Abstract:
Purpose
Intramedullary lengthening nails are an accepted alternative to external fixators but are limited by anatomical preconditions. Therefore, to date the use of external fixators is sometimes inevitable. We report on a new technique for correction of combined limb length discrepancies and complex axis deformities using solely internal devices - a lengthening nail and a locking plate.
Methods
Between October 2008 and November 2011 five patients (two femora, three tibias) with a mean leg length discrepancy of 36 mm (25 to 50) and a complex angular deformity were treated with a fully implantable motorized lengthening nail (Fitbone) and a locking plate. All patients were evaluated with regards to the pre- and postoperative leg length as well as axis alignment, functional outcome, lengthening indices and complications.
Results
A successful leg length equalization was achieved in all cases and physiological joint orientation angles in all but one case. The mean distraction index was 1.2 mm/day, the maturation index 24 days/cm and the consolidation index 35 days/cm. The functional outcome was very encouraging in all cases with bilateral free range of movement. In total, two complications were observed, one nonunion and one loss of leg length after an early locking bolt removal in a peripheral hospital.
Conclusion
The combination of a fully implantable motorized lengthening nail and a locking plate is a valuable alternative option for treating selected cases with limb length discrepancies in combination with a complex deformity of the lower leg. However, the reported technique puts high demands on the preoperative planning, operative technique as well as surgeon’s skills.
Level of evidence
IV (retrospective series)
Keywords: mechanical axis, axis deformity, leg lengthening, intramedullary nailing, fitbone
Introduction
In the last two decades intramedullary limb lengthening has become a valuable alternative to external fixators.1-8 Unlike the application of external systems, however, solid intramedullary nails require certain anatomical preconditions (e.g. adequate medullar dimensions, lack of marked angular deformities/multilevel deformities, etc) which have to be met and taken into consideration both during the preoperative planning and intraoperatively.4,9 Therefore, to date, limb length discrepancies with complex angular deviations such as multilevel deformities have usually been treated using external fixators and/or multiple surgeries. Despite technical modifications and advancement of external devices, complications such as pin tract infections, transfixation of muscles and pain are still commonly reported.10-13 Hexapod fixators facilitate deformity corrections with simultaneous leg lengthening,14-16 but long treatment times are – beside the above-mentioned fixator associated complications – still an issue.10,13 A combination of an intramedullary nail and a temporary external fixator has been shown to reduce treatment time as well as complication rates significantly, but addressing complex deformities remains challenging.17-19
The effectiveness of limb lengthening with fully implantable motorized lengthening nails has previously been shown.4,5,20 Simultaneous deformity correction, however, is required in almost all cases (as lengthening is performed along the anatomical axis) and is, therefore, an integral part of using this technique. Thus, in cases with multi-level deformities or deformities in close proximity to the joint line, lengthening can not be carried out using an intramedullary lengthening nail unless an additional osteotomy is performed.
We report on a preliminary case series of five patients with leg length discrepancies and concomitant complex axis deformities who were treated with a new technique, comprising a double osteotomy and solely internal fixation using a lengthening nail and a locking plate.
Patients and methods
In total five female patients with a mean age of 13.2 years (11 to 15) who were treated between October 2008 and November 2011 for a combined limb length discrepancy and complex axis deformity were included in this retrospective study. The mean leg length discrepancy was 36 mm (25 to 50), the mean follow-up 31 months (16 to 53). In all patients a double osteotomy was performed. The fully implantable motorized lengthening nail Fitbone (three antegrade tibia nails and two retrograde femoral nails; Wittenstein Intens GmbH, Igersheim, Germany) was used in combination with a locking plate (for fixation of the second osteotomy) in all patients (Table 1).
Table 1.
Patient characteristics and used implants
| Case | Age (yrs) | Location | Side | Aetiology | Correction at first osteotomy (nail) | Nail type | Correction at second osteotomy (plate) | Additional implant (plate) | Complication(s) | Follow-up (mths) | Time to nail removal (mths) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 11.0 | Tibia | L | Blount‘s disease | Legthening-varisation osteotomy (open wedge) proximal tibia | Antegrade tibial TAA 1160 | Valgization osteotomy (opening wedge) proximal tibia | Tomofix plate, (DePuy-Synthes, Warsaw, Indiana) | None | 25 | 23 |
| 2 | 11.5 | Tibia | R | Osteomyelitis | Legthening-varisation osteotomy (open wedge) proximal tibia | Antegrade tibial TAA 1160 | Valgization osteotomy (closing wedge) proximal tibia | HTO-plate, (Königsee, Allendorf, Germany) | None | 53 | 47 |
| 3 | 12.3 | Tibia | R | Multiple hereditary exostosis | Legthening-valgization osteotomy (open wedge) proximal tibia | Antegrade tibial TAA 1160 | Varisation osteotomy (closing wedge) distal tibia | 3.5 LCP paediatric condylar plate, (DePuy-Synthes, Warsaw, Indiana) | Loss of length due to early screw removal; revision surgery and re-lengthening | 21 | 14 |
| 4 | 15.4 | Femur | L | Congenital femoral deficiency | Legthening-varisation osteotomy (open wedge) distal femur | Retrograde femoral TAA 1180 | Valgization osteotomy (dome) midshaft | 4,5/5 LCP plate (DePuy-Synthes, Oberndorf, Switzerland) | None | 16 | 8 |
| 5 | 14.9 | Femur | L | Perinatal epiphysiolysis (distal femur) | Legthening-valgization osteotomy (open wedge) distal femur | Retrograde femoral TAA 1040-4 | Varisation-extension osteotomy (closing wedge) midshaft | 4.5/5 LCP Plate (DePuy-Synthes, Warsaw, Indiana) | Nonunion; first revision with exchange nailing, second revision with bone grafting and plating | 40 | 17* |
exchange nailing for revision of femoral pseudarthrosis
TAA, Telescope Active Actuator; HTO, High Tibial Osteotomy; LCP, Locking Compression Plate
Among the tibial deformities (Table 1) were two double deformities comprising a proximal tibial varus-deformity and a diaphyseal valgus-deformity caused by a premature ossification of the medial aspect of the proximal tibial growth plate (Blount’s disease) in one patient (case 1, Fig. 1) and a neonatal osteomyelitis (case 2). The third patient presented with a proximal varus-deformity as well as a distal tibial valgus-deformity due to multiple osteochondromas. Correction of the proximal tibial varus in cases 1 and 2 was accomplished with an open wedge valgization-osteotomy (Table 1) and the diphyseal valgus deformity with a varisation-osteotomy (Fig. 1). In case 3 an additional closing wedge varisation-osteotomy was performed to correct the distal tibial valgus.
Fig. 1.
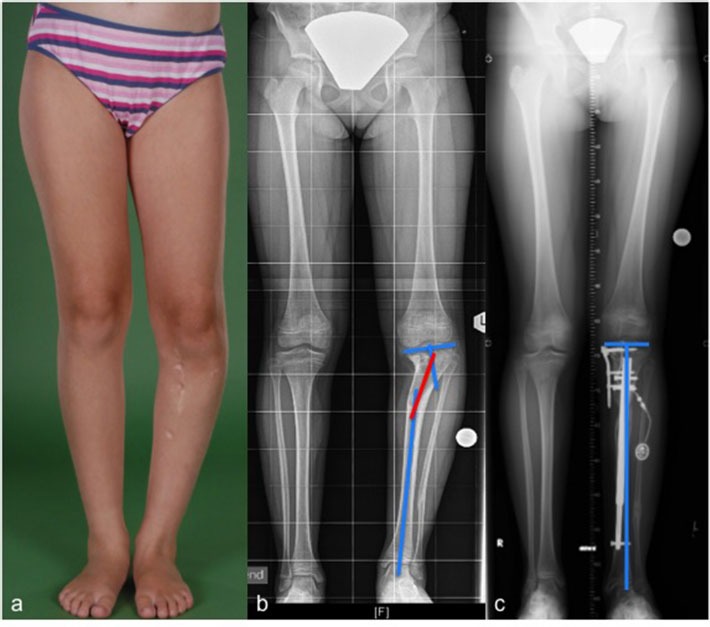
Preoperative imaging of an 11-year-old patient (case 1) with a leg length discrepancy of 25 mm as well as a proximal tibial varus- and a diaphyseal valgus-deformity of the left tibia following treatment of Blount’s disease (a, b). A proximal valgization-osteotomy as well as a lengthening-varisation-osteotomy was performed to achieve equal limb lengths as well as physiologic joint orientation angles (c).
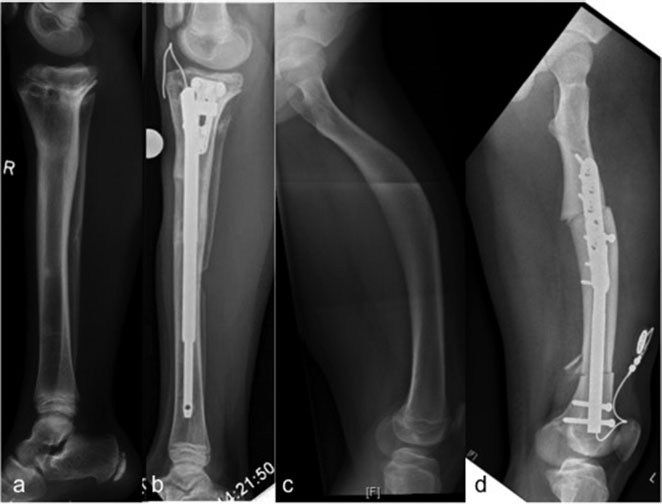
The femoral deformities included a combined varus- and valgus-deformity (case 4, Fig. 2) caused by a congenital femoral deficiency (Pappas VII) as well as a combined varus-, valgus- and (40°) flexion-deformity due to a perinatal distal femoral epiphysiolysis (case 5). In one patient (case 4) correction was achieved by performing a distal lengthening-varus-osteotomy and an additional proximal valgus-osteotomy (Fig. 2). In the other patient (case 5), a distal lengthening-valgization-osteotomy as well as an additional proximal extension-varisation-osteotomy was perfomed (Table 1).
Fig. 2.
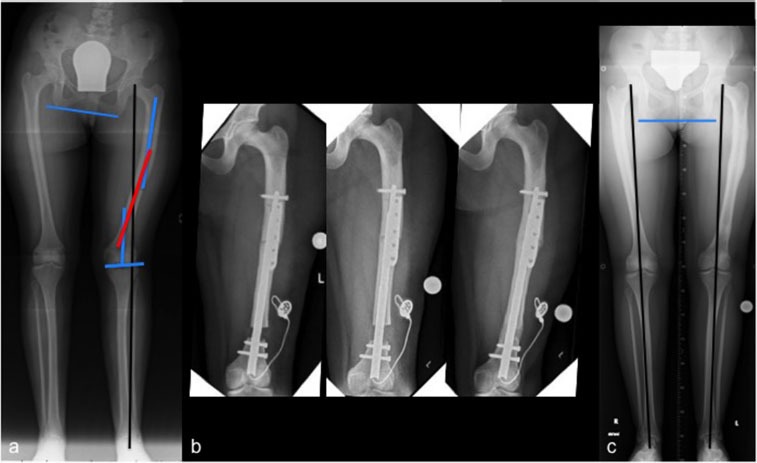
Combined metaphyseal valgus- and diaphyseal varus-deformity of the left femur in a 15-year-old patient (case 4) with a congenital femoral deficiency and a limb length discrepancy of 25 mm (a). Deformity correction was performed by means of a double osteotomy and gradual lengthening of the left femur (b, c). Implant removal was performed eight months after the initial operation with equal limb lengths and physiologic axis alignment despite the persisting slight varus-deformity of the femoral diaphysis (c).
Two patients in the tibial group underwent previous surgeries, including proximal tibial osteotomies as well as an epiphysiolysis with interposition of fat-graft (case 1) or costal cartilage (case 2). In case 2 a tibial hemiepiphysiodesis had previously been performed, too. No patient in the femoral group had previous surgeries.
In two patients with premature (open) growth plates on the contralateral side (case 1 and 2), the remaining growth as well as the expected leg length discrepancy at maturity were calculated preoperatively using the multiplier method.21 In one patient (case 1) an over-lengthening was performed according to the estimated final leg length discrepancy at maturity (Table 2). In the other patient (case 2) the leg length discrepancy at maturity was calculated to be 8 cm (5 cm at the time of surgery, Table 2). Since the used lengthening nail is restricted to a maximum stroke of 6 cm at the tibia, a lengthening of 5 cm (leg length discrepancy at the time of surgery) was conducted and the implant exchanged after skeletal maturity. After the second lengthening procedure equal limb lengths were achieved.
Table 2.
Length gained and lengthening indices
| Case | LLD at presentation (mm) | Planned gain of length (mm) | Achieved length (mm) | Distraction-index (mm/day) | Maturation index (days/cm) | Consolidation index (days/cm) |
|---|---|---|---|---|---|---|
| 1 | 25 | 45* | 40 | 1.0 | 28 | 40 |
| 2 | 50 | 50 | 54 | 1.1 | 11 | 22 |
| 3 | 40 | 40 | 36 | 1.1 | 33 | 44 |
| 4 | 25 | 25 | 28 | 1.4 | 22 | 32 |
| 5 | 40 | 40 | 41 | 1.0 | N/A† | N/A† |
| Mean | 36 | 40 | 40 | 1.2 | 24 | 35 |
patient with open growthplates. The final leg length discrepancy (LLD) at maturity was calculated using the multiplier method
patient with a nonunion of the lengthening osteotomy
The reverse planning method as well as the surgical technique for leg lengthening and deformity correction using the Fitbone nail have been previously described.4,5,22,23
Preoperative planning
The preoperative range of movement of both legs was assessed and leg length discrepancies, mechanical axis deviations and joint orientation angles were measured on standardized long standing radiographs using the TraumaCad software (BrainLAB, Feldkirchen, Germany).24 Additionally, the center of rotation and angulation (CORA) of each deformity was defined and reverse planning performed, in which all deformities were taken into consideration.23,24 Our aim was to restore physiological joint orientation angles and/or symmetrical bilateral axis alignments (Fig. 3a) by using a lengthening nail (retrograde in femoral corrections, antegrade in tibial corrections) and a plate.
Fig. 3.
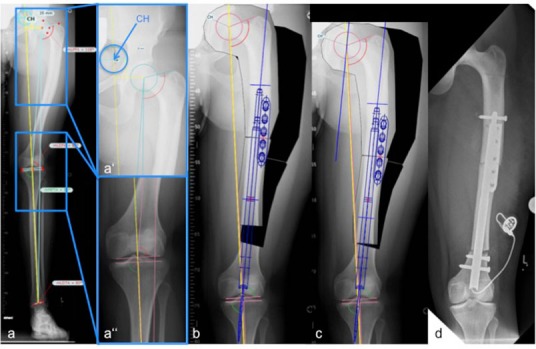
Coronal plane correction planning for case 4. A vertical line was drawn representing the aimed mechanical axis alignment (a). Insert a’ shows the desired endpoint (CH = final position of the centre of the femoral head in femoral corrections) and insert a’’shows the aimed axis alignment after correction (yellow line). After planning the second osteotomy, the diaphyseal segment was cut out and the centre of the femoral head placed onto the aimed endpoint CH (b). The nail end lies in extension of the femoral notch (b). In a ‘reverse’ step, the diaphyseal segment was shifted distally along the axis of the intramedullary nail, with the femoral head lying on postoperative (temporary) endpoint CH’ (c). The postoperative radiograph shows an acceptable result after acute deformity correction and nail implantation (d).
In brief, a vertical line representing the aimed mechanical axis alignment (Fig. 3a) was drawn and the desired endpoint on that line (final position of the centre of the femoral head in femoral corrections, centre of the ankle joint in tibial corrections) defined.23 In a first step, the second osteotomy (proximal tibial osteotomy in cases 1 and 2, distal tibial osteotomy in case 3, diaphyseal femoral osteotomy in cases 4 and 5) was templated using the CORA method.24 A closing wedge osteotomy was planned in three patients (cases 2, 3 and 5), an opening wedge osteotomy in one patient (case 1) and a dome osteotomy in another patient (case 4). An appropriate osteotomy level for the lengthening osteotomy was then chosen, which – when using the Fitbone nail – is recommended to be 8 cm to 11 cm away from the joint line. Afterwards, the anatomic axis of the diaphyseal segment (proximal segment in femoral corrections, distal segment in tibial corrections) was determined and the nail template placed along this axis. The diaphyseal segment (including the nail) was then cut out and the centre of the femoral head/centre of the ankle joint placed onto the desired endpoint (on the aimed alignment line, see above) (Fig. 3b). Additionally, a position of the diaphyseal segment was chosen in which, a) the protruding nail entered the other segment (distal segment in femoral corrections, proximal segment in tibial correction) at the level of the osteotomy, and b) the nail end lay in extension of the femoral notch (Fig. 3b). In accordance with the principles of the reverse planning, the diaphyseal segment was then shifted distally to the level of the osteotomy along the axis of the intramedullary nail (Fig. 3c). Thus, the lengthening procedure was schematically reversed and the corresponding position of both segments relative to one another identified (Figs 3c and 3d). Lateral radiographs were used to analyze deformities in the sagittal plane as well as to anticipate potential obstacles when reaming the medullary canal with straight rigid reamers (e.g. marked femoral bowing) (Fig. 4).
Fig. 4.
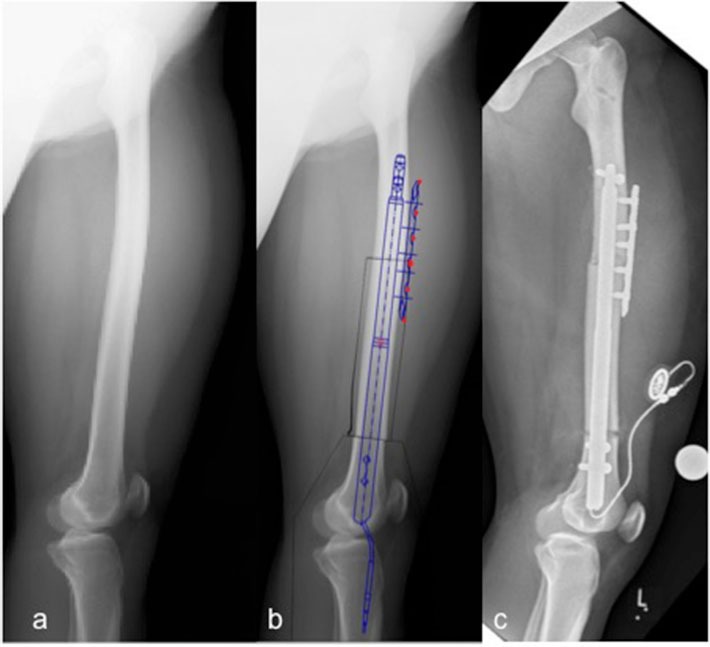
Preoperative lateral femur radiograph of a patient with a congenital femoral deficiency (case 4) (a). A lateral planning was performed for sagittal plane deformity analysis and anticipating potential obstacles when reaming the medullary canal with straight rigid reamers (b). The planning was then meticulously implemented intraoperatively (c).
Intraoperative implementation
Reaming the medullary canal with straight rigid reamers, which do not follow the line of least resistance, serves as one of the key steps in deformity correction using intramedullary nails.9,23 Therefore, the affected bone segment needs to be ‘straightened’ (via the second osteotomy) in order to allow the use of straight rigid reamers. As a rule of thumb, the second osteotomy should be performed first, if its osteotomy level (CORA) is closer to the nail entry point than the level of the lengthening osteotomy and vice versa. Consequently, the valgus osteotomies in case 1 and 2 (CORA close to the joint line) were performed first, while in cases 3, 4 and 5 the additional osteotomies were carried out second (CORA afar from the nail entry point). If the medullary canal is simultaneously reamed across the second osteotomy (via the separate transpatellar approach), the straight reamers can be used for temporary stabilization of the osteotomy while the plate is applied in its final position.
In proximal tibia corrections (cases 1 and 2), the plate should be positioned posteriorly in order to avoid locking interferences (due to over-crowding) between the lengthening nail and the plate (Figs 5a and 5b). In femoral corrections, the plate can be positioned either laterally (Figs 5c and 5d) or anterolaterally (Figs 4b and 4c) using monocortical or diverging bicortical screws, respectively. The ideal plate size and position as well as its fixation (monocortical versus bicortical) – which depends on anatomical preconditions of the affected bone segment such as cortical thickness etc. – should be considered preoperatively. The plates used in our collective are displayed in Table 1. Jamming the plate/screws and the lengthening nail should be omitted in order to avoid a potential blocking of the lengthening mechanism. The Fitbone system includes two standard nails: the Telescope Active Actuator (TAA) 1180 (lengths 245 mm, stroke 80 mm, diaphyseal diameter 11 mm) for femoral corrections and the TAA 1160 (length 225 mm, stroke 60 mm, diaphyseal diameter 11mm, available with or without Herzog curve) for tibial corrections. The medullary canal is reamed up to a diameter of 11 mm and the final preparation carried out using a special step reamer (11 mm and 12 mm) which mirrors the dimensions of the used Fitbone nail. However, implants of different lengths/diameters and even custom-made implants are available on request. In one patient (case 5) a TAA 1040 (length 260 mm, stroke 40 mm, diaphyseal diameter 10 mm) was used in order to bridge the second osteotomy more efficiently and to match the dimensions of the medullary canal in this patient. After preparation of the medullary canal, a trial nail (dummy) is inserted and the axis alignment confirmed under image intensifier using a grid plate. If the achieved correction is deemed satisfactory, the final lengthening nail is implanted and locked using a drill guide (locking jig) at its bottom end and freehand using a radiolucent right-angle gear-hard at the nail tip. All operations were performed by the senior author (AHK).
Fig. 5.
In cases with a second osteotomy of the proximal tibia, the plate was positioned posteriorly in order to avoid locking interferences between the lengthening nail and the locking plate (a, b). In femoral corrections, the plate was positioned either laterally (c, d) or anterolaterally using monocortical or diverging bicortical screws.
Distraction was commenced seven days postoperatively in femoral lengthenings and eight to nine days postoperatively in tibial corrections. Radiographic follow-ups were performed every two weeks during the distraction phase and every four weeks during the consolidation phase. The initial distraction rate was 1.0 mm per day for all patients, but adjustments were made according to the individual regenerate formation. Consolidation was defined as corticalization of at least three sides of the callus on biplane radiographs with subsequent transition to full weight bearing. Nonunion was defined as lack of consolidation after a period of more than three times the length of the distraction period at the femur and more than four times at the tibia. The distraction-, maturation-, and consolidation indices were calculated as previously described.4
Leg lengthening was considered successful in cases with a residual leg length discrepancy of 5 mm or less. An effective deformity correction was assumed in all cases in which either the measured postoperative joint orientation angles were within the physiological range or in which equal mechanical axis alignments were achieved bilaterally.24 Additionally, all complications were recorded and the functional outcome evaluated with respect to the range of movement of the hip, knee and ankle joint.
Results
The preoperative lengthening plan was accomplished in all cases resulting in equalized leg lengths (Table 2).
The mean distraction time was 35 days (19 to 49) with a mean lengthening distance of 40 mm (28 to 54) (Table 2). The distraction, maturation and consolidation indices are listed in Table 2.
Deformity correction was achieved in all but one case (case 3, Table 3), resulting in physiological joint orientation angles such as the mechanical lateral distal femoral angle or the medial proximal tibial angle or the lateral distal tibial angle of the affected bone. Pre- and postoperative data are listed in Table 3.
Table 3.
Mechanical axis deviation (MAD) as well as pre- and postoperative joint orientation angles of the affected bone. In all but one patient (LDTA in case 3) physiological joint orientation angles were achieved
| Case | MAD (mm) preop. | MAD (mm) postop. | mLDFA (°) preop. | mLDFA (°) postop. | MPTA (°) preop. | MPTA (°) postop. | LDTA (°) preop. | LDTA (°) postop. |
|---|---|---|---|---|---|---|---|---|
| 1 | (+) 33 | (-) 7 | 75 | 87 | 90 | 88 | ||
| 2 | (+) 6 | (-) 3 | 82 | 88 | 86 | 90 | ||
| 3 | (-) 15 | (-) 10 | 90 | 89 | 69 | 83 | ||
| 4 | (-) 19 | 0 | 82 | 90 | ||||
| 5 | (-) 13 | (-) 7 | 85 | 90 | ||||
| mean | 17 | 5 | 85 | 90 | 82 | 88 | 82 | 87 |
(+) indicates an axis deviation to the medial side, (-) a deviation to the lateral side
preop., preoperative; postop., postoperative; mLDFA, mechanical lateral distal femoral angle; MPTA, medial proximal tibial angle
The functional outcome was very encouraging in all cases with bilateral free range of movement of the hip, knee and ankle joints at the latest follow-up.
No complications occurred during the initial postoperative phase or the distraction period. In four cases (cases 1, 2, 3 and 4) primary consolidation was achieved within the previewed timeframe. An insufficient bone regenerate was recorded in one patient (case 5). Despite the lack of pain or functional deficits, the lengthening nail was removed and a solid intramedullary nail inserted 17 months after the initial procedure. After revision surgery, slow healing in terms of a progressive bone regenerate was observed but consolidation was not achieved after another ten months. Therefore, an open debridement, bone grafting and stabilization with an angle-stable distal femur plate was performed resulting in bony consolidation after one year. A second complication was encountered in a patient with a tibial correction, in whom the distal locking bolt was removed (for dynamization) six weeks after the end of the distraction phase in a peripheral hospital (case 3). The radiological assessment at presentation in our hospital revealed a loss of distraction length of 2 cm. As the regenerate was still premature at this time, a distal locking screw was reinserted and the lengthening process recommenced. Equal leg lengths were achieved after 21 days of distraction and no further complications were encountered until full consolidation.
Discussion
We report on five patients with leg length discrepancies in combination with complex axis deformities, who were treated with a double osteotomy and internal fixation systems exclusively – an intramedullary lengthening nail and a locking plate. At the latest follow-up, all patients had equal leg lengths (± 5 mm) and all but one patient physiological joint orientation angles. The mean distraction index was 1.2 mm/day, the maturation index 24 days/cm and the consolidation index 35 days/cm. In total two complications were observed, but only one was treatment related.
To date, the prevailing treatment tools for leg length discrepancies with simultaneous complex axis deformities are external fixation devices. One of the major advantages of external devices, and in particular hexapod systems, is the possibility to perform subsequent, even computer-assisted adjustments postoperatively. One of the most frequently encountered problems using external fixators, however, are pin tract infections, wire breakages, muscle transfixation and secondary fractures.13 Intramedullary nails, in contrast, have been shown to have a significantly lower complication rate compared with external devices and offer advantages such as an improved patient comfort as well as a significantly reduced treatment time.4,5,22 Thus, external fixators have been incrementally replaced by intramedullary nails for limb lengthening procedures especially in adolescents and adults.3,6,25,26 Intramedullary nails do not offer the option of postoperative corrections and their use is subject to anatomical preconditions.9 Consequently, a meticulous preoperative planning and intraoperative implementation (of the planned implant position and axis alignment) are of utmost importance. Thanks to advances in the implant design, development of special instruments and the launch of new devices, the indications for intramedullary lengthening nails have broadened over the last decade, whereas even 3D deformity corrections can be performed. Anatomical conditions such as a CORA close to the joint line, a short bone length, multilevel deformities or a long sectional bending of the affected bone, however, still limit the use of intramedullary lengthening nails.9 A staged approach with deformity correction (first step) and a subsequent intramedullary lengthening procedure (second step) can be performed in order to overcome this problem, but multiple surgeries as well as a rather long treatment time might be required. Therefore, hybrid techniques, which simultaneously combine external fixators with nails or plates have been described for limb lengthening as well as deformity corrections and were found to reduce typical fixator-associated complications and/or the ‘time in the frame’.17,18,27,28 However, deep infections of the medullary canal or secondary deformities/fractures are ongoing concerns. Rozbruch et al28 introduced a technique that involved lengthening and then nailing, in which a frame is used for the gradual distraction and then in a second operation, a reamed intramedullary nail is used for the stabilization during the consolidation phase. Alternatively, the external fixator can solely be used in the operating room for correcting the deformity and restoring the axis alignment, whereas an intramedullary lengthening nail is then inserted to hold the position and gradually equalize the limb length discrepancy.29 In our cases with femoral deformity corrections (case 4 and 5), a further option might have been performing an acute correction of the distal femur (with plate fixation) in combination with a proximal (subtrochanteric) lengthening osteotomy and antegrade nailing, too. As lengthening over a straight intramedullary nail occurs along the nail axis, which typically approaches the anatomic axis of the affected bone, changes of the mechanical axis are inevitable during the lengthening process (e.g. a certain degree of valgization in antegrade and retrograde femoral lengthening) and have to be considered preoperatively.9,23 Antegrade nailing, however, is limited by its low capacity to perform axis corrections and – if using a trochanteric entry – the risk of producing a varus deformity of the proximal femur. We, therefore, prefer retrograde nailing as well as the concept of reverse planning, in which all deformity corrections are meticulously planned preoperatively and implemented intraoperatively.23 In cases with multi-level deformities or deformities in close proximity to the joint line, however, an additional (second) osteotomy is indispensable. To our knowledge, this is the first report on leg lengthening and deformity correction using a double osteotomy and solely internal fixation systems – an intramedullary lengthening nail and a locking plate.
Leg lengthening with the fully implantable motorized lengthening nail Fitbone has been shown to have a low complication rate.4 In the current study two complications were recorded, but one (case 3) was caused by an unplanned surgical intervention in a peripheral hospital (early nail dynamization by removal of a locking bolt). In the other patient (case 5) a nonunion was encountered, which required surgical intervention. A correlation between the occurrence of this complication and the used technique cannot be completely ruled out, as the combination of a nail and a plate might compromise the blood supply of both the peri- and endosteum and hence provoke delayed union/nonunion. Nevertheless, as the proximal (second) osteotomy, which healed per primam, was a considerable distance apart from the distal lengthening osteotomy and in a different femoral bone segment (with a separate blood supply), this appears to be less likely in this particular case. Another common cause of delayed union/nonunion in limb lengthening is rapid and/or uncontrolled nail elongation and a distraction of more than 1.5 mm per day.30 The distraction index in this patient, however, was 1.0 mm/day and uncontrolled distraction is, therefore, less likely to be the cause for the delayed bone healing too.
One potential problem of the described technique is, that – especially in cases with a short bone length or a second CORA in close proximity to the lengthening osteotomy – the plate position might interfere with the tip of the nail and hence impede locking of the nail and/or plate. One option to overcome this problem with the described technique might be locking the nail through a hole of the locking plate, but biomechanical implications have to be taken into consideration. Additionally, an exact knowledge of the blood supply of each bone segment is imperative and should be considered preoperatively when performing the described technique. A gentle operation technique as well as the use of low contact plates with limited plate-periosteum contact and/or temporary spacers (between plate and periosteum) is furthermore strongly recommended.
The study at hand is limited by factors such as the small sample size as well as the lack of a matched control group treated with external fixation devices. Additionally, our collective is rather inhomogeneous with regards to the underlying cause for correction (congenital versus acquired deformity), correction site (femur versus tibia) as well as the used locking plates. The last, however, is subject to patient’s age, anatomical preconditions and osteotomy site, as well as the required amount of correction, and cannot, therefore, be standardized. We acknowledge these limitations but are of the opinion that this does not affect our conclusions as we describe a pilot study on a novel treatment technique, which is to be adjusted to the requirements of each patient individually.
Conclusion
The combination of two osteotomies and fixation with a fully implantable lengthening nail as well as a locking plate is a valuable method for treating leg length discrepancies with concomitant axis deformities. Meticulous preoperative planning and intraoperative implementation, however, is mandatory in order to achieve satisfying results. Furthermore, a thorough patient selection (e.g. exclusion of patients with a compromised vascular supply, smokers, etc.) is strongly recommended in order to minimize complication rates.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
OA Licence Text
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Ethical statement
Ethical approval: This study is a technical note and contains solely retrospective, unidentifiable data.
Informed consent: Informed consent was not required for this work.
ICMJE Conflict of interest statement
None declared.
References
- 1.Baumgart R, Bürklein D, Hinterwimmer S, Thaller P, Mutschler W.. The management of leg-length discrepancy in Ollier’s disease with a fully implantable lengthening nail. J Bone Joint Surg [Br] 2005;87-B:1000–1004. [DOI] [PubMed] [Google Scholar]
- 2.Black SR, Kwon MS, Cherkashin AM, et al. Lengthening in congenital femoral deficiency: a comparison of circular external fixation and a motorized intramedullary nail. J Bone Joint Surg [Am] 2015;97:1432–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Horn J, Grimsrud Ø, Dagsgard AH, Huhnstock S, Steen H.. Femoral lengthening with a motorized intramedullary nail. Acta Orthop 2015;86:248–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krieg AH, Lenze U, Speth BM, Hasler CC.. Intramedullary leg lengthening with a motorized nail. Acta Orthop 2011;82:344–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krieg AH, Speth BM, Foster BK.. Leg lengthening with a motorized nail in adolescents : an alternative to external fixators?. Clin Orthop Relat Res 2008;466:189–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Küçükkaya M, Karakoyun Ö Sökücü S, Soydan R.. Femoral lengthening and deformity correction using the Fitbone motorized lengthening nail. J Orthop Sci 2015;20:149–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schiedel FM, Pip S, Wacker S, et al. Intramedullary limb lengthening with the Intramedullary Skeletal Kinetic Distractor in the lower limb. J Bone Joint Surg [Br] 2011;93-B:788–792. [DOI] [PubMed] [Google Scholar]
- 8.Simpson AH, Shalaby H, Keenan G.. Femoral lengthening with the Intramedullary Skeletal Kinetic Distractor. J Bone Joint Surg [Br] 2009;91-B:955–961. [DOI] [PubMed] [Google Scholar]
- 9.Lenze U, Krieg AH.. Intramedullary lengthening nails: can we also correct deformities?. J Child Orthop 2016;10:511–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dahl MT, Gulli B, Berg T.. Complications of limb lengthening. A learning curve. Clin Orthop Relat Res 1994;301:10–18. [PubMed] [Google Scholar]
- 11.Eren I, Eralp L, Kocaoglu M.. Comparative clinical study on deformity correction accuracy of different external fixators. Int Orthop 2013;37:2247–2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ganger R, Radler C, Speigner B, Grill F.. Correction of post-traumatic lower limb deformities using the Taylor spatial frame. Int Orthop 2010;34:723–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res 1990;250:81–104. [PubMed] [Google Scholar]
- 14.Blondel B, Launay F, Glard Y, et al. Limb lengthening and deformity correction in children using hexapodal external fixation: preliminary results for 36 cases. Orthop Traumatol Surg Res 2009;95:425–430. [DOI] [PubMed] [Google Scholar]
- 15.Iobst C. Limb lengthening combined with deformity correction in children with the Taylor Spatial Frame. J Pediatr Orthop B 2010;19:529–534. [DOI] [PubMed] [Google Scholar]
- 16.Rozbruch SR, Segal K, Ilizarov S, Fragomen AT, Ilizarov G.. Does the Taylor Spatial Frame accurately correct tibial deformities? Clin Orthop Relat Res 2010;468:1352–1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim H, Lee SK, Kim KJ, et al. Tibial lengthening using a reamed type intramedullary nail and an Ilizarov external fixator. Int Orthop 2009;33:835–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Popkov A, Aranovich A, Popkov D.. Results of deformity correction in children with X-linked hereditary hypophosphatemic rickets by external fixation or combined technique. Int Orthop 2015;39:2423–2431. [DOI] [PubMed] [Google Scholar]
- 19.Sun XT, Easwar TR, Manesh S, et al. Complications and outcome of tibial lengthening using the Ilizarov method with or without a supplementary intramedullary nail: a case-matched comparative study. J Bone Joint Surg [Br] 2011;93-B:782–787. [DOI] [PubMed] [Google Scholar]
- 20.Krieg AH, Lenze U, Hasler CC.. Ilizarov hip reconstruction without external fixation: a new technique. J Child Orthop 2010;4:259–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paley D, Bhave A, Herzenberg JE, Bowen JR.. Multiplier method for predicting limb-length discrepancy. J Bone Joint Surg [Am] 2000;82-A:1432–1446. [DOI] [PubMed] [Google Scholar]
- 22.Lenze U, Hasler CC, Krieg AH.. Intramedullary motorized nail for equalization of posttraumatic leg length discrepancies. Unfallchirurg 2011;114:604–610. [DOI] [PubMed] [Google Scholar]
- 23.Baumgart R. The reverse planning method for lengthening of the lower limb using a straight intramedullary nail with or without deformity correction. A new method. Oper Orthop Traumatol 2009;21:221–233. [DOI] [PubMed] [Google Scholar]
- 24.Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A.. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am 1994;25:425–465. [PubMed] [Google Scholar]
- 25.Baumgart R, Betz A, Schweiberer L.. A fully implantable motorized intramedullary nail for limb lengthening and bone transport. Clin Orthop Relat Res 1997;343:135–143. [PubMed] [Google Scholar]
- 26.Cole JD, Justin D, Kasparis T, DeVlught D, Knobloch C.. The intramedullary skeletal kinetic distractor (ISKD): first clinical results of a new intramedullary nail for lengthening of the femur and tibia. Injury 2001;32:SD129–SD139. [DOI] [PubMed] [Google Scholar]
- 27.Iobst CA, Dahl MT.. Limb lengthening with submuscular plate stabilization: a case series and description of the technique. J Pediatr Orthop 2007;27:504–509. [DOI] [PubMed] [Google Scholar]
- 28.Rozbruch SR, Kleinman D, Fragomen AT, Ilizarov S.. Limb lengthening and then insertion of an intramedullary nail: a case-matched comparison. Clin Orthop Relat Res 2008;466:2923–2932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Iobst CA, Rozbruch SR, Nelson S, Fragomen A.. Simultaneous acute femoral deformity correction and gradual limb lengthening using a retrograde femoral nail: technique and clinical results. J Am Acad Orthop Surg 2018;26:241–250. [DOI] [PubMed] [Google Scholar]
- 30.Kenawey M, Krettek C, Liodakis E, Meller R, Hankemeier S.. Insufficient bone regenerate after intramedullary femoral lengthening: risk factors and classification system. Clin Orthop Relat Res 2011;469:264–273. [DOI] [PMC free article] [PubMed] [Google Scholar]


