Abstract
Background
This study assessed the health related quality of life of family caregivers (FCs) of leukemia patients by using the health utility scores derived from the EuroQol five-dimensional (EQ-5D) questionnaire.
Methods
A cross-sectional survey was undertaken on 306 family caregivers of leukemia patients to assess their health utility using the EQ-5D-3L. Participants were recruited from three hospitals in China’s Heilongjiang province. The health utility scores of the participants were estimated based on the Chinese EQ-5D-3L value set and compared with those of the local general population. Factors predicting the health utility scores were identified through the Kruskal-Wallis analysis of variance and median regression analyses.
Results
FCs had lower health utility scores than the general population (p < 0.001). The participants with a lower socioeconomic status had lower utility scores and reported more problems than those with a higher socio-economic status. Better family function and higher social support were associated with higher health utility scores. The type of leukemia, household income, and social support are significant predictors of health utility scores of the FCs. Chronic lymphocytic leukemia, low socio-economic status, and low social support are associated with lower health utility scores of the FCs.
Conclusions
FCs for leukemia patients have lower health utility scores than the local general population, as measured by the EQ-5D-3L. There is an immediate need to address the health concerns of FCs, who play an important role in the Chinese health care system.
Electronic supplementary material
The online version of this article (10.1186/s12885-018-4855-y) contains supplementary material, which is available to authorized users.
Keywords: Family caregiver, Leukemia, EQ-5D, Health utility
Background
Leukemia is a group of hematologic cancers with malignant clonal proliferation arising from the bone marrow. They may present as an acute condition, such as acute lymphocytic leukemia (ALL) and acute myelogenous leukemia (AML), or as a chronic condition such as chronic lymphocytic leukemia (CLL) and chronic myelogenous leukemia (CML). Leukemia is the most common type of cancer in children. However, most leukemia patients are adults [6, 31].
Overall, the mortality rate of leukemia is very high. In 2012, about 352,000 people were diagnosed with leukemia globally and 75% (265,000) died [36]. In China, the number of leukemia patients ranks at 11 among all cancer cases; but it is the ninth most common cause of death resulting from cancers. In China, it is estimated that the number of new cases of leukemia were about 75,300 and around 53,400 died from leukemia in 2015 [4].
Cancer is a catastrophic event for the family, and can impose serious stress on both the patients and their family members [35]. Over the last few decades, significant progress has been made in the clinical treatment of leukemia in terms of the 5-year survival of the patients. However, the successful treatment of cancer often requires great physical and emotional commitment from family caregivers (FCs). Strong family support is essential for patients who go through the painful process of cancer treatments. The bleak prospect of cancer, coupled with the suffering of patients resulting from cancer treatments, often make FCs feel hopeless, fearful, guilty and regretful. Studies show that FCs caring for cancer patients usually experience worse levels of anxiety, depression, fatigue, sleep problems, and social isolation than FCs who did not care for patients with cancer [17, 28].
In China, a serious shortage in the nursing workforce is prevalent. According to the national statistics, China has 1.8 nurses per thousand population, well below the average (8.8) of Organisation for Economic Co-operation and Development (OECD) countries [23]. This indicates that FCs in China play an even greater role than their OECD counterparts as an important social source and emotional support for cancer patients [3]. In China, family members have a strong feeling of obligation and provide a wide range of care for patients that is otherwise provided by nurses, not only in homes but also in hospitals as well [10, 16, 41]. In addition, the family of cancer patients has to bear a heavy economic burden and they are highly vulnerable to catastrophic health spending despite the universal coverage of health insurance [19].
Health utility is a concept that has been widely adopted for the economic evaluation of the burden of diseases and the cost-effectiveness of interventional activities. A health utility reflects the preference of a population for different health states [12]. Given the significant role of FCs, it is reasonable to expect FCs to be taken into consideration in the economic evaluation of cancers and cancer interventions. However, there is a paucity of literature assessing the health utility of FCs for cancer patients [14]. Some previous studies have focused on the effects of cancer (including leukemia [24, 29, 43]) on various aspects of the health-related quality of life (HRQOL) of FCs [1]. Although these studies reached the conclusion that FCs of leukemia patients have significantly worse psychological, physical, social and environmental well-being than others [24, 29, 43], the absence of baseline utility scores for cancer FCs has jeopardised efforts to comprehensively evaluate the impact of cancers.
This study aimed to fill the literature gap by determining the health utility scores of FCs for patients with leukemia. We chose leukemia in this study for two reasons. First, empirical evidence shows that leukemia has a greater health impact on FCs than many other diseases [29, 46]. Second, it allows us to explore the associations between various patient conditions (eg. children vs adults, acute vs chronic conditions) and the health utility of their FCs.
Methods
Study design and data collection
We conducted a cross-sectional survey in Heilongjiang, a province in China with a medium-sized population (38.12 million in 2015) and economic products ($6386 per capita GDP in 2015) [34].
Three cancer centres were selected purposively because they were located in the capital city (Harbin) of Heilongjiang province serving as major referral centres for cancer patients. All of the three centres were affiliated to a tertiary hospital, providing specialist care to leukemia patients across the entire province. The investigators obtained permission from the participating hospitals to conduct the study and asked for a list of admitted leukemia patients over the period of data collection (July 2015 to February 2016). The eligibility of the participating patients for this study was assessed by their doctors and nurses. The participating patients had to have a dedicated primary family caregiver, this being the FC who provided their most of time to care without receiving any financial compensation. Then, 12 trained postgraduate research students were deployed to these centres to conduct face-to-face interviews using a structured questionnaire (Additional file 1). These interviewers did not have a service relationship with the participants. They approached the selected FCs, explained the purpose and protocol of the study, and sought written informed consent from the participants. The participants were encouraged to self-complete the questionnaire unless they requested assistance from the interviewers.
In total, 349 primary FCs were invited and 314 (90%) completed the questionnaire. Five returned questionnaires were excluded from the final analyses due to missing items that are essential for calculating health utility. This resulted in a final sample size of 306 (88% of the invited participants).
Measurements
Dependent variable - health utility
Health utility is a numeric index, with 0 indicating death and 1 representing perfect health. Usually, it is obtained using a generic HRQOL instrument [26]. In this study, we chose the EQ-5D-3L simply because it is the most commonly used instrument [11] and a Chinese population preference value set was recently made available [21].
The EQ-5D-3L contains five items measuring mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Respondents were asked to rate their current status and experience at three levels: no problems; moderate problems; extreme problems. Each of the combinations (a total of 243) of the five dimensions was given an index score based on a preference weight derived from the general population [21]. In the Chinese value set, the minimal preference weight is − 0.149, indicating a worse than death status, and the maximal preference weight is 1, indicating full health.
Independent variables
Health utility can be determined by many factors. In this study, we adjusted the health utility scores by the socio-economic characteristics of the FCs, such as age, gender, educational attainment, marital status, employment, household income, and relationship to patient.
Previous studies [22, 46] demonstrated that the characteristics of patients impose a significant impact on the need for family care and the level of emotional distress of the FCs. Our questionnaire captured the following data in relation to patient characteristics: age, gender, ethnicity, classification of medical insurance, time of diagnosis, and classification of leukemia. These characteristics were associated with how patients respond to their illness and the potential clinical outcomes of cancer treatments [5].
Workloads have been widely accepted as an important factor influencing HRQOL. High workloads can lead to stress, anxiety and depression [7]. In this study, we measured the average daily hours committed by the FCs for caring for the patient while in hospital and the overall annual load (months) of care. We used the Hospital Anxiety and Depression Scale (HADS) to measure the level of anxiety (7 items) and depression (7 items) of the FCs in the prior week. The level of anxiety or depression of FCs caring for leukemia patients was classified as severe (15–21 summed score), moderate (11–14 summed score), mild (8–10 summed score), or normal (0–7 summed score) [47].
Support from the family and community may alleviate the stress levels experienced by the FCs and subsequently improve their HRQOL [5, 18]. We measured the level of social support of FCs with the validated Social Support Rating Scale (SSRS), which resulted in a total score ranging from 66 to 0 [30, 42]. Respondents were divided equally into two groups: ‘high support’ or ‘low support’. We used the family APGAR (adaptation, partnership, growth, affection, and resolve) scale to assess the level of family support of FCs, which resulted in a total score ranging from 10 to 0 [8, 9]. Respondents were categorised into three groups for the purpose of statistical analyses. The summed score was graded as 0–3 (severely dysfunctional), 4–6 (moderately dysfunctional), and 7–10 (highly functional).
Data analyses
We reported the means and standard deviations (SDs) of the health utility scores of the FCs, as well as the medians and inter quartile ranges (IQs) of these scores. The distribution of the health utility scores measured by the EQ-5D-3L was biased, with 31.0% of respondents reporting the highest possible score of 1.
We compared the utility scores of the FCs with those of the local (Heilongjiang) general population using the Wilcoxon signed-rank test. Such a comparison was made for the following reasons: (1) Population norms were available from a representative sample of the local population in Heilongjiang as part of the fourth National Health Services Survey (NHSS) 2008, involving 15,875 individuals (from 5530 households) in 13 cities and counties [13]. (2) FCs came from this local population. (3) No comparable FCs for other patients were available.
The independent variables that were associated with the health utility of the FCs were identified through the Kruskal-Wallis analysis of variance (p < 0.05) and then entered into a multivariate median regression model (all independent variables were coded or transformed into categorical measurements). Ceiling effects are common in HRQOL studies [13, 37], including the EQ-5D-3L [2]. The literature recommends Tobit regression, censored least absolute deviations, and median regression to deal with data of such a censored nature [13, 14, 37], because they have theoretical advantages over the ordinary least squares estimator [13, 25, 38]. When censoring occurs in less than 50% of cases, median regression (robust to censoring, outliers and heteroskedasticity) is equivalent to censored least absolute deviations [25].
The findings of the median regression model were further confirmed by testing the difference in the prevalence of problems (moderate or extreme problems in mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) in the FCs across different categories of the independent variables using chi-square or Fisher’s exact tests.
Data analyses were conducted using SPSS version 22 and STATA version 11, with a p value less than 0.05 being deemed as statistically significant.
Results
Characteristics of FCs
The FCs for leukemia patients were mostly parents (43.5%) or spouses (37.3%) of the patients. The majority of FCs were married (94.1%) and had a job (77.1%). More than half (54.6%) were women. The FCs had an average experience of 15.5 months (SD = 6.9) of caring for the leukemia patients. More than 97% of FCs had a certain understanding level about the disease. They spent an average of 17.81 h (SD = 7.21) per day caring for the patients in hospitals. On average, the patients had been diagnosed with leukemia for 21 months. AML (53.3%) and ALL (30.4%) were the two major types of leukemia. The respondents had a mean score of 10.81 for anxiety and 8.17 for depression (Table 1).
Table 1.
Characteristics of patients and family caregivers (n = 306)
| Characteristics of family caregivers (FCs) | |
| Gender (% of women) | 167 (54.6%) |
| Age (years, Mean ± SD) | 41.20 ± 10. 81 |
| Ethnicity (% of Han) | 296 (96.7%) |
| Duration of caregiving (Month, Mean ± SD) | 15.52 ± 6.90 |
| Hours of caregiving per day (Hour, Mean ± SD) | 17.83 ± 7.21 |
| Understanding of the disease (n, %) | |
| Incompletely | 7 (2.3%) |
| Partial | 190 (62.1%) |
| Completely | 109 (35.6%) |
| Relationship to patient (n, %) | |
| Spouse | 114 (37.3%) |
| Parent | 133 (43.5%) |
| Child | 43 (14.0%) |
| Other | 16 (5.2%) |
| Level of education (n, %) | |
| No more than primary school | 38 (12.4%) |
| Middle or high school | 202 (66.0%) |
| University | 66 (21.6%) |
| Marital status (n, %) | |
| Married | 288 (94.1%) |
| Other | 18 (5.9%) |
| Employment (n, %) | |
| Employed | 236 (77.1%) |
| Retired | 22 (7.2%) |
| Unemployed | 48 (15.7%) |
| Religious belief (n, %) | |
| No | 260 (85.0%) |
| Yes | 46 (15.0%) |
| Annual household income (Yuan) | |
| ≤40,000 | 165 (53.9%) |
| 40,001–79,999 | 131 (42.8%) |
| ≥80,000 | 10 (3.3%) |
| Anxiety (Mean ± SD) | 10.81 ± 2.32 |
| Depression (Mean ± SD) | 8.17 ± 2.23 |
| Social support (Mean ± SD) | 37.00 ± 7.91 |
| Family function (APGAR score, Mean ± SD) | 6.76 ± 1.82 |
| Characteristics of patients | |
| Gender | 162 (52.9%) |
| Age | 35.65 ± 20.68 |
| Ethnicity | 292 (95.4%) |
| Types of leukemia (n, %) | |
| ALL | 93 (30.4%) |
| AML | 163 (53.3%) |
| CLL | 8 (2.6%) |
| CML | 42 (13.7%) |
| Medical insurance (n, %) | |
| Yes | 278 (90.8%) |
| No | 28 (9.2%) |
| Duration since diagnosis (Month, Mean ± SD) | 21.31 ± 18.37 |
Health utility scores of FCs
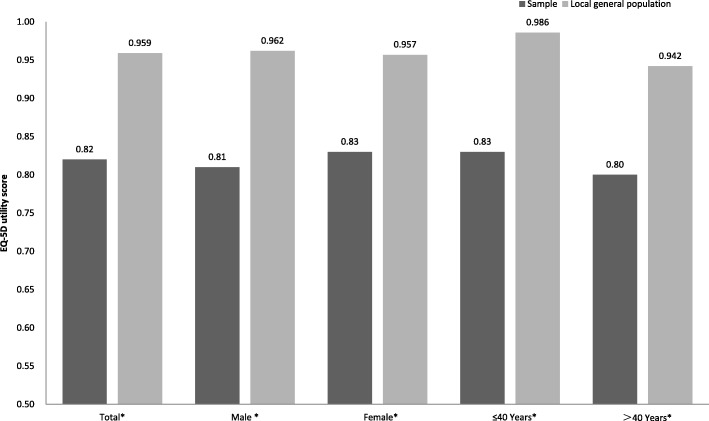
The FCs who cared for leukemia patients had lower health utility scores than the local (Heilongjiang) general populations (p < 0.001, Fig. 1) [13].
Fig. 1.
Health utility scores of the FCs for leukemia patients and the local population. * P < 0.001
The health utility scores of the FCs did not vary across different characteristics of the patients, apart from the type of leukemia (Table 2). The FCs caring for the two chronic conditions had a lower health utility score than those who cared for the two acute conditions.
Table 2.
Health utility scores of family caregivers
| Characteristics | Number | Mean ± SD | Median (range) | p |
|---|---|---|---|---|
| Family caregivers | ||||
| Gender | 0.546 | |||
| Male | 139 | 0.81 ± 0.19 | 0.87 (0.29–1.00) | |
| Female | 167 | 0.83 ± 0.15 | 0.87 (0.29–1.00) | |
| Age (years) | 0.092 | |||
| ≤40 | 154 | 0.83 ± 0.16 | 0.87 (0.29–1.00) | |
| >40 | 152 | 0.80 ± 0.17 | 0.80 (0.33–1.00) | |
| Relationship to patient | 0.010 | |||
| Spouse | 114 | 0.78 ± 0.19 | 0.80 (0.29–1.00) | |
| Parent | 133 | 0.83 ± 0.15 | 0.87 (0.33–1.00) | |
| Child | 43 | 0.85 ± 0.17 | 0.88 (0.29–1.00) | |
| Other | 16 | 0.91 ± 0.14 | 1.00 (0.61–1.00) | |
| Level of education | 0.106 | |||
| No more than primary school | 38 | 0.78 ± 0.16 | 0.78 (0.51–1.00) | |
| Middle or high school | 202 | 0.82 ± 0.18 | 0.87 (0.29–1.00) | |
| University | 66 | 0.85 ± 0.14 | 0.87 (0.40–1.00) | |
| Ethnicity | 0.386 | |||
| Han | 296 | 0.82 ± 0.17 | 0.87 (0.29–1.00) | |
| Other | 10 | 0.87 ± 0.12 | 0.88 (0.71–1.00) | |
| Religious belief | 0.077 | |||
| No | 260 | 0.81 ± 0.17 | 0.87 (0.29–1.00) | |
| Yes | 46 | 0.87 ± 0.14 | 0.88 (0.51–1.00) | |
| Marital status | 0.724 | |||
| Married | 288 | 0.82 ± 0.17 | 0.87 (0.29–1.00) | |
| Other | 18 | 0.85 ± 0.11 | 0.87 (0.61–1.00) | |
| Duration of caregiving (Months) | 0.856 | |||
| ≤6 | 109 | 0.81 ± 0.19 | 0.87 (0.29–1.00) | |
| 7–12 | 69 | 0.84 ± 0.15 | 0.87 (0.29–1.00) | |
| 13–24 | 70 | 0.81 ± 0.16 | 0.80 (0.41–1.00) | |
| >24 | 58 | 0.82 ± 0.16 | 0.87 (0.41–1.00) | |
| Time spent caregiving per day (Hours) | 0.037 | |||
| 0–12 | 126 | 0.83 ± 0.19 | 0.88 (0.29–1.00) | |
| 13–24 | 180 | 0.81 ± 0.16 | 0.80 (0.29–1.00) | |
| Understanding of the disease | 0.606 | |||
| Lacking | 7 | 0.78 ± 0.16 | 0.76 (0.53–1.00) | |
| Partial | 190 | 0.81 ± 0.18 | 0.83 (0.29–1.00) | |
| Fully | 109 | 0.83 ± 0.16 | 0.87 (0.33–1.00) | |
| Annual household income (Yuan) | 0.002 | |||
| ≤40,000 | 165 | 0.79 ± 0.17 | 0.78 (0.29–1.00) | |
| 40,001–79,999 | 131 | 0.85 ± 0.17 | 0.88 (0.29–1.00) | |
| ≥80,000 | 10 | 0.83 ± 0.16 | 0.87 (0.53–1.00) | |
| Employment | 0.021 | |||
| Employed | 236 | 0.83 ± 0.17 | 0.87 (0.29–1.00) | |
| Retired | 22 | 0.71 ± 0.20 | 0.77 (0.41–1.00) | |
| Unemployed | 48 | 0.82 ± 0.14 | 0.79 (0.47–1.00) | |
| Anxiety (HADS score) | 0.063 | |||
| Normal | 23 | 0.88 ± 0.15 | 0.88 (0.51–1.00) | |
| Mild | 118 | 0.83 ± 0.18 | 0.88 (0.29–1.00) | |
| Moderate | 148 | 0.80 ± 0.16 | 0.78 (0.29–1.00) | |
| Severe | 17 | 0.81 ± 0.17 | 0.78 (0.51–1.00) | |
| Depression (HADS score) | 0.393 | |||
| Normal | 120 | 0.82 ± 0.19 | 0.87 (0.29–1.00) | |
| Mild | 145 | 0.82 ± 0.15 | 0.87 (0.29–1.00) | |
| Moderate | 41 | 0.79 ± 0.16 | 0.78 (0.33–1.00) | |
| Social support (SSRSG score) | 0.000 | |||
| Low | 153 | 0.76 ± 0.17 | 0.78 (0.29–1.00) | |
| High | 153 | 0.88 ± 0.14 | 0.88 (0.50–1.00) | |
| Family function (APGAR score) | 0.000 | |||
| Severely dysfunctional | 74 | 0.75 ± 0.18 | 0.78 (0.29–1.00) | |
| Moderate dysfunctional | 155 | 0.82 ± 0.16 | 0.87 (0.29–1.00) | |
| Highly functional | 77 | 0.89 ± 0.15 | 1.00 (0.50–1.00) | |
| Patients | ||||
| Gender | 0.381 | |||
| Male | 144 | 0.81 ± 0.17 | 0.80 (0.29–1.00) | |
| Female | 162 | 0.82 ± 0.17 | 0.87 (0.29–1.00) | |
| Age(years) | 0.303 | |||
| <15 | 72 | 0.81 ± 0.15 | 0.79 (0.33–1.00) | |
| ≥15 | 234 | 0.82 ± 0.18 | 0.87 (0.29–1.00) | |
| Ethnicity | 0.326 | |||
| Han | 292 | 0.82 ± 0.17 | 0.87 (0.29–1.00) | |
| Other | 14 | 0.86 ± 0.16 | 0.88 (0.41–1.00) | |
| Types of leukemia | 0.037 | |||
| All | 93 | 0.83 ± 0.15 | 0.87 (0.29–1.00) | |
| AML | 163 | 0.83 ± 0.18 | 0.87 (0.29–1.00) | |
| CLL | 8 | 0.66 ± 0.17 | 0.73 (0.41–1.00) | |
| CML | 42 | 0.80 ± 0.18 | 0.78 (0.29–1.00) | |
| Duration since diagnosis (months) | 0.258 | |||
| 0–6 | 36 | 0.79 ± 0.19 | 0.78 (0.29–1.00) | |
| 7–12 | 82 | 0.83 ± 0.19 | 0.88 (0.29–1.00) | |
| 12–24 | 91 | 0.81 ± 0.17 | 0.78 (0.29–1.00) | |
| >24 | 97 | 0.82 ± 0.15 | 0.87 (0.41–1.00) | |
| Medical insurance | 0.092 | |||
| No | 278 | 0.77 ± 0.17 | 0.78 (0.41–1.00) | |
| Yes | 28 | 0.82 ± 0.17 | 0.87 (0.29–1.00) | |
No significant differences in health utility scores of the FCs were found across gender, age, level of education, ethnicity, marital status, and religious beliefs of the FCs (Table 2). Understanding of the disease, anxiety and depression of the FCs also did not appear as a significant factor associated with the health utility scores of the FCs. Although duration of caregiving was not a significant factor associated with health utility scores of the FCs, those who spent more time daily caring for patients in hospitals had lower health utility scores (p = 0.037). The FCs who were a spouse to the patients (p = 0.010), currently unemployed (p = 0.021), had a low income (p = 0.002), low social support (p < 0.001), and dysfunctional family (p < 0.001) tended to have a lower health utility score than the others.
The median regression model confirmed that the type of leukemia, household income, and social support were significant predictors of health utility scores of the FCs after controlling for differences in other factors. Table 3 presented standardised regression coefficients of these variables, indicating the direction and rate of the change in the utility index as a function of the above variables (both measured in units of their standard deviations). Those FCs who cared for CLL patients had lower health utility scores than those who cared for ALL patients. Higher social support was associated with higher health utility scores. The FCs with a household income in the middle range had higher health utility scores than those in the lower income range. However, with a further increase in income, this difference in health utility scores disappeared.
Table 3.
Predictors of health utility scores of FCs – results of median regression analyses
| Independent variables | Standardised regression coefficient | 95% Confidence Interval | p | |
|---|---|---|---|---|
| Relationship to patient | ||||
| Spouse | −0.076 | −0.161 | 0.009 | 0.081 |
| Parent | −0.046 | −0.132 | 0.040 | 0.293 |
| Child | −0.030 | −0.123 | 0.063 | 0.525 |
| Other (Reference) | ||||
| Time spent caregiving per day (Hours) | ||||
| 0–12 (Reference) | ||||
| 13–24 | − 0.030 | − 0.069 | 0.009 | 0.133 |
| Annual household income (Yuan) | ||||
| ≤40,000 (Reference) | ||||
| 40,001–79,999 | 0.049 | 0.010 | 0.088 | 0.014 |
| ≥80,000 | −0.021 | −0.126 | 0.084 | 0.695 |
| Employment | ||||
| Employed (Reference) | ||||
| Retired | −0.058 | −0.136 | 0.020 | 0.143 |
| Unemployed | −0.036 | −0.089 | 0.017 | 0.184 |
| Social support | ||||
| Low (Reference) | ||||
| High | 0.122 | 0.078 | 0.166 | 0.000 |
| Family function | ||||
| Highly functional (Reference) | ||||
| Severely dysfunctional | −0.046 | −0.110 | 0.018 | 0.157 |
| Moderate dysfunctional | −0.016 | −0.064 | 0.032 | 0.513 |
| Types of leukemia of patients | ||||
| ALL (Reference) | ||||
| AML | 0.000 | −0.046 | 0.046 | 1.000 |
| CLL | −0.125 | −0.239 | − 0.011 | 0.032 |
| CML | −0.035 | −0.099 | 0.029 | 0.285 |
Reported problems of FCs
The reported health problems provided further explanations on the findings revealed by the health utility analyses. Overall, more problems were reported by the FCs in pain/discomfort and anxiety/depression compared with the other domains (Table 4). However, statistical differences in reported problems appeared in different domains for the FCs with different characteristics. The FCs caring for CLL patients were more likely to report problems in mobility and self-care than those who cared for the other types of leukemia patients. Similarly, retired FCs were also more likely to report problems in mobility and self-care than those who were not retired. In contrast, relationship to patients was associated with differences in reported problems in self-care and anxiety/depression (more problems for spouse). Higher intensities of daily care for patients in hospitals and lower household incomes were associated with more reported problems in usual activities, pain/discomfort, and anxiety/depression. Lower social support was the only factor that was associated with more reported problems in all of the five domains (Table 4).
Table 4.
Reported problems of family caregivers (FCs)
| Characteristics | Mobility | Self-care | Usual Activity | Pain/Discomfort | Anxiety/Depression | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| % with problems | p* | % with problems | p* | % with problems | p* | % with problems | p* | % with problems | p* | |
| Family caregiver | ||||||||||
| Gender | 0.167 | 0.07 | 0.769 | 0.328 | 0.446 | |||||
| Male | 23.74 | 17.27 | 17.27 | 41.73 | 48.92 | |||||
| Female | 17.37 | 10.18 | 18.56 | 47.31 | 53.29 | |||||
| Age(years) | 0.040 | 0.004 | 0.924 | 0.498 | 0.998 | |||||
| ≤40 | 15.58 | 7.79 | 18.18 | 42.86 | 51.30 | |||||
| >40 | 25.00 | 19.08 | 17.76 | 46.71 | 51.32 | |||||
| Relationship to patient | 0.177 | 0.035 | 0.950 | 0.111 | 0.04 | |||||
| Spouse | 25.44 | 20.18 | 18.42 | 48.25 | 60.53 | |||||
| Parent | 19.55 | 9.77 | 18.05 | 48.12 | 48.87 | |||||
| Child | 13.95 | 11.63 | 18.60 | 30.23 | 41.86 | |||||
| Other | 6.25 | 0.00 | 12.50 | 31.25 | 31.25 | |||||
| Level of education | 0.308 | 0.617 | 0.055 | 0.016 | 0.399 | |||||
| No more than primary school | 23.68 | 18.42 | 31.58 | 65.79 | 52.63 | |||||
| Middle or high school | 21.78 | 12.87 | 16.83 | 40.59 | 53.47 | |||||
| University | 13.64 | 12.12 | 13.64 | 45.45 | 43.94 | |||||
| Ethnicity | 0.105 | 0.206 | 0.314 | 0.735 | 0.467 | |||||
| Han | 20.95 | 13.85 | 17.57 | 44.59 | 51.69 | |||||
| Other | 0.00 | 0.00 | 30.00 | 50.00 | 40.00 | |||||
| Religious belief | 0.356 | 0.051 | 0.471 | 0.141 | 0.110 | |||||
| No | 21.15 | 15.00 | 17.31 | 46.15 | 53.08 | |||||
| Yes | 15.22 | 4.35 | 21.74 | 36.96 | 41.3 | |||||
| Marital status | 0.110 | 0.085 | 0.882 | 0.646 | 0.391 | |||||
| Married | 21.18 | 14.24 | 18.06 | 44.44 | 50.69 | |||||
| Other | 5.56 | 0.00 | 16.67 | 50.00 | 61.11 | |||||
| Duration of caregiving (Months) | 0.065 | 0.574 | 0.734 | 0.962 | 0.110 | |||||
| ≤6 | 25.69 | 11.93 | 18.35 | 45.87 | 51.38 | |||||
| 7–12 | 11.59 | 13.04 | 17.39 | 42.03 | 50.72 | |||||
| 13–24 | 15.71 | 11.43 | 21.43 | 45.71 | 61.43 | |||||
| >24 | 25.86 | 18.97 | 13.79 | 44.83 | 39.66 | |||||
| Time spent caregiving per day (Hours) | 0.475 | 0.703 | 0.044 | 0.028 | 0.013 | |||||
| 0–12 | 22.22 | 14.29 | 12.70 | 37.30 | 42.86 | |||||
| 13–24 | 18.89 | 12.78 | 21.67 | 50.00 | 57.22 | |||||
| Understanding of disease | 0.243 | 0.041 | 0.243 | 0.053 | 0.936 | |||||
| Lacking | 42.86 | 42.86 | 14.29 | 0.00 | 57.14 | |||||
| Partial | 21.05 | 14.21 | 15.26 | 46.32 | 51.58 | |||||
| Fully | 17.43 | 10.09 | 22.94 | 44.95 | 50.46 | |||||
| Annual household income (Yuan) | 0.244 | 0.282 | 0.026 | 0.005 | 0.013 | |||||
| ≤40,000 | 23.03 | 13.33 | 23.03 | 53.33 | 58.79 | |||||
| 40,001–79,999 | 16.03 | 12.21 | 12.98 | 35.11 | 43.51 | |||||
| ≥80,000 | 30.00 | 30.00 | 0.00 | 30.00 | 30.00 | |||||
| Employment | 0.022 | 0.000 | 0.061 | 0.216 | 0.106 | |||||
| Employed | 19.92 | 12.29 | 16.53 | 42.8 | 49.15 | |||||
| Retired | 40.91 | 40.91 | 9.09 | 40.91 | 72.73 | |||||
| Unemployed | 12.5 | 6.25 | 29.17 | 56.25 | 52.08 | |||||
| Anxiety | 0.826 | 0.957 | 0.577 | 0.081 | 0.158 | |||||
| Normal | 13.04 | 13.04 | 13.04 | 26.09 | 34.78 | |||||
| Mild | 20.34 | 12.71 | 16.95 | 40.68 | 49.15 | |||||
| Moderate | 20.95 | 13.51 | 18.24 | 51.35 | 56.76 | |||||
| Severe | 23.53 | 17.65 | 29.41 | 41.18 | 41.18 | |||||
| Depression | 0.176 | 0.382 | 0.013 | 0.469 | 0.008 | |||||
| Normal | 25.00 | 16.67 | 11.67 | 43.33 | 41.67 | |||||
| Mild | 15.86 | 11.72 | 19.31 | 43.45 | 54.48 | |||||
| Moderate | 21.95 | 9.76 | 31.71 | 53.66 | 68.29 | |||||
| Social support | 0.000 | 0.029 | 0.011 | 0.000 | 0.000 | |||||
| Low | 30.72 | 17.65 | 23.53 | 60.78 | 68.63 | |||||
| High | 9.8 | 9.15 | 12.42 | 28.76 | 33.99 | |||||
| Family function | 0.023 | 0.075 | 0.129 | 0.000 | 0.000 | |||||
| Severely dysfunctional | 31.08 | 18.92 | 24.32 | 58.11 | 64.86 | |||||
| Moderate dysfunctional | 18.06 | 14.19 | 18.06 | 47.74 | 53.55 | |||||
| Highly functional | 14.29 | 6.49 | 11.69 | 25.97 | 33.77 | |||||
| Patients | ||||||||||
| Gender | 0.421 | 0.566 | 0.127 | 0.416 | 0.840 | |||||
| Male | 22.22 | 14.58 | 21.53 | 47.22 | 50.69 | |||||
| Female | 18.52 | 12.35 | 14.81 | 42.59 | 51.85 | |||||
| Age (years) | 0.594 | 0.066 | 0.154 | 0.067 | 0.274 | |||||
| <15 | 18.06 | 6.94 | 23.61 | 54.17 | 56.94 | |||||
| ≥15 | 20.94 | 15.38 | 16.24 | 41.88 | 49.57 | |||||
| Ethnicity | 0.211 | 0.482 | 0.713 | 0.883 | 0.920 | |||||
| Han | 20.89 | 13.7 | 18.15 | 44.86 | 51.37 | |||||
| Other | 7.14 | 7.14 | 14.29 | 42.86 | 50.00 | |||||
| Types of leukemia | 0.008 | 0.003 | 0.358 | 0.227 | 0.342 | |||||
| ALL | 17.2 | 6.45 | 13.98 | 48.39 | 55.91 | |||||
| AML | 17.79 | 14.72 | 19.02 | 41.1 | 48.47 | |||||
| CLL | 62.50 | 50.00 | 37.50 | 75.00 | 75.00 | |||||
| CML | 28.57 | 16.67 | 19.05 | 45.24 | 47.62 | |||||
| Duration since diagnosis (months) | 0.987 | 0.902 | 0.801 | 0.224 | 0.641 | |||||
| 0–6 | 22.22 | 13.89 | 22.22 | 52.78 | 55.56 | |||||
| 7–12 | 19.51 | 10.98 | 19.51 | 35.37 | 51.22 | |||||
| 12–24 | 19.78 | 14.29 | 15.38 | 47.25 | 54.95 | |||||
| >24 | 20.62 | 14.43 | 17.53 | 47.42 | 46.39 | |||||
| Medical insurance | 0.251 | 0.467 | 0.041 | 0.326 | 0.517 | |||||
| No | 28.57 | 17.86 | 32.14 | 53.57 | 57.14 | |||||
| Yes | 19.42 | 12.95 | 16.55 | 43.88 | 50.72 | |||||
*p values derived from Chi Square tests
We also found that older FCs were more likely to report problems in mobility and self-care than their younger counterparts. Female FCs reported less problems in self-care than male FCs. The FCs with lower education tended to report more pain/discomfort problems than those with higher levels of education. Those who had a poorer understanding of the disease reported more problems in self-care than those who had a better understanding of the disease. The depressed FCs were more likely to report problems in usual activities and anxiety/depression than those less depressed. Highly functional families were associated with a lower likelihood of the FCs reporting problems in mobility, pain/discomfort, and anxiety/depression.
Discussion
Family caregivers (FCs) of leukemia patients have lower health utility scores than the local general population. This finding is consistent with other studies which showed that FCs caring for cancer patients, including leukemia patients, had a lower HRQOL [40, 43]. It is evident that the impact of caregiving on the health utility of FCs depends on the type of disease of the patients [14]. The FCs caring for cancer patients are amongst those who are likely to be exposed to the greatest impact. We found that the health utility of FCs varies with the condition of leukemia patients, with CLL having a greater impact on the FCs than other types of leukemia. Unlike in some western countries [15], CLL in China is rare, but has a worse prognosis than other types of leukemia.
Cost-utility analyses have been increasingly used for determining priorities in health care interventions and budgetary decisions. However, little attention has been paid to FCs in such cost-utility analyses [14]. We strongly advocate for the consideration of FCs, not only because FCs are often the primary source of support for patients in many health systems, but also because the poor HRQOL of FCs may impair their ability to care for the patients and eventually result in negative consequences on patient care outcomes. The cost-utility analyses should adopt a value set derived from the local general population. This study shows that the mean health utility scores of the study sample (family caregivers) and the local general population in Heilongjiang are high: 0.82 and 0.959, respectively. This may be a result of relatively younger age structure because the EQ-5D index scores usually decline with age. Previous studies also revealed that Chinese people are less likely to report problems in the EQ-5D compared with most populations in the western countries [39]. In addition, people’s preferences can be quite different under different cultures [33, 39].
The FCs for leukemia patients with a lower socio-economic status have worse health utility than those with a higher socio-economic status. In our study, the lowest health utility of the FCs appeared in those with the lowest household income. They reported more problems in usual activities, pain/discomfort, and anxiety/depression. Similar findings were also reported in other studies [46]. The leukemia patients living in a household with low socio-economic status usually demand more family care because they have limited resources to pay for other supportive services [14, 32, 45]. Sadly, the low health utility of their FCs may jeopardise their capability of caring for the patients. The high demand of family care for the patients with low socio-economic status itself may be blamed for the low health utility of the FCs. We found that higher commitment intensity of care is associated with lower health utility of the FCs, although such an association disappeared after controlling for difference in other factors in the median regression model.
It is important to acknowledge that financial support alone may not be able to offer a solution to the low heath utility problem of the FCs for leukemia patients. We found that the highest income group (≥¥80,000) of FCs had a similar level of health utility as those with the lowest income (≤¥40,000). Health utility scores are derived from HRQOL assessment, which is a subjective measurement. Empirical evidence shows that health utility scores are sensitive to changes in expectations [26]. Often, people’s expectations rise with increased income, which may lower their HRQOL and health utility scores [20].
Social support can play an important role in improving the health utility of FCs for leukemia patients. We found in this study that the FCs with lower social support reported more problems in all of the five domains of EQ-5D-3L, and social support level is a strong predictor of the health utility of the leukemia patients’ FCs in the median regression model. So far, programs designed to support FCs (e.g. respite care) are lacking in China, despite increased appreciation of the contribution of FCs. The decades’ experience of “one child” family planning policy in China has been accompanied with a paradigm shift of supportive services from families to communities [27]. However, it is unrealistic to expect any dramatic decline in the role of family support in health care due to serious shortage in the nursing workforce. FCs will continue to play an essential role in the health care system in China.
This study has the following limitations. First, this study was conducted in three large hospitals in one province, which limits its generalisability. Second, because the participants of this study were recruited in hospitals, the patients they cared for were more likely to be at an advanced stage of cancer [44]. This may bias the estimation of the health utility of the FCs. Third, since this is a cross-sectional survey, no causal inferences can be made.
Conclusion
FCs for leukemia patients have lower health utility scores than the local general population, as measured by the EQ-5D-3L. The type of leukemia, household income, and social support are significant predictors of health utility scores of the FCs. CLL, low socio-economic status, and low social support are associated with lower health utility scores of the FCs. Cost-utility analyses should consider not only the health utility of patients but also the health utility of FCs. Further studies are warranted to compare the health utility of FCs for different patients.
Additional file
Health Related Quality of Life Questionnaire Survey. (DOCX 46 kb)
Acknowledgements
The authors are most grateful to the study participants.
Funding
This study was supported by the National Natural Scientific Foundation of China (Grant No.71503062) and China Postdoctoral Fund (Grant No. 2017M611402). Part of this study was also funded by the Heilongjiang Postdoctoral Fund (Grant No. LBH-Z16137, LBH-Z16240), Key Lab of Health Technology Assessment, National Health and Family Planning Commission of the People’s Republic of China (Grant No. FHTA2017-08), the HMU Innovation Fund (Grant No. 2017RWZX08), the Hospital Foundation of the First Affiliated Hospital of Harbin Medial University (Grant No. 2015B019) and the Health and Family Planning Commission of Heilongjiang Province project (NO. 2009–230).
Availability of data and materials
Data are available on request.
Abbreviations
- ALL
Acute lymphocytic leukemia
- AML
Acute myelogenous leukemia
- APGAR
(Adaptation, partnership, growth, affection, and resolve) scale
- CLL
Chronic lymphocytic leukemia
- CML
Chronic myelogenous leukemia
- EQ-5D
EuroQol five-dimensional
- FCs
Family caregivers
- GDP
Gross domestic product
- HADS
Hospital Anxiety and Depression Scale
- HRQOL
Health-related quality of life
- OECD
Organisation for Economic Co-operation and Development
Authors’ contributions
WF, LS and YY conceived the study, participated in the design, and made substantial contribution to the intellectual content of the manuscript. HY1, HZ and JY participated in the design of the study, acquisition and interpretation of data, and writing of the manuscript. WH led the design of the study, participated in data acquisition, performed statistical analyses and drafted the manuscript. CL1, GL and LL participated in the design of the study, critical review of the statistical analyses, interpretation of the statistical findings, and revision of the manuscript. CL2, HY2 and JZ contributed to the conceptualisation of the study, participated in the interpretation of the results, and helped draft the manuscript. All authors read and approved the final manuscript and agreed to be accountable for all aspects of the work.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Harbin Medical University (Project Identification Code: HMUIRB2014012). Each potential participate was given an explanation of the study and written consent was obtained from those who agreed to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Hongjuan Yu, Email: yuhongjuan2008@163.com.
Huan Zhang, Email: zhanghuan2010000@163.com.
Jinjin Yang, Email: hrbmuyjj@126.com.
Chaojie Liu, Email: c.liu@latrobe.edu.au.
Chengfang Lu, Email: momi22@163.com.
Hongbin Yang, Email: Yang21hongbin@163.com.
Weidong Huang, Email: weidong218@126.com.
Jin Zhou, Email: jinzhouh85@163.com.
Wenqi Fu, Email: fuwenqi6688@163.com.
Linmei Shi, Email: slm_jl@163.com.
Yan Yan, Email: yyfruit2017@sina.com.
Guoxiang Liu, Email: lgx6301@163.com.
Limin Li, Email: Llilimin@163.com.
References
- 1.Awadalla AW, Ohaeri JU, Gholoum A, Khalid AOA, Hamad HMA, Jacob A. Factors associated with quality of life of outpatients with breast cancer and gynecologic cancers and their family caregivers: a controlled study. BMC Cancer. 2007;7:102. doi: 10.1186/1471-2407-7-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bharmal M, Rd TJ. Comparing the EQ-5D and the SF-6D descriptive systems to assess their ceiling effects in the US general population. Value Health. 2006;9:262. doi: 10.1111/j.1524-4733.2006.00108.x. [DOI] [PubMed] [Google Scholar]
- 3.Bultz BD, Speca M, Brasher PM, Geggie PHS, Page SA. A randomized controlled trial of a brief psychoeducational support group for partners of early stage breast cancer patients. Psycho-Oncology. 2000;9:303–313. doi: 10.1002/1099-1611(200007/08)9:4<303::AID-PON462>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 4.Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 5.Choi YS, Hwang SW, Hwang IC, Lee YJ, Kim YS, Kim HM, Youn CH, Ahn HY, Koh S-J. Factors associated with quality of life among family caregivers of terminally ill cancer patients. Psycho-Oncology. 2016;25:217–224. doi: 10.1002/pon.3904. [DOI] [PubMed] [Google Scholar]
- 6.de Oliveira C, Bremner KE, Liu N, Greenberg ML, Nathan PC, McBride ML, Krahn MD. Costs of cancer care in children and adolescents in Ontario, Canada. Pediatr Blood Cancer. 2017;64(11). [DOI] [PubMed]
- 7.Doubova Svetlana V., Infante-Castañeda Claudia. Factors associated with quality of life of caregivers of Mexican cancer patients. Quality of Life Research. 2016;25(11):2931–2940. doi: 10.1007/s11136-016-1322-6. [DOI] [PubMed] [Google Scholar]
- 8.Fan L, Guang Z, Songyuan L, Tianlun Z, Zhiqiang Z. A study on validity and reliability of the family APGAR. Chin J Public Health. 1999;15:27–28. [Google Scholar]
- 9.Fan L, Yuan G. The family APGAR questionnaire and its clinical application foreign medical sciences( series of hospital management) 1995. pp. 56–59. [Google Scholar]
- 10.Ge C, Yang X, Fu J, Chang Y, Wei J, Zhang F, Nutifafa AE, Wang L. Reliability and validity of the Chinese version of the caregiver reaction assessment. Psychiatry Clin Neurosci. 2011;65:254–263. doi: 10.1111/j.1440-1819.2011.02200.x. [DOI] [PubMed] [Google Scholar]
- 11.Group EQC EuroQol--a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 12.Guyatt G, Jaeschke R, Feeny D, Patrick D. Measurement in clinical trials: choosing the right approach. 1996. [Google Scholar]
- 13.Huang Weidong, Yu Hongjuan, Liu Chaojie, Liu Guoxiang, Wu Qunhong, Zhou Jin, Zhang Xin, Zhao Xiaowen, Shi Linmei, Xu Xiaoxue. Assessing Health-Related Quality of Life of Chinese Adults in Heilongjiang Using EQ-5D-3L. International Journal of Environmental Research and Public Health. 2017;14(3):224. doi: 10.3390/ijerph14030224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khanna R, Jariwala K, Bentley JP. Health utility assessment using EQ-5D among caregivers of children with autism. Value Health. 2013;16:778–788. doi: 10.1016/j.jval.2013.04.007. [DOI] [PubMed] [Google Scholar]
- 15.Klassen AF, Klaassen R, Dix D, Pritchard S, Yanofsky R, O’Donnell M, Scott A, Sung L. Impact of caring for a child with cancer on parents’ health-related quality of life. J Clin Oncol. 2008;26:5884–5889. doi: 10.1200/JCO.2007.15.2835. [DOI] [PubMed] [Google Scholar]
- 16.Kong EH. The influence of culture on the experiences of Korean, Korean American, and Caucasian - American family caregivers of frail older adults. J Korean Acad Nurs. 2007;37:213–220. doi: 10.4040/jkan.2007.37.2.213. [DOI] [PubMed] [Google Scholar]
- 17.Kurtz M, Kurtz J, Given C, Given B. Concordance of cancer patient and caregiver symptom reports. Cancer Pract. 1995;4:185–190. [PubMed] [Google Scholar]
- 18.Lee YJ, Kim JE, Choi YS, Hwang IC, Hwang SW, Kim YS, Kim HM, Ahn HY, Kim SJ. Quality of life discordance between terminal cancer patients and family caregivers: a multicenter study. Support Care Cancer. 2016;(7):2853–60. [DOI] [PubMed]
- 19.Li Y, Wu Q, Liu C, Ning N, Liu G, Hao H, Kang Z. Catastrophic health expenditure and rural household impoverishment in China: what role does the new cooperative health insurance scheme play? PLoS One. 2014;9:e93253. doi: 10.91371/journal.pone.0093253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu C, Li N, Ren X, Liu D. Is traditional rural lifestyle a barrier for quality of life assessment? A case study using the Short Form 36 in a rural Chinese population. Qual Life Res. 2010;19:31–36. doi: 10.1007/s11136-009-9567-y. [DOI] [PubMed] [Google Scholar]
- 21.Liu GG, Wu H, Li M, Gao C, Luo N. Chinese time trade-off values for EQ-5D health states. Value Health. 2014;17:597–604. doi: 10.1016/j.jval.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 22.Northouse L, Williams AL, Given B, McCorkle R. Psychosocial care for family caregivers of patients with cancer. J Clin Oncol. 2012;30:1227–1234. doi: 10.1200/JCO.2011.39.5798. [DOI] [PubMed] [Google Scholar]
- 23.OECD . OECD health statistics 2014: how does China compare? 2014. [Google Scholar]
- 24.Pathirana TI, Goonawardena CSE, Wijesiriwardane I. Quality of life of caregivers and impact on the nuclear family of children with leukaemia in the National Cancer Institute of Sri Lanka. J Postgrad Inst Med. 2015;2:18. doi: 10.4038/jpgim.7863. [DOI] [Google Scholar]
- 25.Powell JL. Least absolute deviations estimation for the censored regression model. J Econ. 1984;25:303–325. doi: 10.1016/0304-4076(84)90004-6. [DOI] [Google Scholar]
- 26.Räsänen P, Roine E, Sintonen H, Semberg-Konttinen V, Ryynänen OP, Roine R. Use of quality-adjusted life years for the estimation of effectiveness of health care: a systematic literature review. Int J Technol Assess Health Care. 2006;22:235. doi: 10.1017/S0266462306051051. [DOI] [PubMed] [Google Scholar]
- 27.Ren X, Meng H, Liu C, Wu J, Dong B, Li N. Family structure and support for the oldest old: a cross-sectional study in Dujiangyan, China. Fam Med Commun Health. 2015;3:5–14. doi: 10.15212/FMCH.2015.0132. [DOI] [Google Scholar]
- 28.Romito F, Goldzweig G, Cormio C, Hagedoorn M, Andersen BL. Informal caregiving for cancer patients. Cancer. 2013;119:2160–2169. doi: 10.1002/cncr.28057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Santo EARE, Gaíva MAM, Espinosa MM, Barbosa DA, Belasco AGS. Taking care of children with cancer: evaluation of the caregivers’ burden and quality of life. Rev Lat Am Enfermagem. 2011;19:515–522. doi: 10.1590/S0104-11692011000300010. [DOI] [Google Scholar]
- 30.Shuiyuan X, Desen Y. The effect of social support on physical and psychological health. J Chin Psychiatry. 1987;1:183–187. [Google Scholar]
- 31.Sneha LM, Sai J, Ashwini S, Ramaswamy S, Rajan M, Scott JX. Financial burden faced by families due to out-of-pocket expenses during the treatment of their cancer children: an Indian perspective. Indian J Med Paediatr Oncol. 2017;38:4–9. doi: 10.4103/0971-5851.203493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Son KY, Lee CH, Park SM, Lee CH, Oh SI, Oh B, Tak SH, Cho B, Lee K, Lee SH. The factors associated with the quality of life of the spouse caregivers of patients with cancer: a cross-sectional study. J Palliat Med. 2012;15:216–224. doi: 10.1089/jpm.2011.0305. [DOI] [PubMed] [Google Scholar]
- 33.Sorensen J, Davidsen M, Gudex C, Pedersen KM, Bronnum-Hansen H. Danish EQ-5D population norms. Scand J Public Health. 2009;37:467–474. doi: 10.1177/1403494809105286. [DOI] [PubMed] [Google Scholar]
- 34.Statistics HPBo . Heilongjiang statistical yearbook. Peking: China Statistics Press; 2015. [Google Scholar]
- 35.Stenberg U, Ruland CM, Miaskowski C. Review of the literature on the effects of caring for a patient with cancer. Psycho-Oncology. 2009;19:1013–1025. doi: 10.1002/pon.1670. [DOI] [PubMed] [Google Scholar]
- 36.Stewart B, Wild CP. World cancer report 2014: World; 2016. http://www.who.int/cancer/publications/WRC_2014/en/
- 37.Sullivan PW, Ghushchyan VH. EQ-5D scores for diabetes-related comorbidities. Value Health. 2016;19:1002–1008. doi: 10.1016/j.jval.2016.05.018. [DOI] [PubMed] [Google Scholar]
- 38.Sullivan PW, Ghushchyan VH, Globe G, Sucher B. Health-related quality of life associated with systemic corticosteroids. Qual Life Res. 2017;26:1037–1058. doi: 10.1007/s11136-016-1435-y. [DOI] [PubMed] [Google Scholar]
- 39.Sun S, Chen J, Johannesson M, Kind P, Xu L, Zhang Y, Burström K. Population health status in China: EQ-5D results, by age, sex and socio-economic status, from the National Health Services Survey 2008. Qual Life Res. 2010;20:309–320. doi: 10.1007/s11136-010-9762-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Suwen F, Jun L, Fang Y, Zhishu Z. Relative factors of life quality of principle caregivers of gynecologic cancer patients. Chin J Nurs. 2006;41:402–404. [Google Scholar]
- 41.Tang YY, Chen SP. Health promotion behaviors in Chinese family caregivers of patients with stroke. Health Promot Int. 2002;17:329–339. doi: 10.1093/heapro/17.4.329. [DOI] [PubMed] [Google Scholar]
- 42.Xiangdong W, Xilin W, Hong M. Rating scales for mental health. Beijing: Chinese Mental Health Journal; 1999. [Google Scholar]
- 43.Yamazaki S, Sokejima S, Mizoue T, Eboshida A, Fukuhara S. Health-related quality of life of mothers of children with leukemia in Japan. Qual Life Res. 2005;14:1079–1085. doi: 10.1007/s11136-004-3288-z. [DOI] [PubMed] [Google Scholar]
- 44.Yang SM, Li JY, Gale RP, Huang XJ. The mystery of chronic lymphocytic leukemia (CLL): why is it absent in Asians and what does this tell us about etiology, pathogenesis and biology? Blood Rev. 2015;29:205–213. doi: 10.1016/j.blre.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 45.Yeh PM, Wierenga ME, Yuan SC. Influences of psychological well-being, quality of caregiver-patient relationship, and family support on the health of family caregivers for cancer patients in Taiwan. Asian Nurs Res. 2009;3:154–166. doi: 10.1016/S1976-1317(09)60027-X. [DOI] [PubMed] [Google Scholar]
- 46.Yu H, Li L, Liu C, Huang W, Zhou J, Fu W, Ma Y, Li S, Chang Y, Liu G, Wu Q. Factors associated with the quality of life of family caregivers for leukemia patients in China. Health Qual Life Outcomes. 2017;15:55. doi: 10.1186/s12955-017-0628-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zuoji Z. Manual of behavioral medicine scale. Beijing: Chin Med Multimedia Press; 2005. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Health Related Quality of Life Questionnaire Survey. (DOCX 46 kb)
Data Availability Statement
Data are available on request.