Abstract
Our understanding of the dynamic interaction between the eye’s growth and its ability to adapt to maintain vision has shown that childhood myopia is a significant prediction of progressive myopia and the potentially severe ocular comorbidities associated with it. It is important for us to better understand this process and its risk factors in order to better develop a prevention and treatment strategy. This article will discuss the epidemiology, risk factors and current therapeutic regimens for reducing myopic progression.
Background
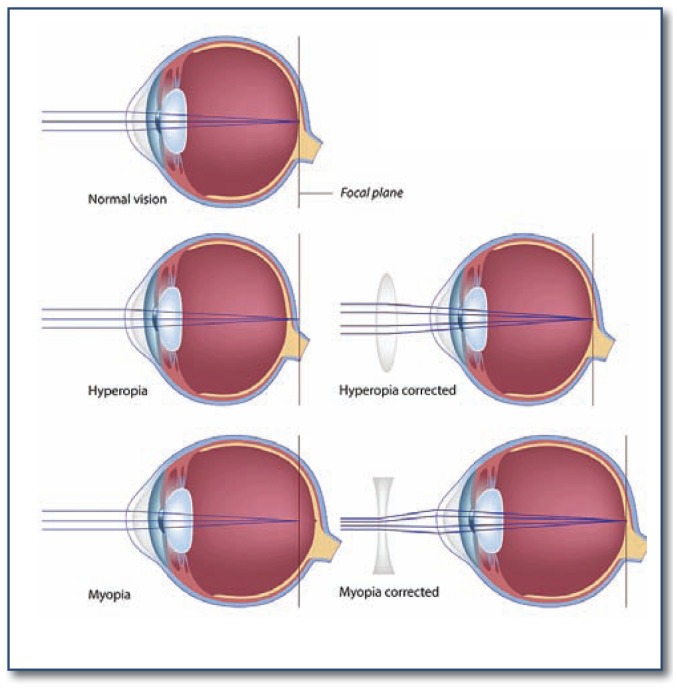
Myopia, or nearsightedness, is a common eye condition in which the image seen by the eye is focused prior to reaching the retina. This produces an unfocused image on the retina and is seen by the patient as a blurred image. In order for an individual to see an object clearly, the image must be projected clearly onto the retina of the eye. Myopia can be optically corrected with glasses to help provide a clear image on the retina. See Figure 1.
Figure 1.
Hyperopia and Myopia
Myopia can be divided into two major categories: refractive and axial. Refractive myopia is due to the focusing power of the eye being abnormally strong and focusing the image in front of the retina. Axial myopia, the more common cause, is due to the axial length of the eye being too long, measured from the cornea to the back of the eye. The normally powered cornea and lens focus the light but the retina is further posterior than the focused image. Animal studies show that the eye is dynamic in managing axial length and optical power in order to maintain a clear image during growth and development. If this autoregulation process is poorly controlled, the eye can elongate out of proportion creating axial myopia.1–3
The process and progression of myopia follows a typical pattern with normal vision at a young age. Starting around school age a myopic shift and rapid increase in myopia begins which continues until late teenage years.4,5 High myopia is associated with significant increased risks for retinal degeneration and detachment, open angle glaucoma, and cataracts at a young age. These associated conditions have a significant lifetime risk of severe visual impairment including blindness.6
Due to the significant risks associated with the development of high myopia, pediatric ophthalmologists have been very interested in the prevention of myopic progression. Recent studies involving drugs and devices have shown that myopic progression can be modulated. We will discuss published literature on the interventions, their risks and efficacy data.
Epidemiology
Prevalence and Incidence
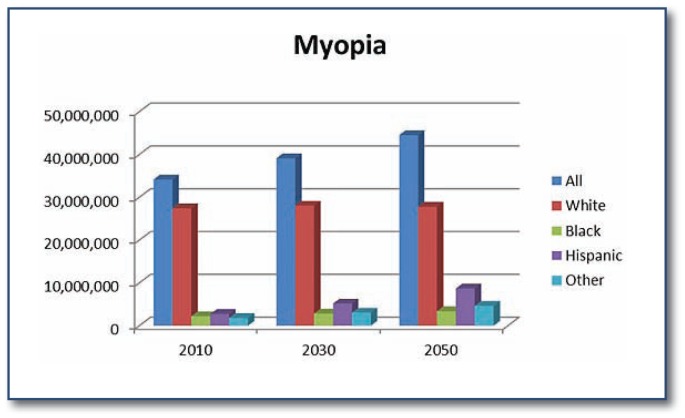
Myopia is an extremely common ocular condition worldwide. See Figure 2. It has been published that the prevalence in Asian populations approaches the rate of 37–60%.8,9 The annual incidence in urban Asian communities has been greater than 14%.10,11 An Australian study found a prevalence of 14.4% and 29.6% in children ages 12 and 17 years, respectively. This same study estimated the annual incidence for the same age groups to be 2.2% and 4.1%, respectively.12 It is has been estimated that myopia affects approximately 25–33% of adults in the United States and Western Europe.13,14 Vitale S. et al. found a 66% increase in the prevalence of myopia in the United States over a 30-year period ending in 2004.15 The Multi-Ethnic Pediatric Eye Disease Study found the prevalence of non-hispanic whites aged 6–72 months in California to be 1.2% while in 3.98% in Asians of the same population.16 The National Health and Nutrition Examination Survey showed that myopia was more common in non-Hispanic whites (35.2%) than in non-Hispanic blacks (28.6%) or Mexican-Americans (25.1%).15 The annual incidence rates of myopia in the United States has been reported as 2.6%17 with children of Euro-Caucasian ethnicity having the lowest odds of incident myopia.12,18
Figure 2.
Projections for Myopia (2010–2030–2050) United States
Risk Factors
Ethnicity
Ethnicity has been looked into as a risk factor for progression due to the higher prevalences and annual incidence rates among Asian populations. Internationally, the annual rate of myopic progression for Singapore has been reported at −0.80 diopters per year,11 while European Caucasian ethnicities report progression rates closer to −0.50 diopters per year.12,19,20 It was shown by Hyman et al. that African-Americans had the least amount of progression after three years compared to Asians, Hispanics, Caucasians, and mixed ethnicities.7 The COMET Group also found that African-Americans stabilized at a younger age (13.82 years) with less absolute myopia at stabilization (−4.36 D). The same study showed that Caucasians took the longest to stabilize (16.32 years) and Asians had the most amount of absolute myopia at stabilization (−5.45 D).4
Age
The most significant predictor of incident myopia is having a less hyperopic refraction at a young baseline age.18 The strongest independent risk factor for myopia progression is having a myopic refraction of at least -1.25 diopters at a young age, particularly at the myopic shift transition point of 6 to 7 years of age. Not only is the endpoint amount of myopia greater in this group, but the rate of progression and axial length elongation is faster.7 The fact that the overall amount of myopia would be greater at stabilization in a young patient with myopia makes intuitive sense but the reason for the rate being faster remains unknown. The COMET Group found that the mean age of stabilization of myopia to be 15.61 years with the average amount of myopia at stabilization to be −4.87 diopters. It was also shown that for every year of delayed stabilization, there was an increase in total amount of myopia (overall 0.27 D more myopia per year delayed).4
Parental Myopia
Studies have shown us that parental myopia, in even one parent, leads to an increased risk for juvenile myopia. It has even been reported that there is greater than a six-fold increased risk of juvenile-onset myopia if both parents are myopic.21 In Austrailia, incident myopia in six-year-old children was increased from 7.8% with no parental myopia to 21.4% and 22.0% with one or both parents having myopia, respectively. This same study found that European Caucasian children with parental myopia had increased incidence of myopia.18
Parental myopia is not only a risk factor for having myopia, but is also a risk factor for progressive myopia in children.22 Saw et al. showed children with at least one myopic parent had increased rates of myopic progression compared to children with no myopic parent (0.63 diopter/ year vs 0.42 diopters/year, respectively).23 This was supported by the COMET group who reported parental myopia was directly related to myopic progression as well as increases in axial length.22
Gender
There is conflicting data when assessing sex predilection of myopia. The COMET study showed that there was no difference between males and females.12,18 The National Health and Nutrition Examination Survey showed that women had a higher prevalence than men for myopia among the 20–40-year-old population (39.9% and 32.6%, respectively, P < .001) but that this was not consistent among other age groups.14
The COMET study’s multivariate analysis found that males have a slower progression rate of myopia than females do,4 which supports the previous conflict of an increased female prevalence of myopia at age 20–39. It is interesting to note that there was no difference in axial length elongation between males and females. The female axial length averaged shorter than males but was compensated by females having steeper, or strong focusing, corneas.
Environmental Factors
Several studies have bern conducted to examine different environmental or non-genetic factors that may factor in the development of myopia. The amount of near work, such as reading or hand-held electronics, a child performs during the day has had weak or no association.23–26 The CLEERE Study Group showed in their longitudinal study that near work activities in children who became myopic did not differ from emmetropic children before myopia, claiming that nearwork cannot be a causative factor for myopia.27 One of the most popular and impactful associations is outdoor time. Many studies have found that outdoor time has a negative, or protective, association with myopia.6, 18, 28 Sherwin et al. performed a meta-analysis to summarize the published reports on the association of outdoor time and myopia in children under 20 years.6 Their results not only confirmed that increasing time spent outdoors reduces the risk of developing myopia, but the pooled information indicated a 2% reduced odds of myopia for each additional hour of time spent outdoors per week. This offers a practical intervention for myopia prevention with the many other health benefits associated with outdoor activities.
There has been much work and investigation into the genetics and inheritance of refractive errors, including myopia, however, there remains much to be learned. It is agreed that there is a genetic and environmental interaction that is involved and our understanding of myopia inheritance will be better understood as these elements are better investigated.21,29
Interventions
The natural progression of myopia and the risk factors associated with it have lead to attempted treatment strategies to not only treat the blurred vision but to prevent the progression of myopia. There are two major therapeutic methods: optical therapy and medication therapy. The following will discuss the more recent and popular researched therapies within each of these categories, but should not be considered a completely inclusive discussion of myopic progression therapy.
Optical Therapies
Bifocals
As discussed previously, the eye can autoregulate its refraction and axial length to attempt a focussed image on the retina. If the eye cannot first adjust its refractive factors, it can elongate to maintain focus.1–3 Bifocals, lined or progressive, can provide a clear image for images at different points, theoretically reducing the need to elongate. In 2011, Leo and Young performed a review of literature and found that randomized, clinical trials in several countries did not show significant slowing of myopia. Progressive lenses were found in many of the studies reviewed to have little significance or insignificant trends slowing progression.1 Most recently, Cheng et al. published a three-year randomized trial that progressive lenses had a significant reduction in the rate of myopic progression in children who were progressing at an already accelerated rate.30 The COMET group did note significant reductions in progression but after further analysis concluded that these reductions were clinically insignificant.19
Orthokeratology
Orthokeratology is a corneal refractive therapy in which the cornea is reshaped using a specifically made hard contact lens in an effort to temporarily flatten the curvature of the cornea, thus lessening the optical power of the cornea and focusing the image onto the retina. These lenses are worn at night and removed during the day.31 Until recently there has been no good long-term data on its effects on myopic progression. Several recent, randomized, clinical trials have shown that orthokeratology can reduce the amount of myopic refractive and axial length progression by 43–63% after two years.32–34 Sample size is a significant limitation to these studies and may skew these results. The smallest study of 28 subjects completing the study had the highest reduction32 and the largest study of less than 80 subjects completing the study had the lowest reduction.33 There is no follow-up data beyond two years or data for the progression rates after cessation of therapy. These studies included children age 6–12 years of age and corrected up to 5 diopters of myopia. The major complications reported by these studies were irregular corneal epithelium, corneal inflammation, and ocular intolerance. A report by the American Academy of Ophthalmology found multiple sight-threatening risks and complications associated with orthokeratology including more than 100 cases of corneal infections.35
Medication Therapies
Atropine
Atropine is a non-selective antimuscarinic with a wide range of effects on the eye, most notably reduction of accommodation and causing pupil dilation (mydriasis). The origin for this treatment of myopia started in the 19th century.1,36 The exact mechanism of atropine for myopia has not been identified, but observations to its effects have been reported through a variety of papers and clinical trials, most of which were limited with short-term data, poor controls, lack of masking, and detailed examinations.37 The ATOM studies37–40 were performed in an effort to assess the effects of atropine on myopic progression as well as side effects with two years of atropine therapy. Children aged 6 to 12 years with low to moderate myopia were randomized into placebo, 1%, 0.5%, 0.1%, and 0.01% atropine. After two years of therapy the atropine groups significantly decreased the rate of myopic progression in a concentration related manner: 77%, 75%, 68%, and 59%, respectively. The differences between the concentrations were considered clinically insignificant. Axial length elongation was also compared and found similar findings though not all concentrations were significant: 100% reduction, 28% reduction, 26% reduction, and 8% more, respectively.37, 39 After the two years, treatment patients stopped therapy and the groups were monitored for progression over the following year. Interestingly, a rebound in progression was found but inversely to the concentration of atropine used: 0.01% atropine with least amount of rebound myopic progression and 1% atropine with the most amount of rebound myopic progression. The total treatment effect of the atropine groups compared to placebo over the three years (two years treatment plus one year no treatment) showed that all atropine groups had less progression but inversely related to the concentrations: 12.5%, 25%, 37.5% and 56.3%, 1% to 0.01% respectively. Interestingly, the average amount of the axial length change over the three years only had a significant change in the 1% atropine group (reduced elongation) when compared to placebo.38,40
Significant visual side effects were mydriasis (pupil dilation), decreased accommodation (ability to adjust focus), and near vision blur from cycloplegia. These were concentration specific with higher concentrations of atropine having more effects and to greater extents than the lower concentrations. In fact, atropine 0.01% had a minimal effect on accommodation and mydriasis and no effect on near vision. All ocular side effects resolved after completion of therapy. The most common side effect was allergic conjunctivitis or dermatitis and again, no cases were found in the 0.01% atropine group.37–40
Pirenzepine
In an effort to reduce the side effects of atropine, in particular mydriasis and cycloplegia, pirenzepine 2% gel has been studied.41–43 Pirenzepine is a selective antimuscarinic with less mydriasis and cycloplegia.44 The U.S. Pirenzepine Study group found that patients randomized to twice daily pirenzepine slowed the rate of refractive myopia significantly but had no significant effect on axial length elongation. This effect was 51% at one year and then 41% after two years of therapy.41,42 The Asian Pirenzepine Study group found the same effect (44% at one year) but with significant reduction on the rate of axial length elongation.43 Significant side effects from the medication included abnormality in accommodation, mydriasis, ocular irritation, reaction, and discomfort, and even some subjective visual acuity decrease.41–43 Though pirenzepine shows potential clinical therapeutic use to reduce myopic progression, financial and regulatory obstacles has stopped its further development.1
Summary
Myopia is a common condition and if severe, has potentially severe ocular debilitating associations. There is much to be learned about its development and progression. Some risk factors have been identified and while gender, parental history, and ethnicity cannot be controlled, the environmental factor of outdoor activities has been shown to help reduce the odds. For those with myopia and in particular the young with actively progressing myopia, there are limited treatment options available.
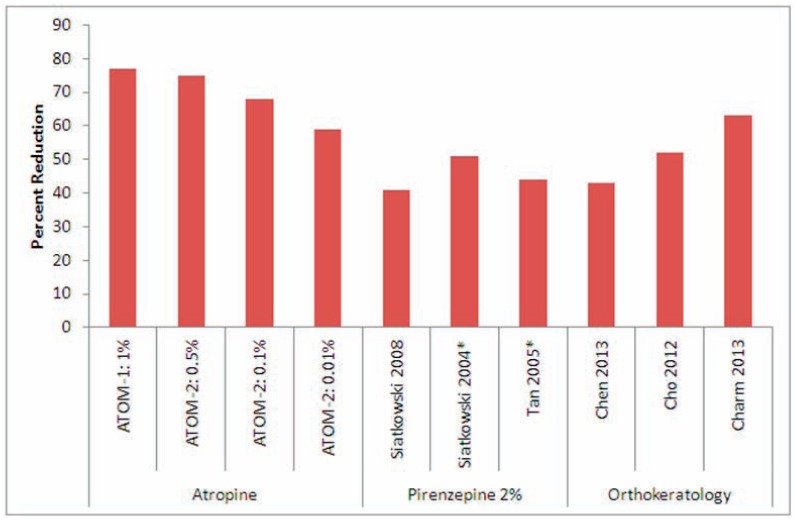
Discussed in this article were four of the most popular therapeutic regimens. Figure 3 shows the therapeutic myopic progression reduction found in the studies discussed in this article. It is to note that the figure is for the active therapy results and does not include any post-therapy results. Bifocals have not shown to be of any significant benefit. Orthokeratology has shown some benefit while wearing the lenses but is complicated by a number of sight threatening complications including infection. Pirenzepine has shown some benefit but due to expense and the evolving literature of atropine, will likely not be further pursued. Atropine has shown in the past as well as much more recently to be the current therapy of choice. The ATOM studies have shown great therapeutic success with minimal side effects.
Figure 3.
Effect of Treatment Modalities on Myopic Progression.
*Represents one-year results
Though further study and testing is necessary, the future of myopia progression therapy is looking brighter and the burden of myopia and its morbidities on the patient and on our society may lighten.
Biography
Matthew Recko, MD, (left ) is a fellow in Pediatric Ophthalmology, Children’s Mercy Hospitals and Clinics, Kansas City, Mo. Erin Durrie Stahl, MD, (right), MSMA member since 2014, is a Pediatric Ophthalmologist, Children’s Mercy Hospitals and Clinics, Kansas city, Mo.
Contact: edstahl@cmh.edu


Footnotes
Disclosure
None reported.
References
- 1.Leo SW, Young TL. An evidence-based update on myopia and interventions to retard its progression. J AAPOS. 2011 Apr;15(2):181–9. doi: 10.1016/j.jaapos.2010.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hung LF, Crawford ML, Smith EL. Spectacle lenses alter eye growth and the refractive status of young monkeys. Nat Med. 1995 Aug;1(8):761–5. doi: 10.1038/nm0895-761. [DOI] [PubMed] [Google Scholar]
- 3.Wallman J, Winawer J. Homeostasis of eye growth and the question of myopia. Neuron. 2004 Aug 19;43(4):447–68. doi: 10.1016/j.neuron.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 4.Group COMET. Myopia stabilization and associated factors among participants in the Correction of Myopia Evaluation Trial (COMET) Invest Ophthalmol Vis Sci. 2013 Dec 3;54(13):7871–84. doi: 10.1167/iovs.13-12403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thorn F, Gwiazda J, Held R. Myopia progression is specified by a double exponential growth function. Optom Vis Sci. 2005 Apr;82(4):286–97. doi: 10.1097/01.opx.0000159370.66540.34. [DOI] [PubMed] [Google Scholar]
- 6.Sherwin JC, Reacher MH, Keogh RH, Khawaja AP, Mackey DA, Foster PJ. The association between time spent outdoors and myopia in children and adolescents: a systematic review and meta-analysis. Ophthalmology. 2012 Oct;119(10):2141–51. doi: 10.1016/j.ophtha.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 7.Hyman L, Gwiazda J, Hussein M, Norton TT, Wang Y, Marsh-Tootle W, Everett D. Relationship of age, sex, and ethnicity with myopia progression and axial elongation in the correction of myopia evaluation trial. Arch Ophthalmol. 2005 Jul;123(7):977–87. doi: 10.1001/archopht.123.7.977. [DOI] [PubMed] [Google Scholar]
- 8.Saw SM, Goh PP, Cheng A, Shankar A, Tan DT, Ellwein LB. Ethnicity-specific prevalences of refractive errors vary in Asian children in neighbouring Malaysia and Singapore. Br J Ophthalmol. 2006 Oct;90(10):1230–5. doi: 10.1136/bjo.2006.093450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Congdon N, Wang Y, Song Y, Choi K, Zhang M, Zhou Z, Xie Z, Li L, Liu X, Sharma A, Wu B, Lam DS. Visual disability, visual function, and myopia among rural chinese secondary school children: the Xichang Pediatric Refractive Error Study (X-PRES)--report 1. Invest Ophthalmol Vis Sci. 2008 Jul;49(7):2888–94. doi: 10.1167/iovs.07-1160. [DOI] [PubMed] [Google Scholar]
- 10.Fan DS, Lam DS, Lam RF, Lau JT, Chong KS, Cheung EY, Lai RY, Chew SJ. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Invest Ophthalmol Vis Sci. 2004 Apr;45(4):1071–5. doi: 10.1167/iovs.03-1151. [DOI] [PubMed] [Google Scholar]
- 11.Saw SM, Tong L, Chua WH, Chia KS, Koh D, Tan DT, Katz J. Incidence and progression of myopia in Singaporean school children. Invest Ophthalmol Vis Sci. 2005 Jan;46(1):51–7. doi: 10.1167/iovs.04-0565. [DOI] [PubMed] [Google Scholar]
- 12.French AN, Morgan IG, Burlutsky G, Mitchell P, Rose KA. Prevalence and 5- to 6-year incidence and progression of myopia and hyperopia in Australian schoolchildren. Ophthalmology. 2013 Jul;120(7):1482–91. doi: 10.1016/j.ophtha.2012.12.018. [DOI] [PubMed] [Google Scholar]
- 13.Kempen JH, Mitchell P, Lee KE, Tielsch JM, Broman AT, Taylor HR, Ikram MK, Congdon NG, O’Colmain BJ Eye Diseases Prevalence Research Group. The prevalence of refractive errors among adults in the United States, Western Europe, and Australia. Arch Ophthalmol. 2004 Apr;122(4):495–505. doi: 10.1001/archopht.122.4.495. [DOI] [PubMed] [Google Scholar]
- 14.Vitale S, Ellwein L, Cotch MF, Ferris FL, 3rd, Sperduto R. Prevalence of refractive error in the United States, 1999–2004. Arch Ophthalmol. 2008 Aug;126(8):1111–9. doi: 10.1001/archopht.126.8.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vitale S, Sperduto RD, Ferris FL., 3rd Increased prevalence of myopia in the United States between 1971–1972 and 1999–2004. Arch Ophthalmol. 2009 Dec;127(12):1632–9. doi: 10.1001/archophthalmol.2009.303. [DOI] [PubMed] [Google Scholar]
- 16.Wen G, Tarczy-Hornoch K, McKean-Cowdin R, Cotter SA, Borchert M, Lin J, Kim J, Varma R Multi-Ethnic Pediatric Eye Disease Study Group. Prevalence of myopia, hyperopia, and astigmatism in non-Hispanic white and Asian children: multi-ethnic pediatric eye disease study. Ophthalmology. 2013 Oct;120(10):2109–16. doi: 10.1016/j.ophtha.2013.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jones-Jordan LA, Sinnott LT, Manny RE, Cotter SA, Kleinstein RN, Mutti DO, Twelker JD, Zadnik K Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) Study Group. Early childhood refractive error and parental history of myopia as predictors of myopia. Invest Ophthalmol Vis Sci. 2010 Jan;51(1):115–21. doi: 10.1167/iovs.08-3210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.French AN, Morgan IG, Mitchell P, Rose KA. Risk factors for incident myopia in Australian schoolchildren: the Sydney adolescent vascular and eye study. Ophthalmology. 2013 Oct;120(10):2100–8. doi: 10.1016/j.ophtha.2013.02.035. [DOI] [PubMed] [Google Scholar]
- 19.Gwiazda J, Hyman L, Hussein M, Everett D, Norton TT, Kurtz D, Leske MC, Manny R, Marsh-Tootle W, Scheiman M. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003 Apr;44(4):1492–500. doi: 10.1167/iovs.02-0816. [DOI] [PubMed] [Google Scholar]
- 20.Donovan L, Sankaridurg P, Ho A, Naduvilath T, Smith EL, 3rd, Holden BA. Myopia progression rates in urban children wearing single-vision spectacles. Optom Vis Sci. 2012 Jan;89(1):27–32. doi: 10.1097/OPX.0b013e3182357f79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pacella R, McLellan J, Grice K, Del Bono EA, Wiggs JL, Gwiazda JE. Role of genetic factors in the etiology of juvenile-onset myopia based on a longitudinal study of refractive error. Optom Vis Sci. 1999 Jun;76(6):381–6. doi: 10.1097/00006324-199906000-00017. [DOI] [PubMed] [Google Scholar]
- 22.Kurtz D, Hyman L, Gwiazda JE, Manny R, Dong LM, Wang Y, Scheiman M COMET Group. Role of parental myopia in the progression of myopia and its interaction with treatment in COMET children. Invest Ophthalmol Vis Sci. 2007 Feb;48(2):562–70. doi: 10.1167/iovs.06-0408. [DOI] [PubMed] [Google Scholar]
- 23.Saw SM, Nieto FJ, Katz J, Schein OD, Levy B, Chew SJ. Familial clustering and myopia progression in Singapore school children. Ophthalmic Epidemiol. 2001 Sep;8(4):227–36. doi: 10.1076/opep.8.4.227.1609. [DOI] [PubMed] [Google Scholar]
- 24.Mutti DO, Mitchell GL, Moeschberger ML, Jones LA, Zadnik K. Parental myopia, near work, school achievement, and children’s refractive error. Invest Ophthalmol Vis Sci. 2002 Dec;43(12):3633–40. [PubMed] [Google Scholar]
- 25.Ip JM, Saw SM, Rose KA, Morgan IG, Kifley A, Wang JJ, Mitchell P. Role of near work in myopia: findings in a sample of Australian school children. Invest Ophthalmol Vis Sci. 2008 Jul;49(7):2903–10. doi: 10.1167/iovs.07-0804. [DOI] [PubMed] [Google Scholar]
- 26.Saw SM, Chua WH, Hong CY, Wu HM, Chan WY, Chia KS, Stone RA, Tan D. Nearwork in early-onset myopia. Invest Ophthalmol Vis Sci. 2002 Feb;43(2):332–9. [PubMed] [Google Scholar]
- 27.Jones-Jordan LA, Mitchell GL, Cotter SA, Kleinstein RN, Manny RE, Mutti DO, Twelker JD, Sims JR, Zadnik K CLEERE Study Group. Visual activity before and after the onset of juvenile myopia. Invest Ophthalmol Vis Sci. 2011 Mar;52(3):1841–50. doi: 10.1167/iovs.09-4997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, Smith W, Mitchell P. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008 Aug;115(8):1279–85. doi: 10.1016/j.ophtha.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 29.Stambolian D. Genetic susceptibility and mechanisms for refractive error. Clin Genet. 2013 Aug;84(2):102–8. doi: 10.1111/cge.12180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cheng D, Woo GC, Drobe B, Schmid KL. Effect of bifocal and prismatic bifocal spectacles on myopia progression in children: three-year results of a randomized clinical trial. JAMA Ophthalmol. 2014 Mar;132(3):258–64. doi: 10.1001/jamaophthalmol.2013.7623. [DOI] [PubMed] [Google Scholar]
- 31.Swarbrick HA. Orthokeratology review and update. Clin Exp Optom. 2006 May;89(3):124–43. doi: 10.1111/j.1444-0938.2006.00044.x. [DOI] [PubMed] [Google Scholar]
- 32.Charm J, Cho P. High myopia-partial reduction ortho-k: a 2-year randomized study. Optom Vis Sci. 2013 Jun;90(6):530–9. doi: 10.1097/OPX.0b013e318293657d. [DOI] [PubMed] [Google Scholar]
- 33.Cho P, Cheung SW. Retardation of myopia in Orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012 Oct 11;53(11):7077–85. doi: 10.1167/iovs.12-10565. [DOI] [PubMed] [Google Scholar]
- 34.Chen C, Cheung SW, Cho P. Myopia control using toric orthokeratology (TO-SEE study) Invest Ophthalmol Vis Sci. 2013 Oct 3;54(10):6510–7. doi: 10.1167/iovs.13-12527. [DOI] [PubMed] [Google Scholar]
- 35.Van Meter WS, Musch DC, Jacobs DS, Kaufman SC, Reinhart WJ, Udell IJ American Academy of Ophthalmology. Safety of overnight orthokeratology for myopia: a report by the American Academy of Ophthalmology. Ophthalmology. 2008 Dec;115(12):2301–2313e1. doi: 10.1016/j.ophtha.2008.06.034. [DOI] [PubMed] [Google Scholar]
- 36.Saw SM, Gazzard G, Au Eong KG, Tan DT. Myopia: attempts to arrest progression. Br J Ophthalmol. 2002 Nov;86(11):1306–11. doi: 10.1136/bjo.86.11.1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chua WH, Balakrishnan V, Chan YH, Tong L, Ling Y, Quah BL, Tan D. Atropine for the treatment of childhood myopia. Ophthalmology. 2006 Dec;113(12):2285–91. doi: 10.1016/j.ophtha.2006.05.062. [DOI] [PubMed] [Google Scholar]
- 38.Tong L, Huang XL, Koh AL, Zhang X, Tan DT, Chua WH. Atropine for the treatment of childhood myopia: effect on myopia progression after cessation of atropine. Ophthalmology. 2009 Mar;116(3):572–9. doi: 10.1016/j.ophtha.2008.10.020. [DOI] [PubMed] [Google Scholar]
- 39.Chia A, Chua WH, Cheung YB, Wong WL, Lingham A, Fong A, Tan D. Atropine for the treatment of childhood myopia: safety and efficacy of 05%, 01%, and 001% doses (Atropine for the Treatment of Myopia 2) Ophthalmology. 2012 Feb;119(2):347–54. doi: 10.1016/j.ophtha.2011.07.031. [DOI] [PubMed] [Google Scholar]
- 40.Chia A, Chua WH, Wen L, Fong A, Goon YY, Tan D. Atropine for the treatment of childhood myopia: changes after stopping atropine 001%, 01% and 05% Am J Ophthalmol. 2014 Feb;157(2):451–457e1. doi: 10.1016/j.ajo.2013.09.020. [DOI] [PubMed] [Google Scholar]
- 41.Siatkowski RM, Cotter SA, Crockett RS, Miller JM, Novack GD, Zadnik K U.S. Pirenzepine Study Group. Two-year multicenter, randomized, double-masked, placebo-controlled, parallel safety and efficacy study of 2% pirenzepine ophthalmic gel in children with myopia. J AAPOS. 2008 Aug;12(4):332–9. doi: 10.1016/j.jaapos.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 42.Siatkowski RM, Cotter S, Miller JM, Scher CA, Crockett RS, Novack GD US Pirenzepine Study Group. Safety and efficacy of 2% pirenzepine ophthalmic gel in children with myopia: a 1-year, multicenter, double-masked, placebo-controlled parallel study. Arch Ophthalmol. 2004 Nov;122(11):1667–74. doi: 10.1001/archopht.122.11.1667. [DOI] [PubMed] [Google Scholar]
- 43.Tan DT, Lam DS, Chua WH, Shu-Ping DF, Crockett RS Asian Pirenzepine Study Group. One-year multicenter, double-masked, placebo-controlled, parallel safety and efficacy study of 2% pirenzepine ophthalmic gel in children with myopia. Ophthalmology. 2005 Jan;112(1):84–91. doi: 10.1016/j.ophtha.2004.06.038. [DOI] [PubMed] [Google Scholar]
- 44.Dörje F, Wess J, Lambrecht G, Tacke R, Mutschler E, Brann MR. Antagonist binding profiles of five cloned human muscarinic receptor subtypes. J Pharmacol Exp Ther. 1991 Feb;256(2):727–33. [PubMed] [Google Scholar]