Abstract
We examined the effects of homecoming support on current mental health among 1730 deployed veterans from Vietnam, Iraq/Afghanistan, Persian Gulf, and other conflicts. The prevalence of current posttraumatic stress disorder (PTSD) was 5.4%, current depression was 8.3%, and 5.4% had suicidal thoughts in the past month. Overall, 26% of veterans had low homecoming support, which was more prevalent among Vietnam veterans (44.3%, p < 0.001). In multivariable logistic regressions, controlling for demographics, combat exposure, number of deployments, trauma history, and operational theater, low postdeployment support was associated with PTSD (odds ratio, 2.13; p = 0.032) and suicidality (odds ratio, 1.91; p < 0.030), but not depression. For suicidality, an interaction was detected for homecoming by theater status, whereby Iraq/Afghanistan veterans with lower homecoming support had a higher probability of suicidal thoughts (p = 0.002). Thus, years after deployment, lower homecoming support was associated with current PTSD and suicidality, regardless of theater and warzone exposures. For suicidality, lower support had a greater impact on Iraq/Afghanistan veterans.
Key Words: Veterans, health status, psychosocial factors, PTSD, suicidality
“How was your homecoming experience?” is a common question asked by mental health practitioners caring for military veterans. In the current study, we examined the impact of homecoming support on mental health outcomes among community-based veterans, including Vietnam, Iraq/Afghanistan, Persian Gulf, and other recent veterans. Consistent with previous research (Adams et al., 2017; Boscarino et al. 2015), the objective of this study is to assess the impact of predeployment and postdeployment psychosocial factors on the mental health status of US veterans. Research related to service in Iraq and Afghanistan suggested that significant numbers of these service members developed mental health disorders after their deployments (Booth-Kewley et al., 2010; Hoge et al., 2004; Jacobson et al., 2008; Kok et al., 2012; Polusny et al., 2017). Earlier studies suggested significant rates of posttraumatic stress disorder (PTSD) and other health problems among former service members after the Vietnam War (Boscarino, 2006, 2007; Kulka et al., 1990b). In addition, a recent follow-up study among these veterans suggested that negative homecoming experiences predicted warzone-related PTSD symptoms up to 40 years postdeployment (Steenkamp et al., 2017).
Given previous research (Boscarino, 1995), our hypothesis was that the prevalence of mental disorders among veterans would be higher among those who experienced negative homecoming experiences, independent of warzone theater, and other variables, such as combat exposure and demographic factors. In the past, knowledge of the mental health impact of the homecoming experience on veterans' mental health had been limited (Frey-Wouters and Laufer, 1986; Lifton, 1973; Polner, 1971). However, more recent studies have confirmed that the homecoming experiences of Vietnam (Fontana and Rosenheck, 1994; Johnson et al., 1997; Koenen et al., 2003; Steenkamp et al., 2017; Schnurr et al., 2004), Croatian (Vuksic-Mihaljevic et al., 2000), and Israeli veterans (Neria et al., 1998), as well as the homecoming experiences of peace-keepers (Bolton et al., 2002), has had an impact on the mental health of veterans. A limitation of past research has been that these studies have primarily assessed the support of family and friends, which may be confounded. In addition, past studies typically assessed a single generation of veterans exposed to the same conflict. As discussed later, our assessment was primarily focused on postdeployment community support, which has been a significant issue among Vietnam veterans since the 1960s (Bowden, 2017). Furthermore, we assessed this homecoming impact among several generations of veterans from different conflicts, which to our knowledge, has not been previously investigated in the same study. As noted later, analysis of different cohorts of veterans has challenges, because these groups have unique differences but also overlap because some veterans have served in multiple conflicts. Nevertheless, understanding of deployment-related risk factors among former service members is important for prevention and treatment of mental health disorders among returning veterans (Adler and Castro, 2013).
METHODS
Sample
The population for the current study included a sample of community-based US military veterans recruited for a study of the health effects of military service (Adams et al., 2017; Boscarino et al., 2015; Lent et al., 2017). All veterans in the study were outpatients in the Geisinger Clinic, the largest multihospital system located in central and northeastern Pennsylvania (Boscarino et al., 2016). In 2007, Geisinger initiated a veterans' registry for patients receiving outpatient care and adult patients since then have been asked to complete a military history questionnaire. To date, over 30,000 patients have provided this information, and this database was used to select a random sample of veterans for the current study. Geisinger is an integrated health services organization with an advanced electronic health record system (www.geisinger.org). This system serves more than 3 million residents throughout 45 counties in central, south-central, and northeast Pennsylvania and encompasses a 25,000 square mile service area. The Geisinger system includes 30,000 employees, 1600 employed physicians, 9 hospital campuses, and a 551,000-member health plan (Boscarino et al., 2016).
With patient consent, trained and supervised interviewers administered structured health interviews by telephone from February 2016 through February 2017. All veterans recruited had one or more warzone deployment. Veteran status and deployment history were confirmed based on military records provided by the veteran. Among the ~10,000 veterans initially selected for the surveys, all were younger than 76 years and served in Vietnam or in another post-Vietnam conflict (i.e., Iraq/Afghanistan, Global War on Terrorism [GWOT], Persian Gulf, or other recent conflict). After 10 telephone calls, we were able to complete 1730 interviews, for an estimated survey cooperation rate of 55% among those eligible for the survey (American Association for Public Opinion Research, 2008; Groves et al., 2009). Deceased patients, nursing home patients, institutionalized patients, those who did not serve in Vietnam, Iraq, Afghanistan, GWOT, Persian Gulf, or other recent post-Vietnam conflict were excluded from this study, as were those who were cognitively impaired, and those unavailable during the survey period.
Measures
To assess PTSD in our study, we used a questionnaire based on the Diagnostic and Statistical Manual of Mental Disorder, Fifth Edition (DSM-5), the PTSD Checklist (Blevins et al., 2015; Bovin et al., 2016). To receive a diagnosis of PTSD, veterans had to meet the DSM-5 diagnostic criteria A through G within the past 12 months (American Psychiatric Association, 2013). This PTSD scale has been used in several recent studies (Cox et al., 2014; Hoge et al., 2014, Wortmann et al., 2016), although there has been debate related to the changes in DSM-5 (Hoge et al., 2016). Nearly 80% of the veterans in the current study reported that the most significant lifetime stressor they experienced was warzone exposure. In addition to PTSD, the survey collected data related to the veteran's military history, concussion exposure, combat exposure, and demographic background. Concussion history was assessed based on reported concussions experienced during military service (e.g., ever dazed, confused, saw stars, or knocked out), a concussion scale that has been widely used and validated in previous research (Boscarino et al., 2015; Schwab et al., 2006).
Depression was assessed using a major depressive disorder scale based on the DSM-4 diagnostic criteria (First and Tasman, 2004; First et al., 1997; Spitzer et al., 1992), which has been used extensively in previous trauma studies (Acierno et al., 2000; Boscarino et al., 2004a, 2014, 2015; Kilpatrick et al., 2003). This measure has been used in telephone-based surveys of World Trade Center Disaster survivors (Boscarino et al., 2006; Galea et al., 2002). Data related to the validity of this depression scale were previously reported and suggest that this scale can be used to diagnose depression in population studies (Boscarino et al., 2004b; Kilpatrick et al., 2003). To meet criteria in the study, subjects had to meet the full DSM-4 criteria for major depression within the past 12 months.
Other postdeployment health outcomes assessed included a measure of suicidality from the Brief Symptom Inventory-18 (BSI-18) scale (Derogatis, 2001). This symptom was assessed for the past 30 days (“please tell me how much thoughts of ending your life distressed or bothered you in the past 30 days”), which was consistent with the current PTSD and depression timeframes used (i.e., past 12 months). The BSI-18 scale is a widely used psychological symptom scale, originally developed from the Hopkins Symptom Inventory, which has a long history in psychiatric research (Adams et al., 2006a; Derogatis and Cleary, 1977; Derogatis et al., 1973, 1976; Franke et al., 2011; Prinz et al., 2013).
Potential mental health risk and protective factors also assessed in the study included demographic factors (e.g., age, sex, race, marital status, and education), multiple warzone deployments, and combat exposure, which were all derived from the survey instruments and used in previous research (Adams et al., 2017; Boscarino et al., 2015). Warzone exposures included the Vietnam War, Persian Gulf War, Afghanistan/Iraq War, and “other” recent warzone deployments, as currently defined by the VA, which encompasses four veteran cohorts of interest: Vietnam, Persian Gulf, Iraq/Afghanistan, and other post-Vietnam deployed veterans. Global War on Terrorism (GWOT) veterans (n = 70) were combined with Iraq/Afghanistan veterans, because these deployments were during the same timeframe and were in supporting theaters of operations. Combat exposure was based on the Combat Experience Scale, which is a widely used measure of combat exposure first used in the Vietnam Legacy Study (Frey-Wouters and Laufer, 1986; Laufer et al., 1984). Versions of this scale have been used in key studies since the Vietnam War, including the Vietnam Experience Study, the National Vietnam Veterans Readjustment Study, the Vietnam Twin Registry, among others (Centers for Disease Control, 1988; Boscarino, 1996; Boscarino et al., 2010; Kulka et al., 1990a; McLeod et al., 2001). The Combat Experience Scale used in the current study was updated for recent conflicts (Adams et al., 2017; Boscarino et al., 2015; Lent et al., 2017). Based on previous research, scale measures for combat exposure were divided into cut-points described elsewhere (Adams et al., 2017; Boscarino et al., 2015).
Our study also assessed the occurrence of 12 lifetime traumatic events (e.g., forced sexual contact, domestic abuse, a serious accident, served in a warzone, experienced a major disaster) (Freedy et al., 1993). As we had no a priori method to judge the severity of these events, based on previous research, we collapsed these exposures into three categories: less than three traumatic events, three to five events, and six or more events. A total of 21% of respondents experienced six or more lifetime traumatic events in the current study. This traumatic event scale was developed from other trauma studies, was used in previous research, and had good reported reliability and validity (Adams and Boscarino, 2006; Boscarino et al., 2004a, 2012, 2013, 201, 2015; Galea et al., 2002; Freedy et al., 1993; Resnick et al., 1993).
Homecoming support was assessed by four Likert survey items (rated “strongly agree” to “strongly disagree”) from the postdeployment section of the Deployment Risk & Resilience Inventory (DRRI), which asked veterans to report their homecoming experiences (e.g., “when I retuned, people made me feel proud to have served,” “the reception I received when I returned from deployment made me feel appreciated,” “the American people made me feel at home,” etc.) (Vogt et al., 2008). The Cronbach's alpha for this DRRI subscale in the current study was 0.86. Those scoring in the lowest quartile were classified as having low homecoming support. Total scores on this scale ranged from 0 to 16 (mean, 9.36; SD, 5.20).
Our study also included measures of current life stressors, current social support, deployment unit support, and VA service use, all of which were based on survey questions (Adams et al., 2017; Boscarino et al., 2015). Current life stressors included a count of eight experiences that could have happened to the respondent in the past 12 months (e.g., death of spouse or close family member, being injured, problems at work, getting married, having financial problems, etc.). Experiencing two or more of these events in the past 12 months (~22% of the survey sample) was classified as high exposure to stressful life events. As with the traumatic event scale, this life stress scale was developed from other trauma studies, used in previous research, and had good reported reliability and validity (Adams and Boscarino, 2006; Boscarino et al., 2004a, 2012, 2013, 2014, 2015; Galea et al., 2002; Freedy et al., 1993; Resnick et al., 1993). Unit support was based on survey items from the DRRI, which asked the veterans to report on their unit experiences during deployment (e.g., “felt a sense of camaraderie between myself and others in my unit”) (Vogt et al., 2008). Cronbach's alpha for this scale in the current study was 0.78. Those scoring in the lowest quartile were classified as having low unit support during deployment. The social support scale used was a version included in the Medical Outcomes Study (Sherbourne and Stewart, 1991) that was used in past trauma research (Boscarino et al., 2004a, 2014; Galea et al., 2002; Freedy et al., 1993). Items for this scale were based on a 4-point Likert scale rated “none of the time” to “all the time” (e.g., someone available to help you if you were confined to bed?) (Boscarino et al., 2014). This scale has been used in previous trauma studies and is considered a reliable and valid measure of current social support (Boscarino et al., 2004b; Galea et al., 2002). This scale was used as a categorical measure in the current study, with low social support defined as the lowest quintile (Boscarino et al., 2014). Cronbach's alpha for this scale in the current study was 0.84. Finally, for descriptive purposes we included several questions related to VA service use and VA disability status used in previous research (Boscarino et al., 2015).
It is noted that our study was guided, in part, by a psychosocial stress model, which is focused on the availability of psychosocial resources and the impact of environmental factors in the onset and course of mental disorders (Adams and Boscarino, 2011; Adams et al., 2006a, 2006b; Rosen et al., 2012; Yamashita, 2012). This model guided our instrument selection and data analyses (Adams et al., 2017).
Data Analyses
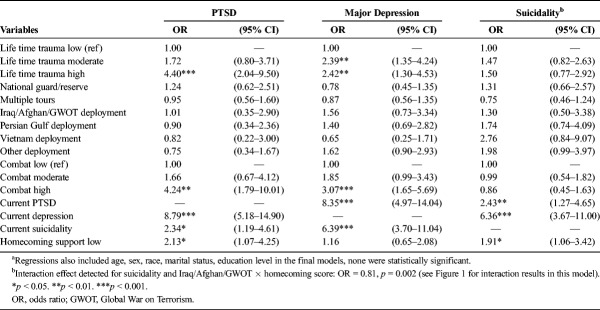
Statistical analyses included descriptive statistics depicting the study population and testing the association between mental health status and the postdeployment homecoming experience. For descriptive purposes, we present the characteristics of the study population and show these results in Tables 1 and 2. Because there were differences expected between the Vietnam and post-Vietnam cohorts, we present these results in Table 3 and discuss these differences. To minimize bias, we also describe these results using pairwise comparisons of column proportions, with a Bonferroni correction for multiple comparisons (Statistical Package for the Social Sciences, 2012; Dawson and Trapp, 2004). For multivariate analyses, we used logistic regression, whereby key risk/protective factors (e.g., combat exposure, cohort status, lifetime trauma exposure, number of deployments, other mental disorders, etc.) were used to estimate the likelihoods (i.e., odds ratios) for PTSD, depression, and suicidality, respectively, controlling for age, sex, marital status, level of education, and other factors that might affect these associations by including these variables in the regression analyses (Table 4).
TABLE 1.
Demographic Profile of Veterans in Veterans' Health Study (N = 1730)
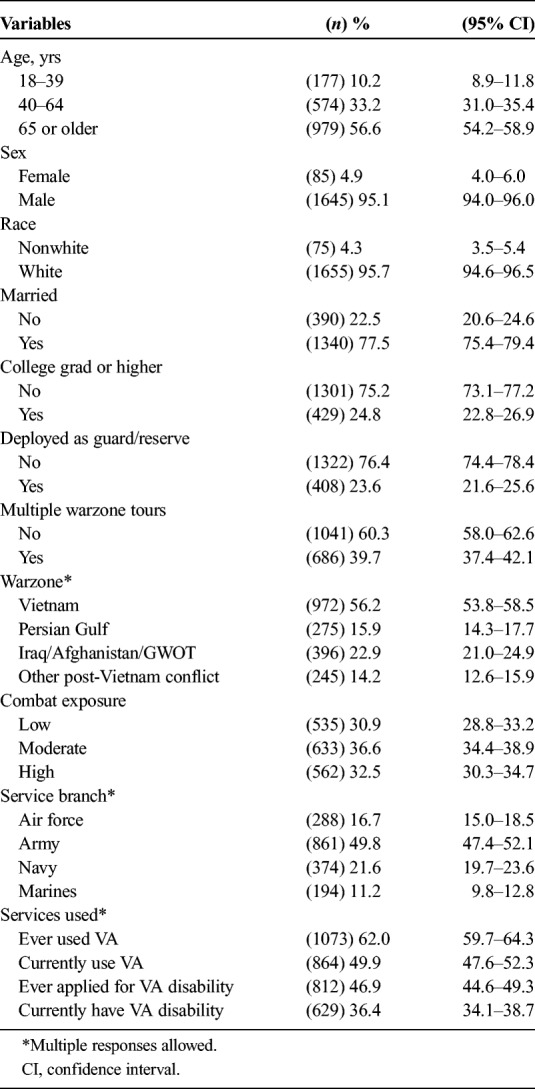
TABLE 2.
Psychosocial Profile of Veterans in Veterans' Health Study (N = 1730)
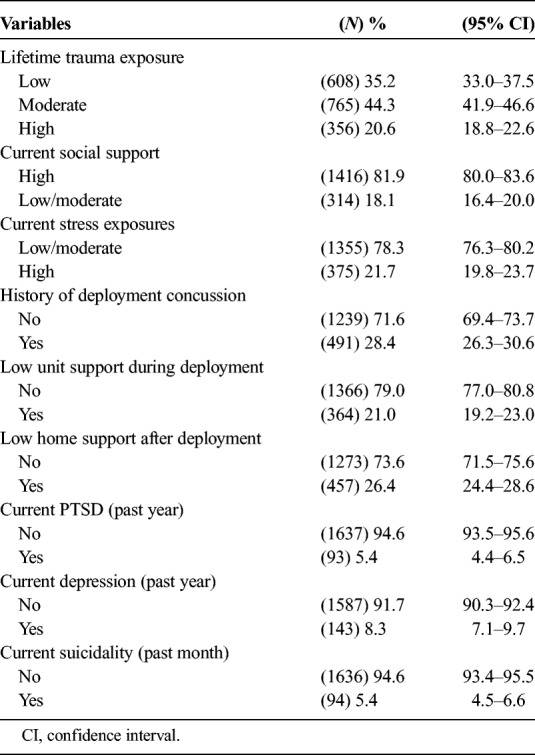
TABLE 3.
Veteran Cohort Status by Postdeployment Risk Factors and Health Outcomes (N = 1722)*
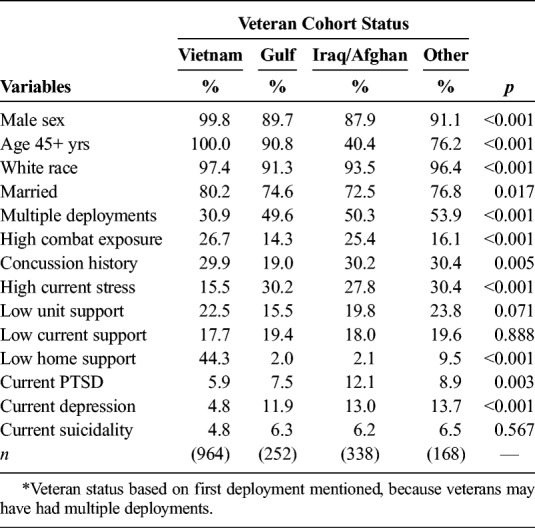
TABLE 4.
Multivariable Logistic Regressions Predicting Current PTSD, Depression, and Suicidality Among Veterans (N = 1730)a
All the variables shown in the final multivariate models are included in the analyses presented, otherwise footnoted in Table 4. Because previous reports suggest that the postdeployment homecoming experiences might vary by theater status (Bowden, 2017; Frey-Wouters and Laufer, 1986; Polner, 1971), in our final analyses, we assess interaction effects for homecoming by warzone theater as a final analysis step. We did this by using cross-product terms (i.e., theater × homecoming score) entered in the final regression step that also included the main effects (Harrell, 2001; Hosmer and Lemeshow, 2000). For this interaction assessment, homecoming used as a continuous scale (range, 0–16). Finally, in the discussion section of the article, we discuss study results as they relate to similar studies. Analyses were conducted using Stata, version 13.1 software (Stata Corporation, 2013).
Review Board Approval
This study was approved by the Institutional Review Boards of the Geisinger Clinic and the Department of Defense. All patients provided their informed consent to participate in the study and were offered small monetary incentives for participation.
RESULTS
Using the medical and demographic data included in the patient's electronic medical records, we examined the differences between survey respondents and nonrespondents in terms of sex, race, age, marital status, having a primary care physician, employment status, smoking status, and the prevalence of major health conditions (Boscarino et al., 2015). The only significant differences found were that survey respondents tended to be younger and married (p < 0.05).
Most veterans studied were older than 65 years (56.6%), male (95.1%), white (95.7%), and were currently married (77.5%). In addition, 23.6% were deployed guard/reserve service members, 56.2% were Vietnam veterans, and 49.8% were US Army veterans (Table 1). Furthermore, 28.4% reported experiencing a concussion during deployment, 5.4% met the criteria for current PTSD, 8.3% met criteria for current major depression, and 5.4% had suicidal thoughts in the past 30 days (Table 2). Examination of veteran cohort status by deployment history, risk/protective factors, and deployment outcomes suggests that, compared with other veterans, Vietnam veterans appeared to be older, more often male, more often white, more often married, and less often served on multiple deployments (Table 3). Conversely, Vietnam veterans appeared less likely to have high current stress, current PTSD, and current depression. However, Vietnam veterans were more likely to report low homecoming support postdeployment, compared with other veterans (44.3%, p < 0.001) (Table 3). Using pairwise comparisons of column proportions for these different veteran cohorts, with a Bonferroni correction for multiple comparisons, generally confirmed these associations with two noteworthy exceptions. Gulf War veterans had significantly lower combat exposure and significantly lower rates of concussion.
In multivariable analyses, significant predictors of current PTSD were high lifetime trauma exposure (p < 0.001), high combat exposure (p < 0.01), current depression (p < 0.001), current suicidality (p < 0.05), and low homecoming support (p < 0.05) (Table 4). The significant predictors of current depression included moderate (p < 0.01) and high (p < 0.01) lifetime trauma exposure, high combat exposure (p < 0.001), current PTSD (p < 0.001), and recent suicidality (p < 0.001). However, low homecoming support was not significant for this outcome. In addition, for veterans, significant predictors of recent suicidality were current PTSD (p < 0.01), current depression (p < 0.001), and low homecoming support (p < 0.05) (Table 4). Of note, guard/reserve status, serving on multiple tours, and theater status were not associated with any of these three study outcomes, nor were the demographic factors we assessed. Because there was a significant difference found for current stressful life events between the veteran groups assessed (Table 3), we added this measure to the regression models for PTSD and suicidality, but this did not change these results. We also assessed interactions effects for theater status by homecoming support score and these were nonsignificant, except for current suicidality among the Iraq/Afghanistan veterans. In this case, a significant interaction was detected, whereby Iraq/Afghanistan veterans with low homecoming support scores were more likely to experience suicidality than other the veterans (p < 0.002), as shown in the effects plot presented in Figure 1.
FIGURE 1.
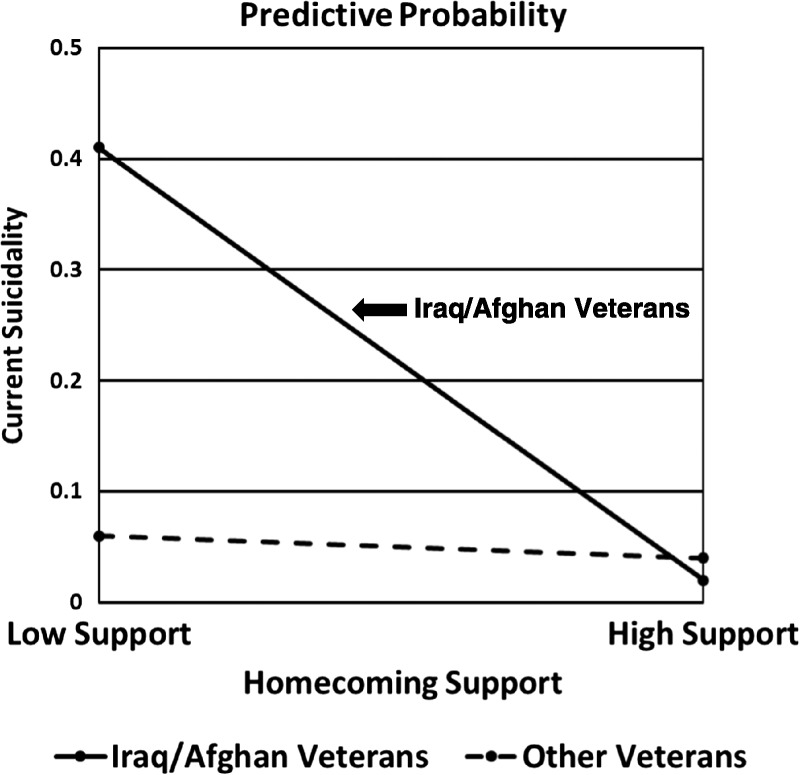
Current suicidality by homecoming support score and veteran status (N = 1730).
DISCUSSION
Given previous research (Boscarino, 1995, 2007; Steenkamp et al., 2017), our premise was that the prevalence of mental disorders among veterans would be higher among those who experienced negative homecoming experiences, regardless of the theater of deployment. Until recently, the impact of the homecoming experience on veterans' mental health status has been mostly anecdotal (Polner, 1971; Frey-Wouters and Laufer, 1986). However, investigators for the National Vietnam Veterans Longitudinal Study (NVVLS) reported that postdeployment risk factors, including the homecoming experience, predicted warzone-related PTSD up to 40 years postdeployment (Steenkamp et al., 2017). There have been previous studies that have examined the impact of homecoming on mental health outcomes among veterans (Fontana and Rosenheck, 1994; Johnson et al., 1997; Koenen et al., 2003; Neria et al., 1998; Vuksic-Mihaljevic et al., 2000), but these mostly assessed the support of family and friends, which may be confounded.
As shown, low postdeployment community homecoming support was associated with PTSD and suicidality, but not depression. Thus, our PTSD finding is consistent with the NVVLS findings (Steenkamp et al., 2017). Recently, there has been an increased focus on psychosocial factors occurring in the predeployment, deployment, and postdeployment periods for service members to minimize the adverse impact of warfighting among veterans (Adler and Castro, 2013; Vogt et al., 2013). We note that similar research efforts emerged after the terrorist attacks in New York City on September 11, 2001, among trauma-exposed civilian populations (Adams and Boscarino, 2006; Hobfoll et al., 2009; Norris et al., 2009; Pietrzak et al., 2014). The detection of an interaction effect for homecoming support score by Iraq/Afghanistan veteran status is an intriguing finding, given that Vietnam veterans were known to have received lower homecoming support postdeployment, compared with more recent veterans (Bowden, 2017), as was shown in Table 3. Nevertheless, Iraq/Afghanistan veterans with lower homecoming support scores were more likely to experience recent suicidal thoughts (Fig. 1).
The current study has several strengths. First, we recruited a large sample of community-based veterans. Second, we used validated scales and measures from previous research (Adams and Boscarino, 2006; Boscarino et al., 2015). Third, we included veterans from Vietnam through to current conflicts in Iraq and Afghanistan, something not typically done in the same study. Fourth, we examined several postdeployment outcomes, including current PTSD, depression, and current suicidality. Fifth, our homecoming measure was focused on community-level support not just family-level support, which may be confounded. Sixth, our multivariable analyses included all the mental health outcomes studied in the final models, considered a conservative approach, because these outcomes tend to be interrelated (Boscarino et al., 2004a). Nevertheless, the results for PTSD and suicidality remained statistically significant (Table 4).
However, our study has several limitations, including that the study was based on a cross-sectional survey. Because of this limitation, it is possible that the associations found in our study could be reversed (Hulley et al., 2013), such that those with postdeployment mental health issues may have a more negative recall of community homecoming support. In addition, although our study was based on a large survey, the study was conducted among mostly white patients in a multihospital system located in central and northeastern Pennsylvania. Furthermore, we found some survey response differences, whereby survey respondents tended to be younger compared with nonrespondents (p < 0.05). Thus, it may not be possible to fully generalize these findings to other geographic areas and study populations. As noted elsewhere, however, there are few stable national samples of veterans available, because this population is dynamic, given different deployments, ongoing conflicts, and the aging of the veteran population (Boscarino, 2007; Hynes et al., 2007; Shen et al., 2003). In addition, most veterans do not use the VA system for health care (Boscarino et al., 2015), which complicates identifying representative samples of veterans for clinical research. Nevertheless, although there were significant differences found between the veteran cohorts in bivariate analyses (Table 3), there were no differences detected in the final multivariable analyses (Table 4).
CONCLUSIONS
Despite these limitations, our findings are consistent with a recent 40-year follow-up study conducted by NVVLS investigators (Steenkamp et al., 2017). Those researchers reported that the service members' homecoming experiences had an adverse impact on mental health decades after deployment. To our knowledge, this postdeployment risk factor has not been previously studied among a multigenerational sample of community-based veterans. We suggest that services to returning veterans that result in a positive and sustained homecoming experiences are important. Further research is advised to both confirm our findings and improve “welcome home” programs that enhance mental health among retuning veterans and their families. Although our sample is limited, it is interesting that Iraq/Afghanistan veterans with low homecoming support scores were more likely to experience recent suicidality (Fig. 1). This was unexpected and warrants further investigation. Although some have advocated a broad occupational health model for service members (Adler and Castro, 2013), it has been suggested that there are few specific behavioral health models to improve the “homecoming” experience for veterans (Bolton et al., 2002; Boscarino, 2007). Although recent research progress has been made (Steenkamp et al., 2017), the reasons why veterans with low homecoming support are at greater risk for both current PTSD and recent suicidality are unclear. Given ongoing conflicts, better understanding of the “active ingredients” of the homecoming experience need to be further delineated, to prevent the onset of mental illness among the next generation of returning service members.
ACKNOWLEDGMENT
The study team acknowledges the efforts of the 1730 veterans who took part in this study. The study Principal Investigator dedicates this research to his twin brother, a Vietnam veteran who never had a homecoming and never found peace, but motivated him to conduct trauma studies so others may avoid his outcome (https://vimeo.com/235786674/e758e9b34c).
DISCLOSURE
The authors declare no conflicts of interests related to this research.
Footnotes
Funding for this research was provided by Geisinger Auxiliary Fund, the Kline & Ditty Health Fund, National Institute of Mental Health (grant no. R21-MH-086317), Wounded Warrior Project, and the Department of Defense (contract no. W81XWH-15-1-0506) to J.A. Boscarino.
A version of this article was presented at: Annual Meeting of The International Society of Traumatic Stress Study, Chicago, IL, November 9–11, 2017.
REFERENCES
- Acierno R, Kilpatrick DG, Resnick H, Saunders B, De Arellano M, Best C. (2000) Assault, PTSD, family substance use, and depression as risk factors for cigarette use in youth: Findings from the National Survey of Adolescents. J Trauma Stress. 13:381–396. [DOI] [PubMed] [Google Scholar]
- Adams RE, Boscarino JA. (2006) Predictors of PTSD and delayed PTSD after disaster: the impact of exposure and psychosocial resources. J Nerv Ment Dis. 194:485–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Boscarino JA. (2011) A structural equation model of perievent panic and posttraumatic stress disorder after a community disaster. J Trauma Stress. 24:61–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Boscarino JA, Galea S. (2006a) Alcohol use, mental health status and psychological well-being 2 years after the World Trade Center attacks in New York City. Am J Drug Alcohol Abuse. 32:203–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Boscarino JA, Galea S. (2006b) Social and psychological resources and health outcomes after the World Trade Center disaster. Soc Sci Med. 62:176–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Urosevich TG, Hoffman SN, Kirchner HL, Hyacinthe JC, Figley CR, Boscarino JJ, Boscarino JA. (2017) Social support, help-seeking, and mental health outcomes among veterans in non-VA facilities: results from the veterans' health study. Mil Behav Health. 5:393–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adler AB, Castro CA. (2013) An occupational mental health model for the military. Military Behavioral Health. 1:41–51. [Google Scholar]
- American Association for Public Opinion Research (2008) Standard definitions: Final dispositions of case codes and outcome rates for surveys. Lenexa, Kansas: American Association for Public Opinion Research. [Google Scholar]
- American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (5th ed). Arlington, DC: American Psychiatric Association. [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. (2015) The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J Trauma Stress. 28:489–498. [DOI] [PubMed] [Google Scholar]
- Bolton EE, Litz BT, Glenn DM, Orsillo S, Roemer L. (2002) The impact of homecoming reception on the adaptation of peasekeepers following deployment. Military Psychology. 14(3):241–251. [Google Scholar]
- Booth-Kewley S, Larson GE, Highfill-McRoy RM, Garland CF, Gaskin TA. (2010) Correlates of posttraumatic stress disorder symptoms in Marines back from war. J Trauma Stress. 23:69–77. [DOI] [PubMed] [Google Scholar]
- Boscarino JA. (1995) Post-traumatic stress and associated disorders among Vietnam veterans: the significance of combat exposure and social support. J Trauma Stress. 8:317–336. [DOI] [PubMed] [Google Scholar]
- Boscarino JA. (1996) Posttraumatic stress disorder, exposure to combat, and lower plasma cortisol among Vietnam veterans: Findings and clinical implications. J Consult Clin Psychol. 64:191–201. [DOI] [PubMed] [Google Scholar]
- Boscarino JA. (2006) Posttraumatic stress disorder and mortality among U.S. Army veterans 30 years after military service. Ann Epidemiol. 16:248–256. [DOI] [PubMed] [Google Scholar]
- Boscarino JA. (2007) Vietnam veterans, postwar experiences and health outcomes. In Fink G. (Ed), Encyclopedia of stress (2nd ed, Vol 3, pp 830–838). New York: Academic Press. [Google Scholar]
- Boscarino JA, Adams RE, Figley CR. (2004a) Mental health service use 1-year after the World Trade Center disaster: Implications for mental health care. Gen Hosp Psychiatry. 26:346–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE, Figley CR. (2006) Worker productivity and outpatient service use after the September 11th attacks: Results from the New York City terrorism outcome study. Am J Ind Med. 49:670–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Forsberg CW, Goldberg J. (2010) A twin study of the association between PTSD symptoms and rheumatoid arthritis. Psychosom Med. 72:481–486. [DOI] [PubMed] [Google Scholar]
- Boscarino JA, Galea S, Adams RE, Ahern J, Resnick H, Vlahov D. (2004b) Mental health service and medication use in New York City after the September 11, 2001, terrorist attack. Psychiatr Serv. 55:274–283. [DOI] [PubMed] [Google Scholar]
- Boscarino JA, Hoffman SN, Adams RE, Figley CR, Solhkhah R. (2014) Mental health outcomes among vulnerable residents after Hurricane Sandy: Implications for disaster research and planning. Am J Disaster Med. 9:107–120. [DOI] [PubMed] [Google Scholar]
- Boscarino JA, Hoffman SN, Pitcavage JM, Urosevich TG. (2015) Mental health disorders and treatment seeking among veterans in non-VA facilities: results and implications from the veterans' health study. Mil Behav Health. 3:244–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Kirchner HL, Hoffman SN, Erlich PM. (2013) Predicting PTSD using the New York Risk Score with genotype data: potential clinical and research opportunities. Neuropsychiatr Dis Treat. 9:517–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Kirchner HL, Hoffman SN, Sartorius J, Adams RE, Figley CR. (2012) The New York PTSD risk score for assessment of psychological trauma: Male and female versions. Psychiatry Res. 200:827–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Kirchner HL, Pitcavage JM, Nadipelli VR, Ronquest NA, Fitzpatrick MH, Han JJ. (2016) Factors associated with opioid overdose: A 10-year retrospective study of patients in a large integrated health care system. Subst Abuse Rehabil. 7:131–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, Keane TM. (2016) Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychol Assess. 28:1379–91. [DOI] [PubMed] [Google Scholar]
- Bowden M. (2017) Hue 1968: a turning point of the American war in Vietnam. New York: Atlantic Monthly Press. [Google Scholar]
- Centers for Disease Control (1988) Health status of Vietnam veterans. I. Psychosocial characteristics. The Centers for Disease Control Vietnam Experience Study. JAMA. 259:2701–2707. [PubMed] [Google Scholar]
- Cox KS, Resnick HS, Kilpatrick DG. (2014) Prevalence and correlates of posttrauma distorted beliefs: Evaluating DSM-5 PTSD expanded cognitive symptoms in a national sample. J Trauma Stress. 27:299–306. [DOI] [PubMed] [Google Scholar]
- Dawson B, Trapp RG. (2004) Basic & clinical statistics (4th ed). New York: Lang Medical Books. [Google Scholar]
- Derogatis LR. (2001) Brief Symptom Inventory 18 (BSI-18) Manual. Bloomington, MN: Pearson. [Google Scholar]
- Derogatis LR, Cleary PA. (1977) Factorial invariance across gender for the primary symptom dimensions of the SCL-90. Br J Soc Clin Psychol. 16:347–356. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Lipman RS, Covi L. (1973) SCL-90: An outpatient psychiatric rating scale—preliminary report. Psychopharmacol Bull. 9:13–28. [PubMed] [Google Scholar]
- Derogatis LR, Rickels K, Rock AF. (1976) The SCL-90 and the MMPI: A step in the validation of a new self-report scale. Br J Psychiatry. 128:280–289. [DOI] [PubMed] [Google Scholar]
- First MB, Tasman A. (Eds) (2004) DSM-IV-TR mental disorders: diagnosis, etiology, and treatment. Hoboken, NJ: John Wiley & Sons, Inc. [Google Scholar]
- First MD, Spitzer RL, Gibbon M, Williams JBW. (1997) Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I)—Clinician Version. Washington: American Psychiatric Association. [Google Scholar]
- Fontana A, Rosenheck R. (1994) Posttraumatic stress disorder among Vietnam Theater Veterans. A causal model of etiology in a community sample. J Nerv Ment Dis. 182:677–684. [DOI] [PubMed] [Google Scholar]
- Franke GH, Ankerhold A, Haase M, Jager S, Togel C, Ulrich C, Frommer J. (2011) The usefulness of the Brief Symptom Inventory 18 (BSI-18) in psychotherapeutic patients. Psychother Psychosom Med Psychol. 61:82–86. [DOI] [PubMed] [Google Scholar]
- Freedy JR, Kilpatrick DG, Resnick HS. (1993) Natural disasters and mental health: Theory, assessment, and intervention. J Soc Behav Personality. 8:49–103. [Google Scholar]
- Frey-Wouters E, Laufer RS. (1986) Legacy of a war: The American soldier in Vietnam. Armonk, NY: Sharpe Pub, Inc. [Google Scholar]
- Galea S, Ahern J, Resnick H, Kilpatrick D, Bucuvalas M, Gold J, Vlahov D. (2002) Psychological sequelae of the September 11 terrorist attacks in New York City. N Engl J Med. 346:982–987. [DOI] [PubMed] [Google Scholar]
- Groves RM, Fowler FJ, Couper MP, Lepkowski JM, Singer E, Tourangeau R. (2009) Survey methodology (2nd ed). New York: Wiley. [Google Scholar]
- Harrell FE. (2001) Regression modeling strategies: With applications to linear models, logistic regression, and survival analysis. New York: Springer. [Google Scholar]
- Hobfoll SE, Palmieri PA, Johnson RJ, Canetti-Nisim D, Hall BJ, Galea S. (2009) Trajectories of resilience, resistance, and distress during ongoing terrorism: The case of Jews and Arabs in Israel. J Consult Clin Psychol. 77:138–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. (2004) Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 351:13–22. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Riviere LA, Wilk JE, Herrell RK, Weathers FW. (2014) The prevalence of post-traumatic stress disorder (PTSD) in US combat soldiers: a head-to-head comparison of DSM-5 versus DSM-IV-TR symptom criteria with the PTSD checklist. Lancet Psychiatry. 1:269–77. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Yehuda R, Castro CA, McFarlane AC, Vermetten E, Jetly R, Koenen KC, Greenberg N, Shalev AY, Rauch SA, Marmar CR, Rothbaum BO. (2016) Unintended consequences of changing the definition of posttraumatic stress disorder in DSM-5: Critique and call for action. JAMA Psychiatry. 73:750–752. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. (2000) Applied logistic regression. New York: Wiley. [Google Scholar]
- Hulley SB, Cummings SR, Browner WS, Grady DG, Newman TB. (2013) Designing clinical research. Philadelphia; Baltimore; New York; London; Buenos Aires; Hong Kong; Sydney; Tokyo: Wolters Kluwer Health/Lippincott Williams & Wilkins. [Google Scholar]
- Hynes DM, Koelling K, Stroupe K, Arnold N, Mallin K, Sohn MW, Weaver FM, Manheim L, Kok L. (2007) Veterans' access to and use of Medicare and Veterans Affairs health care. Med Care. 45:214–223. [DOI] [PubMed] [Google Scholar]
- Jacobson IG, Ryan MA, Hooper TI, Smith TC, Amoroso PJ, Boyko EJ, Gackstetter GD, Wells TS, Bell NS. (2008) Alcohol use and alcohol-related problems before and after military combat deployment. JAMA. 300:663–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson DR, Lubin H, Rosenheck R, Fontana A, Southwick S, Charney D. (1997) The impact of the homecoming reception on the development of posttraumatic stress disorder. The West Haven Homecoming Stress Scale (WHHSS). J Trauma Stress. 10:259–277. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. (2003) Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the National Survey of Adolescents. J Consult Clin Psychol. 71:692–700. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Stellman JM, Stellman SD, Sommer JF., Jr (2003) Risk factors for course of posttraumatic stress disorder among Vietnam veterans: A 14-year follow-up of American Legionnaires. J Consult Clin Psychol. 71:980–986. [DOI] [PubMed] [Google Scholar]
- Kok BC, Herrell RK, Thomas JL, Hoge CW. (2012) Posttraumatic stress disorder associated with combat service in Iraq or Afghanistan: Reconciling prevalence differences between studies. J Nerv Ment Dis. 200:444–450. [DOI] [PubMed] [Google Scholar]
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS. (1990a) The National Vietnam Veterans Readjustment Study: Tables of Findings and Technical Appendices. New York: Brunner/Mazel. [Google Scholar]
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS. (1990b) Trauma and the Vietnam War Generation: Report of findings from the National Vietnam Readjustment Study. New York: Brunner/Mazel. [Google Scholar]
- Laufer RS, Gallops MS, Frey-Wouters E. (1984) War stress and trauma: The Vietnam veteran experience. J Health Soc Behav. 25:65–85. [PubMed] [Google Scholar]
- Lent MR, Hoffman SN, Kirchner HL, Urosevich TG, Boscarino JJ, Boscarino JA. (2017) Attitudes about future genetic testing for posttraumatic stress disorder and addiction among community-based veterans. Front Psychiatry. 8:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lifton RJ. (1973) Home from the War: Vietnam Veterans—neither victims nor executioners. New York: Simon and Schuster. [Google Scholar]
- McLeod DS, Koenen KC, Meyer JM, Lyons MJ, Eisen S, True W, Goldberg J. (2001) Genetic and environmental influences on the relationship among combat exposure, posttraumatic stress disorder symptoms, and alcohol use. J Trauma Stress. 14:259–275. [DOI] [PubMed] [Google Scholar]
- Neria Y, Solomon Z, Dekel R. (1998) An eighteen-year follow-up study of Israeli prisoners of war and combat veterans. J Nerv Ment Dis. 186:174–182. [DOI] [PubMed] [Google Scholar]
- Norris FH, Tracy M, Galea S. (2009) Looking for resilience: understanding the longitudinal trajectories of responses to stress. Soc Sci Med. 68:2190–2198. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Feder A, Singh R, Schechter CB, Bromet EJ, Katz CL, Reissman DB, Ozbay F, Sharma V, Crane M, Harrison D, Herbert R, Levin SM, Luft BJ, Moline JM, Stellman JM, Udasin IG, Landrigan PJ, Southwick SM. (2014) Trajectories of PTSD risk and resilience in World Trade Center responders: An 8-year prospective cohort study. Psychol Med. 44:205–219. [DOI] [PubMed] [Google Scholar]
- Polner M. (1971) No victory parades: The return of the Vietnam Veteran. New York: Holt, Rinehart and Winston. [Google Scholar]
- Polusny MA, Erbes CR, Kramer MD, Thuras P, DeGarmo D, Koffel E, Litz B, Arbisi PA. (2017) Resilience and posttraumatic stress disorder symptoms in national guard soldiers deployed to Iraq: A prospective study of latent class trajectories and their predictors. J Trauma Stress. 30:351–361. [DOI] [PubMed] [Google Scholar]
- Prinz U, Nutzinger DO, Schulz H, Petermann F, Braukhaus C, Andreas S. (2013) Comparative psychometric analyses of the SCL-90-R and its short versions in patients with affective disorders. BMC Psychiatry. 13: 104,244X-13-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. (1993) Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol. 61:984–991. [DOI] [PubMed] [Google Scholar]
- Rosen RC, Marx BP, Maserejian NN, Holowka DW, Gates MA, Sleeper LA, Vasterling JJ, Kang HK, Keane TM. (2012) Project VALOR: design and methods of a longitudinal registry of post-traumatic stress disorder (PTSD) in combat-exposed veterans in the Afghanistan and Iraqi military theaters of operations. Int J Methods Psychiatr Res. 21:5–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnurr PP, Lunney CA, Sengupta A. (2004) Risk factors for the development versus maintenance of posttraumatic stress disorder. J Trauma Stress. 17:85–95. [DOI] [PubMed] [Google Scholar]
- Schwab K, Baker G, Ivins B, Sluss-Tiller M, Lux W, Warden D. (2006) The Brief Traumatic Brain Injury Screen (BTBIS): investigating the validity of a self-report instrument for detecting traumatic brain injury (TBI) in troops returning from deployment in Afghanistan and Iraq. Neurology. 66(suppl 2): A235. [Google Scholar]
- Shen Y, Hendricks A, Zhang S, Kazis LE. (2003) VHA enrollees' health care coverage and use of care. Med Care Res Rev. 60:253–267. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Stewart AL. (1991) The MOS social support survey. Soc Sci Med. 32:705–714. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. (1992) The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Arch Gen Psychiatry. 49:624–629. [DOI] [PubMed] [Google Scholar]
- Statistical Package for the Social Sciences (2012) Version 20. Chicago: SPSS, Inc. [Google Scholar]
- Stata Corporation (2013) Stata, Version 13.1. College Station, TX.
- Steenkamp MM, Schlenger WE, Corry N, Henn-Haase C, Qian M, Li M, Horesh D, Karstoft KI, Williams C, Ho CL, Shalev A, Kulka R, Marmar C. (2017) Predictors of PTSD 40 years after combat: Findings from the National Vietnam Veterans longitudinal study. Depress Anxiety. 34:711–722. [DOI] [PubMed] [Google Scholar]
- Vogt D, Smith BN, King LA, King DW, Knight J, Vasterling JJ. (2013) Deployment risk and resilience inventory-2 (DRRI-2): an updated tool for assessing psychosocial risk and resilience factors among service members and veterans. J Trauma Stress. 26:710–717. [DOI] [PubMed] [Google Scholar]
- Vogt DS, Proctor SP, King DW, King LA, Vasterling JJ. (2008) Validation of scales from the Deployment Risk and Resilience Inventory in a sample of Operation Iraqi Freedom veterans. Assessment. 15:391–403. [DOI] [PubMed] [Google Scholar]
- Vuksic-Mihaljevic Z, Mandic N, Bensic M, Mihaljevic S. (2000) Posttraumatic stress disorder among Croatian veterans: A causal model. Psychiatry Clin Neurosci. 54:625–636. [DOI] [PubMed] [Google Scholar]
- Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, Foa EB, Young-McCaughan S, Yarvis JS, Hembree EA, Mintz J, Peterson AL, Litz BT. (2016) Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychol Assess. 28:1392–1403. [DOI] [PubMed] [Google Scholar]
- Yamashita J. (2012) A review of psychological assessments for disaster mental health studies. Psychol Trauma. 4:560–567. [Google Scholar]