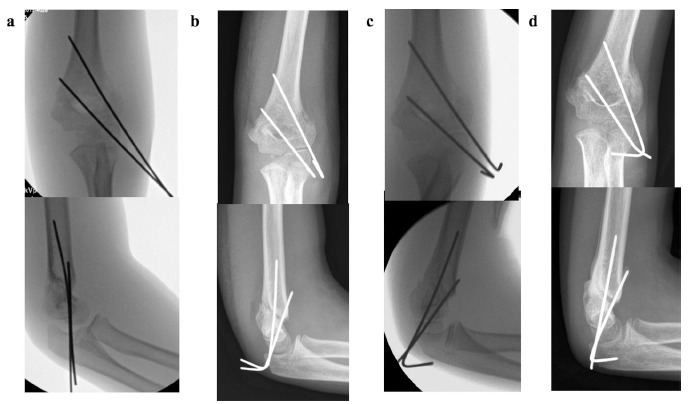
Radiographs of patient whose pin was pulled back at early follow-up visit: (a) patient’s intraoperative radiographs; (b) at early follow-up prior to pin adjustment and; (c) after the pin was pulled back; (d) radiographs at time of pin removal. Pins shown are 1.6 mm in diameter.
In all, 12 early follow-up patients (1.5%) had previously-undocumented neuropathies identified at the initial postoperative visit (five median, four anterior interosseous nerve, two radial and one ulnar). One patient’s care was altered as a result as previously described. All 12 had complete resolution of symptoms at final follow-up, although these patients were followed for a significantly longer course postoperatively than those without a late-documented neuropathy (15 versus ten weeks, p = 0.0004). No demographic factors were predictive of late-presenting neuropathies, nor was mechanism of injury or fracture type. Pin construct was not predictive of late-neuropathy (1.4% in all lateral versus 1.3% incidence in cross-pin, p > 0.999) but there was a correlation between number of pins and late-presenting neuropathy, with a preponderance treated with a three-pin construct (p = 0.047, Table 1).
Table 1.
Newly-diagnosed nerve injuries noted at the early follow-up visit*
| Nerve injury newly noted at first postoperative visit? | ||||||
|---|---|---|---|---|---|---|
| No | Yes | |||||
| Count | % | Count | % | p-value | ||
| Gender | Female | 410 | 47.6 | 3 | 25.0 | 0.15† |
| Male | 451 | 52.4 | 9 | 75.0 | ||
| Fracture type | Flexion | 47 | 5.5 | 0 | 0.0 | |
| Extension, type II | 319 | 37.5 | 2 | 16.7 | ||
| Extension, type III | 484 | 56.9 | 10 | 83.3 | ||
| Pin construct | All lateral | 562 | 65.3 | 8 | 66.7 | > 0.999‡ |
| Cross-pin | 299 | 34.7 | 4 | 33.3 | ||
| Mechanism | Low | 368 | 43.0 | 4 | 33.3 | |
| Medium | 251 | 29.3 | 4 | 33.3 | ||
| High | 237 | 27.7 | 4 | 33.3 | ||
| Number of pins | 2 | 430 | 49.9 | 2 | 16.7 | 0.047† |
| 3 | 401 | 46.6 | 10 | 83.3 | ||
| 4 to 5 | 30 | 3.5 | 0 | 0.0 | ||
no previously undocumented neuropathies were newly diagnosed in those patients who were not seen at one week postoperatively
chi-squared test
Fisher’s Exact test
All patients in the delayed follow-up cohort had radiographs obtained at their first postoperative visit which occurred at a mean of 21 days (sd 5) postoperatively. In all, 35 (70%) had their pins pulled at their initial visit, 11 (22%) had their splints overwrapped and four (8%) had their splints removed and replaced with a long-arm cast (Fig. 1).
A total of 26 patients had unscheduled clinic or ED visits postoperatively. There was no difference in the number of unscheduled visits between patients who were seen early and those with delayed first follow-up visits (2.9% versus 4%, p = 0.66, Table 2). Among early follow-up patients who presented for an unscheduled evaluation, 15 patients had cast or splint-related concerns, six were diagnosed with pin site infections and one patient each had an unrelated rash, unrelated fever and constipation. The two patients with delayed first clinic visits had an unscheduled clinic/ER evaluation and both presented for cast/splint related discomfort.
Table 2.
Comparison of patients seen at one week versus those not seen at one week
| Follow-up schedule | |||
|---|---|---|---|
| Delayed first visit | Early first visit | p-value | |
| Mean visits after surgery, n (sd) | 1.9 (0.9) | 3.0 (0.6) | < 0.005* |
| Mean radiographs obtained, n (sd) | 1.7 (0.9) | 2.6 (0.8) | < 0.005* |
| Mean time from OR to pin pull, n (sd) (days) | 24.1 (6.4) | 26.4 (5.5) | 0.006* |
| Mean time from OR to final follow-up, n (sd) (days) | 60.7 (51.1) | 69.2 (35.3) | 0.109* |
| Unscheduled clinic/emergency department visits, n (%) | 2 (4.0) | 24 (2.9) | 0.656† |
| Complications noted postoperatively (after one-week visit), n (%) | 0 (0.0) | 13 (1.6) | > 0.999† |
independent samples t-test
Fisher’s Exact test
The early follow-up visit was not associated with a reduced incidence of postoperative complications (1.6% versus 0%, p > 0.99, Table 2). Overwrapping or exchanging the splint for a cast at the early follow-up visit was not associated with a reduction in unscheduled clinic/ED visits (4.7% in those without versus 2.8% in those with alterations, p = 0.37) nor was splint alteration associated with a reduced incidence of complications (2.3% versus 1.5%, p = 0.48, Table 3).
Table 3.
Comparison of patients with changes to immobilization versus those without changes during the early follow-up visit
| Changes to immobilization? | |||
|---|---|---|---|
| No | Yes | p-value* | |
| Unscheduled clinic/emergency department visits, n (%) | 2 (4.7) | 22 (2.8) | 0.3603 |
| Complications noted postoperatively (after one-week visit), n (%) | 1 (2.3) | 12 (1.5) | 0.5048 |
Fisher’s Exact test
At final follow-up, all patients, independent of postoperative protocol, achieved radiographic union without clinical deformity limiting function. Final mean Baumann’s angle for the entire cohort was 74.5° sd 6.5°, and final mean LHCA for the entire cohort was 40.3° sd 10.3°. There was no correlation between timing of the initial postoperative clinical visit and radiographic parameters. Mean Baumann’s angle in patients seen at one-week postoperatively was 74.5° sd 6.5° compared with 73.7° sd 6.4° in those seen after one-week (p = 0.40). Mean LHCA in patients seen at one-week postoperatively was 40.2° sd 10.4° compared with 41.2° sd 8.8° (p = 0.53).
Discussion
While there is evidence supporting the type and manner of reduction and fixation or paediatric SCF, there is little evidence to support an ideal postoperative clinical and radiographic follow-up protocol.2,3,6,7 As a result, postoperative protocols can vary significantly, even between providers at a single institution.8 This study demonstrates nine fellowship-trained paediatric orthopaedic surgeons utilizing seven distinct protocols at a single institution without any demonstrable reduction in unscheduled clinical/ED visits nor any reduction in complication rates with any singular protocol.
In our review, all 873 patients went onto radiographic union with similar radiographic and satisfactory clinical outcomes regardless of the postoperative protocol. Of over 800 patients seen for early follow-up postoperatively, only eight had changes in management based on clinical findings and one patient had a change in management based off isolated radiographic findings. Furthermore, although 12 new neuropraxias were detected at the early visit, the majority had no changes in treatment and all patients had complete, spontaneous return to normal neurologic function. Neither an early visit nor an alteration to the postoperative splint was found to be associated with a reduction in unscheduled clinic/ED visits or postoperative complications. Given that our results were comparable with previously-published low complication rates with a multitude of treatment protocols, we could not identify one best postoperative practice in terms of complication reduction or clinical outcome.9–12
Our findings are in keeping with what has been previously demonstrated in the literature from smaller series. Ponce et al13 also reviewed 104 patients treated with CRPP with variable postoperative protocols at a single institution. These authors reported no benefit associated with early clinical follow-up in terms of complication rate nor any difference in radiographic outcomes between patients with and without early follow-up. However, this study included only 104 patients total (52 patients per group). Although no significant difference was found in complication rate and radiographic parameters regardless of postoperative follow-up protocol, it is possible that the study was under-powered, given the low rates of postoperative complications among patients who require CRPP for SCF.9,10
Karamitopoulos et al14 reported a high prevalence of one-week postoperative radiographs without a demonstrable influence on clinical management in 643 patients. Likewise, Garg et al15 demonstrated that obtaining radiographs prior to pin pull did not alter clinical management in a series of 389 patients. However, neither of these studies directly compared early to late clinical and radiographic follow-up protocols, and neither reported the effects of interval clinical or radiographic exam on ultimate clinical results.
Karalius et al16 evaluated the utility of obtaining early (seven to ten days postoperative) and late (prior to pin pull) radiographs. These authors concluded that early radiographs were of value, as 1.6% of patients had an alteration in management based on these radiographs, including revision surgery, early pin removal and pin adjustment. There was no discussion as to whether these patients had any clinical finding that may have prompted radiographs and/or alterations in care. In our series, we found that early follow-up resulted in the alteration of management in a similarly small percentage of patients (1%), but in considering clinical findings in addition to radiographic findings, only one patient (0.1%) had his/her care altered based on early radiographs alone which most likely did not influence the clinical outcome.
This study does have limitations. This is a retrospective review of a large series of patients with inherent biases including assignment of patients to groups based on surgeon preference of a postoperative management protocol. This lead to an uneven distribution of patients with fewer patients who had a delayed first clinic visit than those who were seen early (Fig. 1). Despite this disparity, there was no clear trend toward improved outcomes for any singular postoperative protocol. The retrospective nature of the study may also lead to missing or inaccurate data elements; however, significant complications would most likely not have been missed. Finally, each of the surgeons who participated in this study is a fellowship-trained paediatric orthopaedist and takes call at a busy Level 1 paediatric trauma centre. While these results suggest that early radiographs in that asymptomatic patient did not alter treatment, it is possible that the results of this study may be altered if the surgeons managing these patients had less experience.
We cannot retrospectively assign value to the one-week visit in terms of parent satisfaction, patient satisfaction or patient education. Surveys such as the The Child Consumer Assessment of Healthcare Providers & Systems or alternative validated satisfaction measure must be employed to further define the role, if any, of earlier, more frequent postoperative follow-up. We also did not complete a comprehensive cost analysis, which would necessarily include facility fees, the cost of radiographs and cast alterations and splint overwraps and the cost of lost productivity resulting from parents missing work and patients missing school for additional clinic visits. A larger matched cohort study that includes both patient/parent satisfaction data and a comprehensive cost analysis is necessary to determine the specific role of early follow-up after CRPP of closed SCF.
In conclusion, our results suggest that obtaining radiographs at the early follow-up visit in the asymptomatic patient does not alter management or clinical outcome. The one-week visit provides an opportunity for the clinician to make changes in the clinical course but we did not find that this visit altered the overall outcome of the patients in this study. Whether the one-week visit provides enough value to the patient with respect to parent/patient education and satisfaction with care is unclear from this study. Multiple higher volume paediatric trauma surgeons at our institution continue to see patients for early follow-up after CRPP but radiographs at this visit are now being ordered on a case-by-case basis. Each practitioner and family must weigh the theoretical benefits of an additional early clinical postoperative visit with the cost to the family and healthcare system when determining appropriate postoperative management of patients with closed SCF.
Compliance with Ethical Standards
Funding Statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
OA Licence Text
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) license (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Ethical Statement
Ethical approval: This study was approved by our Institutional Review Board (IRB).
Informed consent: Informed consent was obtained at the time of patient enrolment into the prospective database but repeat informed consent was not required by the IRB to utilize information from the database for retrospective review.
ICMJE Conflict of Interest Statement
None of the authors report any conflicts of interest relating to this study.
References
- 1.Houshian S, Mehdi B, Larsen MS. The epidemiology of elbow fracture in children: analysis of 355 fractures, with special reference to supracondylar humerus fractures. J Orthop Sci 2001;6:312–315. [DOI] [PubMed] [Google Scholar]
- 2.Howard A, Mulpuri K, Abel MF, et al. The treatment of pediatric supracondylar humerus fractures. J Am Acad Orthop Surg 2012;20:320–327. [DOI] [PubMed] [Google Scholar]
- 3.Mulpuri K, Hosalkar H, Howard A. AAOS clinical practice guideline: the treatment of pediatric supracondylar humerus fractures. J Am Acad Orthop Surg 2012;20:328–330. [DOI] [PubMed] [Google Scholar]
- 4.Mulpuri K, Wilkins K. The treatment of displaced supracondylar humerus fractures: evidence-based guideline. J Pediatr Orthop 2012;32:S143–S152. [DOI] [PubMed] [Google Scholar]
- 5.Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet 1959;109:145–154. [PubMed] [Google Scholar]
- 6.Kocher MS, Kasser JR, Waters PM, et al. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children. A randomized clinical trial. J Bone Joint Surg [Am] 2007;89-A:706–712. [DOI] [PubMed] [Google Scholar]
- 7.Slobogean BL, Jackman H, Tennant S, Slobogean GP, Mulpuri K. Iatrogenic ulnar nerve injury after the surgical treatment of displaced supracondylar fractures of the humerus: number needed to harm, a systematic review. J Pediatr Orthop 2010;30:430–436. [DOI] [PubMed] [Google Scholar]
- 8.Schlechter JA, Dempewolf M. The utility of radiographs prior to pin removal after operative treatment of supracondylar humerus fractures in children. J Child Orthop 2015;9:303–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bashyal RK, Chu JY, Schoenecker PL, et al. Complications after pinning of supracondylar distal humerus fractures. J Pediatr Orthop 2009;29:704–708. [DOI] [PubMed] [Google Scholar]
- 10.Basques BA, Lukasiewicz AM, Samuel AM, et al. Which pediatric orthopaedic procedures have the greatest risk of adverse outcomes? J Pediatr Orthop 2017;37:429–434. [DOI] [PubMed] [Google Scholar]
- 11.Khoshbin A, Leroux T, Wasserstein D, et al. The epidemiology of paediatric supracondylar fracture fixation: a population-based study. Injury 2014;45:701–708. [DOI] [PubMed] [Google Scholar]
- 12.Guven MF, Kaynak G, Inan M, et al. Results of displaced supracondylar humerus fractures treated with open reduction and internal fixation after a mean 22.4 years of follow-up. J Shoulder Elbow Surg 2015;24:640–646. [DOI] [PubMed] [Google Scholar]
- 13.Ponce BA, Hedequist DJ, Zurakowski D, Atkinson CC, Waters PM. Complications and timing of follow-up after closed reduction and percutaneous pinning of supracondylar humerus fractures: follow-up after percutaneous pinning of supracondylar humerus fractures. J Pediatr Orthop 2004;24:610–614. [DOI] [PubMed] [Google Scholar]
- 14.Karamitopoulos MS, Dean E, Littleton AG, Kruse R. Postoperative radiographs after pinning of supracondylar humerus fractures: are they necessary? J Pediatr Orthop 2012;32:672–674. [DOI] [PubMed] [Google Scholar]
- 15.Garg S, Bloch N, Cyr M, Carry P. Routine radiographs at time of pin removal after closed reduction and percutaneous pinning for type 2 supracondylar humerus fractures do not change management: a retrospective cohort study. J Child Orthop 2016;10:329–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karalius VP, Stanfield J, Ashley P, et al. The utility of routine postoperative radiographs after pinning of pediatric supracondylar humerus fractures. J Pediatr Orthop 2017;37:e309–e312. [DOI] [PubMed] [Google Scholar]


