Abstract
Background:
Whether types of hospitals with high readmission rates also have high overall post-discharge acute care utilization (including emergency department and observation care) is unknown.
Design:
Cross-sectional analysis
Setting:
Subjects:
Non-federal United States acute care hospitals
Measures:
Using methodology established by the Centers for Medicare & Medicaid Services, we calculated each hospital’s “excess days in acute care” (EDAC) for fee-for-service Medicare beneficiaries aged over 65 years discharged after hospitalization for acute myocardial infarction (AMI), heart failure or pneumonia, representing the mean difference between predicted and expected total days of acute care utilization in the 30 days following hospital discharge, per 100 discharges. We assessed the multivariable association of 8 hospital characteristics with EDAC and the proportion of hospitals with each characteristic that were statistical outliers (95% credible interval estimate excludes zero).
Results:
We included 2,184 hospitals for AMI (228 [10.4%] better than expected, 549 [25.1%] worse than expected), 3,720 hospitals for heart failure (484 [13.0%] better and 840 [22.6%] worse), and 4,195 hospitals for pneumonia (673 [16.0%] better, 1,005 [24.0%] worse). Results for all conditions were similar. Worse than expected outliers for pneumonia included: 18.8% of safety net hospitals vs. 26.1% of non-safety net hospitals; 16.7% of public hospitals vs. 33.1% of for-profit hospitals; 19.5% of non-teaching hospitals vs. 52.2% of major teaching hospitals; 7.9% of rural hospitals vs. 42.1% of large urban hospitals; 5.9% of hospitals with 24 to <50 beds vs. 58% of hospitals with >500 beds; and 29.0% of hospitals with nurse-to-bed ratios >1.0 to 1.5 vs. 21.7% of hospitals with ratios >2.0.
Conclusions:
Including ED and observation stays in measures of post-discharge utilization produces similar results as measuring only readmissions in that major teaching, urban and for-profit hospitals still perform disproportionately poorly versus non-teaching or public hospitals. However, it enables identification of more outliers and a more granular assessment of the association of hospital factors and outcomes. .
Keywords: hospital quality, readmissions, emergency department, health service research
Introduction
Readmission rates have fallen nationally in recent years.1 Hospital readmission, however, is only one type of acute, unscheduled care post-discharge. Patients may return to the emergency department, or may be observed for a period without requiring an inpatient stay.2 Both emergency and observation care are costly to patients in terms of time, lost opportunity for work, copayments, and caregiver burden, yet are not captured by readmission measures. Observation care may be replacing some readmissions, making it harder to fully characterize post-discharge outcomes from the patient perspective.3,4 In addition, current measures report readmissions only as a binary outcome (i.e., any versus no readmission), ignoring multiple return visits and the length of the rehospitalizations.
To more fully capture patients’ post-hospitalization experience, the Centers for Medicare & Medicaid Services (CMS) reported new measures of post-discharge acute care use following hospitalization for acute myocardial infarction (AMI) and heart failure in 2017, and will report for pneumonia in 2018.5–7 These measures, referred to as “excess days in acute care” (EDAC) measures, were designed to capture all days in acute care that a patient experiences in the 30 days post-discharge, including emergency department (ED) visits, observation stays, and unplanned inpatient readmissions.
It has not yet been established which types of hospitals best support patient goals to minimize time spent in acute care post-discharge. Variation in performance according to hospital characteristics has been separately described for readmission outcomes, observation care and ED visits.4,8–12 For example, large hospitals, teaching hospitals and urban hospitals tend to have slightly higher readmission rates.13–16 Whether the types of hospitals with low readmission rates also have low overall post-discharge utilization, however, is uncertain. The structures, organization and resources that are associated with reduced readmission risk may not function similarly for other types of acute care utilization. ED treat-and-release visits, for example, may have different etiologies than readmissions. By identifying types of hospitals that are able to avoid all three types of post-discharge utilization – that is, to generate fewer days in acute care of any kind – we may be able to identify means of more broadly improving healthcare delivery. For example, some types of hospitals might be better able to connect patients to community resources, such as free medications or clinics with evening hours, that would help patients avoid coming to the ED at all, not only avoid readmission. Accordingly, we used the EDAC measures to characterize hospitals’ performance and to identify hospital characteristics associated with post-discharge utilization.
Methods
Subjects
All United States non-federal hospitals were eligible for the study, with the following exclusions: hospitals with fewer than 25 eligible inpatient discharges (N=2,008 for AMI, 831 for heart failure, 383 for pneumonia), hospitals that could not be matched to the 2013 American Hospital Association (AHA) annual survey file (N=21 for AMI, 62 for heart failure and 84 for pneumonia)and hospitals which could not be matched to 2013 National Center for Health Statistics (NCHS) Urban-Rural classifications (N=14 for AMI, 26 for heart failure and 30 for pneumonia; largely, hospitals in US territories).
Study data
To calculate the outcome measures, we used the Medicare data derived for the 2016 public reporting measures of AMI, HF and pneumonia readmission for discharges between July 2012 to June 2015, which includes the inpatient discharge, 12-month comorbidity history, and post-discharge outcomes retrieved from the Medicare hospital inpatient claims and outpatient claims data, physician carrier claims (Part B claims) and the Medicare enrollment data. To obtain our independent variables, we used the 2013 AHA annual survey data and the 2013 NCHS Urban-Rural classifications file.
Outcome
Our primary outcome is a hospital level metric, EDAC, that is based on the number of days that patients discharged alive from that hospital spend in acute care during the 30 days post discharge. To construct the EDAC measures, we first identified all discharges between July 1, 2012-June 30, 2015 from United States non-federal short-term acute care or critical access hospitals for patients over 65 years with Medicare fee-for-service insurance who qualified for the 2016 specifications of the publicly-reported AMI, heart failure and pneumonia readmission measures respectively. Those measures and the related updates have previously been described in detail.17–20 Briefly, we included inpatient discharges for patients who had the relevant qualifying condition (AMI, heart failure or pneumonia), were discharged alive, had one year of prior enrollment in Medicare FFS, and were not transferred to another acute care hospital. We excluded discharges of patients without one month of post-discharge enrollment data and those discharged against medical advice. Patients could have more than one eligible discharge during the study period but qualifying admissions that were themselves readmissions were excluded. (Appendix 1)
We defined days in acute care as days spent in an ED, admitted to observation status, or admitted as an unplanned readmission for any cause within 30 days from the date of discharge from the index hospitalization. See Appendix 2 for definitions of ED and observation visits. Each ED visit was counted as one half day based on average duration of ED visits. Observation stays are billed in terms of hours; we rounded hours up to the nearest half-day. We defined a readmission as any unplanned acute care hospital inpatient hospitalization within 30 days of the discharge date for the index hospitalization. “Planned” readmissions are those planned by providers for anticipated medical treatment or procedures that must be provided in the inpatient setting. To exclude planned readmissions, we used the planned readmission algorithm version 2.1 developed for each publicly reported readmission measure.21 We considered all observation stays and ED visits to be unplanned. Each readmission was counted in days according to the length of stay. Admissions that extended beyond the 30-day follow-up period were truncated on day 30.
When an ED visit, observation stay, or readmission overlapped with another event on the same day, we counted only one event. If the readmission and either an observation stay or ED visit happened on the same day, we recorded one readmission day; if an observation stay and an ED visit happened on the same day, we recorded one observation stay.
We use multivariable modeling to convert each patient’s observed days in acute care to hospital-level EDAC. The hospital-level EDAC is defined as the difference between predicted days and expected days in acute care within thirty days following discharge among all index discharges in the specific hospital.5–7 The predicted days and expected days in acute care for each index admission are calculated using a two-part logit/truncated Poisson hierarchical model that includes the final risk adjustment variables in the specification of the 2016 publicly-reported readmission measures: age, sex and comorbidities (Appendix 3).20 Comorbidities present only during the index admission are included if they are not likely to be in-hospital complications of care. We added two random effects to the model for predicted days – one hospital effect for the logit part and one hospital effect for the truncated Poisson part – with a non-zero covariance between the two random effects. These random effects allowed us to account for within-hospital correlation of the observed outcome and accommodated the assumption that underlying differences in quality across hospitals leads to systematic differences in outcomes. We calculated the expected days using the same model but assuming the hospital random effect was zero. The models include an offset for days alive, such that only days in which a patient was alive to experience an event are included. In this, the measures differ from the CMS readmission measures, for which all patient admissions are considered equally at risk for readmission regardless of vital status post-discharge.
In both cases, we estimated the models using fully Bayesian Markov Chain Monte Carlo (MCMC) estimation, retaining 3,000 simulated predicted and expected values for each hospital. We then calculated 3,000 EDACs for each hospital as the mean of each admission’s difference in predicted and expected days. Of these 3,000 EDACs, we reported the median EDAC for each hospital as the hospital level EDAC, and defined the 95% credible interval (CI) as the EDAC values at 2.5th and 97.5th percentile. To be consistent with the reporting of the CMS 30-day readmission measures, we multiplied the final measure by 100 so that EDAC represents excess days per 100 discharges.
A mean EDAC of zero (predicted-expected difference = 0) indicates no difference between the performance of the hospital and the result those same patients would experience at an average performing hospital. A negative difference indicates that patients discharged from that hospital are predicted to experience fewer days in acute care than expected if discharged from an “average” hospital; in other words, that the hospital has better than average performance. A positive difference indicates that the hospital has worse than expected performance.
Outlier status
To characterize hospital outlier status, we compared each hospital’s EDAC credible interval estimate to zero, which represents no difference from expected. We classified a hospital to be no different than expected if the 95% CI included zero, higher than expected if the full 95% CI was above zero, and lower than expected if the full 95% CI was below zero.
Independent variables
For this first, exploratory analysis of the new EDAC measure, we elected primarily to examine hospital characteristics, not community effects, and to include only those for which contemporaneous, reliable data was available for the great majority of hospitals and that had previously been shown to be associated with readmission rates. We assessed eight hospital characteristics, identified from the 2013 AHA annual survey data and 2013 NCHS urban-rural classifications data: safety net status (a public hospital, or a private hospital with a Medicaid caseload more than one standard deviation above the state average22),13,15,23 hospital ownership (not-for-profit, for-profit or public),14,15 teaching status (major teaching [member of Council of Teaching Hospitals], minor teaching hospital, non-teaching),13,15 availability of cardiac procedures (capable of cardiac bypass surgery, capable only of cardiac catheterization, not capable of either) as a proxy for overall advanced surgical or procedural capacity, metropolitan status (defined according to the National Center for Health Statistics classification24),15 geographic region (US Census Bureau division),15,25 bed size (divided by AHA into 8 categories with smallest 6–24 beds and largest 500 or more),13,15,16 and nurse/bed ratio (full-time equivalent RN/total beds set up and staffed).8,14,15,26
Statistical analysis
We examined the distribution of the hospital-level EDAC and plotted the corresponding histograms for each condition. We used descriptive statistics to describe mean EDAC according to hospital characteristics for each condition. We also described the proportion of high and low outlier hospitals for each characteristic and for readmission measure outlier status. We then constructed a linear regression model for each condition including all hospital characteristics simultaneously to determine the adjusted association of each with EDAC for each condition. To account for the lower precision of the outcome in hospitals with fewer discharges, we weighted by the inverse of the variance, which was estimated using width of the credible interval. All tests were two-tailed and we considered a p-value <0.05 to be statistically significant. The study was approved by the Yale Institutional Review Board including a waiver of informed consent.
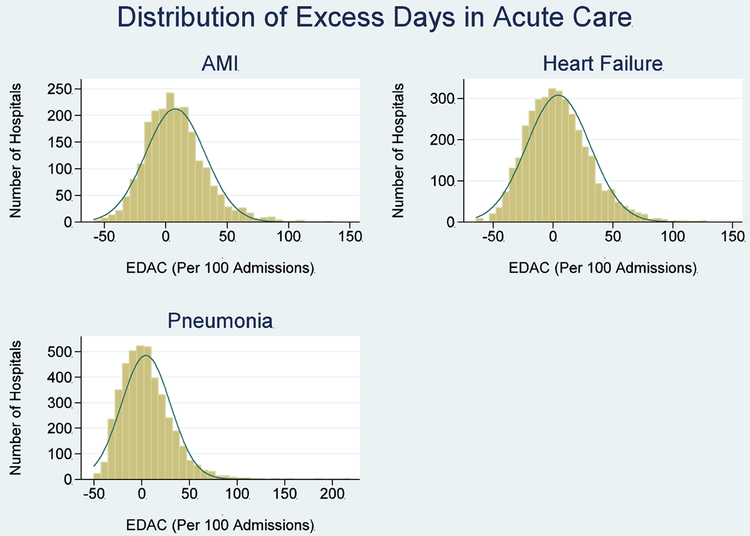
Results
We included 2,184 hospitals for AMI, 3,720 hospitals for heart failure, and 4,195 hospitals for pneumonia; these represent over 97% of hospitals with at least 25 cases in the study period. The median EDAC per 100 discharges was −0.4 for AMI (interquartile range −12.8, 13.5), 0.1 for heart failure (interquartile range, −15.8, 16.4) and −1.2 for pneumonia (interquartile range −16.1, 14.3). See Figure 1 for histograms.
Figure 1:
Distribution of excess days in acute care by hospital
Overall, we identified 228 (10.4%) better than expected hospitals for AMI, 484 (13.0%) for heart failure and 673 (16.0%) for pneumonia. We identified 549 (25.1%) worse than expected hospitals for AMI, 840 (22.6%) for heart failure and 1,005 (24.0%) for pneumonia. By comparison, the CMS readmission measure identified 12 (0.5%) better than expected hospitals for AMI, 89 (2.4%) for heart failure and 78 (1.9%) for pneumonia. The CMS readmission measure identified 26 (1.2%) worse than expected hospitals for AMI, 129 (3.5%) for heart failure and 184 (4.4%) for pneumonia.
In weighted bivariate analyses, safety net status, ownership type, teaching status, advanced cardiac capacity, metropolitan status, census region, number of beds and nursing to bed ratio were all significantly associated with EDAC for heart failure and pneumonia. For AMI, ownership and advanced cardiac capacity were not significant (Table 1). In multivariable analyses simultaneously including all hospital characteristics (Table 2), for profit hospitals, major teaching hospitals, hospitals without cardiac surgery capability, urban hospitals, hospitals in the middle Atlantic region and hospitals with 500 or more beds all had significantly higher EDACs than hospitals without those characteristics for all three conditions. Hospitals with fewer than 2 nurses per bed had significantly higher EDACs than hospitals with 2 or more, except for the AMI measure. Safety net status was not associated with EDAC for AMI and heart failure, and was associated with fewer excess days for pneumonia. Census region had the largest variability among characteristics, with the Mountain region having on average 24.7 fewer excess days per 100 discharges than the Middle Atlantic region for pneumonia.
Table 1:
Bivariate associations of hospital characteristics with hospital excess days in acute care, by condition
| Description | AMI | Heart failure | Pneumonia | |||
|---|---|---|---|---|---|---|
| Mean EDAC (lower 95%, upper 95%) |
P | Mean EDAC (lower 95%, upper 95%) |
P | Mean EDAC (lower 95%, upper 95%) |
P | |
| Overall | 1.04 (−28.13, 34.72) | 1.43 (−35.17, 43.44) | 0.66 (−32.30, 41.28) | |||
| Safety net hospital | 0.0986 | 0.0345 | <0.001 | |||
| No | 0.75 (−0.15, 1.66) | 1.84 (0.95, 2.74) | 1.87 (1.06, 2.68) | |||
| Yes | 2.76 (0.61, 4.90) | −0.27 (−1.86, 1.32) | −3.35 (−4.68, −2.01) | |||
| Ownership | 0.1427 | <0.001 | <0.001 | |||
| Government | 2.14 (−0.57, 4.85) | −1.43 (−3.25, 0.38) | −4.11 (−5.61, −2.61) | |||
| Not-for-profit | 0.55 (−0.42, 1.52) | 1.18 (0.21, 2.15) | 0.82 (−0.04, 1.69) | |||
| For profit | 2.60 (0.59, 4.62) | 5.26 (3.41, 7.11) | 5.76 (3.97, 7.54) | |||
| Teaching status | <0.001 | <0.001 | <0.001 | |||
| Major teaching | 8.96 (6.58, 11.34) | 15.16 (12.35, 17.98) | 16.11 (13.27, 18.95) | |||
| Minor teaching | 1.56 (0.04, 3.07) | 3.97 (2.07, 5.86) | 6.98 (5.20, 8.77) | |||
| Non-teaching | −1.16 (−2.23, −0.09) | −1.44 (−2.32, −0.56) | −2.39 (−3.14, −1.63) | |||
| Cardiac facility | 0.1658 | <0.001 | <0.001 | |||
| CABG surgery | 1.32 (0.33, 2.31) | 4.45 (3.32, 5.59) | 5.36 (4.29, 6.44) | |||
| Cath Lab | −1.16 (−3.41, 1.10) | 2.03 (−0.31, 4.37) | 2.78 (0.65, 4.91) | |||
| Other | 1.41 (−0.79, 3.60) | −4.49 (−5.69, −3.29) | −6.12 (−7.07, −5.16) | |||
| Metropolitan status | <0.001 | <0.001 | <0.001 | |||
| Large central metro | 5.88 (4.22, 7.54) | 10.46 (8.62, 12.30) | 10.84 (8.96, 12.72) | |||
| Large fringe metro | 4.89 (3.01, 6.77) | 8.05 (6.16, 9.95) | 7.76 (5.98, 9.55) | |||
| Medium metro | −0.36 (−1.94, 1.22) | 0.11 (−1.64, 1.85) | 1.60 (0.05, 3.16) | |||
| Small metro | −2.72 (−4.77, −0.67) | −2.05 (−4.19, 0.08) | 0.17 (−1.81, 2.14) | |||
| Micropolitan | −4.60 (−6.94, −2.26) | −6.27 (−8.02, −4.51) | −6.65 (−8.12, −5.18) | |||
| Non-core (rural) | −11.76 (−18.01, −5.52) | −9.63 (−11.34, −7.91) | −10.38 (−11.57, −9.18) | |||
| Census Region | <0.001 | <0.001 | <0.001 | |||
| New England | 0.88 (−2.70, 4.46) | 1.87 (−1.50, 5.25) | 0.57 (−2.21, 3.35) | |||
| Middle Atlantic | 14.32 (11.80, 16.85) | 19.93 (17.14, 22.72) | 18.73 (15.82, 21.64) | |||
| South Atlantic | 5.58 (3.77, 7.39) | 7.72 (5.94, 9.50) | 9.61 (7.94, 11.28) | |||
| East North Central | −1.12 (−3.09, 0.84) | −2.81 (−4.59, −1.02) | −3.00 (−4.64, −1.37) | |||
| East South Central | 7.86 (5.02, 10.69) | 7.10 (4.73, 9.48) | 9.23 (7.17, 11.29) | |||
| West North Central | −5.15 (−7.54, −2.76) | −8.30 (−10.14, −6.47) | −8.04 (−9.47, −6.62) | |||
| West South Central | 0.17 (−2.14, 2.47) | −0.23 (−2.06, 1.60) | −2.92 (−4.50, −1.34) | |||
| Mountain | −10.70 (−13.27, −8.12) | −15.06 (−17.96, −12.16) | −12.91 (−14.86, −10.96) | |||
| Pacific | −4.27 (−6.57, −1.98) | −4.80 (−6.96, −2.65) | −3.61 (−5.74, −1.48) | |||
| Number of beds | <0.001 | <0.001 | <0.001 | |||
| <25 | −1.41 (−69.60, 66.77) | −14.62 (−17.76, −11.49) | −14.92 (−16.73, −13.11) | |||
| 24 to <50 | −9.25 (−14.74, −3.75) | −12.79 (−14.38, −11.20) | −13.55 (−14.69, −12.41) | |||
| 50 to <100 | −10.35 (−12.85, −7.86) | −7.33 (−9.07, −5.58) | −7.17 (−8.58, −5.76) | |||
| 100 to <200 | −3.36 (−4.93, −1.79) | 0.06 (−1.48, 1.59) | 0.68 (−0.72, 2.09) | |||
| 200 to <300 | 1.22 (−0.52, 2.95) | 4.95 (2.96, 6.94) | 7.57 (5.61, 9.54) | |||
| 300 to <400 | 2.58 (0.35, 4.81) | 4.68 (2.06, 7.29) | 8.49 (6.07, 10.91) | |||
| 400 to <500 | 5.41 (2.85, 7.98) | 10.04 (6.90, 13.17) | 10.95 (7.84, 14.06) | |||
| >=500 | 7.42 (5.32, 9.53) | 13.81 (11.06, 16.57) | 16.49 (13.94, 19.04) | |||
| Nursing to Bed Ratio | 0.2956 | 0.006 | <0.001 | |||
| <=1.0 | 0.82 (−3.07, 4.70) | −0.26 (−2.28, 1.77) | −4.37 (−5.83, −2.90) | |||
| >1.0 to 1.5 | 2.44 (0.76, 4.11) | 3.84 (2.36, 5.31) | 3.85 (2.46, 5.24) | |||
| >1.5 to 2.0 | 0.49 (−0.89, 1.87) | 1.73 (0.26, 3.21) | 1.94 (0.57, 3.31) | |||
| >2.0 | 0.61 (−0.81, 2.03) | −0.28 (−1.75, 1.18) | −0.90 (−2.21, 0.40) | |||
Table 2:
Multivariate association of hospital characteristics with excess days in acute care, by condition
| Description | AMI (N=2,184) |
Heart failure (N=3,720) |
Pneumonia (N=4,195) |
|||
|---|---|---|---|---|---|---|
| Mean EDAC (lower 95%, upper 95%) |
P | Mean EDAC (lower 95%, upper 95%) |
P | Mean EDAC (lower 95%, upper 95%) |
P | |
| Safety net hospital | 3.04 (−0.63, 6.72) | 0.10 | 0.30 (−2.72, 3.33) | 0.84 | −2.67 (−5.23, −0.12) | 0.04 |
| Ownership | 0.001 | <0.001 | <0.001 (<0.001, <0.001) | <.001 | ||
| Government | −2.04 (−6.40, 2.33) | 1.88 (−1.60, 5.36) | 4.00 (1.15, 6.85) | |||
| For profit | 3.99 (1.68, 6.31) | 4.89 (2.78, 7.01) | 4.93 (3.07, 6.79) | |||
| Not for profit | REF | REF | REF | |||
| Teaching status | 0.004 | <0.001 | 0.009 | |||
| Major teaching | 3.77 (0.64, 6.90) | 3.59 (0.44, 6.74) | 3.40 (0.40, 6.39) | |||
| Minor teaching | −1.00 (−2.99, 0.99) | −2.94 (−4.93, −0.95) | −1.01 (−2.81, 0.79) | |||
| Non-teaching | REF | REF | REF | |||
| Cardiac facility | 0.05 | <0.001 | 0.025 | |||
| Cardiac catheterization | 1.61 (−1.00, 4.23) | 1.10 (−1.24, 3.44) | 2.05 (0.02, 4.09) | |||
| Neither | 3.18 (0.61, 5.76) | 1.10 (−1.01, 3.22) | 2.31 (0.48, 4.13) | |||
| CABG capacity | REF | REF | REF | |||
| Metropolitan status | <0.001 | <0.001 | <.001 | |||
| Large fringe metro | −1.87 (−4.38, 0.65) | −2.40 (−4.73, −0.07) | −2.09 (−4.24, 0.05) | |||
| Medium metro | −6.18 (−8.34, −4.01) | −9.56 (−11.73, −7.40) | −8.03 (−10.03, −6.04) | |||
| Small metro | −6.32 (−8.77, −3.86) | −9.22 (−11.74, −6.71) | −6.60 (−8.87, −4.33) | |||
| Micropolitan | −7.27 (−10.40, −4.15) | −9.12 (−11.85, −6.39) | −8.05 (−10.40, −5.69) | |||
| Non-core (rural) | −13.77 (−20.50, −7.04) | −8.76 (−12.23, −5.29) | −6.39 (−9.17, −3.61) | |||
| Large central metro | REF | REF | REF | |||
| Census Region | <.001 | <0.001 | <.001 | |||
| New England | −4.22 (−8.04, −0.39) | −3.25 (−6.59, 0.09) | −6.13 (−9.08, −3.18) | |||
| Middle Atlantic | 7.64 (4.60, 10.67) | 10.45 (7.74, 13.15) | 6.64 (4.11, 9.17) | |||
| East North Central | −5.29 (−7.89, −2.69) | −7.63 (−9.93, −5.33) | −8.91 (−10.97, −6.85) | |||
| East South Central | 3.37 (0.01, 6.73) | 1.98 (−0.95, 4.91) | 2.62 (0.07, 5.17) | |||
| West North Central | −7.79 (−10.92, −4.65) | −10.06 (−12.82, −7.29) | −10.14 (−12.44, −7.85) | |||
| West South Central | −4.66 (−7.57, −1.75) | −5.82 (−8.38, −3.26) | −9.25 (−11.45, −7.06) | |||
| Mountain | −15.23 (−18.41, −12.06) | −19.58 (−22.81, −16.34) | −18.09 (−20.66, −15.53) | |||
| Pacific | −9.49 (−12.42, −6.56) | −11.26 (−13.97, −8.55) | −10.83 (−13.18, −8.48) | |||
| South Atlantic | REF | REF | REF | |||
| Number of beds | <.001 | <0.001 | <.001 | |||
| <50 | −9.10 (−16.47, −1.73) | −19.46 (−23.38, −15.54) | −24.18 (−27.54, −20.81) | |||
| 50 to <100 | −13.35 (−17.50, −9.20) | −16.37 (−19.94, −12.80) | −19.51 (−22.70, −16.33) | |||
| 100 to <200 | −6.20 (−9.30, −3.10) | −10.14 (−13.19, −7.09) | −12.85 (−15.69, −10.02) | |||
| 200 to <300 | −2.25 (−5.16, 0.66) | −5.68 (−8.62, −2.74) | −6.38 (−9.14, −3.62) | |||
| 300 to <400 | −1.22 (−4.07, 1.63) | −5.88 (−8.83, −2.93) | −5.35 (−8.17, −2.54) | |||
| 400 to <500 | 1.52 (−1.57, 4.62) | 0.03 (−3.22, 3.28) | −2.25 (−5.35, 0.84) | |||
| >500 | REF | REF | REF | |||
| Nursing to Bed Ratio | 0.24 | <0.001 | <0.001 | |||
| <=1.0 | −2.19 (−6.26, 1.88) | 3.01 (0.25, 5.77) | 0.92 (−1.28, 3.11) | |||
| >1.0 to 1.5 | 1.45 (−0.74, 3.65) | 3.50 (1.53, 5.47) | 3.44 (1.74, 5.14) | |||
| >1.5 to 2.0 | 0.74 (−1.12, 2.60) | 1.97 (0.21, 3.72) | 1.62 (0.08, 3.16) | |||
| >2.0 | REF | REF | REF | |||
The same associations were largely present when considering distribution of outliers rather than mean performance (Table 3), although safety net status, ownership type, cardiac care capacity and nursing ratio were not associated with outlier performance for AMI. The pneumonia hospital cohort was largest, with the largest differences in outlier performance, and is described here. A total of 19.5% of non-teaching hospitals were worse performing outliers for pneumonia, compared with 52.2% of major teaching hospitals; by contrast, 18.1% of non-teaching hospitals were better outliers compared with only 3.2% of major teaching hospitals. A total of 42.1% of hospitals in large urban areas were worse outliers, as opposed to 7.9% of hospitals in rural areas. Conversely, 7.1% of urban hospitals were better outliers, compared with 20.0% of rural hospitals. Hospitals without any advanced cardiac capacity were worse outliers 14.3% of the time and better outliers 18.9% of the time, compared with hospitals with cardiac surgery capability, of which 34.6% were worse outliers and 12.3% were better.
Table 3:
Distribution of outliers by hospital characteristic, by condition
| Description | AMI | Heart failure | Pneumonia | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Better | Worse | Total | Better | Worse | Total | Better | Worse | |||||||
| N | % | % | % | P | N | % | % | % | P | N | % | % | % | P | |
| All hospitals | 2184 | 100 | 10.4 | 25.1 | 3720 | 100 | 13.0 | 22.6 | 4195 | 100 | 16.0 | 24.0 | |||
| Safety net hospital | 0.3112 | <0.001 | <0.001 | ||||||||||||
| No | 1804 | 82.6 | 10.9 | 24.8 | 2745 | 73.8 | 13.6 | 23.9 | 2969 | 70.8 | 15.4 | 26.1 | |||
| Yes | 380 | 17.4 | 8.4 | 26.8 | 975 | 26.2 | 11.5 | 18.9 | 1226 | 29.2 | 17.7 | 18.8 | |||
| Ownership | 0.5302 | <0.001 | <0.001 | ||||||||||||
| Government | 233 | 10.7 | 9.9 | 26.6 | 699 | 18.8 | 11.6 | 16.3 | 915 | 21.8 | 18.4 | 16.7 | |||
| Not-for-profit | 1523 | 69.7 | 11.0 | 24.4 | 2388 | 64.2 | 14.7 | 23.3 | 2607 | 62.1 | 16.6 | 24.1 | |||
| For profit | 428 | 19.6 | 8.6 | 27.1 | 633 | 17.0 | 8.1 | 26.9 | 673 | 16.0 | 10.5 | 33.1 | |||
| Teaching status | <0.001 | <0.001 | <0.001 | ||||||||||||
| Major teaching | 244 | 11.2 | 6.6 | 43.0 | 249 | 6.7 | 4.4 | 48.2 | 251 | 6.0 | 3.2 | 52.2 | |||
| Minor teaching | 503 | 23.0 | 7.8 | 26.8 | 551 | 14.8 | 13.8 | 32.5 | 564 | 13.4 | 9.4 | 38.3 | |||
| Non-teaching | 1437 | 65.8 | 12.0 | 21.5 | 2920 | 78.5 | 13.6 | 18.5 | 3380 | 80.6 | 18.1 | 19.5 | |||
| Cardiac facility | 0.0668 | <0.001 | <0.001 | ||||||||||||
| CABG surgery | 1358 | 62.2 | 10.8 | 26.7 | 1563 | 42.0 | 11.6 | 29.4 | 1596 | 38.0 | 12.3 | 34.6 | |||
| Cath Lab | 375 | 17.2 | 11.7 | 21.3 | 452 | 12.2 | 13.7 | 25.7 | 457 | 10.9 | 15.8 | 32.2 | |||
| Other | 451 | 20.7 | 8.2 | 23.7 | 1705 | 45.8 | 14.1 | 15.5 | 2142 | 51.1 | 18.9 | 14.3 | |||
| Metropolitan status | <0.001 | <0.001 | <0.001 | ||||||||||||
| Large central metro | 582 | 26.6 | 6.2 | 32.1 | 672 | 18.1 | 6.4 | 37.6 | 689 | 16.4 | 7.1 | 42.1 | |||
| Large fringe metro | 465 | 21.3 | 8.8 | 29.9 | 624 | 16.8 | 9.5 | 31.7 | 648 | 15.4 | 11.1 | 35.8 | |||
| Medium metro | 471 | 21.6 | 11.7 | 21.7 | 632 | 17.0 | 15.7 | 22.3 | 675 | 16.1 | 14.8 | 26.8 | |||
| Small metro | 304 | 13.9 | 16.1 | 19.7 | 407 | 10.9 | 17.4 | 21.1 | 451 | 10.8 | 17.1 | 23.7 | |||
| Micropolitan | 299 | 13.7 | 11.4 | 17.7 | 674 | 18.1 | 17.4 | 13.4 | 725 | 17.3 | 24.0 | 15.9 | |||
| Non-core (rural) | 63 | 2.9 | 20.6 | 12.7 | 711 | 19.1 | 13.4 | 10.1 | 1007 | 24.0 | 20.0 | 7.9 | |||
| Census Region | <0.001 | <0.001 | <0.001 | ||||||||||||
| New England | 123 | 5.6 | 13.0 | 22.8 | 168 | 4.5 | 14.9 | 22.6 | 174 | 4.1 | 17.2 | 21.8 | |||
| Middle Atlantic | 291 | 13.3 | 2.7 | 47.4 | 366 | 9.8 | 3.6 | 52.7 | 373 | 8.9 | 4.8 | 52.8 | |||
| South Atlantic | 427 | 19.6 | 6.8 | 29.0 | 609 | 16.4 | 7.7 | 31.9 | 643 | 15.3 | 8.2 | 38.9 | |||
| East North Central | 365 | 16.7 | 9.3 | 20.3 | 645 | 17.3 | 18.6 | 19.1 | 672 | 16.0 | 21.0 | 19.8 | |||
| East South Central | 152 | 7.0 | 5.9 | 33.6 | 340 | 9.1 | 5.9 | 27.4 | 367 | 8.7 | 6.3 | 33.0 | |||
| West North Central | 157 | 7.2 | 17.8 | 11.5 | 433 | 11.6 | 15.9 | 7.6 | 589 | 14.0 | 18.7 | 8.0 | |||
| West South Central | 262 | 12.0 | 11.1 | 21.8 | 509 | 13.7 | 11.4 | 15.5 | 587 | 14.0 | 18.6 | 16.4 | |||
| Mountain | 138 | 6.3 | 25.4 | 8.7 | 245 | 6.6 | 27.8 | 9.0 | 339 | 8.1 | 29.8 | 7.1 | |||
| Pacific | 269 | 12.3 | 14.9 | 17.5 | 405 | 10.9 | 15.8 | 16.0 | 451 | 10.8 | 19.5 | 22.0 | |||
| Number of beds | <0.001 | <0.001 | <0.001 | ||||||||||||
| <25 | 3 | 0.1 | 0.0 | 33.3 | 174 | 4.7 | 16.7 | 5.2 | 361 | 8.6 | 22.4 | 4.7 | |||
| 24 to <50 | 58 | 2.7 | 10.3 | 6.9 | 759 | 20.4 | 16.9 | 7.9 | 939 | 22.4 | 25.0 | 5.9 | |||
| 50 to <100 | 237 | 10.9 | 18.6 | 7.6 | 627 | 16.9 | 15.2 | 11.5 | 704 | 16.8 | 19.0 | 13.4 | |||
| 100 to <200 | 657 | 30.1 | 11.4 | 19.2 | 886 | 23.8 | 12.3 | 21.8 | 908 | 21.6 | 13.9 | 26.0 | |||
| 200 to <300 | 488 | 22.3 | 8.4 | 27.9 | 522 | 14.0 | 10.9 | 34.9 | 524 | 12.5 | 10.7 | 42.2 | |||
| 300 to <400 | 301 | 13.8 | 11.3 | 32.6 | 308 | 8.3 | 11.7 | 35.4 | 311 | 7.4 | 7.1 | 43.4 | |||
| 400 to <500 | 168 | 7.7 | 6.0 | 31.0 | 171 | 4.6 | 8.8 | 44.4 | 174 | 4.1 | 6.9 | 50.6 | |||
| >=500 | 272 | 12.5 | 6.6 | 41.9 | 273 | 7.3 | 5.5 | 50.9 | 274 | 6.5 | 2.6 | 58.0 | |||
| Nursing to Bed Ratio | 0.5244 | <0.001 | <0.001 | ||||||||||||
| <=1.0 | 172 | 7.9 | 8.1 | 28.5 | 669 | 18.0 | 9.1 | 18.5 | 918 | 21.9 | 15.0 | 15.5 | |||
| >1.0 to 1.5 | 636 | 29.1 | 9.7 | 27.2 | 1019 | 27.4 | 10.7 | 25.5 | 1125 | 26.8 | 12.2 | 29.0 | |||
| >1.5 to 2.0 | 724 | 33.2 | 11.5 | 23.6 | 1018 | 27.4 | 14.4 | 25.2 | 1070 | 25.5 | 16.4 | 28.2 | |||
| >2.0 | 652 | 29.9 | 10.6 | 23.9 | 1014 | 27.3 | 16.5 | 19.6 | 1082 | 25.8 | 20.6 | 21.7 | |||
| Readmission Outlier Classification | <0.001 | <0.001 | <0.001 | ||||||||||||
| Better | 12 | 0.5 | 91.7 | 0.0 | 89 | 2.4 | 57.3 | 1.1 | 78 | 1.9 | 67.9 | 0.0 | |||
| No Different | 2146 | 98.3 | 10.1 | 24.4 | 3502 | 94.1 | 12.4 | 20.5 | 3933 | 93.8 | 15.8 | 21.0 | |||
| Worse | 26 | 1.2 | 0.0 | 96.2 | 129 | 3.5 | 0.0 | 93.0 | 184 | 4.4 | 0.0 | 96.7 | |||
However, some hospital characteristics that have been associated with likelihood of penalty on the readmission measures did not show similar associations with outlier EDAC performance. For example, 18.8% of safety net hospitals were worse outliers, compared with 26.1% of non-safety net hospitals; 17.7% were better outliers, compared with 15.4% of non-safety net hospitals. Public hospitals were worse outliers only 16.7% of the time, compared with 33.1% of for profit hospitals; while 18.4% were better outliers, compared with 10.5% of for profit hospitals.
The EDAC and readmission measures agreed on outlier status for two-thirds of hospitals (66% agreement for AMI, 68% for heart failure, 65% for pneumonia). Only one hospital was identified as a different type of outlier by each measure (better than expected for heart failure readmission but worse than expected for EDAC). However, the EDAC measure identified many more outliers than the readmission measure: 741 more outliers for AMI; 1,152 for heart failure and 1,447 for pneumonia.
Discussion
In this study of a comprehensive set of post-discharge outcomes encompassing readmission, emergency department and observation care use, we found marked variation in performance according to hospital characteristics, most of which were similar to those previously observed for readmissions. EDAC rates were highest among for profit hospitals, major teaching hospitals, urban hospitals, middle Atlantic hospitals, hospitals with more than 500 beds, and hospitals with fewer than 2 nurses per bed.
Readmission days form the bulk of the EDAC outcome, so it is not surprising that results are directionally similar to those seen for readmission metrics.10,13–15 The EDAC measures do, however, add some important information. The EDAC measures are able to identify more statistical outliers, providing a more granular view of performance by hospital characteristics. This particularly relevant for smaller hospitals, which consistently appear no different than average on readmission measures because of small sample size. We found that hospitals in rural and micropolitan regions or with fewer than 100 beds performed well on the EDAC measures, with one fifth to one quarter performing statistically better than average compared with 16% overall (and compared to virtually none on the readmission measures). Prior studies of readmissions have suggested that patients discharged from small volume hospitals have lower readmission rates; we are now able to confirm these findings for a broader set of outcomes, using measures that account for competing mortality risk.16 The reasons for these results remain uncertain. It is possible that rural hospitals have more barriers to return to acute care because of distance, or that rural and small hospitals may be more familiar with community resources. By contrast, large, urban, academic medical centers have disproportionately worse outcomes on the EDAC measures, as they do for readmissions.13 These differences may be a result of unmeasured additional patient risk, although large, academic medical centers tend to have disproportionately low mortality,27,28 suggesting their patients are unlikely to be markedly sicker than other hospitals. Competing mortality is not a likely explanation as these measures include only days alive. The quality of transitional and post-discharge care may also be different at these hospitals.29–31
Since the EDAC measures capture the length of stay of post-discharge events and include ED and observation stays, concern was raised during development of the measures that hospitals with few community resources or with underserved populations might be at a disadvantage on these measures. Yet we found that safety net hospitals and public hospitals do disproportionately well on the EDAC measures. We cannot determine from our data why this might be the case. It is possible that their patient population is disinclined to seek care because of financial or other hardships, though this should be somewhat mitigated by the fact that we include only older, insured patients in the measures. It is possible that these hospitals are better connected with community resources to facilitate post-discharge care, reducing post-discharge risk. Competing mortality, which is often considered as a potential mechanism for improved readmission rates, is unlikely to be an explanation because these measures only measure outcomes during days in which patients are alive.
It is notable that nursing ratios of at least 2 per bed were associated with lower EDAC rates. Prior studies of nursing staffing and readmission rates have been inconsistent, with some studies finding increased nursing ratios to be protective,14,26,32 but others finding no significant association.15,16 Studies previously finding no significant association used the same measure as in this study, whereas those finding protective effects used different, potentially more accurate measures (nurse equivalents/1000 patient-days, nurse’s report of patients per nurse on last shift, hours of nurse staffing/day). It is possible that the more nuanced outcomes used here allowed for detection of an effect even with our potentially less accurate nursing measure. This study adds to the evidence of the value of nursing staff in improving post-discharge outcomes.
EDAC rates were highest in the middle Atlantic region (New York, New Jersey, Pennsylvania), even after accounting for its disproportionately high number of urban centers and large teaching hospitals. High utilization in general has been observed in this region. New York has the highest number of contact days with the healthcare system for Medicare beneficiaries in the nation, including acute care visits, outpatient visits and testing. New Jersey is third and Pennsylvania is eighth.33 Interestingly, this region has fewer acute care beds per capita than the national average,34 but more physicians and specialists per capita.35 Moreover, this region has average or above average per capita capacity of skilled nursing facilities, with higher than national average occupancy rates and average or above average percentage of residents living in a nursing home,36 suggesting community resources are not lacking or being underutilized as a means of avoiding acute care. The reason for higher EDACs in this region therefore appears to be more a reflection of cultural practice patterns than of infrastructure and capacity.
Our study has several limitations. These analyses are observational and cannot be used to draw causal conclusions about contribution of hospital characteristics to outcomes. We were unable to exclude potentially planned observation stays or ED visits because there is no validated algorithm to do so. We did not account for socioeconomic status, consistent with the publicly reported measures. Our comparison of EDAC and readmission measure outliers is limited by the few outliers identified by the readmission measures. We studied only a handful of hospital and community characteristics; others, such as regional competition, community resources or financial status of the hospital, are likely also important. Small hospitals are less likely to be scored as outliers because their results have wider confidence intervals; however, the EDAC measures capture many more outliers than readmission measures. Finally, the EDAC measures include only patients with fee-for-service Medicare; results for younger, uninsured, managed Medicare or commercially-insured patients might be different.
In summary, we find that hospital characteristics are significantly associated with excess days in acute care, a comprehensive measure of post-discharge acute care utilization. For the most part, these associations are similar to but stronger than associations previously found for readmissions. We did not substantiate concerns that safety net or public hospitals would demonstrate greater use of acute care after discharge.
Supplementary Material
Acknowledgments
Financial support: This work was performed under contract HHSM-500-2013-13018I-Task Order HHSM-500-T0001, entitled, “Development, Reevaluation, and Implementation of Hospital Outcome/Efficiency Measures, Option Year 2,” funded by CMS, an agency of the US Department of Health and Human Services. This work was also supported by the Agency for Healthcare Research and Quality (R01HS022882). No funding source had any role in the study design; in the collection, analysis, and interpretation of data; or in the writing of the report. The CMS reviewed and approved the use of its data for this work and approved submission of the manuscript.
Footnotes
Conflicts of Interest: All authors have received support via their institution from the Centers for Medicare & Medicaid Services for the submitted work. In addition, Arjun Venkatesh reports honoraria from Martin Gottleib Associates, Emergency Medicine Associates, Emergency Medicine Physicians Group and funding from the Agency for Healthcare Research and Quality.
References
- 1.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, Observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374(16):1543–1551. [DOI] [PubMed] [Google Scholar]
- 2.Baier RR, Gardner RL, Coleman EA, Jencks SF, Mor V, Gravenstein S. Shifting the dialogue from hospital readmissions to unplanned care. The American journal of managed care. 2013;19(6):450–453. [PubMed] [Google Scholar]
- 3.Feng Z, Wright B, Mor V. Sharp rise in Medicare enrollees being held in hospitals for observation raises concerns about causes and consequences. Health affairs (Project Hope). 2012;31(6):1251–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vashi AA, Fox JP, Carr BG, et al. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA. 2013;309(4):364–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Horwitz LI, Wang C, Altaf FK, et al. Excess Days in Acute Care after Hospitalization for Heart Failure (version 1.1). Updated Measure Methodology Report. 2016; https://www.qualitynet.org/dcs/ContentServer?cid=1228775310395&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page. Accessed 14 Sep, 2016. [Google Scholar]
- 6.Horwitz LI, Wang C, Altaf FK, et al. Excess Days in Acute Care after Hospitalization for Acute Myocardial Infarction (version 1.1). Updated Measure Methodology Report. 2016; https://www.qualitynet.org/dcs/ContentServer?cid=1228775310395&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page. Accessed 14 Sep, 2016. [Google Scholar]
- 7.Horwitz LI, Wang C, Altaf FK, et al. Excess Days in Acute Care after Hospitalization for Pneumonia (version 1.0). Measure Methodology Report. 2016; https://www.qualitynet.org/dcs/ContentServer?cid=1228775310395&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page. Accessed 14 Sep, 2016. [Google Scholar]
- 8.Tsai TC, Joynt KE, Orav EJ, Gawande AA, Jha AK. Variation in surgical-readmission rates and quality of hospital care. N Engl J Med. 2013;369(12):1134–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berry JG, Toomey SL, Zaslavsky AM, et al. Pediatric readmission prevalence and variability across hospitals. JAMA. 2013;309(4):372–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horwitz LI, Partovian C, Lin Z, et al. Development and use of an administrative claims measure for profiling hospital-wide performance on 30-day unplanned readmission. Ann Intern Med. 2014;161(10 Suppl):S66–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Venkatesh AK, Wang C, Ross JS, et al. Hospital Use of Observation Stays: Cross-sectional Study of the Impact on Readmission Rates. Med Care. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singh S, Lin YL, Nattinger AB, Kuo YF, Goodwin JS. Variation in readmission rates by emergency departments and emergency department providers caring for patients after discharge. J Hosp Med. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA. 2013;309(4):342–343. [DOI] [PubMed] [Google Scholar]
- 14.Joynt KE, Jha AK. Who has higher readmission rates for heart failure, and why? Implications for efforts to improve care using financial incentives. Circ Cardiovasc Qual Outcomes. 2011;4(1):53–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Horwitz LI, Bernheim SM, Ross JS, et al. Hospital Characteristics Associated With Risk-standardized Readmission Rates. Med Care. 2017;55(5):528–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Horwitz LI, Lin Z, Herrin J, et al. Association of hospital volume with readmission rates: a retrospective cross-sectional study. BMJ. 2015;350:h447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lindenauer PK, Normand SL, Drye EE, et al. Development, validation, and results of a measure of 30-day readmission following hospitalization for pneumonia. J Hosp Med. 2011;6(3):142–150. [DOI] [PubMed] [Google Scholar]
- 18.Keenan PS, Normand SL, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29–37. [DOI] [PubMed] [Google Scholar]
- 19.Krumholz HM, Lin Z, Drye EE, et al. An administrative claims measure suitable for profiling hospital performance based on 30-day all-cause readmission rates among patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2011;4(2):243–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dorsey K, Grady JN, Desai N, et al. 2016 Condition-Specific Measures Updates and Specifications Report Hospital-Level 30-Day Risk-Standardized Readmission Measures. 2016; https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page. Accessed 11 Nov, 2017. [Google Scholar]
- 21.Grady JN, Lin Z, Wang C, et al. 2013 Condition-Specific Measures Updates and Specifications Report Hospital-Level 30-Day Risk-Standardized Readmission Measures for Acute Myocardial Infarction, Heart Failure, and Pneumonia (Version 6.0) 2013; https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page. Accessed 11 Nov, 2017.
- 22.Ross JS, Cha SS, Epstein AJ, et al. Quality of care for acute myocardial infarction at urban safety-net hospitals. Health Aff (Millwood). 2007;26(1):238–248. [DOI] [PubMed] [Google Scholar]
- 23.Gilman M, Adams EK, Hockenberry JM, Milstein AS, Wilson IB, Becker ER. Safety-net hospitals more likely than other hospitals to fare poorly under Medicare’s value-based purchasing. Health Aff (Millwood). 2015;34(3):398–405. [DOI] [PubMed] [Google Scholar]
- 24.National Center for Health Statistics. NCHS Urban-Rural Classification Scheme for Counties. 2006; http://www.cdc.gov/nchs/data_access/urban_rural.htm. Accessed 2013, 6 Sept.
- 25.Dartmouth Atlas Project, PerryUndem Research & Communications. The Revolving Door: A Report on U.S. Hospital Readmissions. Robert Wood Johnson Foundation; 2013: http://www.rwjf.org/content/dam/farm/reports/reports/2013/rwjf404178. Accessed 11 Sep 2015.
- 26.Ma C, McHugh MD, Aiken LH. Organization of Hospital Nursing and 30-Day Readmissions in Medicare Patients Undergoing Surgery. Med Care. 2015;53(1):65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taylor DH Jr., Whellan DJ, Sloan FA. Effects of admission to a teaching hospital on the cost and quality of care for Medicare beneficiaries. N Engl J Med. 1999;340(4):293–299. [DOI] [PubMed] [Google Scholar]
- 28.Allison JJ, Kiefe CI, Weissman NW, et al. Relationship of hospital teaching status with quality of care and mortality for Medicare patients with acute MI. JAMA. 2000;284(10):1256–1262. [DOI] [PubMed] [Google Scholar]
- 29.Frick AP, Martin SG, Shwartz M. Case-mix and cost differences between teaching and nonteaching hospitals. Med Care. 1985;23(4):283–295. [DOI] [PubMed] [Google Scholar]
- 30.Goldfarb MG, Coffey RM. Case-mix differences between teaching and nonteaching hospitals. Inquiry. 1987;24(1):68–84. [PubMed] [Google Scholar]
- 31.Shahian DM, Liu X, Meyer GS, Normand SL. Comparing teaching versus nonteaching hospitals: the association of patient characteristics with teaching intensity for three common medical conditions. Acad Med. 2014;89(1):94–106. [DOI] [PubMed] [Google Scholar]
- 32.Weiss ME, Yakusheva O, Bobay KL. Quality and cost analysis of nurse staffing, discharge preparation, and postdischarge utilization. Health Services Research. 2011;46(5):1473–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.The Dartmouth Atlas of Health Care. Average number of contact days with the health care system by beneficiary. 2012; http://www.dartmouthatlas.org/. Accessed 20 Sep, 2016.
- 34.The Dartmouth Atlas of Health Care. Acute care hospital beds per 1,000 residents. 2012; http://www.dartmouthatlas.org/. Accessed 20 Sep, 2016.
- 35.The Dartmouth Atlas of Health Care. All physicians per 100,000 residents; all specialists per 100,000 residents. 2011; http://www.dartmouthatlas.org/. Accessed 20 Sep, 2016.
- 36.Centers for Medicare & Medicaid Services. Nursing Home Data Compendium 2013 Edition. Vol 2016 Baltimore, MD: CMS; 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.