Abstract
Background
Given high levels of traumatic stress for low-income, inner-city women, investigating the link between PTSD and pain is especially important.
Purpose
Using the Conservation of Resources (COR) Theory, we investigated direct and indirect relationships of PTSD symptoms, vulnerability factors (i.e., resource loss, depressive symptoms and social undermining), and resilience factors (i.e., optimism, engagement, and social support) to acute pain reports in a sample of low-income, inner-city women.
Method
Participants (N= 341; M Age = 28 years; 58.0% African American) were recruited from an inner-city Emergency Department (ED) following presentation with an acute pain-related complaint. Study data were gathered from psychosocial questionnaires completed at a baseline interview.
Results
Structural Equation Modeling examined direct and indirect relationships among PTSD symptoms, vulnerability factors and resilience factors on self-reported pain intensity and pain interference. PTSD symptoms were directly related to higher pain intensity and pain interference and indirectly related through positive associations with vulnerability factors (all p’s < .05). Pathways through resilience factors were not supported.
Conclusions
Results suggest that presence of PTSD symptoms is associated with elevated acute pain responses both indirectly via psychosocial vulnerability factors and directly, independent of the psychosocial factors assessed. Resilience factors did not play a significant role in determining acute pain responses. Consistent with COR theory, the negative effects of vulnerability factors outweighed the positive effects of resilience factors.
Keywords: COR theory, PTSD symptoms, acute pain, vulnerability factors
INTRODUCTION
Approximately 20–70% of individuals with Posttraumatic Stress Disorder (PTSD) report pain-related complaints [1]. Theoretical models that have addressed this overlap, particularly the Mutual Maintenance Model and the Shared Vulnerability Model, highlight a number of potential mechanisms by which pain and PTSD may be linked [(e.g., negative attentional biases, physical deconditioning); 2]. Notably, these models and the majority of studies evaluating the overlap between PTSD and pain have focused on PTSD symptoms occurring in the context of chronic pain [3]. Few studies have investigated factors that may confer vulnerability or resilience to worsening pain among individuals with PTSD suffering from acute pain. From the perspective of the Conservation of Resources Theory [(COR); 4–5], the current study evaluated whether vulnerability and resilience factors mediated links between PTSD symptoms and acute pain and pain-related interference in a sample of predominantly low-income women residing in the inner-city.
COR theory is a well-validated, dynamic, and integrated model of the stress process. COR theory posits that individuals are motivated to acquire, retain and protect valued personal, social, and material resources and that psychological distress, arise when actual or threatened resource loss occurs [4–5]. COR theory emphasizes the impact of resource loss over resource gains in the stress process and posits that individuals who begin with the fewest resources are the most vulnerable to additional loss precisely because they lack sufficient initial resources to apply towards recovery and management of future stressors [6]. In this way, the use of limited resources to manage an acute stressor can lead to long-term resource loss cycles in which existing vulnerability factors are exacerbated, leading to further loss and distress, and existing resilience factors are diminished, also leading to further loss and distress [6]. Prior studies have supported this notion by highlighting resource loss and loss cycles as critical in explaining poor health-related outcomes following trauma, [7]. In the context of pain, COR theory would suggest that PTSD would enhance vulnerability factors and decrease resilience factors to acute pain, with the PTSD-vulnerability-pain pathway being more robust than the PTSD-resilience-pain pathway.
To date, COR theory has not been evaluated in relation to pain, however, COR theory’s conceptualization of resource loss as a primary driver of vulnerability in the stress process may provide a theoretical bridge linking the PTSD and pain literatures. Specifically, resource loss may amplify PTSD symptoms following trauma and, in the process, increase vulnerability and diminish resilience to acute pain. Although there are several other candidate factors that may confer vulnerability or resilience to acute pain in the context of PTSD, key factors, including social undermining [8], depressive symptoms [9–10], optimism [11], engagement [12], and social support [13–14] have received marked attention in both the PTSD and pain literature.
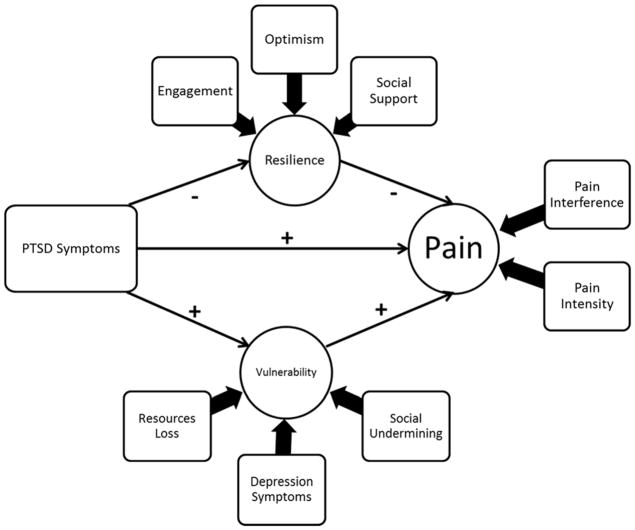
In the present study, we investigated whether vulnerability and resilience factors mediated the relationship between PTSD symptoms and acute pain and pain interference. These relationships were examined in a diverse sample of low-income women who presented to an inner-city Emergency Department (ED) with an acute pain complaint. Following our conceptual model (see Fig. 1), we generalized from the chronic pain and PTSD literature to hypothesize that there would be a significant direct relationship between PTSD symptoms and acute pain factors and that PTSD would also be significantly linked to pain factors through positive relationships with vulnerability factors and negative relationships with resilience factors. As informed by COR theory’s emphasis on loss over gain in the stress process, we further expected that PTSD would be linked to pain factors more strongly through vulnerability factors than through resilience factors.
Fig 1.
Conceptual model depicting direct effects of PTSD symptoms on vulnerability, resilience and pain factors and indirect effects of PTSD symptoms on pain factors through resilience and vulnerability factors.
METHODS
Participants
The data from the current study are part of an ongoing longitudinal study exploring the relationship between trauma and pain among women who presented to our institution’s inner-city Chicago ED with an acute pain complaint. At the time of the current analysis, 1374 women had been approached for recruitment. Of those 1374 women, 1052 (76.6%) were deemed eligible to participate (Ineligible = 382). Of those 1052 women, 925 (89.6%) were interested in participating (Refused participation = 127). Of those 925 women, 341 (36.8.1%) completed their baseline interview (lost to follow up = 55).
In the current study, only data collected at the baseline interview (N = 341) were used for analyses. This baseline sample was approximately 28.61 years-old (SD = 6.06) and predominantly African American (58.0%), followed by Hispanic/Latina (21.9%), White/Non-Hispanic (14.6%), and Other (5.0%). Race/ethnicity composition of the sample of women who completed baseline interviews was not significantly different from the samples of women who did not complete baseline interviews (i.e., those who refused to participate, were ineligible or were lost to follow up) See Table 1 for additional baseline sample characteristics.
Table 1.
Characteristics for Total Sample
| Total Sample N = 341 |
||
|---|---|---|
|
| ||
| Demographic Variables | M/n | SD/% |
| Age | 28.61 | 6.06 |
|
|
||
| Race/Ethnicity | ||
| African American | 199 | 58.0 |
| Hispanic/Latina | 75 | 21.9 |
| White/Non-Hispanic/Latina | 50 | 14.6 |
| Other | 17 | 5.0 |
|
|
||
| Education | ||
| High School or Less | 128 | 37.3 |
| Some college | 138 | 40.2 |
| College degree or Higher | 75 | 22.9 |
|
|
||
| Employment | ||
| Unemployed | 91 | 26.5 |
| Part-Time/Multiple Jobs | 88 | 25.7 |
| Full-Time | 162 | 47.2 |
|
|
||
| Annual Income | ||
| < $10,000 | 122 | 35.6 |
| $10,000–$39,999 | 132 | 38.5 |
| > $40,000–$59,999 | 80 | 23.3 |
| Don’t Know | 7 | 2.0 |
|
|
||
| Pain Location at ED Visit | ||
| Abdomen | 181 | 53.1 |
| Back | 30 | 8.8 |
| Chest | 79 | 23.2 |
| a Other | 51 | 15 |
|
|
||
| Suspected Cause of Pain Complaint at ED Visit | ||
| Infectious Disease Process | 114 | 33.4 |
| Musculoskeletal | 52 | 15.2 |
| Genital-Related | 22 | 6.5 |
| Gastrointestinal-Related | 17 | 5.1 |
| Nonspecific/Undetermined Cause | 94 | 27.6 |
| Combination/Multiple Etiologies | 16 | 4.7 |
| b Other | 24 | 7.5 |
|
| ||
| Primary Study Variables | M | SD |
|
| ||
| PTSD Symptoms | ||
| PCL-5 Total Score (Range = 0–80) | 17.06 | 15.93 |
|
| ||
| Latent Variables | M | SD |
|
| ||
| Vulnerability | ||
| Resource Loss Total Score (Range = 0–33) | 8.10 | 6.80 |
| PROMIS-4, Depression Scale Total Score (Range = 4–20) | 7.39 | 3.96 |
| Social Undermining Total Score (Range = 7–35) | 15.40 | 6.02 |
| Resilience | ||
| Optimism Total Score (Range = 0–24) | 15.73 | 4.154 |
| Engagement Total Score (Range = 0–48) | 31.16 | 8.57 |
| Social Support Total Score (Range = 0–20) | 15.05 | 4.33 |
| Pain | ||
| Pain Intensity (Range = 0–10) | 5.29 | 3.01 |
| Pain Interference (Range = 0–32) | 14.00 | 8.88 |
Other locations of pain upon presentation to ED: Neck = 9; Shoulder = 3; Pelvis = 20; Combination/Multiple Sites = 18.
Other suspected causes of acute pain complaint at ED visit: Metabolic = 4; Inflammatory = 4; Surgical = 3; Toxicology = 1; Neuro-Related = 1; Psychiatric = 6; Cardiac/Pulmonary = 5; Hematologic = 1.
Procedure
The following study procedures were approved by our Institutional Review Board. Study staff approached women at the ED with information about participating in a study about trauma and pain. For women who expressed interest in participating, study staff collected contact information and then conducted a brief telephone-screening interview within 72-hours of the ED visit to determine eligibility to participate in the study. Inclusion criteria were as follows: (1) female, (2) 18–40 years old, (3) premenopausal, (4) able to read and write English sufficiently to provide informed consent, and (5) presented to our institution’s ED with an acute pain complaint of the chest, abdomen/pelvis, neck/shoulder, or back (i.e., not extremity or head pain). Exclusion criteria were as follows: (1) pain intensity or any injury or illness great enough to impair concentration or capacity to understand study instructions or the nature of being in the study, (2) current chronic illness that involved constant or frequent pain, (3) history of chronic pain on presentation in ED or documented in the Electronic Medical Record (EMR), (4) appearing intoxicated or under the influence of drugs at the ED visit, (5) self-reported or EMR-documented daily opiate use over the prior 3 months, or (6) the presenting ED pain complaint was due to a traumatic circumstance (e.g., a motor vehicle accident [MVA]), physical assault, sexual assault, etc.). This latter exclusionary criterion was established in order to avoid the confounding effects of the presenting pain complaint and any reported PTSD symptoms being from the same event (e.g., a MVA survivor may have both pain and PTSD from the MVA, not because pain and PTSD impact each other). In addition, participant EMRs and notes from their ED encounter were individually reviewed by a co-author who is an Emergency Medicine physician to affirm the location and suspected cause of the acute pain complaint.
Following completion of the telephone screening interview, eligible participants were scheduled for a baseline interview where they completed in-person informed consent. The baseline interview collected information on participants’ demographic characteristics, mood, psychosocial functioning, pain intensity, pain-related interference, and current/past PTSD symptoms. Participants were compensated for their time in the form of gift cards from a local retail store and were paid up to $150 for completion of all baseline interviews and pain assessments.
Measures
PTSD Symptoms
The total score from the 20-item PTSD Checklist for DSM-5 [(PCL-5); 15] was used to measure PTSD symptoms. Prior to administration of the PCL-5, participants were asked to reflect on their worst or most distressing trauma (i.e., their index trauma) and were then asked to rate the degree to which over the previous month, on a 0 (not at all) to 4 (extremely) scale, they had experienced PTSD symptoms related to re-experiencing, avoidance, hyperarousal, and negative alterations in cognition and mood. Total scores range from 0–80 with higher scores indicating more severe symptoms of PTSD. Scores above 33 are suggestive of a potential PTSD diagnosis. The measure has adequate reliability [(α = .94); 16].
Resilience Factors
Social Support was assessed with a 10-item scale based on Weiss’s [17] theory of social provisions using a scale from 0–2 (No= 0, 1 = Sometimes, 2 = Yes) with 5 negatively worded items reversed scored. Respondents were asked if they feel they have someone in whom they can confide, with whom they can talk about problems, who will help with chores and responsibilities, to whom they can turn for support, and who makes them feel loved and wanted. Total scores can range from 0–20, with higher scores indicating higher perceived social support (α = .81).
Optimism was assessed with the total score from The Life Orientation Test – Revised [LOT-R; 18], a 10-item measure designed to assess individual differences in generalized optimism versus generalized pessimism on a 0 (Strongly Disagree) to 4 (Strongly Agree) scale. The scale contains three optimism items, three pessimism items and four “filler” items. Pessimism items are reversed scored and total scores are calculated without “filler” items. Higher total scores on the LOT-R indicate higher Optimism (α = .73).
Engagement was measured with an 8-item adapted version of Schaufeli et al.’s [19] Work-Engagement scale. Items were adapted to reflect engagement across broad life domains rather than engagement in specific employment-related settings and tasks. Previous studies on the role of engagement in traumatized populations have been published with this adapted scale [12]. The adapted Engagement Scale asks respondents to rate, on a 0 (Never) to 6 (Always) scale, the degree to which they feel full of energy, enthusiastic, proud of their accomplishments, find meaning in their activities and are absorbed by their activities. Total scores can range from 0–48 with higher scores indicating higher levels of Engagement (α = .87).
Vulnerability Factors
Resource Loss
Resource Loss was assessed via the total score from an 11-item adapted version of the COR-Evaluation [20], which asks respondents to rate over the past six months, on a scale from 0 (no loss at all) to 3 (lost very much), the extent to which they have lost personal, social and/or material resources (e.g., employment, finances, intimacy in relationships, family stability, perceived sense of self). Total scores can range from 0–33, with higher scores indicating greater loss of resources (α => .86). Prior research has shown high concordance between perceived and actual resource loss [21].
Depressive Symptoms were assessed with the total raw score from the PROMIS-4 Short-Form Depression scale [22] that asks respondents to rate, on a scale from 1 (not at all) to 5 (very much), how much they felt worthless, helpless, hopeless, and had a depressed mood over the previous 7 days. Total raw scores can range from 4–20, with higher scores indicating higher total of depressive symptoms. The measure has adequate reliability [(α = .91); 22].
Social Undermining was assessed with The Social Undermining Scale [23], a 7-item scale that asks respondents to rate, on a scale from 1 (not at all) to 5 (nearly all the time), how often individuals closest to the respondent display negative affect towards the respondent, negatively evaluate or criticize the respondent, and hinder the respondent’s attainment of personal goals. Total scores can range from 7–35, with higher scores indicating more frequent experiences of social undermining (α = .89).
Pain Intensity
Pain intensity was measured on 11-point numeric rating scale [24] of how much pain they were experiencing at that moment (0 = None at All – 10 = Extreme) in the same area of their body that they experienced pain on presentation to the ED.
Pain Interference
Pain interference was measured with the total raw score from the PROMIS 8-item short form scale [25] that asks respondents to rate, on a scale from 0 (not at all) to 4 (very much), how much their pain that brought them to the ED had interfered with their engagement in and enjoyment of daily work, home and social-related activities. Total raw scores can range from 0–32, with higher scores indicating higher pain-related interference. The measure has adequate reliability [(α = .93); 26].
Data Analytic Strategy
Descriptive statistics and bivariate correlations were first examined to characterize our primary study variables. Structural equation modeling (SEM) was then conducted with Mplus v.7.4 software [27] to examine relationships among our variables of interest (see Fig. 1). SEM techniques afford the opportunity to create and analyze latent variables (which represent the common variance underlying a group of observed variables). We derived a vulnerability latent variable from the Resource Loss total score, the PROMIS-4 Depression total raw score, and the Social Undermining Scale total score. We derived the resilience latent variable from the Engagement Scale total score, the Social Support Scale total score and the Optimism Scale total score. Finally, we derived the pain latent variable from the Pain Intensity rating and the Pain Interference total score. PTSD symptoms were measured at the indicator level with the total score from the PCL-5.
Bootstrapping techniques and maximum likelihood estimation were used in the estimation of our measurement and structural models. Bootstrapping techniques provided 95% confidence intervals to determine the significance of indirect effects. Maximum likelihood estimation allowed all cases in the dataset to be analyzed, even those with missing data (of which < .05% were missing). Model fit was determined via several fit indices, including the root mean square error of approximation (RMSEA), the comparative fit index (CFI), and the standardized root mean square residual (SRMR). Adequate model fit was determined based on published recommendations [28] with RMSEA values < .08, CFI values > .95 and SRMR values < .09. Prior to evaluation of our structural model, we evaluated the fit of our three latent variables in a measurement model.
RESULTS
Sample Characteristics
Table 1 provides descriptive statistics for demographic and primary study variables and location of participant pain on presentation to the ED. The sample was predominantly African American (58.0%), followed by Hispanic/Latina (21.9%), White/Non-Hispanic (14.6%), and Other (5.0%). Just over a third (35.6%) of the sample reported an annual household income of less than $10,000, less than half (47.2%) reported full-time employment outside the home, and 37.3% reported obtaining a high school education or less. Just over half of the sample (53.1%) presented to the ED with pain-related complaint in the abdomen and the most common suspected cause of the pain related complaint was an infectious disease process. Nearly all (93.5%) participants reported experiencing at least one prior traumatic event in their lives and 18.2% of the sample scored above the clinical cutoff for a suspected PTSD diagnosis. Table 2 presents bivariate correlations among primary study variables. Apart from non-significant correlations between optimism and pain intensity and optimism and pain interference, all other primary study variables were significantly correlated at the p < .01 level.
Table 2.
Bivariate correlations among primary study variables.
| Study Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. PTSD | 1 | |||||||
| 2. Social Support | −.49** | 1 | ||||||
| 3. Optimism | −.25** | .33** | 1 | |||||
| 4. Engagement | −.32** | .24** | .49** | 1 | ||||
| 5. Resource Loss | .52** | −.49** | −.47** | −.43** | 1 | |||
| 6. Depression | .63** | −.36** | −.39** | −.51** | .64** | 1 | ||
| 7. Social Undermining | .49** | −.52** | −.33** | −.38** | .51** | .44** | 1 | |
| 8. Pain Intensity | .31** | −.18** | −.10 | −.18** | .21** | .28** | .17** | 1 |
| 9. Pain Interference | .32** | −.18** | −.08 | −.15** | .22** | .31** | .16** | .69** |
Note. Significant bivariate correlations are bolded and denoted
p<.05 and
p < .01
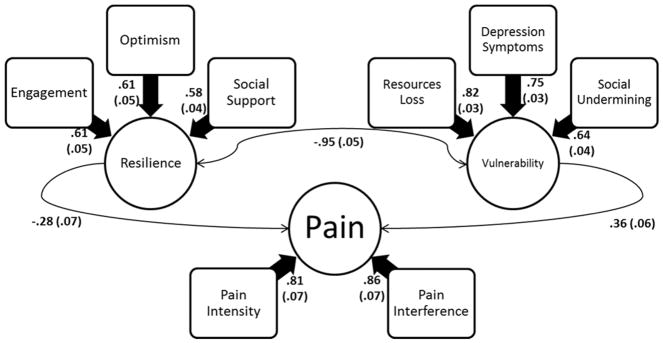
Measurement Model Fit of Latent Variables
The measurement model of the three latent variables was analyzed following Figure 2. The measurement model demonstrated good fit [(X2 (16) = 48.08, p = .000, CFI = .97, RMSEA = .07, 90% C.I. [.05, .10], SRMR = .04] and all respective indicators loaded significantly on to their latent Vulnerability, Resilience or Pain variable (all p’s < .05)
Fig 2.
Latent variables evaluated in a cross-sectional Measurement Model with corresponding standardized parameter estimates and standard errors significant at p <.05.
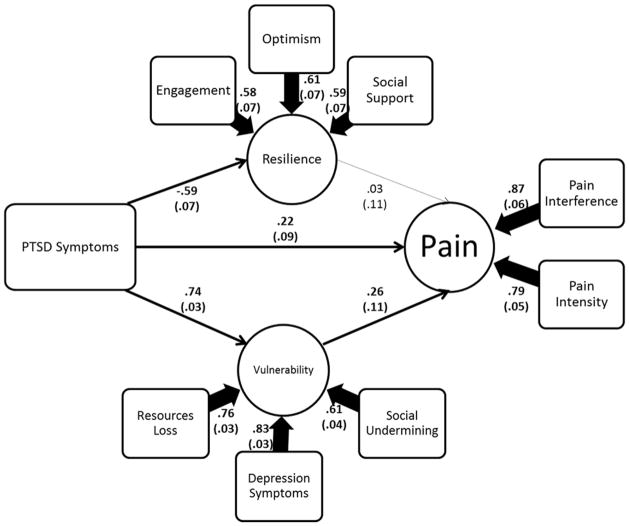
Structural Model Fit and Results
The structural model was first analyzed in accordance with Figure 3. The structural model demonstrated poor fit [(X2 (23) = 231.94, p = .000, CFI = .818, RMSEA = .16, 90% C.I. [.15, .18], SRMR = .11]. However, the only non-significant path in the model was between the resilience latent variable and the pain latent variable. Accordingly, it was determined via changes in fit indices with and without the latent resilience variable included in the model that a more parsimonious model without the resilience variable provided a better fit of the data [29].
Fig 3.
Conceptual Model evaluated in a cross-sectional Structural Equation Model. Solid highlighted paths and the corresponding standardized parameter estimates and standard errors are significant at p <.05.
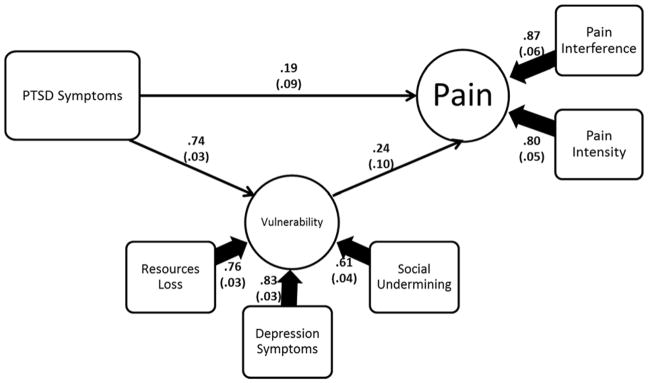
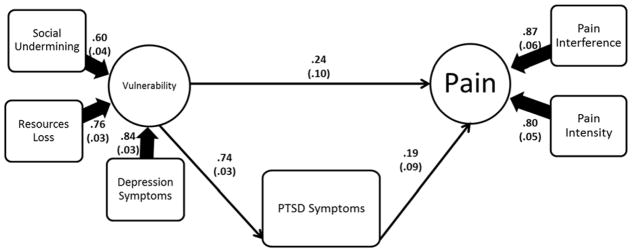
Revised Structural Model Fit and Results
The revised structural model was next analyzed as presented in Figure 4. The revised structural model without the resilience latent variable demonstrated good fit [(X2 (7) = 21.26, p =.004, CFI = .98, RMSEA = .07, 90% C.I. [.04, .12], SRMR = .02]. Higher PCL-5 scores (i.e., PTSD symptoms) were directly related to higher vulnerability factor values (B = .74) and higher pain factor values (B = .19). Higher vulnerability factor values, in turn, were directly related to higher pain factor values (B = .24). The indirect effect of PCL-5 scores on pain factor values through vulnerability factor values was significant (B = .18) (all p’s < .05). Because this model was based on cross sectional data, we also evaluated a plausible alternative model in which vulnerability and/or resilience variables preceded PTSD symptoms in relation to pain outcomes.
Fig. 4.
Revised Conceptual Model evaluated in a cross-sectional Structural Equation Model. Solid highlighted paths and the corresponding standardized parameter estimates and standard errors are significant at p <.05. (AIC = 9707.17).
Reverse Pathway Structural Model Fit and Results
The alternative, revised structural model addressing possible reversed paths was analyzed as presented in Figure 5. This alternative reverse-path model without the resilience variable retained identical factor loadings and path coefficients as the original, revised structural model. In addition, model fit indices between the original and the alternative, revised structural model for X,2, RMSEA, CFI and SRMR were identical. Accordingly, Akaike Information Criteria (AIC) values were compared to determine which model had smaller AIC values and, thus, better fit. The original, revised model’s AIC was 9707.17 and the alternative, revised model’s AIC was 12564.79. Thus, the original, revised model (in which PTSD symptoms are linked to increased vulnerability which in turn leads to increased pain) had better fit and was therefore retained as the final model.
Fig. 5.
Alternative, Reverse-Pathway Model evaluated in a cross-sectional Structural Equation Model. Solid highlighted paths and the corresponding standardized parameter estimates and standard errors are significant at p <.05. (AIC = 12564.79).
DISCUSSION
Through the lens of COR theory, we investigated whether PTSD symptoms would be indirectly related to higher acute pain and pain-related interference through mediating pathways of lower levels of resilience and higher levels of vulnerability. We tested this model in a diverse sample of low-income women living in an inner-city. We found that higher PTSD symptoms were directly related to higher pain intensity and pain interference and indirectly related to higher pain intensity and pain interference through positive associations with vulnerability factors, specifically, resource loss (a key element of COR theory), depressive symptoms, and social undermining. Pathways linking PTSD symptoms to pain intensity and pain interference through resilience factors, specifically, optimism, engagement, and social support, were not supported. Accordingly, these results are consistent with COR theory [4–5] and a large body of research showing that losses or negative stimuli exert stronger effects on outcomes than gains or positive stimuli [30].
The current study affords a number of contributions. To our knowledge, this is the first study to apply COR theory to a study examining PTSD and pain and the first to examine resource loss as a key vulnerability factor in relation to pain. As such, the present findings may suggest that the oft-reported relationship between PTSD symptoms and pain may involve a more complex interplay of vulnerability factors, including resource loss, depressive symptoms, and social undermining. Although ours is the first study to link resource loss to pain-related outcomes, previous studies have found similar relationships between resource loss and other health-related outcomes, including lowered immune functioning [31]. Our results, and the application of COR theory, support and expand these studies by highlighting vulnerability factors, including resource loss, depressive symptoms, and social undermining, as key components to explore in pain-related processes among individuals with a trauma history.
Our findings also highlight the potential importance of considering socioeconomic status and pre-existing resource levels when interpreting studies of the health-relevance of resource gains or positive factors. Consider our finding that vulnerability factors were more strongly related to pain outcomes than resilience factors. This finding is in contrast with the recent attention given to the roles of positive constructs in pain-related adaptation and coping processes. Specifically, previous studies have proposed that factors like positive affect [32] and pain-related acceptance [33] may promote resilience against pain and its negative psychosocial sequelae. Critically, the demographic makeup of the majority of these studies’ samples were overwhelming White, educated and living above the poverty line. Such methodological limitations may limit the generalizability of findings regarding factors that promote resilience against pain among more racially diverse and economically disadvantaged populations.
This study has important clinical implications. Foremost for clinicians, especially those in inner-city environments where the risk for traumatic exposure is high, is the potential benefit of screening ED patients for trauma history and PTSD symptoms. Such individuals may be at an elevated risk for high levels of resource loss, pain intensity, and pain interference, making social work or psychiatric referrals critical. Further, identifying precipitating and perpetuating factors, such as PTSD symptoms that may hasten the transition to chronic pain and reliance on opioid medication, may guide clinicians to recommend alternative treatment courses. Such increased awareness of risk factors may potentially lower the chances of transitioning from acute to chronic pain and the possibility of adverse outcomes with opioid use. Finally, although the main theoretical models of comorbid PTSD and chronic pain [(i.e., mutual maintenance model, shared vulnerability model) 2–3] differ in their conceptualization of how PTSD and pain overlap, a common denominator across these models is behavioral avoidance of pain and PTSD-related stimuli. Thus, a critical strategy for prophylactic interventions targeting PTSD and pain processes may involve exposure-based procedures to increase the approach to and tolerance of reminders, cues and triggers for pain and trauma-related stimuli.
Limitations of the current study must also be delineated. At the current stage of our study, we are not yet able to investigate whether and how our variables of interest relate longitudinally to the transition from acute to chronic pain. Similarly, the cross-sectional nature of our data precludes drawing causal inferences among trauma, resource loss, vulnerability factors, and pain, although we note that the alternative, reverse-path model evaluated in the present study exhibited worse model fit than the model described above. Accordingly, it would be important for future studies to test our COR theory-based model in a longitudinal design to determine how variables such as resource loss play a role in the development of chronic pain. It is also important to note that our sample’s representation of women who face significant health disparities may limit the generalizability of our findings to women who reside outside low-income, inner-city environments with a corresponding lower risk of trauma exposure. Despite these limitations, our findings provide an important perspective on the extensive trauma and health-related burden affecting low-income, inner-city women.
In summary, our findings support COR theory as a promising theoretical framework from which to explore the overlap between PTSD and pain and suggest that resource loss may be a critical component to evaluate in pain-related processes. In addition, our results highlight the comparative magnitude of vulnerability factors over resilience factors when examining psychosocial correlates of pain-related outcomes and improve upon the existing literature by demonstrating these relationships in an understudied and vulnerable population.
Supplementary Material
Acknowledgments
This study was funded by the National Institute of Drug Abuse (NIDA; R01DA039522). None of the authors have any conflicts of interest to disclose.
References
- 1.Beck JG, Clapp JD. A different kind of co-morbidity: understanding posttraumatic stress disorder and chronic pain. Psychol Trauma. 2011;3(2):101–108. doi: 10.1037/a0021263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Asmundson GJ, Coons MJ, Taylor S, Katz J. PTSD and the experience of pain: research and clinical implications of shared vulnerability and mutual maintenance models. The Canadian Journal of Psychiatry. 2002 Dec;47(10):930–7. doi: 10.1177/070674370204701004. [DOI] [PubMed] [Google Scholar]
- 3.Brennstuhl MJ, Tarquinio C, Montel S. Chronic pain and PTSD: evolving views on their comorbidity. Perspectives in psychiatric care. 2015 Oct 1;51(4):295–304. doi: 10.1111/ppc.12093. [DOI] [PubMed] [Google Scholar]
- 4.Hobfoll SE. The ecology of stress. Taylor & Francis; 1988. [Google Scholar]
- 5.Hobfoll SE. Conservation of resources: A new attempt at conceptualizing stress. American psychologist. 1989 Mar;44(3):513. doi: 10.1037//0003-066x.44.3.513. [DOI] [PubMed] [Google Scholar]
- 6.Hobfoll SE, Johnson RJ, Ennis N, Jackson AP. Resource loss, resource gain, and emotional outcomes among inner city women. Journal of personality and social psychology. 2003 Mar;84(3):632. [PubMed] [Google Scholar]
- 7.Schumm JA, Hobfoll SE, Keogh NJ. Revictimization and interpersonal resource loss predicts PTSD among women in substance-use treatment. Journal of Traumatic Stress. 2004 Apr 1;17(2):173–81. doi: 10.1023/B:JOTS.0000022624.53181.21. [DOI] [PubMed] [Google Scholar]
- 8.Kaniasty K, Norris FH. Longitudinal linkages between perceived social support and posttraumatic stress symptoms: sequential roles of social causation and social selection. J Trauma Stress. 2008;21(3):274–281. doi: 10.1002/jts.20334. [DOI] [PubMed] [Google Scholar]
- 9.Flory JD, Yehuda R. Comorbidity between post-traumatic stress disorder and major depressive disorder: alternative explanations and treatment considerations. Dialogues in clinical neuroscience. 2015 Jun;17(2):141. doi: 10.31887/DCNS.2015.17.2/jflory. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fishbain DA, Cutler R, Rosomoff HL, Rosomoff RS. Chronic pain-associated depression: antecedent or consequence of chronic pain? A review. The Clinical journal of pain. 1997 Jun 1;13(2):116–37. doi: 10.1097/00002508-199706000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Wright MA, Wren AA, Somers TJ, et al. Pain acceptance, hope, and optimism: relationships to pain and adjustment in patients with chronic musculoskeletal pain. J Pain. 2011;12(11):1155–1162. doi: 10.1016/j.jpain.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Hobfoll SE, Johnson RJ, Canetti D, et al. Can people remain engaged and vigorous in the face of trauma? Palestinians in the West Bank and Gaza. Psychiatr. 2012;75(1):60–75. doi: 10.1521/psyc.2012.75.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schumm JA, Briggs-Phillips M, Hobfoll SE. Cumulative interpersonal traumas and social support as risk and resiliency factors in predicting PTSD and depression among inner-city women. J Trauma Stress. 2006;19(6):825–836. doi: 10.1002/jts.20159. [DOI] [PubMed] [Google Scholar]
- 14.Stevens NR, Gerhart J, Goldsmith RE, Heath NM, Chesney SA, Hobfoll SE. Emotion regulation difficulties, low social support, and interpersonal violence mediate the link between childhood abuse and posttraumatic stress symptoms. Behav Ther. 2013;44(1):152–161. doi: 10.1016/j.beth.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5) Scale available from the National Center for PTSD. 2013 at www.ptsd.va.gov.
- 16.Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress. 2015 Dec 1;28(6):489–98. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- 17.Weiss RS. The provisions of social relationships. In: Rubin Z, editor. Doing Unto Others. Englewood Cliffs, NJ: Prentice Hall; 1974. pp. 17–26. [Google Scholar]
- 18.Glaesmer H, Rief W, Martin A, Mewes R, Brähler E, Zenger M, Hinz A. Psychometric properties and population-based norms of the Life Orientation Test Revised (LOT-R) British journal of health psychology. 2012 May 1;17(2):432–45. doi: 10.1111/j.2044-8287.2011.02046.x. [DOI] [PubMed] [Google Scholar]
- 19.Schaufeli WB, Salanova M, González-Romá V, Bakker AB. The measurement of engagement and burnout: A two sample confirmatory factor analytic approach. Journal of Happiness studies. 2002 Mar 1;3(1):71–92. [Google Scholar]
- 20.Hobfoll SE, Lilly RS. Resource conservation as a strategy for community psychology. Journal of community psychology. 1993 Apr 1;21(2):128–48. [Google Scholar]
- 21.Ehrlich M, Harville E, Xiong X, Buekens P, Pridjian G, Elkind-Hirsch K. Loss of resources and hurricane experience as predictors of postpartum depression among women in southern Louisiana. Journal of Women’s Health. 2010 May 1;19(5):877–84. doi: 10.1089/jwh.2009.1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schalet BD, Pilkonis PA, Yu L, Dodds N, Johnston KL, Yount S, Riley W, Cella D. Clinical validity of PROMIS Depression, Anxiety, and Anger across diverse clinical samples. Journal of clinical epidemiology. 2016 May 31;73:119–27. doi: 10.1016/j.jclinepi.2015.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vinokur AD, Price Richard H, Caplan Robert D. Hard Times and Hurtful Partners: How Financial Strain Affects Depression and Relationship Satisfaction of Unemployed Persons and Their Spouses. Journal of Personality and Social Psychology. 1996 Jul;71(1):166–79. doi: 10.1037//0022-3514.71.1.166. [DOI] [PubMed] [Google Scholar]
- 24.Farrar JT, Young JP, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001 Nov 30;94(2):149–58. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 25.Amtmann D, Cook KF, Jensen MP, Chen WH, Choi S, Revicki D, Cella D, Rothrock N, Keefe F, Callahan L, Lai JS. Development of a PROMIS item bank to measure pain interference. Pain. 2010 Jul 31;150(1):173–82. doi: 10.1016/j.pain.2010.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Broderick JE, Schneider S, Junghaenel DU, Schwartz JE, Stone AA. Validity and Reliability of Patient-Reported Outcomes Measurement Information System Instruments in Osteoarthritis. Arthritis care & research. 2013 Oct 1;65(10):1625–33. doi: 10.1002/acr.22025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Muthén LK, Muthén BO. Statistical analysis with latent variables Version. 2015. Mplus; p. 7. [Google Scholar]
- 28.Marsh HW, Hau KT, Wen Z. In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Structural equation modeling. 2004 Jul 1;11(3):320–41. [Google Scholar]
- 29.Satorra A, Bentler PM. Ensuring positiveness of the scaled difference chi-square test statistic. Psychometrika. 2010;75:243–248. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vaish A, Grossmann T, Woodward A. Not all emotions are created equal: the negativity bias in social-emotional development. Psychological bulletin. 2008 May;134(3):383. doi: 10.1037/0033-2909.134.3.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ironson G, Wynings C, Schneiderman N, Baum A, Rodriguez M, Greenwood D, et al. Posttraumatic stress symptoms, intrusive thoughts, loss, and immune function after Hurricane Andrew. Psychosomatic Medicine. 1997;59:128–141. doi: 10.1097/00006842-199703000-00003. [DOI] [PubMed] [Google Scholar]
- 32.Strand EB, Zautra AJ, Thoresen M, Ødegård S, Uhlig T, Finset A. Positive affect as a factor of resilience in the pain—negative affect relationship in patients with rheumatoid arthritis. Journal of psychosomatic research. 2006 May 31;60(5):477–84. doi: 10.1016/j.jpsychores.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 33.McCracken LM. Learning to live with the pain: acceptance of pain predicts adjustment in persons with chronic pain. Pain. 1998 Jan 31;74(1):21–7. doi: 10.1016/S0304-3959(97)00146-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.