Abstract:
Purpose
Open reduction and internal fixation with a tension band construct is the standard treatment for displaced transverse intra-articular olecranon fractures. The purpose of this study is to describe the outcomes of tension band fixation of olecranon fractures in children, specifically assessing the need for revision fixation and hardware removal.
Methods
Patients less than 18 years of age diagnosed with a displaced transverse intra-articular olecranon fracture and treated with tension band fixation between 2008 and 2017 were retrospectively enrolled. Operative treatment was with tension band wire (TBW) or tension band suture (TBS) constructs.
Results
A total of 46 patients, 36 male and ten female with a mean age of 12.3 years (6 to 17), were included. Surgical fixation was with TBW in 17 patients and TBS in 29 patients. Revision fixation due to failure and fracture displacement was required in 6% of the TBW group and 14% of the TBS group (p = 0.19). The patients who required revision fixation in the TBS group were older (14.7 years versus 11.6 years, p = 0.05) and heavier (70.5 kg versus 48.5 kg, p = 0.05) than those in the same group who did not require revision fixation.
Conclusion
Paediatric olecranon fractures treated with TBW or TBS fixation unite in the majority of patients with similar need for hardware removal due to prominence and/or pain between fixation techniques. In a select group of older patients weighing greater than 50 kg, TBS constructs demonstrate increased failure rates, requiring revision fixation, and should be avoided in this population group.
Level of Evidence:
IV
Keywords: olecranon fracture, paediatric orthopaedics, tension band, trauma, upper extremity
Introduction
Fractures of the olecranon represent approximately 5% of all elbow fractures in children.1 Displaced intra-articular olecranon fractures are most commonly treated with open reduction and internal fixation. There are multiple strategies for fixation, including plates, compression screws and tension band constructs. Multiple studies in adults have described and compared outcomes of these various fixation strategies2,5–7 and the fracture pattern often dictates the type of fixation.
Tension band fixation is the standard of care for displaced transverse intra-articular fracture of the olecranon. Traditionally, this technique involves fracture reduction followed by the placement of two parallel Kirschner (K)-wires placed through the olecranon and across the fracture site. A transverse hole is drilled in the ulna distal to the fracture site, a steel wire is passed through the bone, and then a figure-of-eight tension band is constructed to incorporate the K-wires.5 Although tension band fixation has been shown to provide articular compression and resist high loads prior to failure, this technique is also associated with painful hardware resulting in implant removal in up to 88% of patients.2 Tension band wires (TBWs) in active children with a thin subcutaneous layer can be especially prominent and painful and necessitate a return trip to the operating room for hardware removal. Substituting braided, nonabsorbable suture for the 18-gauge wire in the tension band construct has grown in popularity and is theorized to potentially be less prominent and painful. Figure 1 illustrates the radiographic appearance of tension band fixation constructs with wire and suture.
Fig. 1.

Tension band constructs with wire (a) and suture (b).
Biomechanical studies have been performed to determine strengths and load to failure of various sutures and wires used in tension band constructs with the goal of determining the ideal fixation strategy for stable osteosynthesis.8–10 Tension band fixation constructs with wire or ultrahigh molecular weight braided polyester suture (FiberWire) were superior with respect to fixation failure as compared with braided polyester suture (Ethibond).9
Aside from a biomechanical study11 and a small case series4 there are no studies of a paediatric population that compare outcomes of olecranon fractures treated with various methods of tension band fixation. The purpose of this study is to describe the outcomes of tension band fixation of olecranon fractures in children and adolescents, specifically assessing the need for additional surgery for hardware removal and/or revision fixation.
Materials and methods
All patients less than 18 years of age diagnosed with a displaced transverse intra-articular olecranon fracture and treated with tension band fixation between January 2008 to May 2017 at a single centre were retrospectively enrolled in this institutional review board-approved study. Patients were identified by International Classification of Disease (ICD)-9 (https://www.cdc.gov/nchs/icd/icd9cm.htm), ICD-10 (https://www.cdc.gov/nchs/icd/icd10cm.htm) and Current Procedural Terminology (CPT) codes. Operative treatment was with a TBW construct or tension band suture (TBS) construct with nonabsorbable braided suture. Fixation construct was based on physician preference. All patients were immobilized with a long-arm cast or splint for two to four weeks post-operatively. Exclusion criteria included patients 18 years of age and older, lack of follow-up to fracture union, surgical fixation with a technique other than tension band with wire or braided suture, olecranon stress fractures and a new or pre-existing diagnosis of osteogenesis imperfecta. Chart review of clinical notes, operative reports and imaging was performed for all patients to determine demographic characteristics, surgical technique and clinical follow-up.
Statistical analyses were performed using SAS 9.3 (2002-2010; SAS, Cary, North Carolina). Descriptive statistics were calculated for study population characteristics, including means and sd for continuous variables (e.g. age, body mass index). Unadjusted comparisons were performed between tension band constructs and failures and non-failures using two-sample t-tests for continuous variables and chi-squared tests for dichotomous or categorical variables. Then, p-values were generated to determine if there was a difference between groups with differences considered to be statistically significant at the 95% level.
Results
In total 46 patients were identified as having displaced transverse intra-articular olecranon fractures treated with open reduction and internal fixation using a tension band construct during the study period. There were 36 boys and ten girls, with a mean age of 12.3 years (6 to 17) Surgical fixation in 17 patients was a tension band construct with K-wires and an 18-gauge stainless steel wire and in 29 patients was a tension band construct with K-wires and FiberWire No 2 or 5 (Arthrex Inc., Naples, Florida). Mean duration of follow-up was 9.1 months (2 to 55). Demographics, follow-up duration and outcomes are described for each treatment cohort in Table 1. Age, weight and follow-up duration were not significantly different between groups.
Table 1.
Demographics and outcome by fixation type
| Wire | Suture | p-value | |
|---|---|---|---|
| Number of patients | 17 | 29 | |
| Age (yrs) | 12.9 | 12.0 | 0.3029 |
| Weight (kg) | 58.6 | 51.6 | 0.2686 |
| Follow-up (mths) | 6.4 | 9.6 | 0.2874 |
| Hardware removal, n (%) | 12 (70.6) | 17 (58.6) | 0.2107 |
| Revision fixation, n (%) | 1 (5.9) | 4 (13.8) | 0.1863 |
| Any return to OR, n (%) | 13 (76.5) | 24 (72.4) | 0.6134 |
p-values were determined as follows: Continuous variables (age, weight, follow-up duration) are a t-test. Categorical variables (yes/no hardware removal, revision fixation, and return to OR) are chi-square tests.
OR, operating room
All olecranon fractures were intra-articular and indicated for surgery based on 2 mm or greater displacement on initial injury radiographs or increasing displacement on follow-up imaging. Mean time from injury to surgery was four days (0 to 32).
Five children sustained additional ipsilateral upper extremity fractures at the time of their injury, including four radial neck fractures and one distal radius fracture. Aside from closed reduction and immobilization dictated by the olecranon fracture, none of these additional fractures required additional operative treatment.
Mean follow-up was 6.4 months (2 to 13) in the TBW group and 9.6 months (2 to 55) in the TBS group (p = 0.29). Hardware removal was performed in 12 patients with TBW (71%) and 17 patients with TBS (59%) (p = 0.21). Mean time from surgery to hardware removal was 6.1 months (3 to 12) in the TBW group and 6.4 months (3 to 12) in the TBS group, (p = 0.65). In all, 41 of 46 patients (89%) had union of their fracture following their initial surgery.
Revision fixation due to failure and fracture displacement occurred in one patient in the TBW group (6%) and four patients in the TBS group (14%) (p = 0.19). Average time from initial surgery to revision was 23 days (7 to 37). The patient with failure of their TBW construct was revised to a plate and screw construct and went on to union. The patients with failed TBS constructs were revised with various techniques including another TBS construct (one), TBW construct (one), plate and screw construct (one) and single screw (one). The patient revised with the single intramedullary screw had increasing fracture displacement necessitating a second revision with a plate and screw construct 17 days following his first revision. All patients went on to union following their revision. Figure 2 includes representative images of a patient with TBS fixation that failed and required revision fixation.
Fig. 2.
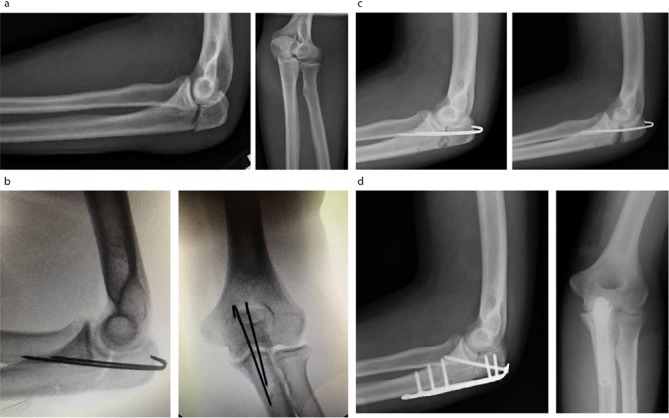
A 16-year-old male patient who sustained an olecranon fracture after jumping out of a car (a). The patient underwent tension band fixation with suture five days post-injury (b). At two weeks and six weeks post-operatively, there is increasing displacement at the fracture site without evidence for healing (c). The patient underwent revision fixation with a plate eight weeks after his initial surgery (d).
The four patients who required revision fixation in the TBS group were older (mean 14.7 years versus 11.6 years (6 to 16), p = 0.05) and heavier (mean 70.5 kg versus 48.5 kg (22 to 100), p = 0.05) than those in the same group who did not require revision fixation. This difference between groups is depicted in Table 2. There was a total of 26 patients with weight greater than 50 kg, 13 with TBW and 13 with TBS. The rate of failure among patients greater than 50 kg was 8% with TBW and 31% with TBS (p = 0.15).
Table 2.
Comparison of revised versus non-revised tension band with suture constructs
| Revised | Non-revised | p-value | |
|---|---|---|---|
| Number of patients | 4 | 25 | |
| Mean age (yrs) | 14.7 (12 to 16) | 11.6 (6 to 16) | 0.0535 |
| Mean weight (kg) | 70.5 (53 to 98) | 48.5 (22 to 100) | 0.0473 |
p-values were determined by t-test.
Discussion
Tension band fixation of displaced transverse intra-articular olecranon fractures in children and adolescents, including both TBW and TBS constructs, produces good outcomes with union occurring in nearly 90% of fractures with a single surgical procedure. However, within a subgroup of patients with TBS constructs, weight greater than 50 kg was predictive of failure and need for revision fixation. All olecranon fractures in patients less than 50 kg went on to successful union with a single surgical procedure.
With regards to failure of fixation, cadaveric studies have shown suture materials to have variable loads to failure and ability to maintain fracture compression as compared with stainless steel wires. Lalliss and Branstetter9 performed cyclic loading to simulated olecranon fractures repaired with wire, No 5 Ethibond and No 2 FiberWire. Ethibond demonstrated separation across the osteotomy but the stainless steel wire and FiberWire both showed no evidence of failure. In a similar study performed with 18-gauge stainless steel wire and No 2 Vicryl suture, suture had equal fracture displacement with low-loads, but had significantly greater displacement at high-loads as compared to wire.3 Residual compression at the articular surface was also noted to be greater with wire as compared with suture. Lastly, Harrell et al10 performed a biomechanical comparison of tension band constructs with either 18-gauge stainless steel wire, Mersilene tape or Ethibond suture, and found that the stiffness and load at failure of a single loop of Ethibond was significantly less than that of both Mersilene tape and stainless steel wire.10
Together, these studies suggest that TBS constructs may be appropriate in patients who generate lower loads across their olecranon fixation. However, in patients placing higher loads across their repair of an intra-articular injury requiring rigid fixation, a TBS construct may not be sufficient. We believe that these biomechanical loads translate to patient size, with larger patients generating greater loads across the fracture. The results of our study are thus in agreement with these biomechanical studies, with children heavier than 50 kg having higher rates of fixation failure with TBS constructs as compared with lighter patients.
The initial strategy behind TBS fixation rather than wire was to minimize pain due to hardware prominence, yet in our study we found no difference in the occurrence for hardware removal between these two forms of fixation. Since the K-wires are the common denominator of both constructs, we believe that they are the source of the pain rather than the 18-gauge wire. The rate of hardware removal in our paediatric series (63%) is notably higher than those published in the adult literature which range from 6% to 25%.11,12 The reasons for this are likely multifactorial, including a thin subcutaneous layer that makes hardware more prominent, increased activity levels and surgeon and/or parent preference for hardware removal. We recommend that physicians counsel patients and their families regarding the potential of hardware pain and prominence necessitating hardware removal, regardless of whether a wire or suture tension band construct is selected. Suture constructs should not be chosen over wire constructs with the anticipation that this will reduce the need for hardware removal.
There are several limitations of our study that relate to the retrospective study design. Several orthopaedic surgeons provided care to the 46 patients, resulting in some heterogeneity of fixation constructs. Hardware removal is a difficult variable to assess in a retrospective manner, as there were no set requirements that dictated need for removal. Individual surgeons may provide different guidance to patients and their families regarding need for and timing of hardware removal, some recommending removal only if painful and others recommending routine removal of hardware after fracture union. That said, we cannot conclude based on our study outcomes that TBS fixation is correlated with any less frequent need for hardware removal than TBW fixation. Finally, follow-up as short as two months in some patients may limit our ability to capture painful hardware requiring removal. Despite short follow-up in some patients, all patients had radiographic union at the time of final follow-up. For this reason, we do not feel that the most important outcome of our study – the need for revision fixation – was affected by this short follow-up in those patients. The assessment of long-term outcomes was not a goal of our study, and thus longer-term follow-up was not necessary. However, the good results of initial tension band fixation of displaced intra-articular olecranon fractures have been described to be durable in the long term.2
In conclusion, our series of 46 children and adolescents treated with tension band fixation for displaced transverse intra-articular olecranon fractures suggests that good outcomes with high rates of union can be expected with both wire and suture fixation. Overall, we found no direct benefits of tension band suture fixation versus wire fixation and therefore do not feel it has a role in the treatment of olecranon fractures. Tension band fixation with suture resulted in no fewer returns to the operating room for hardware removal than did tension band fixation with wire, and thus suture fixation should not be selected for this benefit. Weight greater than 50 kg was a predictor of failure of tension band fixation with suture, so we advocate that larger patients should be treated with a tension band construct with wire as opposed to suture.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
OA Licence Text
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) license (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Ethical statement
Ethical approval: This research involves a retrospective chart review of human subjects. Approval was obtained from our institutional review board.
Informed consent: Informed consent was not obtained due to the retrospective nature of the study.
ICMJE Conflict of interest statement
None of the authors declare any conflict of interest relevant to this study.
References
- 1.Rockwood CA, Wilkins KE, Beaty JH, et al. Fractures in Children. Philadelphia: Lippincott-Raven, 1996. [Google Scholar]
- 2.Flinterman HJ, Doornberg JN, Guitton TG, et al. Long-term outcome of displaced, transverse, noncomminuted olecranon fractures. Clin Orthop Relat Res 2014;472:1955–1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parent S, Wedemeyer M, Mahar AT, et al. Displaced olecranon fractures in children: a biomechanical analysis of fixation methods. J Pediatr Orthop 2008;28:147–151. [DOI] [PubMed] [Google Scholar]
- 4.Gortzak Y, Mercado E, Atar D, Weisel Y. Pediatric olecranon fractures: open reduction and internal fixation with removable Kirschner wires and absorbable sutures. J Pediatr Orthop 2006;26:39–42. [DOI] [PubMed] [Google Scholar]
- 5.Wilkerson JA, Rosenwasser MP. Surgical techniques of olecranon fractures. J Hand Surg Am 2014;39:1606–1614. [DOI] [PubMed] [Google Scholar]
- 6.Wilson J, Bajwa A, Kamath V, Rangan A. Biomechanical comparison of interfragmentary compression in transverse fractures of the olecranon. J Bone Joint Surg [Br] 2011;93-B:245–250. [DOI] [PubMed] [Google Scholar]
- 7.Matar HE, Ali AA, Buckley S, Garlick NI, Atkinson HD. Surgical interventions for treating fractures of the olecranon in adults. Cochrane Database Syst Rev 2014;26:CD010144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sadri H, Stern R, Singh M, et al. Transverse fractures of the olecranon: a biomechanical comparison of three fixation techniques. Arch Orthop Trauma Surg 2011;131:131–138. [DOI] [PubMed] [Google Scholar]
- 9.Lalliss SJ, Branstetter JG. The use of three types of suture and stainless steel wire tension banding for the fixation of simulated olecranon fractures: a comparison study in cadaver elbows. J Bone Joint Surg [Br] 2010;92-B:315–319. [DOI] [PubMed] [Google Scholar]
- 10.Harrell RM, Tong J, Weinhold PS, Dahners LE. Comparison of the mechanical properties of different tension band materials and suture techniques. J Orthop Trauma 2003;17:119–122. [DOI] [PubMed] [Google Scholar]
- 11.Claessen FM, Braun Y, Peters RM, et al. Factors associated with reoperation after fixation of displaced olecranon fractures. Clin Orthop Relat Res 2016;474:193–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Snoddy MC, Lang MF, An TJ, et al. Olecranon fractures: factors influencing re-operation. Int Orthop 2014;38:1711–1716. [DOI] [PMC free article] [PubMed] [Google Scholar]


