Abstract
A 5-month-old baby presented with a low-grade fever and tachypnoea and was found to have right upper lobe consolidation on chest radiograph. He was admitted with the diagnosis of bronchopneumonia and the treatment protocol for pneumonia was initiated. Blood culture samples were collected, and he was started on a course of intravenous amoxicillin–clavulanate. Blood culture results displayed pansensitive Gemella morbillorum bacteraemia and he was continued on intravenous antibiotic to which he responded in a short period and was discharged in good condition on the fourth day.
Keywords: paediatrics, pneumonia (respiratory medicine)
Background
Gemella morbillorum is a microaerophilic cocci that can be found as part of the commensal flora in the human body. Infection with G. morbillorum is uncommon, and its reports in literature are rather limited; however, it is most commonly known to cause infective endocarditis in susceptible or immunocompromised patients. While other organs may be affected in some cases, a respiratory focus for the infection is relatively uncommon. The majority of the diagnosed cases are usually adult males. We present the first reported case of G. morbilliform causing a pulmonary infection and bacteraemia in an infant, who was also otherwise healthy and had no other comorbidities.
Case presentation
We present a case of 5-month-old baby who had a history of dry cough and fever associated with progressive breathing difficulty for 6 days. The cough was also associated with post-tussive vomiting, but no other systemic features were present. No other relevant medical or surgical history of note. No contact history or history of recent travel was given. He was appropriately immunised for his age.
On examination, the baby was appropriately developed for age and well nourished. He had a low-grade fever and was mildly tachypnoeic. Cardiovascular examination was unremarkable; respiratory auscultation revealed diffuse wheezes and rales with equal bilateral air entry. No rash was appreciated on the body and there were no palpable lymph nodes.
Investigations
Lab investigations revealed a slightly elevated C-reactive protein of 41.5 mg/L and a procalcitonin level of 0.15 ng/mL. The white cell count and its differentials on admission can be found in table 1.
Table 1.
Lab investigations on admission
| Laboratory parameter | Reference range and units | Patient’s result |
| White cell count | 6.0–18.0×109/L | 14.4 |
| Neutrophils absolute | 1.0–6.0×109/L | 2.6 |
| Lymphocytes absolute | 4.0–10.0×109/L | 9.2 |
| Monocytes absolute | 0.2–1.2×109/L | 2.5 |
| Eosinophils absolute | 0.1–1.0×109/L | 0.0 |
| Basophils absolute | 0.0–0.1×109/L | 0.0 |
Chest X-ray revealed a consolidation in the upper right lobe, with increased bronchovascular and hilar markings (figure 1). All other conducted investigations were found to be normal.
Figure 1.
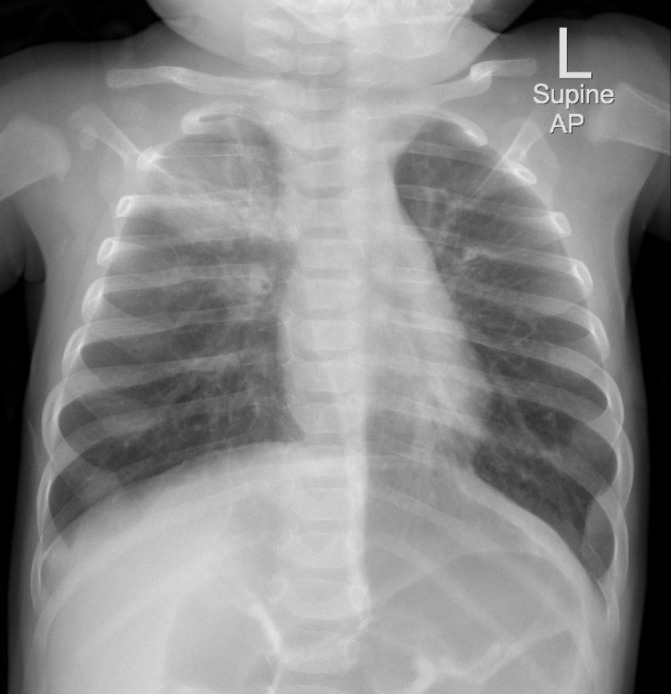
Consolidation in the right upper lobe with prominent bronchovascular and hilar markings.
Differential diagnosis
A viral infection was initially considered as a differential in this patient. However, further viral tests were not performed at the time due to the quick positive blood culture results, radiographic findings of consolidation, the immediate response to antibiotics, as well as the negative family or contact history of note.
A suspicion of chlamydial pneumonia was also ruled out due to the lack of relevant clinical signs or symptoms in both the mother and child, including neonatal conjunctivitis which may preclude pneumonitis in some cases. Moreover, the prompt response to a penicillin type antibiotic also dissuades from an underlying chlamydial infection being present, especially as pneumonia secondary to Chlamydia trachomatis may require a more prolonged course of treatment before responding.1
Lung collapse was considered in light of the relevant radiological findings. However, the fever and its resolution, decreasing C-reactive protein levels and the return to clinical baseline after antibiotic admission dissuaded against this diagnosis.
Treatment
He was admitted as a case of bronchopneumonia and was started on intravenous amoxicillin–clavulanate 30 mg/kg every 8 hours after samples were collected for blood cultures. Blood culture results displayed pansensitive G. morbillorum using matrix-assisted laser desorption ionisation-time of flight mass spectrometry (MALDI-TOF MS) technology. He was hence continued on the same antibiotic regimen until the time of discharge.
Outcome and follow-up
Patient began clinically improving on the second day after admission and was discharged on the fourth day after he had recovered fully with resolution of the fever. Repeat blood cultures were collected prior to discharge and were negative, and repeated C-reactive protein levels were found to be decreasing (31.2 mg/L). He is since following up in the paediatric clinic with no problems.
Discussion
We report the first case of pulmonary infection with G. morbillorum in the middle east and the youngest patient to have been diagnosed with a respiratory focus for the disease.
It is pertinent to address that colonisation with G. morbillorum was less likely in this infant as he was acutely symptomatic, responded well to antibiotics and had some raised inflammatory markers at the time. Additionally, a diagnosis of bacteremia was deemed to be most likely despite the rather modestly raised C-reactive protein levels. This was cumulatively due to the above-mentioned points, but especially with regard to the positive blood culture results that displayed pansensitive G. morbillorum.
G. morbillorum is a Gram positive, catalase negative, facultatively anaerobic coccus that was first isolated in 1917. It was then renamed and reclassified several times until it was finally placed in the genus Gemella in 1988, where it is now found with five other species.2 3
While the microaerophilic organism may be found as a part of the normal flora in the human body, it may cause an opportunistic infection in some cases where it presents as a severe localised or generalised infection.2 3 Infections tend to progress rapidly but respond well to early antibiotic therapy as observed in our case. Affected individuals are usually adult males between the ages of 20 to 80 years, usually with poor dental hygiene or a recent history of dental procedures.2 4 5 Another possible route for pulmonary infection is through aspiration of oral intake, which is likely in our patient.5 The infection is especially common among individuals with predisposing factors such as immunosuppressed patients, diabetics or patients with known cardiac abnormalities.3
The results of a comprehensive literature review revealed that most of the case reports are based in Far East Asian countries, with very few Middle Eastern reports of the disease. A study conducted in 1994 over the period of 15 years found a total of five cases of G. morbillorum among 1962 specimens studied for anaerobic bacteria, all of which were found in abscesses.6 While a definitive incidence of the organism is currently not known, the actual number of cases are estimated to higher in number than what is currently recorded in the literature. This may be either because the bacteria can be easily decolourised during Gram staining which may make a confirmatory diagnosis more difficult; but it may also be due to the inconsistent collection of blood or sputum cultures among patients diagnosed with pneumonia.2 5 In this regard, a Medline search among English speaking papers yielded no more than seven publications regarding patients diagnosed with pulmonary infections caused by G. morbillorum.5 7–12 Most of the mentioned case reports occurred among adults, with very few reports among adolescents, and none among infants. In addition, almost all the cases were then further complicated by an abscess formation or empyema and had an initial predisposing factor in the form of increased alcohol intake, poor oral hygiene, intubation or intravenous drug abuse. Our patient was an infant with a developing immune system; this may also be considered as a potential predisposing factor.
The authors recommend further studies into the clinical relevance of G. morbillorum especially among the paediatric population. The emerging significance of previously lesser well-known microorganisms such as G. morbillorum needs to be taken into consideration in future large-scale microbiological studies.
Learning points.
Gemella morbillorum is a commensal organism that may present as a severe opportunistic infection.
G. morbillorum is most commonly known to cause endocarditis, but may also affect other organs, including the lungs.
Routes for the infections are usually orodental; however, in a pulmonary focus aspiration of the bacteria is also possible.
Footnotes
Contributors: SH has drafted the content, with an extensive literature review and took the lead in writing the manuscript. SaH has assisted in the production and critical revision of the report. MA oversaw the creation of the report, provided critical feedback and was also involved in the direct care of the patient.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Parental/guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Miller KE. Diagnosis and treatment of Chlamydia trachomatis infection. Am Fam Physician 2006;73:1411–6. [PubMed] [Google Scholar]
- 2.Benedetti P, Rassu M, Branscombe M, et al. Gemella morbillorum: an underestimated aetiology of central nervous system infection? J Med Microbiol 2009;58:1652–6. 10.1099/jmm.0.013367-0 [DOI] [PubMed] [Google Scholar]
- 3.Godinho AR, Tomé E, Vaz A, et al. Endocardite por Gemella: uma entidade agressiva. Revista Portuguesa de Cardiologia 2013;32:1027–30. 10.1016/j.repc.2013.06.005 [DOI] [PubMed] [Google Scholar]
- 4.Akiyama K, Taniyasu N, Hirota J, et al. Recurrent aortic valve endocarditis caused by Gemella morbillorum–report of a case and review of the literature. Jpn Circ J 2001;65:997–1000. [DOI] [PubMed] [Google Scholar]
- 5.Famularo G, De Simone C, Minisola G, et al. Pneumonia and sepsis caused by Gemella morbillorum: an unusual association. Intern Med 2006;45:1253–4. 10.2169/internalmedicine.45.1792 [DOI] [PubMed] [Google Scholar]
- 6.Brook I. Microaerophilic streptococcal infection in children. J Infect 1994;28:241–9. 10.1016/S0163-4453(94)91543-1 [DOI] [PubMed] [Google Scholar]
- 7.Bahrani-Mougeot FK, Paster BJ, Coleman S, et al. Molecular analysis of oral and respiratory bacterial species associated with ventilator-associated pneumonia. J Clin Microbiol 2007;45:1588–93. 10.1128/JCM.01963-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blitman NM, Steiner AM, Bell MD, et al. Pulmonary nodules associated with Gemella bacteremia: CT findings in two children with osteosarcoma. J Thorac Imaging 2007;22:182–4. 10.1097/01.rti.0000213582.21849.15 [DOI] [PubMed] [Google Scholar]
- 9.Poulose V. Gemella empyema cured without antibiotics: a case report. Ann Acad Med Singapore 2002;31:802–4. [PubMed] [Google Scholar]
- 10.da Costa CT, Porter C, Parry K, et al. Empyema thoracis and lung abscess due to Gemella morbillorum. Eur J Clin Microbiol Infect Dis 1996;15:75–7. 10.1007/BF01586189 [DOI] [PubMed] [Google Scholar]
- 11.Valipour A, Koller H, Setinek U, et al. Pleural empyema associated with Gemella morbillorum: report of a case and review of the literature. Scand J Infect Dis 2005;37:378–81. 10.1080/00365540510035319 [DOI] [PubMed] [Google Scholar]
- 12.Yamakawa H, Hayashi M, Tanaka K, et al. Empyema due to gemella morbillorum is diagnosed by 16s ribosomal rna gene sequencing and a phylogenetic tree analysis: a case report and literature review. Intern Med 2015;54:2231–4. 10.2169/internalmedicine.54.4950 [DOI] [PubMed] [Google Scholar]


