Abstract
Urine drug screens are commonly used in various clinical settings and situations. Immunoassays are the most commonly available method of testing for urine drug screens in hospitals. Although convenient, immunoassays are prone to false positive and false negative results. It is important for the health care provider to understand the principles of the laboratory methods involved with urine drug screens as this will help guide appropriate result interpretation and therefore improve clinical care.
Introduction
Laboratory testing, including urine drug testing, is often utilized in the evaluation and management of intoxicated patients as well as those with non-specific presentations such as altered mental status. Urine drug testing is also used in other circumstances, such as legal and forensic cases including those involving minors or sexual assault victims. Urine drug screens are also used commonly for pre-employment testing or in situations involving workplace-associated injuries. Physicians may also use urine drug screens to document compliance (or lack thereof) to prescribed opioid therapy.1
Historically, immunoassays were developed for employment screening.2 Urine drug testing is now common in certain occupations such as those that involve federally regulated transportation (i.e., truck drivers and train engineers) or those employed in safety-sensitive occupations (i.e., operating large industrial equipment).3 Interpretation of drug test results in this setting is often performed by a medical review officer, who is trained and certified in result interpretation. Given the ramifications involved it is important for health care providers to understand the pitfalls in interpreting urine drug screen results.
Knowledge of laboratory methods involved with urine drug testing help to facilitate test result interpretation. Multiple methods exist to assess for the presence of drugs in the urine, however only a few methods are commonly used in hospital laboratories. Immunoassays are the most common utilized by hospital laboratories as they are easily automated for laboratory personnel. They have several advantages in that they are relatively inexpensive, are not labor intensive, and have short turn-around time to obtain results.4 Immunoassays rely on a chemical reaction between an antibody and drug of interest. For each drug class on the immunoassay there is an antibody to a representative drug in that class (i.e. the opiate class often uses an antibody to morphine). A critical concept is that not all drugs within a class have similar chemical structures and therefore may or may not react with the antibody included in the assay.4 Depending on the manufacturer there may be variable cross reactivity to various substances (discussed in further detail below). The manufacturer often does preliminary testing and reports some agents in their package insert known to cross-react with each class. This list should not be considered exhaustive as many unlisted substances cross react. The sensitivity and specificity of the various components of the immunoassays also can vary between manufactures as well. Thus, health care providers should be aware of the specifications of the immunoassay that is used by their laboratory.
Several other advanced laboratory drug screening techniques are available to the clinician but are less commonly employed by hospital laboratories. Thin layer chromatography (TLC) and gas chromatography/mass spectrometry (GC/MS) are two other methods used for urine drug testing.5 The advantage of both is that they can screen for a higher number of substances. TLC tends to be less sensitive than immunoassay but is more specific.5 GC/MS is both more sensitive and specific than immunoassay.5, 6 Both are generally more expensive, slower, and not readily available for acute management. Given the poor sensitivity and specificity of immunoassays the clinician should consider obtaining more definitive confirmation (such as GC/MS), especially in cases with forensic or legal ramifications. There are multiple reputable reference laboratories that perform such testing and the clinician should discuss with their own laboratory personal regarding send-out laboratory procedures.
There are several other limitations that clinicians should be aware of when interpreting urine drug screens. Each analyte of the UDS has a cutoff or detection level of specified urine metabolite above which the test will be positive. Although these values are applied to clinical testing these cutoff limits were originally developed for workplace testing to decrease false positives (i.e. increase specificity) given the large volume of employment testing performed.3 How these cutoff values apply to clinical medicine and determination of intoxication is largely unknown.7 It is possible (depending on dose, pharmacokinetic elimination patterns, and timing of last exposure) for a patient to have be exposed to a substance and have a negative urine drug test. Conversely, it is also important to be aware that some components of immunoassays lack specificity and are prone to false positive results (discussed below).1, 4, 5 Other limitations involve understanding that detection times in the urine vary significantly based on multiple factors including: dose, elimination half-life, urine pH, urine dilution, frequency of use, and time of last use.8 Table 1 lists general detection times for urine drug metabolites.
Table 1.
Length of Time that Urine Drug Screens Can Detect Drugs since Last Use*
| Substance | Length of Detection |
|---|---|
| Amphetamines | 3 days |
|
| |
| Barbiturates | |
| Short/Intermediate acting (butalbital) | 24–72 hours |
| Long acting (phenobarbital) | 2–3 weeks |
|
| |
| Benzodiazepines | |
| Short acting | 3 days |
| Long acting | 3 weeks |
|
| |
| Cannabinoids | |
| Single use | 3 days |
| Heavy user | 4–6 weeks |
|
| |
| Cocaine | 3–5 days |
|
| |
| Opioids | 3–5 days |
|
| |
| Phencyclidine | 8 days |
Amphetamines
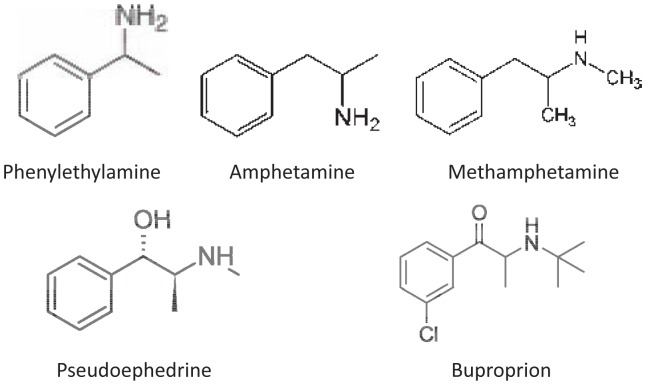
Amphetamines are prescribed most commonly for attention deficit hyperactivity disorder, but are also widely misused and abused. Many illicit and designer/synthetic amphetamines exist such as metamphetamine and methylenedioxymethamphetamine (MDMA, ecstasy). Immunoassays are a good screening testing for basic amphetamine compounds such as amphetamine salts (ADHD medications) and methamphetamine. There are some immunoassays that screen specifically for methamphetamine. Most general amphetamine immunoassays will often be positive as methamphetamine is metabolized to amphetamine. Although the sensitivity is high for amphetamine salts there is poor specificity due to a large number of substances that cross react and result in false positive results. Any pharmaceutical that has a phenylethylamine structure (See Figure 1) within the compound can result in a false positive. Numerous substances have been shown to result in false positives (See Table 2). Each immunoassay has slightly different sensitivity and specificity to these agents but due to widespread use of many of these agents false positives are common. The sensitivity for other designer or synthetic amphetamine compounds is variable. Substances such as MDMA and “bath salts” have variable cross-reactivity but are often not detected.9
Figure 1.
Structure of Phenylethylamine
Table 2.
Agents Known to Produce False Positive and False Negative Urine Immunoassays*
| False Positive | False Negative | |
|---|---|---|
| Amphetamines | Amantadine Buproprion Ephedrine Labetolol Methylphenidate Phentermine Pseudoephedrine Ranitidine Seligiline Trazadone |
MDMA (ecstasy) Synthetic amphetamines (cathinones, bath salts, etc) |
| Benzodiazepines | Oxaprozin Sertraline Efavirenz |
Alprazolam Clonazepam Lorazepam |
| Cannabinoids | Ibuprofen Naproxen Efavirenz Baby washes |
Synthetic cannabinoids |
| Opioids | Poppy seeds Quinolones Verapamil |
Fentanyl Hydrocodone Hydromorphone Meperidine Methadone Oxycodone |
| Phencyclidine | Dextromethorphan Diphenhydramine Ketamine Tramadol Venlafaxine |
|
| Tricyclic Antidepressants | Carbamazepine Cyclobenzaprine Diphenhydramine Phenothiazines |
Barbiturates
The barbiturate class is still included on many assays, however, it has less clinical relevance since these are prescribed and/or abused infrequently. There are two main barbiturates that are still prescribed occasionally in the United States. Phenobarbital, once a mainstay in seizure management, has become less attractive for seizure management and has been replaced by anticonvulsants with better side effect profiles. Butalbital is another barbiturate that is formulated as a combination product with acetaminophen and caffeine and is still prescribed for the treatment of migraine headaches. Other barbiturates are used as intravenous sedation or rarely prescribed. The barbiturate immunoassay looks for the structure of secobarbital as a representative for the entire barbiturate class.10 The most commonly used agents such as phenobarbital and butabital are reliably identified with good sensitivity as is primidone, which is metabolized to phenobarbital.10 There have been occasional reports of substances resulting in false positives; both ibuprofen and naproxen have been noted to result in false positive test results.10 But, in general the barbiturate immunoassay has good sensitivity and specificity.
Benzodiazepines
Benzodiazepines are widely prescribed for various medical conditions and are also commonly abused. Similar to the other drug classes on immunoassays the benzodiazepine class is subject to poor sensitivity and specificity. Oxazepam, a metabolite of diazepam and chlordiazepoxide, is the chemical that most immunoassays are designed to detect.4 There are some commonly used benzodiazepines (i.e., alprazolam, clonazepam) that can result in negative testing results although cross-reactivity is not uncommon. There are also several reports of NSAIDS and an HIV medication (efavirenz) producing false positive results (See Table 2). Flunitrazepam is a benzodiazepine that, while not legal in the United States, can be purchased legally in Mexico and Europe. It is a very potent benzodiazepine that has been used in drug-facilitated sexual assaults since it produces profound impairment and amnesia and is not detected on routine immunoassay drug testing.11
Cannabinoids
Cannabis is the most widely used illicit drug. As more states decriminalize the use and possession of cannabis, its use will likely become even more widespread. The major psychoactive chemical in cannabis is delta-9-tetrahydrocannabinol (THC). Urine drug screens are designed to detect 11-nor-delta-9-tetrahydrocannabinol-9-carboxylic acid (9-carboxy-THC). Due to the high lipid solubility and slow excretion of 9-carboxy-THC into the urine, one time use of cannabis can cause a positive urine drug screen for three days up to one week. Heavy, daily cannabis users can have a positive urine drug screen for 4–6 weeks after cessation. Although considered one of the more specific items on the urine drug screen, false positives for cannabis have been reported with dronabinol, efavirenz, NSAIDs, promethazine, riboflavin, ethacrynic acid, and baby soaps.4,12,13,14 Of note, newer synthetic cannabinoids (i.e., JWH-018, “spice”, “K2”, etc.) are not detected by the standard urine drug screen.
Cocaine
Cocaine has been used for its stimulant properties for centuries. It is derived from the Coca plant and then processed into different forms such as crack (which can be smoked) or powder cocaine. Cocaine is metabolized to three metabolites: norcocaine, ecgonine methyl ester, and benzoylecgonine (BE). Commonly performed immunoassays generally detect BE.15 Unlike most drug classes that are tested for on immunoassays the cocaine assay is relatively sensitive and specific for cocaine. False negative testing could occur if the urine is collected shortly after use and an insufficient amount of BE has been excreted in the urine. Otherwise, it is a sensitive test to determine recent exposure to cocaine. False positives have not been reported; although it is possible that a positive test could result from drinking Coca tea which is commonly available in South American but is illegal in the United States since does contain small amounts of cocaine.4
Opioids
Although often used interchangeably, opiates and opioids refer to different classes of xenobiotics. Opiates are derivatives of the opium poppy (morphine and codeine). Opioids refers to a very broad class of drugs with opium-like effects (hydrocodone, oxycodone, propoxyphene, hydromorphone, fentanyl, methadone, propoxyphene, etc.). Most urine drug screens are designed to detect opiates (namely morphine) and drugs metabolized to morphine by the human body (i.e., heroin) and often “miss” the majority of semi-synthetic and synthetic opioids; although, cross-reactivity does occur and is assay dependent. False-positive opiate tests have reportedly been caused by dextromethorphan, diphenhydramine, quinine, quinolones, rifampin, verapamil, and poppy seeds.4 In the hopes of testing for medical adherence, some urine drug screens specifically include methadone. Of note, false positive methadone screens have been reported to be caused by quetiapine, doxylamine, olanzapine, diphenhydramine, and verapamil.16
Phencyclidine (PCP)
Phencyclidine is a dissociative agent structurally related to ketamine. Although not fully pharmacologically understood, PCP is a N-methyl-D-aspartic acid (NMDA) receptor antagonist. It has a wide range of effects depending on the dose and the patient. Effects include dissociation, euphoria, decreased inhibition, hypertension, tachycardia, and nystagmus. Patients can be comatose or extremely combative. Clinically, a false positive urine drug screen can be due to numerous xenobiotics: dextromethorphan, diphenhydramine, doxylamine, ibuprofen, imipramine, ketamine, meperidine, venlafaxine, buproprion, methylenedioxpyrolvalerone (MDPV), and tramadol.4, 17, 18, 19
Tricyclic Antidepressants (TCAs)
Although not a “drug of abuse”, many urine drug screens also test for tricyclic antidepressants due to the high number of mortalities seen with TCA overdoses in the 1980s and 1990s. Other ringed xenobiotics like carbamazepine, cyproheptadine, cyclobenzaprine, and quetiapine have been reported to cause false positives. Likewise, structurally similar agents like diphendyramine, hydroxyzine, cetirizine can also cause false positive TCA screens.4, 20, 21, 22
Utility in Clinical Management
At some point in medical training, all physicians-in-training have been asked the loaded question, “What are you going to do with the results of that test?” The urine drug screen is no different. Oftentimes, the physician orders a urine drug screen “to see if the patient is on something.” Hopefully, the aforementioned discussion of false positives, false negatives, laboratory cutoffs, etc. for the various drugs of abuse has provided evidence that this logic is fraught with error.
A positive or negative urine drug screen is just a yes or no answer. That is to say, the results of a urine drug screen are not quantitative. Consider other quantitative toxicologic testing (i.e., serum salicylate concentration, serum acetaminophen concentration, and blood alcohol concentration). These quantitative assays have the ability to change clinical management based on their numerical result. A urine drug screen positive for cocaine, on the other hand, does not mean that the patient’s presenting signs or symptoms can be explained by the clinical result. Consider a patient with a low-grade fever, tachycardia, and altered mental status. A “frequent flyer” with a urine drug screen positive for cocaine may result in early closure of the diagnostic work-up in a patient whose symptoms are due to meningitis, pneumonia, urinary tract infection, or countless other possibilities.
A negative urine drug screen does not “rule out” that a patient’s presenting signs and symptoms are due to a drug of abuse. As mentioned previously, the immunoassay for benzodiazepines is designed to detect oxazepam. Some of the more commonly abuse benzodiazepines like alprazolam (Xanax) and clonazepam (Klonopin) are not metabolized to oxazepam and would then be “missed” by most urine drug screens.
Multiple studies in the adult and pediatric populations confirm that the results of a urine drug screen very rarely change clinical management.6,23,24,25,26,27 The cost of the urine drug screen varies widely between institutions. The cost of misdiagnosis due to the misinterpretation of the urine drug screen is likely very similar between institutions.
There are certainly clinical scenarios when a urine drug screen should be ordered. Most commonly, a urine drug screen is required by receiving mental health institutions. While there is some evidence that the results of a urine drug screen rarely change the management of psychiatric conditions28, in clinical practice most emergency physicians still have to send urine drug screens, as well as other labs “screening” for medical conditions, as a requirement by mental health institutions. Urine drug screens can also have important implications in child abuse and neglect cases.29 Positive screens should be confirmed by GC/MS and/or quantitative levels of the specific drug of abuse in question should be sent in these types of cases. Lastly, urine drug screens can also provide some useful information in certain clinical situations. The urine drug screen has to be interpreted in the light of its many short-comings.
Conclusion
Urine drug screens are commonly ordered by emergency physicians. The results of a UDS rarely change clinical management. Among the agents that are tested for by a UDS, the sensitivity and specificity vary greatly as does the length of time that a test is positive for since the last use. Given the aforementioned short-comings of the UDS, the results of this test (positive or negative) should be interpreted with caution.
Biography
D. Adam Algren, MD, (left) and Michael R. Christian, MD, (right) MSMA member since 2012, are Assistant Professors of Emergency Medicine and Pediatrics at the University of Missouri- Kansas City School of Medicine, and Department of Emergency Medicine at Truman Medical Center, and in the Department of Clinical Pharmacology and Medical Toxicology at Children’s Mercy Hospital and Clinics.
Contact: adam.algren@tmcmed.org

Footnotes
Disclsoure
None reported.
References
- 1.Standridge JB, Adams SM, Zotos AP. Urine drug screening: A valuable office procedure. Am Fam Physician. 2010;81:635–640. [PubMed] [Google Scholar]
- 2.Hammett-Stabler CA, Pesce AJ, Cannon DJ. Urine drug screening in the medical setting. Clin Chim Acta. 2002;315:125–135. doi: 10.1016/s0009-8981(01)00714-8. [DOI] [PubMed] [Google Scholar]
- 3.United States Department of Transportation. Office of Drug & Alcohol Policy and Compliance. [Last accessed 11/25/14]. Located at www.dot.gov/odapc.
- 4.Moeller KE, Lee KC, Kissack JC. Urine drug screening: A practical guide for clinicians. Mayo Clin Proc. 2008;83:66–76. doi: 10.4065/83.1.66. [DOI] [PubMed] [Google Scholar]
- 5.Eskridge KD, Guthrie SK. Clinical issues associated with urine testing of substances of abuse. Pharmacotherapy. 1997;17:497–510. [PubMed] [Google Scholar]
- 6.von Mach MA, Weber C, Meyer MR, et al. comparison of urinary on-site immunoassay screening and gas chromatography-mass spectrometry results of 111 patients with suspected poisoning presenting to an emergency department. Ther Drug Monit. 2007;29:27–39. doi: 10.1097/FTD.0b013e31802bb2aa. [DOI] [PubMed] [Google Scholar]
- 7.Council on Scientific Affairs. Scientific Issues in Drug Testing. JAMA. 1987;257:3110–3114. [PubMed] [Google Scholar]
- 8.Heit HA, Gourlay DL. Urine drug testing in pain medicine. J Pain Symptom Manage. 2004;27:260–267. doi: 10.1016/j.jpainsymman.2003.07.008. [DOI] [PubMed] [Google Scholar]
- 9.Petrie M, Lynch KL, Ekins S, et al. Cross-reactivity studies and predictive modeling of “bath salts” and other amphetamine-type stimulants with amphetamine screening immunoassays. Clin Toxicol. 2013;51:83–91. doi: 10.3109/15563650.2013.768344. [DOI] [PubMed] [Google Scholar]
- 10.Fitzgerald RL, Rexin DA, Herold DA. Detecting benzodiazepines: immunoassays compared with negative chemical ionization gas chromatography/mass spectrometry. Clin Chem. 1994;40:373–380. [PubMed] [Google Scholar]
- 11.Verstraete AG. Detection times of drugs of abuse in blood, urine, and oral fluid. Ther Drug Monit. 2004;26:200–205. doi: 10.1097/00007691-200404000-00020. [DOI] [PubMed] [Google Scholar]
- 12.Cotton SW, Duncan DL, Burch EA, et al. Unexpected interference of baby wash products with a cannabinoid (THC) immunoassay. Clin Biochem. 2012;45:605–609. doi: 10.1016/j.clinbiochem.2012.02.029. [DOI] [PubMed] [Google Scholar]
- 13.la Porte CJ, Droste JA, Burger DM. False-positive results in urine drug screening in healthy volunteers participating in phase 1 studies with efavirenz and rifampin. Ther Drug Monit. 2006;28:286. doi: 10.1097/01.ftd.0000199359.87636.5d. [DOI] [PubMed] [Google Scholar]
- 14.Musshoff F, Burkhard M. Review of biologic matrices (urine, blood, hair) as indicators of recent or ongoing cannabis use. Ther Drug Monit. 2006;28:155–163. doi: 10.1097/01.ftd.0000197091.07807.22. [DOI] [PubMed] [Google Scholar]
- 15.Maurer HH, Sauer C, Theobald DS. Toxicokinetics of drugs of abuse: Current knowledge of the isoenzymes involved in the human metabolism of tetrahydrocannabinol, cocaine, heroin, morphine, and codeine. Ther Drug Monit. 2006;28:447–453. doi: 10.1097/01.ftd.0000211812.27558.6e. [DOI] [PubMed] [Google Scholar]
- 16.Rogers SC, Pruitt CW, Crouch DJ, Caravati EM. Rapid urine drug screens: diphenhydramine and methadone cross-reactivity. Pediatr Emerg Care. 2010;26:665–666. doi: 10.1097/PEC.0b013e3181f05443. [DOI] [PubMed] [Google Scholar]
- 17.King AM, Pugh JL, Menke NB, et al. Nonfatal tramadol overdose may cause false-positive phencyclidine on emit-II assay. Am J Emerg Med. 2013;31:444.e5–444.e9. doi: 10.1016/j.ajem.2012.05.028. [DOI] [PubMed] [Google Scholar]
- 18.Ly BT, Thornton SL, Buono C, et al. False-positive urine phencyclidine immunoassay screen result caused by interference by tramadol and its metabolites. Ann Emerg Med. 2012;59:545–547. doi: 10.1016/j.annemergmed.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 19.Macher AM, Penders TM. False-positive phencyclidine immunoassay results caused by 3, 4methylenedioxypyrovalerone (MDPV) Drug Test Anal [serial online] 2012 Apr 17; doi: 10.1002/dta.1371. [DOI] [PubMed] [Google Scholar]
- 20.Matos ME, Burns MM, Shannon MW. False-positive tricyclic antidepressant drug screen results leading to the diagnosis of carbamazepine intoxication. Pediatrics. 2000;105:e66. doi: 10.1542/peds.105.5.e66. [DOI] [PubMed] [Google Scholar]
- 21.Dasgupta A, Wells A, Datta P. False-positive serum tricyclic antidepressant concentrations using fluorescence polarization immunoassay due to the presence of hydroxyzine and cetirizine. Ther Drug Monit. 2007;29:134–139. [PubMed] [Google Scholar]
- 22.Yuan CM, Spandorfer PR, Miller SL, et al. Evaluation of tricyclic antidepressant false positivity in a pediatric case of cyproheptadine (periactin) overdose. Ther Drug Monit. 2003;25:299–304. doi: 10.1097/00007691-200306000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Tenenbein M. Do you really need that emergency drug screen? Clin Toxicol. 2009;47:286–291. doi: 10.1080/15563650902907798. [DOI] [PubMed] [Google Scholar]
- 24.Montague RE, Grace RF, Lewis JH, Shenfield GM. Urine drug screens in overdose patients do not contribute to immediate clinical management. Ther Drug Monit. 2001;23:47–50. doi: 10.1097/00007691-200102000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Belson MG, Simon HK. Utility of comprehensive toxicologic screens in children. Am J Emerg Med. 1999;17:221–224. doi: 10.1016/s0735-6757(99)90109-2. [DOI] [PubMed] [Google Scholar]
- 26.Belson MG, Simon HK, Sullivan K, Geller RJ. The utility of toxicologic analysis in children with suspected ingestions. Pediatr Emerg Care. 1999;15:383–387. doi: 10.1097/00006565-199912000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Sugarman JM, Rodgers GC, Paul RI. Utility of toxicology screening in a pediatric emergency department. Pediatr Emerg Care. 1997;13:194–197. doi: 10.1097/00006565-199706000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Schiller MJ, Shumway M, Batki SL. Utility of routine drug screening in a psychiatric emergency setting. Psychiatr Serv. 2000;51:474–478. doi: 10.1176/appi.ps.51.4.474. [DOI] [PubMed] [Google Scholar]
- 29.Hoffman RJ, Nelson L. Rational use of toxicology testing in children. Curr Opin Pedatr. 2001;13:183–188. doi: 10.1097/00008480-200104000-00017. [DOI] [PubMed] [Google Scholar]