Abstract
Background
Prior research has found a reliable and robust association between poor dyadic (e.g., marital) adjustment and depression and anxiety. However, it is possible that this association may be due, at least in part, to confounding variables (i.e., variables that are causally associated both with marital adjustment and psychopathology and could account for their covariation). The present study was conducted using a genetically informative sample of twins to examine the association between dyadic adjustment and symptoms of depression and anxiety, accounting for unmeasured genetic and shared environmental confounds.
Methods
A Swedish sample of monozygotic and dizygotic twins (218 female twin pairs and 321 male twin pairs) and their spouse or long-term partner completed self-report measures of dyadic adjustment, depressive symptoms, and anxiety symptoms.
Results
Results suggest that dyadic adjustment was significantly and negatively associated with depressive symptoms and anxiety symptoms in twins, and nonshared environmental influences largely accounted for this association. Furthermore, results obtained from partners’ reports of dyadic adjustment were largely consistent with those obtained from twins’ reports, suggesting that results were not a function of shared method variance.
Limitations
Longitudinal research in genetically informative samples would provide a stronger test of the causal association between dyadic adjustment and psychopathology.
Conclusions
The pattern of findings suggest that common nonshared environmental influences, such as partners’ characteristics, may lead to poorer dyadic adjustment and depression and anxiety. Therefore, couple-based interventions that improve dyadic adjustment may be effective in preventing and treating psychopathology in relationship partners.
Keywords: depression, anxiety, marital discord, marital adjustment, marital satisfaction, twin
1. Introduction
Poor marital adjustment is associated with mood, anxiety, and substance use disorders in population samples (McShall and Johnson, 2015; Whisman, 1999, 2007). Many of these studies have examined how marital adjustment contributes to subsequent psychopathology, while acknowledging that psychopathology may also impact relationship adjustment (Whisman and Uebelacker, 2009). This study was conducted to examine genetic and environmental influences on the covariation between marital adjustment and symptoms of depression and anxiety in a sample of male and female twins and their spouse or long-term partner.
Much of the research on intimate relationships and psychopathology has focused on depression (Beach and Whisman, 2012; Whisman and Baucom, 2012). Cross-sectional studies suggest that poor marital adjustment is associated with higher levels of depressive symptoms (Proulx et al., 2007; Whisman, 2001) and prevalence of major depression (McShall and Johnson, 2015; Whisman, 1999, 2007). Longitudinal studies suggest poor marital adjustment is associated with increases in depressive symptoms (Beach et al., 2003; Whisman and Uebelacker, 2009) and incidence of depressive disorders (Overbeek et al., 2006; Whisman and Bruce, 1999) in two-wave studies, and bidirectional associations between poor marital adjustment and depressive symptoms in multi-wave studies (Davila et al., 2003; Kouros et al., 2008; Whitton et al., 2008).
These results are consistent with the perspective that poor dyadic adjustment may be causally related to depression (Beach et al., 1990). However, stronger inferences regarding potential causal associations can be made if it is shown that these associations are not due to shared variance with other variables that could be causally associated both with poor dyadic adjustment and depression (McNamee, 2003). Studies have tried to rule out potential rival explanations by statistically adjusting for potential confounding variables, including personality traits (Cao et al., 2017; Vento and Cobb, 2011; Whisman et al., 2006), quality of participants’ relationships with their relatives and friends (Whisman et al., in press; Whisman et al., 2000), and self-esteem and stressful life events (Cao et al., 2017). Although these studies are important, they are typically limited because of measurement error in the assessment of confounding variables. Furthermore, as researchers must select which variables to control, and generally can only select a few variables, the assessment of confounding variables is not comprehensive (i.e., there are other unmeasured variables that could account for the association) (Irons et al., 2015).
One alternative to statistical control of potential confounds is to leverage genetically informative twin studies to account for unmeasured confounding variables and better understand potential causal associations between variables (Rutter, 2007). Because monozygotic (MZ) twins share 100% of their genes, whereas dizygotic (DZ) twins share only 50% of their segregating genes on average, and because twins reared together are raised in the same families at the same time, twin studies allow researchers to control for unmeasured genetic and shared environmental factors (i.e., environmental factors that lead siblings raised in the same family to be similar). If observed (i.e., phenotypic) associations between variables remain statistically significant after taking genetic and shared environmental confounds into account, then findings are consistent with a causal relationship; such phenotypic associations have been described as quasi-causal (Turkheimer and Harden, 2014). However, this approach cannot provide definitive evidence of a causal relationship, as the association may be explained by nonshared environmental influences, such as stressful life events, that lead to both poor marital adjustment and depression in one twin.
Research suggests there are genetic influences on dyadic adjustment (Spotts et al., 2004b; Spotts et al., 2006) and psychopathology (Burmeister et al., 2008), and researchers have begun to use genetically informative samples to account for genetic confounds that may explain the association between dyadic adjustment and psychopathology (for a review, see Whisman and South, 2017). In a study of female twins, there were shared genetic influences on the covariation between wives’ self-reported dyadic adjustment and depressive symptoms (Spotts et al., 2004a). Further evidence for shared genetic effects came from husband-reported dyadic adjustment, suggesting that a wife’s genetically influenced characteristics may impact her own and her husband’s dyadic adjustment. There was also evidence of non-shared environmental influences on the covariation between husbands’ report of dyadic adjustment and wives’ depressive symptoms, which may reflect the influence of partners’ characteristics (i.e., twins being married to different partners). Also, in a sample of male and female twins, the association between marital support and depressive symptoms was statistically significant after adjusting for genetic effects of marital support on depressive symptoms, suggesting that the association between marital support and depressive symptoms was not an artifact of selection (Beam et al., 2011).
Dyadic adjustment has also been found to covary with anxiety. For example, poor marital adjustment is associated with symptoms of anxiety (Leach et al., 2013) and anxiety disorders (McLeod, 1994; Pankiewicz et al., 2012; Whisman, 1999, 2007). Furthermore, poor marital adjustment at baseline was associated with increased risk for incidence of the broad category of anxiety disorders (and the specific diagnosis of social phobia) two to three years later (Overbeek et al., 2006). However, we are not aware of any twin studies that have evaluated genetic and environmental influences on the covariation between dyadic adjustment and anxiety.
This study was conducted to examine the association between dyadic adjustment and symptoms of depression and anxiety in a sample of Swedish twins and their spouse or long-term partner1. Both male and female twins and their partners were included, which allowed us to evaluate gender and respondent differences in genetic and environmental influences on the associations between variables. In addition, this is the first study known to us to examine genetic and environmental influences on the covariation between dyadic adjustment and anxiety symptoms. Consistent with the perspective that poor marital adjustment increases risk for psychopathology (Beach et al., 1990), we predicted that dyadic adjustment would be negatively associated with depressive and anxiety symptoms for both female and male twins, and that nonshared environmental influences would primarily account for these associations.
2. Method
2.1 Participants
Participants were drawn from Cohort 2 of the Twin and Offspring Study in Sweden (TOSS; Neiderhiser and Lichtenstein, 2008), which consists of same-sex twin pairs born between 1944–1971, identified through The Swedish Twin Registry. To be eligible, each member of the twin pair (a) had to be involved in a long-term (i.e., ≥5-year) relationship with a partner residing in the same home; and (b) have an 11- to 22-year-old adolescent child who was the same sex as the co-twin’s child with no more than a 4-year age difference between cousins. TOSS was reviewed by the Institutional Review Board in Sweden and the United States. We included a subset of twin pairs for whom data were complete for both partners. The sample consisted of 218 female twin pairs and 321 male twin pairs and their spouse or partner. On average, female twins were 43.2 years old (SD=4.7) and their partners were 45.5 years old (SD=6.1), whereas male twins were 46.9 years old (SD=4.7) and their partners were 44.7 years old (SD=4.8).
2.2 Measures
2.2.1 Dyadic Adjustment
Dyadic adjustment was measured with the 32-item Dyadic Adjustment Scale (DAS; Spanier, 1976, 1989). Except for Item 31, which was answered on a 7-point scale, the remaining items were answered using a 6-point scale. Furthermore, response options for Item 16 to Item 30 ranged from Never to Always, which differs from the traditional response options. A summary score is computed by reverse scoring the negative items and computing the sum of the items, with higher scores indicating greater adjustment. Because the number of and labels for response options for several items differs from how it is usually scored, the resulting scores are not directly comparable to those obtained using traditional scoring.
2.2.2 Depressive Symptoms
Depressive symptoms were assessed with the 20-item Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977). Items are rated on a 4-point scale for the frequency of occurrence during the past week. A summary score is computed by reverse scoring the positive items and computing the sum of the items, with total scores ranging from 0–60 and higher scores indicating greater symptom severity.
2.2.3 Anxiety Symptoms
Anxiety symptoms were measured with the 21-item Beck Anxiety Inventory (BAI; Beck et al., 1988). The BAI was developed to be relatively independent of depression, and it has demonstrated convergent and discriminant validity (Fydrich et al., 1992). Items are rated on a 4-point scale, indicating how often the respondent has been bothered by each symptom during the past week. A summary score is calculated by computing the sum of the items, with total scores ranging from 0–63 and higher scores indicating greater symptom severity.
2.3 Statistical Analysis
Descriptive information on original study variables is presented in Table 1. After visually inspecting the data for univariate outliers, we used a log transformation of the CES-D to improve normality; after transformation, skewness and kurtosis were <1. Log and square root transformations did not sufficiently improve normality for the BAI; thus, we created an ordinal BAI variable that enabled us to estimate the underlying liability based on the frequencies within each category and decrease risk of biased parameter estimates typical of highly skewed variables (Derks et al., 2004). The ordinal BAI variable has 5 categories: 545 people with a score of 0, 549 with a score of 1–2, 475 with a score of 3–5, 305 with a score of 6–9, and 268 with a score of ≥10.
Table 1.
Descriptive Information on Original Study Measures for Twins and Their Spouse or Partner
| Respondent and Measure | Mean | SD | Skewness | Kurtosis | Range |
|---|---|---|---|---|---|
| Twin | |||||
| DAS | 151.34 | 17.53 | −0.79 | 1.32 | 70 – 191 |
| CES-D | 9.81 | 8.11 | 1.36 | 1.71 | 0 – 45 |
| BAI | 3.95 | 5.49 | 2.94 | 13.48 | 0 – 47 |
| Spouse/Partner | |||||
| DAS | 150.25 | 17.85 | −0.72 | 0.68 | 83 – 191 |
| CES-D | 10.82 | 8.57 | 1.19 | 1.54 | 0 – 54 |
| BAI | 4.57 | 5.55 | 2.50 | 9.37 | 0 – 46 |
Note. DAS = Dyadic Adjustment Scale. CES-D = Center for Epidemiologic Studies Depression Scale. BAI = Beck Anxiety Inventory.
Structural equation models (SEM) were conducted using Mplus 7.4 (Muthén and Muthén, 1998–2015). For models that included the BAI, we used the means and variance adjusted weighted least squares (WLSMV) estimation method, which uses pairwise deletion for participants with missing data on one or more measures. For all other models, we used maximum likelihood (ML) estimation, which uses full-information maximum likelihood (FIML) for missing data. This method treats missing data as missing at random, uses all available data to compute parameter estimates, and is robust to non-normality (Enders, 2001).
We used the χ2 statistic to assess model fit. Because the χ2 is sensitive to sample size, we also used the comparative fit index (CFI; Bentler, 1990) and the root mean square error of approximation (RMSEA; Browne and Cudeck, 1993). As recommended by Hu and Bentler (1998), we used a CFI >.95 and RMSEA <.06 as indications of good fit. To conduct nested model comparisons, we used chi-square difference (Δχ2) tests incorporating the scaling factors (Satorra and Bentler, 2001). To determine significance of specific parameters, we used p values for the z static, but if the p value and the Δχ2 led to inconsistent conclusions, the Δχ2 was used. Gender differences in parameters were evaluated by comparing model fit of a model in which the parameters were allowed to be free across gender versus constrained to be equal across gender. The power to detect a difference between these models ranged from .28 to .322.
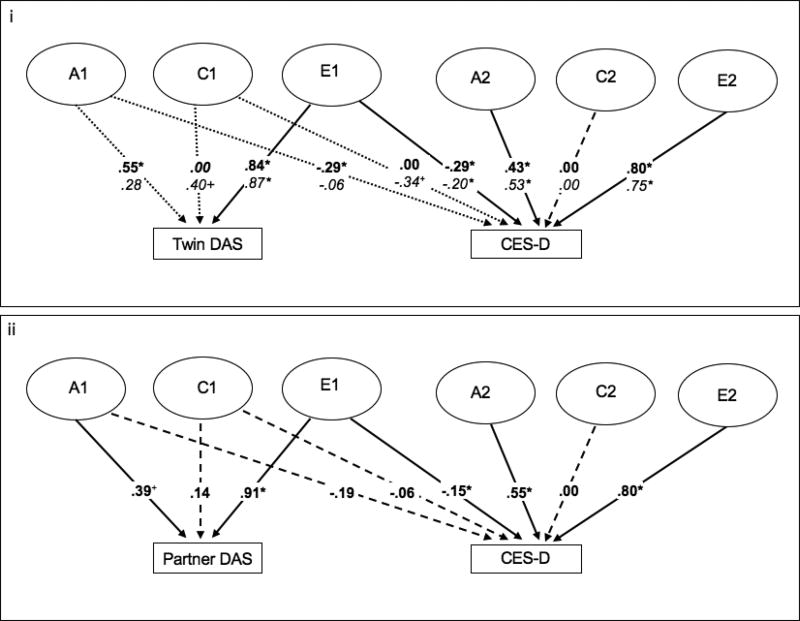
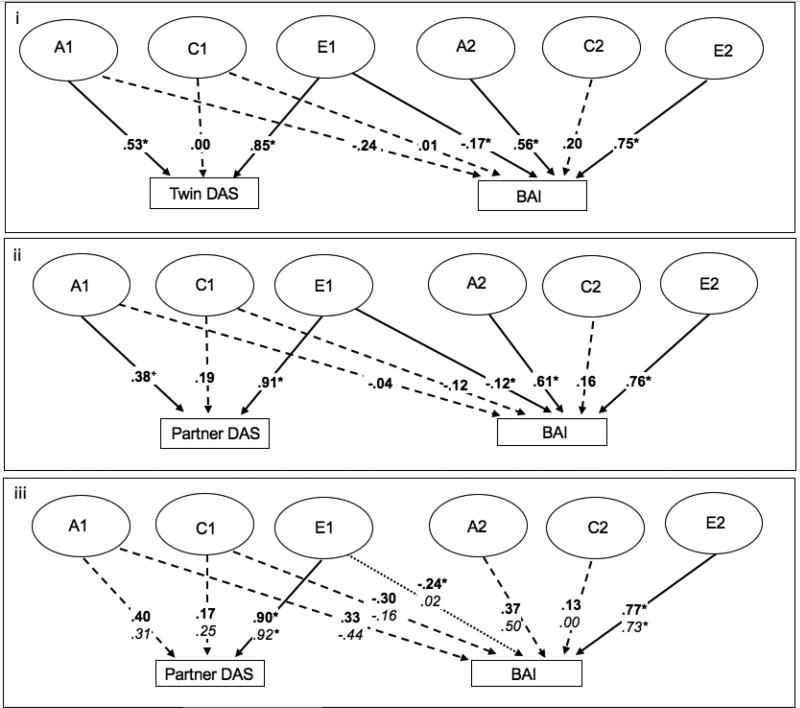
We conducted a multivariate Cholesky decomposition to examine the magnitude of the correlation between dyadic adjustment and depressive symptoms or anxiety symptoms explained by additive genetic (A), shared or common environment (C), or nonshared environmental influences (E), using path tracing rules on the paths shown in Figures 1 and 2. The Cholesky decomposition leverages the genetically informative twin sample and extends univariate ACE models to multiple variables by partitioning the covariance matrix with a set of ACE components (Loehlin, 1996; Neale and Cardon, 1992). For example, A1 in Figure 1i represents all the genetic influences on twin-reported dyadic adjustment, which are also allowed to predict twins’ depression symptoms. A2 represents the genetic influences that are unique to twins’ depression symptoms (i.e., unrelated to twin-reported dyadic adjustment). These models are depicted for Twin 1 in Figures 1 and 2, but are also estimated for Twin 2. The correlation between the A of Twin 1 and Twin 2 can be constrained to 1 for MZ twins and .5 for DZ twins because they share 100% of their genes and 50% of their segregating genes on average, respectively. As all twins in this sample were reared together, the correlation between the C of Twin 1 and Twin 2 can be constrained to 1 for both MZ and DZ twins. To improve the interpretability of the results from the Cholesky decompositions, we also calculated the percent of the correlation between dyadic adjustment and either depressive or anxiety symptoms that was attributable to genetic, shared environmental, or nonshared environmental influences. We ran each Cholesky decomposition twice, once using twin-reported (i.e., self-reported) dyadic adjustment and once using partner-reported dyadic adjustment.
Figure 1.
Cholesky decomposition of depressive symptoms with twin-reported dyadic adjustment (panel i) and partner-reported dyadic adjustment (panel ii). The figure depicts the model for one twin. However, the Cholesky decomposition estimates the same model for both twins, and constrains the correlation between A of Twin 1 and Twin 2 to be 1 in MZ twins to reflect that MZ twins share 100% of their genes, and .5 in DZ twins to reflect that DZ twins share 50% of their segregating genes on average. The correlation between C of Twin 1 and Twin 2 is constrained to 1 to reflect that all twins share a common environment. In panel i, parameters are presented separately for men and women, with men in bold and women in italics. In panel ii, parameters were constrained to be equal across men and women. Dashed lines indicate nonsignificant paths. In panel i, dotted lines indicate paths that are significant in one sex and nonsignificant in the other. Ellipses indicate latent variables, and rectangles indicate observed variables. A1=additive genetic influences common to both the DAS and the CES-D; A2=additive genetic influences specific to the CES-D; C1=shared environmental influences common to the DAS and CES-D; C2=shared environmental influences specific to the CES-D; E1=nonshared environmental influences common to the DAS and CES-D; E2=nonshared environmental influences specific to the CES-D; DAS=Dyadic Adjustment Scale; CES-D=Center for Epidemiologic Studies Depression Scale. * p < .05. + p < .10.
Figure 2.
Cholesky decomposition of anxiety symptoms with twin-reported dyadic adjustment (panel i) and partner-reported dyadic adjustment (panels ii and iii). The figure depicts the model for one twin. However, the Cholesky decomposition estimates the same model for both twins, and constrains the correlation between A of Twin 1 and Twin 2 to be 1 in MZ twins to reflect that MZ twins share 100% of their genes, and .5 in DZ twins to reflect that DZ twins share 50% of their segregating genes on average. The correlation between C of Twin 1 and Twin 2 is constrained to 1 to reflect that all twins share a common environment. In panels i and ii, parameters were constrained to be equal across men and women. In panel iii, parameters were not constrained to be equal across sex (parameters for men in bold and women in italics), and dotted lines indicate paths that are significant in one sex but not in the other. Dashed lines indicate nonsignificant paths. Ellipses indicate latent variables, and rectangles indicate observed variables. A1=additive genetic influences common to both the DAS and the BAI; A2=additive genetic influences specific to the BAI; C1=shared environmental influences common to the DAS and BAI; C2=shared environmental influences specific to the BAI; E1=nonshared environmental influences common to the DAS and BAI; E2=nonshared environmental influences specific to the BAI; DAS=Dyadic Adjustment Scale; BAI=Beck Anxiety Inventory. *p < .05.
3. Results
Twin- and partner-reported dyadic adjustment were highly correlated (r=.58, p<.001), suggesting that twins and partners were consistent in their assessment and reporting of the level of adjustment in their relationships. There was also evidence of similarity between partners in depression and anxiety; depression symptoms of twins and their partners were positively correlated (r=.20, p<.001), as were anxiety symptoms of twins and partners (r=.07, p=.03).
3.1 Association Between Dyadic Adjustment and Symptoms of Depression and Anxiety
We examined phenotypic, within-trait cross-twin, and cross-trait cross-twin correlations between dyadic adjustment and depressive and anxiety symptoms. Constraining the correlations across gender significantly reduced model fit, Δχ2(56)=78.04, p=.027. Thus, we allowed the correlations to vary across gender, χ2(277)=290.68, p=.274, CFI=.987, RMSEA=.019 [.000, .040]. Lower levels of dyadic adjustment were associated with greater depressive symptoms in men (r=−.42, p<.001) and women (r=−.32, p<.001), and greater anxiety symptoms in men (r=−.25, p<.001) and women (r=−.27, p<.001). As expected, depressive and anxiety symptoms were highly correlated in both men (r=.53, p<.001) and women (r=.60, p<.001).
The main aim of the present study was to examine the association between dyadic adjustment and depressive and anxiety symptoms after accounting for unmeasured genetic and shared environmental confounds. First, we examined the correlation between within-pair difference in dyadic adjustment and within-pair difference in depressive and anxiety symptoms in MZ twin pairs, who share 100% of genetic and shared environmental influences and differ only in nonshared environmental influences (Table 2). Except for the correlation between the within-pair difference in partner-reported dyadic adjustment and anxiety in women, these correlations were statistically significant and suggest evidence consistent with causality.
Table 2.
Correlations Between Within-Pair Difference in Dyadic Adjustment and Within-Pair Difference in Depressive or Anxiety Symptoms in MZ Twin Pairs
| Gender | Twin DAS and CES−D |
Partner DAS and CES−D |
Twin DAS and BAI |
Partner DAS and BAI |
|---|---|---|---|---|
| Men | −.28* | −.19* | −.35* | −.25* |
| Women | −.34* | −.21* | −.23* | .01 |
Note. DAS = Dyadic Adjustment Scale. CES-D = Center for Epidemiologic Studies Depression Scale. BAI = Beck Anxiety Inventory.
p < .05.
Next, we examined MZ and DZ twin correlations by gender (Table 3). Results suggested genetic influences on all constructs, as within-trait cross-twin MZ correlations were greater than DZ correlations. The cross-trait cross-twin MZ correlations were also greater than the cross-trait cross-twin DZ correlations, suggesting genetic influences on the correlation between dyadic adjustment and depressive and anxiety symptoms in men. The cross-trait cross-twin MZ and DZ correlations were more similar in women, suggesting shared environmental influences on the correlation. The presence of phenotypic correlations that are larger than MZ cross-trait cross-twin correlations provided preliminary evidence of nonshared environmental influences on the correlation between dyadic adjustment and depressive and anxiety symptoms, and evidence consistent with correlations between the within-pair differences in dyadic adjustment and depressive and anxiety symptoms (Table 2).
Table 3.
Twin Correlations by Gender
| Gender and Twin |
Twin DAS |
Partner DAS |
CES-D | BAI | Twin DAS and CES-D |
Partner DAS and CES-D |
Twin DAS and BAI |
Partner DAS and BAI |
CES-D and BAI |
|---|---|---|---|---|---|---|---|---|---|
| Men | |||||||||
| MZ | .31* | .19* | .31* | 35* | −.17* | −.01 | −.10 | .08 | .20* |
| DZ | .06 | .11 | .08 | .23 | −.03 | .03 | .03 | .02 | .09+ |
| Women | |||||||||
| MZ | .30* | .18* | .55* | 47* | −.18* | −.17* | −.17* | −.18* | .37* |
| DZ | .19+ | .12 | .14 | .23 | −.20* | −.17* | −.19* | −.12 | .03 |
Note. DAS = Dyadic Adjustment Scale. CES-D = Center for Epidemiologic Studies Depression Scale. BAI = Beck Anxiety Inventory.
p < .05.
p < .10.
3.1.1. Dyadic adjustment and depressive symptoms
Results of the Cholesky decompositions for the association between the twin-reported dyadic adjustment and depressive symptoms are depicted in Figure 1i and 1ii. Constraining parameters to be equal across gender significantly reduced model fit, Δχ2(8)=27.95, p<.01. Thus, we report results from a noninvariant model3, χ2(36)=47.12, p=.102, CFI=.947, RMSEA=.048 [.000, .083] (Figure 1i). The results from this model indicate significant nonshared environmental influences on the correlation between dyadic adjustment and depressive symptoms. The percent of the correlation between dyadic adjustment and depressive symptoms that was attributable to genetic, shared environmental, or nonshared environmental influences are depicted in Table 4. Specifically, 60% and 54% of the dyadic adjustment-depressive symptom correlation in men and women, respectively, was due to nonshared environmental influences. Genetic influences also contributed to the association between dyadic adjustment and depression in men, with additive genetic influences explaining 40% of the correlation. Although neither genetic influences nor shared environmental influences explained a statistically significant proportion of the correlation in women, 41% of the correlation between dyadic adjustment and depressive symptoms was attributable to shared environmental influences. This result is consistent with the similar MZ and DZ cross-trait cross-twin correlations (Table 3). Importantly, it should be noted that the unique shared environmental influences on depression had to be fixed to zero for model convergence3.
Table 4.
Decomposition of Correlations between Dyadic Adjustment and Depressive or Anxiety Symptoms
| Measures | A | C | E | Total |
|---|---|---|---|---|
| Twin DAS and CES-D (Men) | −.16* (40%) | .00 (0%) | −.24* (60%) | −.40* |
| Twin DAS and CES-D (Women) | −.02 (5%) | −.13 (41%) | −.17* (54%) | −.32* |
| Partner DAS and CES-D | −.07 (34%) | −.01 (4%) | −.14* (62%) | −.22* |
| Twin DAS and BAI | −.13 (47%) | .00 (0%) | −.14* (53%) | −.27* |
| Partner DAS and BAI | −.02 (11%) | −.02 (16%) | −.10* (73%) | −.14* |
| Partner DAS and BAI (Men) | .13 (−98%) | −.05 (37%) | −.21* (161%) | −.13* |
| Partner DAS and BAI (Women) | −.13 (85%) | −.04 (25%) | .01 (−10%) | −.16* |
Note. Results are presented separately for men and women for the association between twin DAS and CES-D because constraining the parameters to be equal between men and women led to a significant decrement in fit, Δχ2(8)=27.95, p<.01. For the association between partner DAS and BAI, results are presented for men and women together and separately; constraining all of the parameters to be equal did not lead to a significant decrement in fit, Δχ2(9)=9.82, p=.36, but constraining the nonshared environmental covariance path did, Δχ2(1) =5.64, p=.02. Percentages were calculated by taking the correlation attributable to A, C, or E and dividing it by the total correlation and multiplying it by 100 (e.g., −.16/−.40 = .40×100 = 40%). Negative percentages indicate that the correlation due to genetic or environmental influences is in the opposite direction as the total correlation. A = additive genetics, C = shared or common environment, E = nonshared environment. DAS = Dyadic Adjustment Scale; CES-D = Center for Epidemiologic Studies Depression Scale; BAI = Beck Anxiety Inventory.
p < .05.
In the model examining the correlation between partner-reported dyadic adjustment and depressive symptoms (Figure 1ii), we were able to constrain parameters across gender without reducing model fit, Δχ2(10)=13.32, p=.206. Thus, we report results from a gender-invariant model, χ2(44)=49.43, p=.265, CFI=.940, RMSEA=.030 [.000, .067]. As with the model examining twin-reported dyadic adjustment, we found evidence of nonshared environmental influences on the correlation between dyadic adjustment and depressive symptoms. Sixty-two percent of the correlation between partner-reported dyadic adjustment and depressive symptoms was explained by nonshared environmental factors (Table 4). Together, these results suggest that nonshared environmental factors, rather than genetic or shared environmental confounds, primarily explain the association between dyadic adjustment and depressive symptoms. These results are consistent with a potentially causal association between dyadic adjustment and depressive symptoms.
3.1.2 Dyadic adjustment and anxiety symptoms
The Cholesky decompositions for dyadic adjustment and anxiety symptoms are depicted in Figure 2. Constraining parameters to be equal across gender did not significantly reduce model fit for the model examining twin-reported dyadic adjustment, Δχ2(9)=10.35, p=.323. Thus, we report results from a gender invariant model, χ2(61)=68.73, p=.232, CFI=.947, RMSEA=.031 [.000, .063] (Figure 2i), which suggest that there are nonshared environmental influences common to both twin-reported dyadic adjustment and anxiety symptoms. Fifty-three percent of the correlation between twin-reported dyadic adjustment and anxiety symptoms was explained by nonshared environmental influences, and the remaining 47% was explained by additive genetic influences (Table 4).
A model examining genetic and environmental influences on partner-reported dyadic adjustment and anxiety symptoms resulted in similar results. Constraining paths to be equal did not significantly reduce model fit for the model examining partner-reported dyadic adjustment, χ2(9) = 9.82, p = .365; this gender invariant model is depicted in Figure 2ii, χ2(61)=57.36, p=.608, CFI=1.00, RMSEA=.000 [.000, .047]. Results from this model were consistent with the twin-reported dyadic adjustment model, with 73% of the dyadic adjustment–anxiety symptom correlation explained by nonshared environmental influences (Table 4). As was true for depressive symptoms, evidence of common nonshared environmental influences is consistent with a potentially causal association between dyadic adjustment and anxiety symptoms. However, we note that the nonshared environmental covariance path was .02 in women and −.24 in men, and equating this single parameter did lead to a significant decrement in fit χ2(1) = 5.64, p = .02; Figure 2iii depicts the model with separate parameters for men and women. In women, there was not adequate power to determine whether the correlation between partner-reported dyadic adjustment and anxiety symptoms is due to genetic vs. environmental influences, whereas in men, the correlation due to nonshared environmental influences was statistically significant (Table 4).
Finally, we examined whether the strong correlation between depressive and anxiety symptoms was explained by dyadic adjustment by conducting a trivariate Cholesky model examining dyadic adjustment, depression, and anxiety. The parameters could be constrained across gender without significant decrement in fit, both in the model examining twin-reported dyadic adjustment, χ2(18)=20.06, p=.33, and the model examining partner-reported dyadic adjustment, χ2(19)=24.79, p=.17. The correlation between depression and anxiety symptoms (r=.55, p < .001) was not explained significantly by either twin-reported dyadic adjustment (r=.10, p=.99) or partner-reported dyadic adjustment (r=−.02, p=.76).
4. Discussion
This study examined genetic and environmental influences on the covariation between dyadic adjustment and symptoms of depression and anxiety in a sample of Swedish male and female twins and their spouse or long-term partner. The use of a genetically informative sample allowed us to conduct several analyses to test causal inferences between dyadic adjustment and psychopathology in relationship partners (Rutter, 2007). First, consistent with a potential causal hypothesis (De Moor et al., 2008), within-pair differences in dyadic adjustment were significantly correlated with within-pair differences in depressive and anxiety symptoms in MZ twins, except for the correlation between the within-pair difference in partner-reported dyadic adjustment and anxiety in women. Second, consistent with the hypothesis that poor relationship functioning may be causally associated with psychopathology, we found negative associations between dyadic adjustment and both depressive and anxiety symptoms, and results suggest that these associations were largely due to nonshared environmental factors. A significant nonshared environmental influence on the correlation between dyadic adjustment and depressive or anxiety symptoms provides evidence consistent with a quasi-causal effect of one variable on the other after accounting for unmeasured genetic and shared environmental confounds (Turkheimer & Harden, 2014). Third, if a variable is causally associated with another variable, then genetic and environmental influences on the predictor variable will also, through the causal chain, influence the outcome variable (De Moor et al., 2008). In general, results indicated the genetic and environmental influences on dyadic adjustment also had an influence on depressive or anxiety symptoms. In the following paragraphs, we elaborate on these results and their implications.
We found that dyadic adjustment was significantly and negatively correlated with depressive symptoms, which is consistent with what has been found in prior studies (Proulx et al., 2007; Whisman, 2001). Nonshared environmental influences accounted for 60% and 54% of the correlation between dyadic adjustment and depressive symptoms in men and women, respectively. These results are consistent with results obtained in an independent sample of Swedish female twins (Spotts et al., 2004) and a sample of Australian male and female twins (Beam et al. 2014). In men, there were significant genetic influences on dyadic adjustment, which also significantly influenced depressive symptoms. Turning to the results for partners’ reports of dyadic adjustment, there was a significant negative correlation between partners’ dyadic adjustment and twins’ depressive symptoms, and nonshared environmental influences accounted for most (62%) of this correlation. The finding that similar results were obtained with twins and partners’ report of dyadic adjustment suggest that the results obtained for twins is not the result of reporter bias. It may be that the source of the nonshared environmental influences that affect twins’ depression are also contributing to how both partners feel about their relationship (Spotts et al., 2004). There was also a trend of genetic influences on partners’ dyadic adjustment, which did not have a significant influence on twins’ reports of depressive symptoms.
With respect to anxiety, dyadic adjustment was significantly and negatively correlated with anxiety symptoms, consistent with prior studies (Leach et al., 2013). Nonshared environmental influences accounted for most (i.e., 53%) of the association between twins’ reports of dyadic adjustment and anxiety symptoms. It also accounted for most (i.e., 73%) of the association between partners’ reports of dyadic adjustment and twins’ report of anxiety symptoms, although this evidence may be limited to men. Similarly, a longitudinal study of marital adjustment and psychopathology found poor marital adjustment was prospectively associated with symptoms of generalized anxiety disorder in men but not women (Whisman et al., in press). Older men report receiving most emotional support from their wives, whereas older women report receiving most emotional support from their children, friends, and relatives (Gurung et al., 2003), which may partially explain why nonshared environmental influences accounted for most of the correlation between dyadic adjustment and anxiety symptoms only in men. There were significant genetic influences on twin-reported dyadic adjustment and a trend for genetic influences on partner-reported dyadic adjustment, but these did not have significant influences on anxiety symptoms.
In summary, there was evidence consistent with the perspective that nonshared environmental influences on dyadic adjustment may be causally associated with symptoms of both depression and anxiety. Characteristics of partners (i.e., differences between partners of Twin 1 and Twin 2) may be a major source of this nonshared environmental influence (Spotts et al., 2004). In a study on psychological characteristics of spouses of twins, including personality, interests, and talents, there was little similarity between the spouse of Twin 1 and the spouse of Twin 2 (i.e., spouse-spouse pairs), and MZ spouse-spouse pairs were no more similar than DZ spouse-spouse pairs (Lykken and Tellegen, 1993). Another study found evidence for greater similarity between spouses of twins, but little evidence for similarity between spouses on characteristics known to be important risk factors for both poor marital adjustment and psychopathology (Philippe Rushton and Ann Bons, 2005). These results suggest that partners of twins may not be very similar to one another, and as such, may substantially contribute to the nonshared environmental influences on differences that exist between twins in levels of depressive or anxiety symptoms. In addition, there may be other sources of common nonshared environmental influences between dyadic adjustment and depressive and anxiety symptoms, such as stressful life events or, because all participants were parents, characteristics of children.
In interpreting the study findings, it is important to consider several strengths and limitations. One strength of the study was the inclusion of both male and female twins, which allowed us to test for gender differences. Another strength was that both twins and their partners completed measures of dyadic adjustment. Although the correlation between twins and their partners was large (r=.58), it was not a perfect correlation, which supports our decision to model the associations between twins’ symptoms and both twins’ and partners’ reports of dyadic adjustment. Because results were generally consistent for analyses involving twins’ versus partners’ report of dyadic adjustment, the association between dyadic adjustment and psychopathology cannot be explained solely by method covariance. There are also several limitations of the study. Most importantly, findings are cross-sectional. Stronger evidence for causation would be obtained through longitudinal studies, in which researchers test whether dyadic adjustment is prospectively associated with symptoms of psychopathology in MZ and DZ twins and the magnitude of genetic and environmental influences on the prospective association. Also, power to detect gender differences in parameters was low.
Additional research is needed on the association between dyadic adjustment and other forms of psychopathology in genetically informative samples. For example, the measure of anxiety used in the current study – the BAI – largely consists of somatic items, and may be best conceptualized as a measure of panic symptoms (Leyfer et al., 2006). Therefore, research involving genetically informative samples is needed on dyadic adjustment and general measures of anxiety and symptoms of other anxiety disorders. For example, marital adjustment is prospectively associated with symptoms of generalized anxiety disorder (Whisman et al., in press) and incidence of social phobia (Overbeek et al., 2006), suggesting that it may be fruitful to examine the association between dyadic adjustment and these anxiety disorders in genetically informative samples. Finally, it will be important to examine other relationship parameters, including relationship status and aspects of relationship functioning other than relationship quality, in genetically informative samples to fully understand how relationships influence and are influenced by psychopathology. For example, a longitudinal twin study of marriage and desistance of antisocial behavior found evidence for selection (i.e., men less inclined toward antisocial behavior were more likely to marry) and causation (i.e., married twins engaged in less antisocial behavior following marriage relative to unmarried co-twins) (Burt et al., 2010).
In summary, results from this sample of Swedish male and female twins and their spouse or long-term partner are consistent with prior twin studies in suggesting that dyadic adjustment may be causally associated with symptoms of depression, and extend prior research by including both women and men and examining data on dyadic adjustment for both partners. In addition, the current findings are the first to demonstrate support for a potential causal association between dyadic adjustment and anxiety symptoms in both women and men using a genetically informative sample. The use of a genetically informative sample of twins allowed us to account for unmeasured genetic and shared environmental confounds, which provides an important advance in enhancing understanding the nature of the association between dyadic adjustment and both depression and anxiety. Furthermore, in suggesting that nonshared environmental influences may largely account for this covariation, which may be due to partner characteristics, these results have important clinical implications. Specifically, findings suggest that changing partner characteristics, could result in changes in psychopathology. As such, couple-based interventions that target changing behavior (e.g., enhancing communication) and thereby improving dyadic adjustment may be effective in preventing and treating depression and anxiety. Indeed, a growing literature suggests that couple-based interventions are effective in treating psychopathology (Whisman, 2013; Whisman and Baucom, 2012). The current findings support continued research on the role of dyadic adjustment in the onset and course of psychopathology and the use of couple-based treatments for the prevention and treatment of psychopathology.
Highlights.
Examined dyadic adjustment, depression, and anxiety in female and male twins.
Dyadic adjustment was negatively correlated with depressive and anxiety symptoms.
Similar results were obtained using partners’ report of dyadic adjustment.
Common nonshared environmental influences between dyadic adjustment and symptoms.
Partners’ characteristics may influence dyadic adjustment, depression, and anxiety.
Limitations.
Longitudinal research in genetically informative samples would provide a stronger test of the causal association between dyadic adjustment and psychopathology.
Acknowledgments
Role of the funding source:
This work was supported by the National Institutes of Health [grant numbers MH016880 and MH054610]. The funding source had no role in the study design; in the collection, analysis and interpretation of the data; or in the decision to submit the article for publication.
None
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The current sample is completely independent of the sample used by Spotts et al. (2004a).
Power was calculated by obtaining the predicted covariance matrix from the model allowing gender-specific parameters, then estimating the model with the gender-constrained parameters using the predicted covariance matrix as the sample data. This process could not be used for models examining anxiety; Mplus does not allow an analysis of a covariance matrix when categorical variables and multiple groups are analyzed.
Both models examining dyadic adjustment and depressive symptoms resulted in a warning that the first-order derivative product matrix was non-positive definite. Further examination of parameter estimates indicated that the unique shared environmental influences on CES-D were zero in both men and women. Thus, for both models, we fixed these estimates to be zero.
Contributors:
Mark Whisman developed the study concept and assisted in writing the manuscript; Alta du Pont and Soo Rhee conducted the data analyses and assisted in writing the manuscript; Erica Spotts Paul Lichtenstein, Jody Ganiban, David Reiss, and Jenae Neiderhiser provided critical and meaningful feedback for revision of the manuscript. All authors contributed to and have approved the final manuscript.
Conflict of Interest
All authors declare that they have no conflicts of interest.
References
- Beach SRH, Katz J, Kim S, Brody GH. Prospective effects of marital satisfaction on depressive symptoms in established marriages: A dyadic model. Journal of Social and Personal Relationships. 2003;20:355–371. [Google Scholar]
- Beach SRH, Sandeen EE, O'Leary KD. Depression in marriage: A model for etiology and treatment. Guilford Press; New York: 1990. [Google Scholar]
- Beach SRH, Whisman MA. Affective disorders. Journal of Marital and Family Therapy. 2012;38:201–219. doi: 10.1111/j.1752-0606.2011.00243.x. [DOI] [PubMed] [Google Scholar]
- Beam CR, Horn EE, Hunt SK, Emery RE, Turkheimer E, Martin N. Revisiting the effect of marital support on depressive symptoms in mothers and fathers: A genetically informed study. Journal of Family Psychology. 2011;25:336–344. doi: 10.1037/a0023758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Sage; Newbury Park, CA: 1993. pp. 136–162. [Google Scholar]
- Burmeister M, McInnis MG, Zollner S. Psychiatric genetics: Progress amid controversy. Nature Reviews Genetics. 2008;9:527–540. doi: 10.1038/nrg2381. [DOI] [PubMed] [Google Scholar]
- Burt SA, Donnellan MB, Humbad MN, Hicks BM, McGue M, Iacono WG. Does marriage inhibit antisocial behavior?: An examination of selection vs causation via a longitudinal twin design. Archives of General Psychiatry. 2010;67:1309–1315. doi: 10.1001/archgenpsychiatry.2010.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao H, Zhou N, Fang X, Fine M. Marital well-being and depression in Chinese marriage: Going beyond satisfaction and ruling out critical confounders. Journal of Family Psychology. 2017 doi: 10.1037/fam0000312. [DOI] [PubMed] [Google Scholar]
- Davila J, Karney BR, Hall TW, Bradbury TN. Depressive symptoms and marital satisfaction: Within-subject associations and the moderating effects of gender and neuroticism. Journal of Family Psychology. 2003;17:557–570. doi: 10.1037/0893-3200.17.4.557. [DOI] [PubMed] [Google Scholar]
- De Moor MHM, Boomsma DI, Stubbe JH, Willemsen G, de Geus EJC. Testing causality in the association between regular exercise and symptoms of anxiety and depression. Archives of General Psychiatry. 2008;65:897–905. doi: 10.1001/archpsyc.65.8.897. [DOI] [PubMed] [Google Scholar]
- Derks EM, Dolan CV, Boomsma DI. Effects of censoring on parameter estimates and power in genetic modeling. Twin Research. 2004;7:659–669. doi: 10.1375/1369052042663832. [DOI] [PubMed] [Google Scholar]
- Enders CK. A primer on maximum likelihood algorithms available for use with missing data. Structural Equation Modeling. 2001;8:128–141. [Google Scholar]
- Fydrich T, Dowdall D, Chambless DL. Reliability and validity of the Beck Anxiety Inventory. Journal of Anxiety Disorders. 1992;6:55–61. [Google Scholar]
- Gurung RAR, Taylor SE, Seeman TE. Accounting for changes in social support among married older adults: Insights from the MacArthur Studies of Successful Aging. Psychology and Aging. 2003;18:487–496. doi: 10.1037/0882-7974.18.3.487. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3:424–453. [Google Scholar]
- Irons DE, Iacono WG, McGue M. Tests of the effects of adolescent early alcohol exposures on adult outcomes. Addiction. 2015;110:269–278. doi: 10.1111/add.12747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouros CD, Papp LM, Cummings EM. Interrelations and moderators of longitudinal links between marital satisfaction and depressive symptoms among couples in established relationships. Journal of Family Psychology. 2008;22:667–677. doi: 10.1037/0893-3200.22.5.667. [DOI] [PubMed] [Google Scholar]
- Leach LS, Butterworth P, Olesen SC, Mackinnon A. Relationship quality and levels of depression and anxiety in a large population-based survey. Social Psychiatry and Psychiatric Epidemiology. 2013;48:417–425. doi: 10.1007/s00127-012-0559-9. [DOI] [PubMed] [Google Scholar]
- Leyfer OT, Ruberg JL, Woodruff-Borden J. Examination of the utility of the Beck Anxiety Inventory and its factors as a screener for anxiety disorders. Journal of Anxiety Disorders. 2006;20:444–458. doi: 10.1016/j.janxdis.2005.05.004. [DOI] [PubMed] [Google Scholar]
- Loehlin JC. The Cholesky approach: A cautionary note. Behavior Genetics. 1996;26:65–69. [Google Scholar]
- Lykken DT, Tellegen A. Is human mating adventitious or the result of lawful choice? A twin study of mate selection. Journal of Personality and Social Psychology. 1993;65:56–68. doi: 10.1037//0022-3514.65.1.56. [DOI] [PubMed] [Google Scholar]
- McLeod JD. Anxiety disorders and marital quality. Journal of Abnormal Psychology. 1994;103:767–776. doi: 10.1037//0021-843x.103.4.767. [DOI] [PubMed] [Google Scholar]
- McNamee R. Confounding and confounders. Occupational and Environmental Medicine. 2003;60:227–234. doi: 10.1136/oem.60.3.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McShall JR, Johnson MD. The association between relationship distress and psychopathology is consistent across racial and ethnic groups. Journal of Abnormal Psychology. 2015;124:226–231. doi: 10.1037/a0038267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 7. Authors; Los Angeles, CA: 1998–2015. [Google Scholar]
- Neale MC, Cardon LR. Methodology for genetic studies of twins and families. Kluwer Academic Publishers; Doordrecht, The Netherlands: 1992. [Google Scholar]
- Neiderhiser JM, Lichtenstein P. The Twin and Offspring Study in Sweden: Advancing our understanding of genotype-environment interplay by studying twins and their families. Acta Psychologica Sinica. 2008;40:1116–1123. [Google Scholar]
- Overbeek G, Vollebergh W, de Graaf R, Scholte R, de Kemp R, Engels R. Longitudinal associations of marital quality and marital dissolution with the incidence of DSM-III-R disorders. Journal of Family Psychology. 2006;20:284–291. doi: 10.1037/0893-3200.20.2.284. [DOI] [PubMed] [Google Scholar]
- Pankiewicz P, Majkowicz M, Krzykowski G. Anxiety disorders in intimate partners and the quality of their relationship. Journal of Affective Disorders. 2012;140:176–180. doi: 10.1016/j.jad.2012.02.005. [DOI] [PubMed] [Google Scholar]
- Philippe Rushton J, Ann Bons T. Mate choice and friendship in twins: Evidence for genetic similarity. Psychological Science. 2005;16:555–559. doi: 10.1111/j.0956-7976.2005.01574.x. [DOI] [PubMed] [Google Scholar]
- Proulx CM, Helms HM, Buehler C. Marital quality and personal well-being: A meta-analysis. Journal of Marriage and Family. 2007;69:576–593. [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rutter M. Proceeding from observed correlation to causal inference: The use of natural experiments. Perspectives on Psychological Science. 2007;2:377–395. doi: 10.1111/j.1745-6916.2007.00050.x. [DOI] [PubMed] [Google Scholar]
- Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–514. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family. 1976;38:15–28. [Google Scholar]
- Spanier GB. Dyadic Adjustment Scale manual. Multi- Health Systems, Inc.; North Tonawanda, NY: 1989. [Google Scholar]
- Spotts EL, Neiderhiser JM, Ganiban J, Reiss D, Lichtenstein P, Hansson K, Cederblad M, Pedersen NL. Accounting for depressive symptoms in women: A twin study of associations with interpersonal relationships. Journal of Affective Disorders. 2004a;82:101–111. doi: 10.1016/j.jad.2003.10.005. [DOI] [PubMed] [Google Scholar]
- Spotts EL, Neiderhiser JM, Towers H, Hansson K, Lichtenstein P, Cederblad M, Pedersen NL, Reiss D. Genetic and environmental influences on marital relationships. Journal of Family Psychology. 2004b;18:107–119. doi: 10.1037/0893-3200.18.1.107. [DOI] [PubMed] [Google Scholar]
- Spotts EL, Prescott C, Kendler K. Examining the origins of gender differences in marital quality: A behavior genetic analysis. Journal of Family Psychology. 2006;20:605–613. doi: 10.1037/0893-3200.20.4.605. [DOI] [PubMed] [Google Scholar]
- Turkheimer E, Harden KP. Behavior genetic research methods: Testing quasi-causal hypotheses using multivariate twin data. In: Reis HT, Judd CM, editors. Handbook of research methods in social and personality psychology. 2. Cambridge University Press; New York: 2014. pp. 159–187. [Google Scholar]
- Vento PWPD, Cobb RJ. Chronic stress as a moderator of the association between depressive symptoms and marital satisfaction. Journal of Social and Clinical Psychology. 2011;30:905–936. [Google Scholar]
- Whisman MA. Marital dissatisfaction and psychiatric disorders: Results from the National Comorbidity Survey. Journal of Abnormal Psychology. 1999;108:701–706. doi: 10.1037//0021-843x.108.4.701. [DOI] [PubMed] [Google Scholar]
- Whisman MA. The association between depression and marital dissatisfaction. In: Beach SRH, editor. Marital and family processes in depression: A scientific foundation for clinical practice. American Psychological Association; Washington, DC: 2001. pp. 3–24. [Google Scholar]
- Whisman MA. Marital distress and DSM-IV psychiatric disorders in a population-based national survey. Journal of Abnormal Psychology. 2007;116:638–643. doi: 10.1037/0021-843X.116.3.638. [DOI] [PubMed] [Google Scholar]
- Whisman MA. Relationship discord and the prevalence, incidence, and treatment of psychopathology. Journal of Social and Personal Relationships. 2013;30:163–170. [Google Scholar]
- Whisman MA, Baucom DH. Intimate relationships and psychopathology. Clinical Child and Family Psychology Review. 2012;15:4–13. doi: 10.1007/s10567-011-0107-2. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Bruce ML. Marital dissatisfaction and incidence of major depressive episode in a community sample. Journal of Abnormal Psychology. 1999;108:674–678. doi: 10.1037//0021-843x.108.4.674. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Robustelli BL, Labrecque LT. Specificity of the association between marital discord and longitudinal changes in symptoms of depression and generalized anxiety in The Irish Longitudinal Study on Ageing. Family Process. doi: 10.1111/famp.12351. in press. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Sheldon CT, Goering P. Psychiatric disorders and dissatisfaction with social relationships: Does type of relationship matter? Journal of Abnormal Psychology. 2000;109:803–808. doi: 10.1037//0021-843x.109.4.803. [DOI] [PubMed] [Google Scholar]
- Whisman MA, South SC. Gene–environment interplay in the context of romantic relationships. Current Opinion in Psychology. 2017;13:136–141. doi: 10.1016/j.copsyc.2016.08.002. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Uebelacker LA. Prospective associations between marital discord and depressive symptoms in middle-aged and older adults. Psychology and Aging. 2009;24:184–189. doi: 10.1037/a0014759. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Uebelacker LA, Tolejko N, Chatav Y, McKelvie M. Marital discord and well-being in older adults: Is the association confounded by personality? Psychology and Aging. 2006;21:626–631. doi: 10.1037/0882-7974.21.3.626. [DOI] [PubMed] [Google Scholar]
- Whitton SW, Stanley SM, Markman HJ, Baucom BR. Women’s weekly relationship functioning and depressive symptoms. Personal Relationships. 2008;15:533–550. [Google Scholar]