Abstract
Improved, innovative strategies are needed for the prevention and promotion of recovery from mental illness as these disorders leading cause of disability worldwide. This article will review the evidence linking dietary pattern to brain-based illnesses and provide an overview of the mechanisms that underlie the association between brain health and the food we eat. Considerations for dietary intervention will be discussed including encouraging a shift towards a traditional or whole foods dietary pattern.
Clinical Vignette
Robert, a 43-year-old married man who presents with irritability and a low mood for two months. He has a history of attention deficit disorder, first diagnosed two years ago, and is currently treated with Vyvanse 70 mg. While his focus and work function are improved, he reports low appetite, fatigue, and difficulty sleeping. He notes that he tends to be quite irritable during mealtimes to the extent that his wife has asked him to stay at work past dinnertime to “stay out of the way.” He feels guilty and, concerned about not connecting emotionally to his young children ages 1 and 3. Further history and medical workup reveal no substance use, no active medical issues, and blood work reveals no abnormalities.
The evidence is growing: food choice is strongly implicated in mental health risk. In cases like Robert’s, a food history is a vital piece of data, both in assessing low appetite as a possible medication side effect, or as a symptom of depression. Furthermore, a food history is imperative to understand whether targeted dietary recommendations could assist in his recovery.
An approach to consider for patients with mental health symptoms is to offer counseling on lifestyle interventions, such as diet.1 Physicians often feel ill-equipped to discuss diet due to lack of training, limited time, and a poor reimbursement structure. Physician uncertainty is likely exacerbated by the wide variety of specific dietary recommendations and dietary “tribes” that exist in our society today. Over 2,000 years ago, Hippocrates said, “let thy food be thy medicine and thy medicine be thy food.”2 The evidence base is increasing that we should re-examine his counsel, as the effect of good food has profound implications for brain health.
The global burden of mental illness, both in terms of financial cost and disability, rivals that of all cancers combined.3,4,5 In addition, unipolar depression is the leading cause of disability in high and middle-income countries. Among individuals aged 15–44, it is the leading cause of disability worldwide.6 In light of this, it is essential to explore strategies that prevent mental disorders.7 While several risk factors such as socioeconomic status and trauma are not amenable to simple interventions, nutrition has a simple appeal: all patients eat. Shifting the diet is not only a means to promote mental health; it is also a way to promote recovery from mental illness once it has already taken hold.8, 9
Several nutritional deficiencies, such as vitamin B12, B9 (folate), and zinc, can cause symptoms of depression and dementia such as low mood, fatigue, cognitive decline, and irritability.10, 11 The evidence linking diet to mental illness has evolved from a focus on specific nutrient deficiencies to an emphasis on overall dietary pattern. Dietary patterns high in processed foods, or a “western dietary pattern,” are strongly correlated with an increased risk of developing depression, mild cognitive impairment, and ADHD.12–14 Food insecurity, or inadequate access to sufficient nutritious and culturally appropriate food, is also independently associated with mood and anxiety disorders.15 On the other hand, a “whole foods,” traditional, and a Mediterranean diet have been found to be protective against developing depression among other mental illnesses.16–18 For instance, a prospective cohort study of over 10,000 university students over 4.4 years of follow up, found that students who most closely adhered to a Mediterranean dietary pattern had a 42% reduced risk of developing depression.19 This research has taken into account several potential confounders including socioeconomic status. What could underlie this connection between mental illness risk and the food we eat?
This is Your Brain on Food
The brain is an organ with very high metabolic and nutrient demands. On average, the brain consumes 20% of a person’s daily caloric intake, approximately 400 calories per day. It is composed of 60% fat, and contains high concentrations of cholesterol and polyunsaturated fatty acids (PUFAs) such as Omega-3s.
Production of monoamine neurotransmitters such as serotonin, norepinephrine, and dopamine, important in the pathophysiology of mental illness, depends on adequate building blocks of amino acids, and mineral dependent co-factors. Folate and other B vitamins are essential for the methylation cycle, which produces a co-factor crucial for monoamine neurotransmitter synthesis, BH-4.20, 21 Proper function of the methylation cycle also reduces homocystiene elevated levels of which are linked to cardiovascular disease and depression.
Omega-3 fatty acids form an integral part of neuronal cell membranes and influence a number of essential processes in the central nervous system. More specifically, they regulate neurotransmission, influence gene expression, and directly effect neurogenesis and neuronal survival. They also act as anti-oxidants and have anti-inflammatory properties.22 Along with omega-3 intake, the balance of omega-6 and omega-3 fatty acids also appears to be relevant. Western diets tend to be abundant in omega-6 fatty acids, and quite low in omega-3s, a phenomenon that has occurred with the shift towards industrialized and processed food.23 Omega-6 fatty acids are the primary fatty acid in many vegetable oils, such a corn oil and soy oil, often the cooking fats of choice in packaged and restaurant food. Long chained omega-3 fatty acids are found in fish, seafood, and grass-fed beef. Typically, these are not foods that come to mind as staples of the standard American diet. Grass fed beef omega-3 content varies greatly, but generally contains 100mg of long-chained omega-3 fatty acids per 100g serving, much less than an equivalent serving of fatty fish.24 This highlights the importance of educating patients about meat quality and alternatives, such as grass-fed beef, which is generally more nutrient dense than conventionally-raised beef.25
Omega-3 fatty acids have been shown to be effective as either stand-alone or adjunctive treatment for ADHD, major depressive disorder, bipolar depression, and PTSD.26, 27 In addition, an elevated omega-6 to omega-3 fatty acid ratio in the blood has been associated with major depressive disorder and ADHD.28, 29 There is some evidence that reducing the omega-6 to omega-3 ratio with omega-3 supplements lead to improvement in symptoms of ADHD.30 Several possible biological mechanisms underlie these associations, i.e., the same enzymes are required to convert both short chain omega-3 and omega-6 fatty acids to their long chain biologically active versions. Thus, excess omega-6 could interfere with the production of omega-3s by limiting the conversion to the longer chain forms.23
As part of the clinical assessment, you decide to engage Robert in a discussion about food and complete a dietary history. Robert admits that he is not generally hungry in the morning and tends to skip breakfast. Lunch is often rushed, and he usually consumes a bowl of cold cereal with skim milk at his desk. Dinner is quite variable and snacks consist of crackers or low-fat granola bars.
These foods are not rich sources of nutrients crucial for brain health. When considering brain health, fish and seafood are among the most nutrient dense foods that one can eat. This food category is rich in all of the nutrients discussed so far namely: omega-3 fatty acids and B vitamins. Is Robert eating any fish or seafood? It may be reasonable to consider asking him this question. Moreover, greens such as kale, beans, and legumes are excellent sources of folate, as are fiber, and B-vitamins. Are these foods part of his diet?
Inflammation may play an important role in mediating the link between diet and mental health.31 Multiple lines of research support the pathogenic role of neuroinflammation in mental illness.32 Lucas et al. (2014) used several inflammatory biomarkers including CRP, TNF alpha receptor 2, and IL-6 and data from food frequency questionnaires to derive an inflammatory dietary pattern from a sample of over 12,000 participants from the Nurses Health Study. Participants who consumed a diet consistent with the inflammatory dietary pattern had a statistically significant increased risk of developing depression over time after adjusting for multiple confounders.33 Specifically, over twelve years of follow up, participants with the highest adherence to the inflammatory dietary pattern had a relative risk of 1.41 (1.22–1.63) of developing depression according to the strict definition (physician diagnosis and anti-depressant use). The inflammatory dietary pattern was high in in sugar-sweetened soft drinks, refined grains, red meat, diet soft drinks, and margarine and low in wine, coffee, olive oil, green leafy, and yellow vegetables.
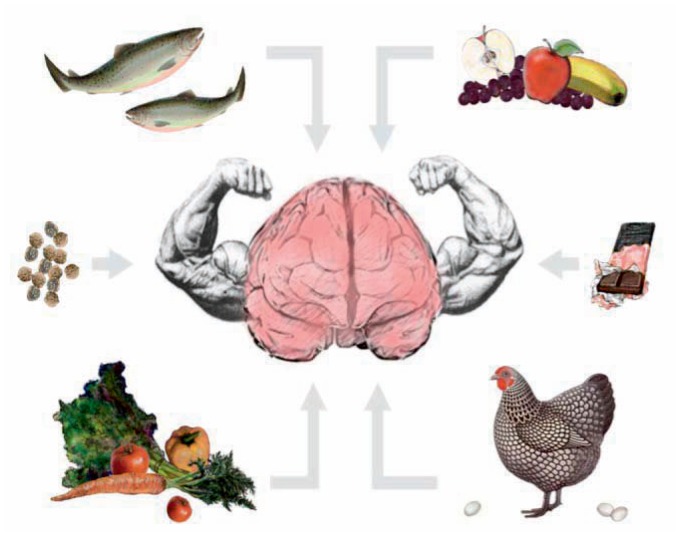
Figure credit Mala Nimalasuriya
Any mention of olive oil, wine, and vegetables when speaking about nutrition leads to thoughts about the Mediterranean diet. This dietary pattern is based on the traditional cooking style of countries bordering the Mediterranean Sea and is rich in fish, olive oil, legumes, and whole grains. It also contains small, but regular amounts of red wine, cheese, and yogurt. The Mediterranean diet has been associated with decreased incidence and prevalence of depression.34 In an attempt to explore the potential mechanisms to explain this association, one research group looked at brain derived neurotrophic factor or BDNF.
BDNF is an important neurochemical that is active in many areas of the brain. It plays a role in many crucial functions such as neuroplasticity, neuronal survival, and growth and differentiation of new neurons and synapses.
Low serum levels of BDNF have been found in a number of mental disorders including major depressive disorder, PTSD, Schizophrenia, and Alzheimer’s dementia.35–38 BDNF has also been implicated in the mechanism of action of anti-depressant medications.39 One prospective study examined the impact of diet on plasma BDNF levels in humans. Participants were randomized to follow one of three diets: the American Heart Association guidelines, a Mediterranean diet augmented with olive oil, and a Mediterranean diet augmented with nuts. After three years of follow up, the Mediterranean diet with nuts group had a relative risk of 0.22 (0.05–0.90) of having a very low plasma BDNF level. What is more, individuals in this group who had depression at baseline had significantly higher mean plasma levels of BDNF at the end of the study.40
Another aspect on the frontier of the link between diet and mental health is the microbiome. Fermented foods have been part of the human diet since the Paleolithic period and they remain part of the dietary practices of most known traditional diets today.41
These types of foods are commonly referred to as probiotic since they contain microorganisms that positively influence health. Prebiotics, on the other hand include non-digestible fiber, which stimulates the growth and or activity of these beneficial microorganisms. The impact of the microbiome on mental health is an emerging area of research42 that is beyond the scope of this article. Suffice it to say that the microbiome provides another link between diet and mental health since short-term dietary changes can induce species level changes to intestinal microbes.43
Therefore, it appears that dietary pattern can influence mental health through a number of mechanisms. Basic building blocks of the brain such as monoamine neurotransmitters, myelin, and neuronal membranes depend on adequate nutrient intake. Food choice influences neuroplastic processes via effects on BDNF expression and systemic inflammation via omega-3 to omega-6 ratio. Finally, food is the primary arbiter of the microbiome, an emerging area of research in general and mental health.
Summary
In order to promote mental health and recovery from mental illness, one could consider encouraging patients to eat a diet that is optimal for brain health. Specifically, this diet would include adequate building blocks for monoamine neurotransmitters, be rich in omega-3 fatty acids, be anti-inflammatory, foster BDNF production, and support a healthy microbiome. While this might seem to be very ambitious goal, many traditional diets are based on nutrient dense whole foods and contain all of these nutrients. The Mediterranean diet is an accessible template, but it is only one example.
Robert is provided with education regarding the importance of adequate nutrition for his mental health and encouraged to make some changes to his diet in line with the considerations discussed above. He is glad to hear about steps he can take on his own to improve his mental wellbeing and his self-efficacy increases. You work with Robert to find some nutrient-dense and convenient breakfast options such as scrambled eggs or a nutrient-dense smoothie. He decides to start eating breakfast.
A few weeks later in follow-up, Robert states that despite not feeling hungry when he wakes up, he feels subjectively better ten minutes or so after having breakfast. He also introduces nuts as snacks, instead of crackers and low-fat granola bars, and has started to pack a fruit or vegetable to eat with his lunch. Robert’s irritability improves. It is possible that the stimulant medication is suppressing his appetite and his irritability was due to hypoglycemia. Upon further clinical evaluation, Robert endorses some residual depressive symptoms and you recommend a trial of anti-depressant medication. Robert has had one previous depressive episode; however, he did not find medication to be helpful at that time. He is somewhat hesitant but consents to a trial of medication.
After six weeks of treatment with medication and ongoing food intervention, Robert’s depressive symptoms have significantly improved. He feels less irritable at mealtimes, is enjoying spending time with his children more, and is having less conflict with his wife. He is feeling positive about the direction his life is heading, and plans to continue to pay attention to his food choices.
Helping patients to eat a diet that is rich in brain food – fish, seafood, beans & legumes, leafy greens and other vegetables, olive oil (monounsaturated fat), yogurt, nuts – can be an effective and relatively simple way to promote mental health and recovery from mental illness that can easily be integrated into health care. Possible side effects and food-medicine interactions, for example leafy greens and wafarin, should be considered. That being said, the side effects in the case of nutritional counseling can include increased self-efficacy and improved physical health. Two more reasons to consider this foundational intervention: talking to our mental health patients about food.
Biography
Laura Lachance, MD, (left) is at the University of Toronto. Drew Ramsey, MD, (right) is Assistant Clinical Professor of Psychiatry at Columbia University College of Physicians and Surgeons in New York, NY.
Contact: laura.lachance@utoronto.ca

Footnotes
Disclosure
None reported.
References
- 1.Sanchez-Villegas A, Martínez-Gonzáez M. Diet, a new target to prevent depression? Metabolism, Diet, and Disease. 2013;11(3) doi: 10.1186/1741-7015-11-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Graham T, Ramsey D. The Happiness Diet: A Nutritional Prescription for a Sharp Brain, Balanced Mood, and Lean, Energized Body: Rodale. 2011 [Google Scholar]
- 3.Murray C, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010 a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2010;380(9859):2197–223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 4.Bloom D, Cafiero E, Jané-Llopis E, et al. The global economic burden of noncommunicable diseases. Program on the Global Demography of Aging. 2012:8712. [Google Scholar]
- 5.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020 Global Burden of Disease Study. The Lancet. 349(9064):1498–504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 6.Mathers C, Fat DM, Boerma J. The global burden of disease: 2004 update. World Health Organization; 2008. [Google Scholar]
- 7.Author. Changing directions, changing lives: The mental health strategy for Canada. Calgary, AB: Mental Health Commission of Canada; 2012. [Google Scholar]
- 8.Sarris J, Logan A, Akbaraly T, et al. Consensus Statement ed. 2014. Nutritional Medicine as Mainstream in Psychiatry: A Consensus Position Statement from the International Society for Nutritional Psychiatry Research (ISNPR) [Google Scholar]
- 9.Rucklidge J, Johnstone J, Kaplan B. Single bullet madness–why do we continue to perpetuate this fallacy. Br J Psychiatry. 2013;203:154–5. doi: 10.1192/bjp.203.2.154. [DOI] [PubMed] [Google Scholar]
- 10.Sensi S, Paoletti P, Koh J, Aizenman E, Bush A, Hershfinkel M. The Neurophysiology and Pathology of Brain Zinc The Journal of Neuroscience. 2011;31(45):16076–85. doi: 10.1523/JNEUROSCI.3454-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Skarupski K, Tangney C, Li H, Ouyang B, Evans D, Morris M. Longitudinal association of vitamin B-6, folate, and vitamin B-12 with depressive symptoms among older adults over time. The American journal of clinical nutrition. 2010;92(2):330–5. doi: 10.3945/ajcn.2010.29413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Howard A, Robinson M, Smith G, Ambrosini G, JP P, Oddy W. ADHD is associated with a “Western” dietary pattern in adolescents. Journal of attention disorders. 2011;15(5):403–11. doi: 10.1177/1087054710365990. [DOI] [PubMed] [Google Scholar]
- 13.Akbaraly T, Brunner E, Ferrie J, Marmot M, Kivimaki M, Singh-Manoux A. Dietary pattern and depressive symptoms in middle age. The British Journal of Psychiatry. 2009;195(5):408–13. doi: 10.1192/bjp.bp.108.058925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scarmeas N, Luchsinger J, Schupf N, et al. Physical activity, diet, and risk of Alzheimer disease. JAMA. 2009;302(6):627–37. doi: 10.1001/jama.2009.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tarasuk V, Mitchell A, McLaren L, McIntyre L. Chronic Physical and Mental Health Conditions among Adults May Increase Vulnerability to Household Food Insecurity. The Journal of nutrition. 2013;143(11):1785–93. doi: 10.3945/jn.113.178483. [DOI] [PubMed] [Google Scholar]
- 16.Lai J, Hiles S, Bisquera A. A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults. American Journal of Clinical Nutrition. 2013;99(1):181–97. doi: 10.3945/ajcn.113.069880. [DOI] [PubMed] [Google Scholar]
- 17.Pelsser LM, Frankena K, Toorman J, et al. Effects of a restricted elimination diet on the behaviour of children with attention-deficit hyperactivity disorder (INCA study): a randomised controlled trial. The Lancet. 2011;377(9764):494–503. doi: 10.1016/S0140-6736(10)62227-1. [DOI] [PubMed] [Google Scholar]
- 18.J FN, K PJ, MB, dS-S AM, et al. A Prospective Study of Diet Quality and Mental Health in Adolescents. PLoS ONE. 2011;6(9):e24805. doi: 10.1371/journal.pone.0024805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sánchez-Villegas A, Delgado-Rodríguez M, Alonso A, et al. Association of the Mediterranean dietary pattern with the incidence of depression: the Seguimiento Universidad de Navarra/University of Navarra follow-up (SUN) cohort. Archives of General Psychiatry. 2009;66(10):1090–8. doi: 10.1001/archgenpsychiatry.2009.129. [DOI] [PubMed] [Google Scholar]
- 20.Miller A. The methylation, neurotransmitter, and antioxidant connections between folate and depression. Alternative Medicine Review. 2008;13(3):216–26. [PubMed] [Google Scholar]
- 21.Stahl S. L-Methylfolate: A Vitamin for Your Monoamines. Journal of Clinical Psychiatry. 2008;69(9):1352–3. doi: 10.4088/jcp.v69n0901. [DOI] [PubMed] [Google Scholar]
- 22.Zeman M, Jirak R, Vecka M, Raboch J, Zak A. N-3 polyunsaturated fatty acids in psychiatric diseases: Mechanisms and clinical data. Neuroendocrinology Letter. 2012;33(8):736–48. [PubMed] [Google Scholar]
- 23.Simopoulos A. Evolutionary Aspects of Diet: The Omega-6/Omega-3 Ratio and the Brain. Molecular Neurobiology. 2011;44:203–15. doi: 10.1007/s12035-010-8162-0. [DOI] [PubMed] [Google Scholar]
- 24.Nuernberg K, Nuernberg G, Ender K, et al. N-3 fatty acids and conjugated linoleic acids of longissimus muscle in beef cattle. European Journal of Lipid Science and Technology. 2002;104(8):463–71. [Google Scholar]
- 25.Daley CA, Abbott A, Doyle PS, Nader GA, Larson S. A review of fatty acid profiles and antioxidant content in grass-fed and grain-fed beef. Nutrition journal. 2010;9(1):10. doi: 10.1186/1475-2891-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bloch MH, Qawasmi A. Omega-3 fatty acid supplementation for the treatment of children with attention-deficit/hyperactivity disorder symptomatology: Systematic review and meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50(10):991–1000. doi: 10.1016/j.jaac.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mischoulon D, Freeman M. Omega-3 fatty acids in psychiatry. Psychiatric Clinics of North America. 2013;36(1):15–23. doi: 10.1016/j.psc.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 28.Adams P, Lawson S, Sanigorski A, Sinclair A. Arachidonic Acid to Eicosapentaenoic Acid Ratio in Blood Correlates Positively with Clinical Symptoms of Depression. Lipids. 1996;31 doi: 10.1007/BF02637069. [DOI] [PubMed] [Google Scholar]
- 29.Mikirova N, Casciari J, Hunninghake R. The Orthomolecular Correction of Metabolic Imbalances Found in Attention Deficit Hyperactivity Disorder: A Retrospective Analysis in an Outpatient Clinic. 2013;28(2):1–10. [Google Scholar]
- 30.Sorgi P, Hallowell E, HL H, Sears B. Effects of an open-label pilot study with high-dose EPA/DHA concentrates on plasma phospholipids and behavior in children with attention deficit hyperactivity disorder. Nutrition Journal. 2007;6(16) doi: 10.1186/1475-2891-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Galland L. Diet and Inflammation Nutrition in Clinical Practice. 2010;25(6):634–40. doi: 10.1177/0884533610385703. [DOI] [PubMed] [Google Scholar]
- 32.Najjar S, Pearlman D, Alper K, Najjar A, Devinsky O. Neuroinflammation and psychiatric illness. Journal of Neuroinflammation. 2013;10:43. doi: 10.1186/1742-2094-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lucas M, Chocano-Bedoya P, Shulze M, et al. Inflammatory dietary pattern and risk of depression among women. Brain, behavior, and immunity. 2014;36:46–53. doi: 10.1016/j.bbi.2013.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rienks J, Dobson A, Mishra G. Mediterranean dietary pattern and prevalence and incidence of depressive symptoms in mid-aged women: results from a large community-based prospective study. European journal of clinical nutrition. 2013;67(1):75–82. doi: 10.1038/ejcn.2012.193. [DOI] [PubMed] [Google Scholar]
- 35.Bocchio-Chiavetto L, Bagnardi V, Zanardini R, et al. Serum and plasma BDNF levels in major depression: a replication study and meta-analyses. World Journal of Biological Psychiatry. 2010;11(6):763–73. doi: 10.3109/15622971003611319. [DOI] [PubMed] [Google Scholar]
- 36.Faria MC, Goncalves G, Rocha N, et al. Increased plasma levels of BDNF and inflammatory markers in Alzheimer’s disease. Journal of psychiatric research. 2014;53:166–72. doi: 10.1016/j.jpsychires.2014.01.019. [DOI] [PubMed] [Google Scholar]
- 37.Angelucci F, Ricci V, Gelfo F, et al. BDNF serum levels in subjects developing or not post-traumatic stress disorder after trauma exposure. Brain and cognition. 2014;84(1):118–22. doi: 10.1016/j.bandc.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 38.RN, MK, HS BDNF and schizophrenia: from neurodevelopment to neuronal plasticity, learning, and memory. Frontiers in Psychiatry. 2013;4(45) doi: 10.3389/fpsyt.2013.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.EC, Rantamaki T. Role of brain-derived neurotrophic factor in the aetiology of depression: implications for antidepressant treatment. CNS Drugs. 2010;24:1–73. doi: 10.2165/11530010-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 40.Sáchez-Villegas A, Galbete C, Martinez-Gonzáez M, et al. The effect of the Mediterranean diet on plasma brain-derived neurotrophic factor (BDNF) levels: the PREDIMED-NAVARRA randomized trial. Nutritional Neuroscience. 2011;14(5):195–201. doi: 10.1179/1476830511Y.0000000011. [DOI] [PubMed] [Google Scholar]
- 41.Selhub EM, Logan Alan C, Bested Alison C. Fermented foods, microbiota, and mental health: ancient practice meets nutritional psychiatry. Journal of Physiological Anthropology. 2014;33(1):2. doi: 10.1186/1880-6805-33-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cryan J, Dinan T. Mind-Altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nature Reviews Neuroscience. 2012 doi: 10.1038/nrn3346. [DOI] [PubMed] [Google Scholar]
- 43.Bested A, Logan A, Selhub E. Intestinal microbiota, probiotics and mental health: from Metchnikoff to modern advances: Part II – contemporary contextual research. Gut Pathogens. 2013;5(3) doi: 10.1186/1757-4749-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]