Abstract
Objectives:
To determine whether caregiver relationship and race modify associations between physical functioning of persons with dementia and their caregiver’s burden and general depressive symptoms.
Method:
We pooled data from four behavioral intervention trials (N=1,211). Using latent growth modeling, we evaluated associations of physical functioning of persons with dementia with the level and rate of change in caregiver burden and general depressive symptoms of caregivers. We then tested for differences by caregiver relationship (spouse vs. non-spouse) and race (white vs. non-white).
Results:
Persons with dementia were, on average, 81 years old (68% female) and followed up, on average, 0.5 years. More baseline physical impairment of persons with dementia was associated with less worsening in caregiver burden over time (β=−0.23, 95% CI: −0.29, −0.14). Neither caregiver relationship nor race of the caregiver modified this relationship. More impaired baseline physical functioning of persons with dementia was not associated with changes in depressive symptoms (β=−0.08, 95% CI: −0.17, 0.00), but was associated with less worsening in depressive symptoms among spousal (β=−0.08, 95% CI: −0.17, 0.00) and non-white (β=−0.08, 95% CI: −0.17, 0.00) caregivers.
Conclusions:
Dementia caregivers may experience reduced caregiver-related burden over time as a consequence of adjusting to the functional status of persons with dementia, while spousal and non-white caregivers may experience less depressive symptoms resultant of adjustment to functional status.
Keywords: physical functioning, harmonization, caregiver burden, dementia, depression
Introduction
There are approximately 5.3 million Americans age 65 and older living with Alzheimer’s disease, the most common type of dementia (Hebert, Weuve, Scherr, & Evans, 2013). An estimated 15 million Americans provide unpaid care for people with Alzheimer’s disease and other dementias (Alzheimer’s Association, 2016; National Alliance for Caregiving & AARP Public Policy Institute, 2015), and persons with dementia often live with caregivers (Kasper, Freedman, Spillman, & Wolff, 2015). With disease progression, caregivers are in the forefront of providing hands-on assistance with physical functioning, e.g., instrumental and basic self-care activities of daily living, of persons with dementia.
Dementia caregivers, tasked with assisting with growing demands of physical limitations of persons with dementia, may experience feelings of burden and depression. Higher levels of dependency in basic and instrumental activities of daily living of persons with dementia, coupled with the severity of behavioral problems, may add to feelings of burden and depression as well as physical morbidity of dementia caregivers (Knight et al., 2002; Hooker et al., 2002; Lee & Kolomer, 2005; Mendez-Luck et al., 2008; Ory, Hoffman, Yee, Tennstedt, & Schulz, 1999; Pinquart & Sörensen, 2005). Individual differences in management of stressors of caring for someone with dementia might be explained by stress process models. Particularly, Pearlin’s stress process framework focuses on sources of stress directly and indirectly related to the caregiving role (Pearlin, Mullan, Semple, & Skaff, 1990). Although there are indirect stressors related to the caregiving role, we are focused on the effects of higher levels of functional impairment, as defined by basic and instrumental activities of daily living, in persons with dementia on levels and change of both caregiver burden and depressive symptoms over time in this study (Figure 1).
Figure 1.
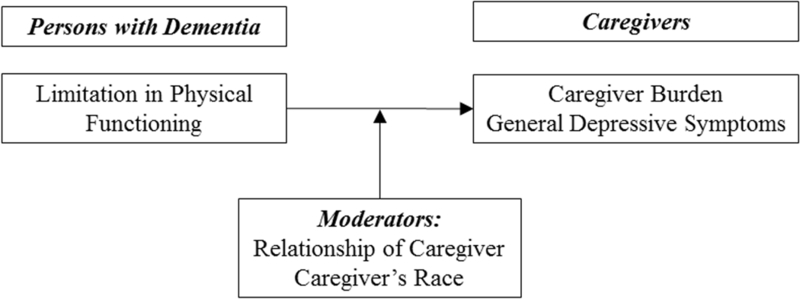
Conceptual Framework. We hypothesized that greater impairment in baseline physical functioning of persons with dementia is associated with greater levels of, and longitudinal worsening of, depressive symptoms and caregiver burden in the overall sample. We further hypothesized that associations are strongest among caregivers of persons with dementia who were white and who were spouses.
The association of functional impairment in persons with dementia with level and change in both caregiver burden and depressive symptoms could be moderated by certain caregiver characteristics. In this study, we were interested in the moderating role of a caregiver’s relationship to a person with dementia and caregiver race (Figure 1). Previous results of caregiver’s relationship to both caregiver burden and depressive symptoms are mixed. There have been negative effects of physical and mental changes in older adults with dementia on spouses (de Vugt et al., 2003; Eloniemi-Sulkava et al., 2002; Gallagher-Thompson, Dal Canto, Jacob, & Thompson, 2001; Narayan, Lewis, Tornatore, Hepburn, & Corcoran-Perry, 2001). Feelings of loneliness and loss have been reported by spousal caregivers (Beeson, 2003). Nonspousal caregivers reported higher rates of depression and perceived burden than other caregivers, but this finding could have been attributed to sex and cultural differences (Pinquart & Sörensen, 2005). A study by Välimäki, Martikainen, Hallikainen, Väätäinen, and Koivisto (2015) found that spousal caregivers were more likely to experience distress and depression than non-spousal caregivers at baseline and three years after the observation period. Age of caregiver is interrelated with caregiver’s relationship to person with dementia, as spousal caregivers are more likely to be older than non-spousal caregivers (National Alliance for Caregiving & AARP Public Policy Institute, 2015). Older caregivers tend to experience more age-associated health problems and functional impairments themselves, which may complicate physical care for another (Connell, Janevic, & Gallant, 2001; Schneider, Murray, Banerjee, & Mann, 1999). Because of health complications, spousal caregivers could be adversely affected by greater physical impairment of persons with dementia.
Besides caregiver’s relationship, cultural variation, for which race may be interpreted as a surrogate, may affect the association of greater functional impairment in persons with dementia with level and change of both caregiver burden and depressive symptoms (King, Hartke, & Houle, 2010). Previous studies have reported that Caucasian caregivers report higher levels of burden and depression than African American caregivers (Connell & Gibson, 1997; Janevic & Connell, 2001). Caucasian caregivers may view caregiving as unsettling and abrupt, while African American caregivers may view caregiving as expected and commonplace, an expectation that could be protective against distress (Haley et al., 1996). African American caregivers of persons with dementia are more likely to report more positive caregiving experiences, i.e., rewards and satisfaction of caregiving, due to active coping and greater resilience (Dilworth-Anderson et al., 2005; Roth, Dilworth-Anderson, Huang, Gross, & Gitlin, 2015). In our study, we would expect to see worsening of both caregiver burden and depressive symptoms with greater physical impairment of persons with dementia among white, not non-white, caregivers.
In this study, we addressed whether physical functioning of persons with dementia is associated with negative aspects of caregiving, including caregiver burden and depressive symptoms, in caregivers of persons with dementia who are seeking intervention services. Figure 1 summarizes the hypothesized associations we sought to test in this study. We hypothesized that more impaired baseline physical functioning of persons with dementia is associated with greater levels of and longitudinal worsening of depressive symptoms and caregiving burden in the overall sample (Figure 1). We further examined whether caregivers’ relationship and race modified these associations, hypothesizing that associations would be strongest among caregivers of persons with dementia who were spouses and white, as compared to non-spouses and non-whites (Figure 1). To address our questions in a large, generalizable sample of dementia caregivers seeking intervention services, we pooled longitudinal data on physical functioning, caregiver burden, and caregiver depressive symptoms across four behavioral intervention studies involving dementia caregivers who sought intervention services.
Methods
Participants
The sample consisted of 1,211 individuals pooled from the following four behavioral intervention trials: Advancing Caregiver Training (ACT, N=272), Care of Persons with Dementia in their Environments (COPE, N=237), Resources for Enhancing Alzheimer’s Caregiver Health II (REACH II, N=643), and the Tailored Activity Program (TAP, N=59). Institutional Review Boards at each study’s home institution approved study design and data collection procedures, and this study was approved by the Johns Hopkins Bloomberg School of Public Health IRB.
ACT was a randomized controlled efficacy trial of family caregivers of persons with dementia exhibiting behavioral symptoms that tested a home-based intervention to manage or reduce distressful behavioral symptoms (Gitlin et al., 2006). Data used from ACT consisted of baseline, four-month, and six-month follow-ups. COPE was a randomized intervention to test a behavioral approach to support physical functioning and quality of life of persons with dementia and caregiver well-being (Gitlin, Winter, Dennis, Hodgson, & Hauck, 2010). Data used from COPE consisted of baseline, four-month, and nine-month follow-ups. REACH II was a multi-site randomized intervention to improve quality of caregiving among dementia caregivers (Belle et al., 2006). REACH II data consisted of baseline and six-month follow-ups. The TAP study tested a home-based occupational therapy intervention that provided activities tailored to interests and abilities of persons with dementia and trained their family caregivers in their use as part of routine care to reduce behavioral symptoms (Gitlin et al., 2009). Data used from TAP consisted of baseline and four-month follow-ups. ACT, COPE, and TAP were conducted in Philadelphia, PA, while REACH II was conducted across five U.S. sites (Birmingham, AL; Memphis, TN; Miami, FL; Palo Alto, CA; and Philadelphia, PA).
Eligibility criteria of persons with dementia and primary outcomes were similar across studies, since persons with dementia had to have a physician diagnosis of Alzheimer’s disease-related dementia or Mini Mental State Examination (MMSE) score <24, yet they could not be bed-bound and have MMSE=0. The primary outcomes of ACT and COPE were functional dependence, quality of life, frequency of agitated behaviors, and engagement for patients and well-being, confidence using activities, and perceived benefits for caregivers. The primary outcome of REACH II was a quality-of-life indicator comprised of caregiver depression, burden, self-care, and social support and problem behaviors of the person with dementia, while the primary outcome for TAP included frequency of targeted problem behavior and caregiver upset with and confidence managing it at 4 months. In all studies, caregivers’ quality of life was improved with the non-pharmalogical intervention.
The control group in each study differed. The control group in COPE received educational materials and three telephone calls. The control group in ACT did not receive any intervention, whereas the control group in TAP was wait-listed for the intervention for four months after the intervention took place. The control group in REACH II was mailed a packet of educational materials and given two telephone calls 3 and 5 months after randomization. In all studies, caregivers’ quality of life was improved with the non-pharmalogical intervention.
Variables
Physical functioning of Persons with Dementia
We derived and validated a harmonized measure of physical functioning of persons with dementia across the datasets used in this study (Armstrong et al., 2017; Gross, Jones, & Inouye, 2014). Details about methods and results are provided in Armstrong et al., 2017. We provided a list of physical functioning items that were used for the summary physical functioning measure in Supplementary Table 1. Briefly, we estimated factor scores from a 1-parameter logistic graded response item response theory (IRT) model using common and unique questions about activities of daily living (ADLs) and instrumental activities of daily living (IADLs) (Lord, 1953; Takane & Leeuw, 1987). Higher factor scores, scaled to have a mean of 50 and standard deviation (SD) of 10, indicate worse functional impairment. We winsorized the lowest 4% of the distribution of physical functioning scores.
Caregiver burden
Caregiver burden was defined by 13 questions from a self-report measure of burdens related to caregiving in COPE, TAP, REACH II, and ACT (Bédard et al., 2001; Zarit, Orr, & Zarit, 1985). The self-report measure included questions about not having time for oneself because of the time spent in caregiving, feeling stressed while balancing caregiving with other responsibilities, feeling angry or strained when around the care recipient, feeling that the care recipient affects the caregiver’s relationships with other family members or friends adversely, feeling that physical health and/or social life was suffering due to caregiving, not having privacy, feelings of loss of control, uncertainty about the care recipient, and feelings of guilt for not doing more for the care recipient. Using these items, we constructed a factor score of caregiver burden using a 2-parameter logistic IRT model (Samejima, 1969). The factor score was scaled to a T-score (mean 50, SD 10) and was scored such that higher values indicate greater burden.
Caregiver Depressive Symptoms
Depressive symptoms in each study were measured using different versions of the Centers for Epidemiologic Studies – Depression (CES-D) scale (Radloff, 1977). TAP used a 20-item version, ACT and COPE used a 10-item version, and REACH II used a 12-item version. Similar to caregiver burden, using a 2-parameter logistic IRT model (Samejima, 1969), we constructed a summary factor score of caregiver depressive symptoms on a T-score scale and scored such that higher values indicate more depressive symptoms.
Covariates
We adjusted models for characteristics of persons with dementia, including continuous age at baseline visit, sex, race/ethnicity, education attainment level, and intervention group. Race/ethnicity was categorized as non-Hispanic white vs. non-white. Education attainment level was categorized as high school graduate or lower vs. more than high school. Educational attainment could be more relevant adjustment variable than years in school, due to regional and racial differences in years of education (Glymour & Manly, 2008). To adjust for intervention group, we used a binary indicator of whether participants were in an intervention vs. control arm of a trial.
Caregiver Characteristics.
Caregivers self-reported whether they were a spouse or non-spouse of the person with dementia. Self-reported race/ethnicity of caregivers was coded as either non-Hispanic white or non-white, inclusive of Hispanics, African Americans, and Other. Due to the sample compositions of COPE, ACT, and TAP having few Hispanics, we collapsed self-reported race/ethnicity into white vs. non-white. Age of caregivers was categorized based on the median age of 60 years (≥60 years vs. <60 years).
Statistical analysis
We first described demographic characteristics of the sample in each dataset, using chi-squared tests for categorical variables and t-tests for continuous variables.
Associations of physical functioning of persons with dementia with baseline level and rate of change in negative aspects of caregiving
We estimated associations of physical functioning of persons with dementia with each negative aspect of caregiving outcome using latent growth curve models, which are equivalent to mixed effects models with random intercepts and slopes. We adjusted for age, sex, race, education level, and study intervention group of persons with dementia. To test for effect modification by caregiver relationship and race, we further estimated models separately in groups defined by caregiver relationship and race. We used Mplus software to estimate models, using a maximum likelihood estimator with robust standard error estimation under the expectation-maximization algorithm (Muthen & Muthen, 1998–2012). Since the eligibility criteria were similar across studies in terms of dementia severity of persons with dementia, we did not evaluate whether dementia severity moderated the association of physical functioning of persons with dementia with each negative aspect of the caregiving outcome.
Sensitivity analyses
We performed four sets of sensitivity analyses. First, to confirm that no single study unduly influenced estimates in the pooled sample, we removed each study one at a time and reran the main models (Nordahl et al., 2014). Second, we further estimated models separately in groups defined by caregiver age to determine whether there were similar associations to those found by caregiver relationship (spouse vs. non-spouse), since caregiver age and relationship are highly correlated with one another. In a third sensitivity analysis, instead of adjusting for intervention condition as in the main analysis, we excluded participants in the intervention arms of each trial and pooled control participants from each study (N=606) to determine whether inferences changed.
Results
Sample characteristics
There were 1,211 participants across the four behavioral intervention studies (ACT, COPE, REACH II, and TAP) (Table 1). The pooled sample of persons with dementia was mostly female (67.8%) and approximately half were white (51.5%). Approximately 47% had more than a high school level of education. Participants contributed on average 2.2 (SD=0.6 visits) study visits over a mean of 6 months (SD=2.4 months). Baseline age, sex, race/ethnicity, years of education, and years in study of persons with dementia differed among the studies (all p’s<0.01). Mean baseline age was younger in REACH II and TAP than in ACT and COPE. ACT and COPE had more women (>80%) than REACH II or TAP. ACT, COPE, and TAP were predominantly white (>70%). COPE, on average, had more follow-up time (0.75 years) than other studies (Table 1).
Table 1.
Characteristics of Study Sample
| Characteristics of Persons with Dementia | Overall | Advancing Caregiver Training (ACT) |
Care of Persons with Dementia in their Environments (COPE) |
Resources for Enhancing Alzheimer’s Caregiver Health (REACH II) |
Tailored Activity Program (TAP) |
p-value for difference in means |
|---|---|---|---|---|---|---|
| Sample Size | 1211 | 272 | 237 | 643 | 59 | |
| Age (in Years), mean (SD) | 80.5 (9.1) | 82.4 (8.4) | 82.7 (8.7) | 79.0 (9.3) | 79.4 (9.4) | <0.01 |
| Female, n (%) | 727 (58.7) | 147 (54.0) | 165 (69.6) | 390 (58.2) | 25 (42.4) | <0.01 |
| Race/Ethnicity, n (%) | <0.01 | |||||
| White | 624 (51.5) | 191 (70.2) | 167 (70.5) | 220 (34.2) | 46 (78.0) | |
| African American | 355 (29.3) | 73 (26.8) | 62 (26.2) | 209 (32.5) | 11 (18.6) | |
| Hispanic | 218 (18.0) | 5 (1.8) | 4 (1.7) | 207 (32.2) | 2 (3.4) | |
| Other | 14 (1.2) | 3 (1.1) | 4 (1.7) | 7 (1.1) | 0 (0) | |
| Educational Attainment Level, n (%) | <0.01 | |||||
| High School or Less | 639 (52.8) | 94 (34.6) | 73 (30.8) | 456 (70.9) | 16 (27.1) | |
| More than High School | 571 (47.2) | 178 (65.4) | 164 (69.2) | 187 (29.1) | 42 (71.2) | |
| MMSE score, mean (SD) | 12.6 (7.9) | 12.7 (8.1) | 13.4 (8.0) | 12.3 (7.7) | 11.5 (8.1) | 0.17 |
| Intervention Group, n (%) | 605 (50.0) | 137 (50.4) | 117 (49.4) | 323 (50.3) | 28 (48.3) | 0.99 |
| Maximum number of visits, mean (SD) | 2.2 (0.6) | 3.0 (0.0) | 2.0 (0.0) | 1.8 (0.4) | 3.0 (0.0) | <0.01 |
| Maximum years in study, mean (SD) | 0.5 (0.2) | 0.5 (0.0) | 0.75 (0.0) | 0.4 (0.2) | 0.5 (0.2) | <0.01 |
| Characteristics of Caregivers | ||||||
| Age (≥60 years), n (%) | 687 (56.7) | 185 (68.0) | 141 (59.5) | 324 (50.4) | 37 (62.7) | <0.01 |
| Female, n (%) | 1029 (83.1) | 220 (80.9) | 202 (85.2) | 555 (82.8) | 52 (88.1) | 0.42 |
| Race (white vs. non-white), n (%) | 730 (60.3) | 193 (71.0) | 169 (71.3) | 322 (50.1) | 46 (78.0) | <0.01 |
| Spouse, n (%) | 616 (50.9) | 138 (50.7) | 152 (64.1) | 285 (44.3) | 41 (69.4) | <0.01 |
SD = standard deviation
White caregivers were 2.1 times more likely to be spouses than were caregivers in the non-white group (95% CI: 1.6, 2.6). As expected, caregivers aged 60+ years were 4.6 times more likely to be spouses of the person with dementia than were caregivers less than 60 years old (95% CI: 3.7, 5.9) (Table 1).
Associations in the overall sample
Physical functioning of persons with dementia shared considerable variance at baseline with both caregiver burden and depressive symptoms of caregivers (Table 2) such that higher physical functioning impairment scores were associated with greater caregiver burden and more depressive symptoms. Despite this, greater levels of impairment in physical functioning were associated with slower worsening in caregiver burden (β=−0.23, 95% CI: −0.29, −0.14), but not with changes in depressive symptoms of caregivers (β=−0.08; 95% CI: −0.17, 0.00).
Table 2.
Associations of Summary Physical Functioning Factor for Persons with Dementia and Aspects of Caregiving (N=1,211)
| Parameter | Caregiver burden | Depressive symptoms of the caregiver |
||||
|---|---|---|---|---|---|---|
| Estimate | Standard Error |
95% Confidence Interval |
Estimate | Standard Error |
95% Confidence Interval |
|
| Residual baseline covariance | 3.37* | 1.89 | (1.47, 5.26) | 2.74* | 2.23 | (0.51, 4.96) |
| Regression of slope on PWD physical functioning |
−0.23* | 0.04 | (−0.29, −0.14) | −0.08 | 0.04 | (−0.17, 0.00) |
| Intercept for PWD physical functioning | 43.52 | 0.34 | 43.49 | 0.35 | ||
| Intercept for model outcome | 51.34 | 0.29 | 51.09 | 0.30 | ||
| Slope for model outcome | 4.82 | 2.17 | −2.32 | 2.76 | ||
p<0.05, PWD = persons with dementia
Note: The first row presents associations of the intercept of the summary physical functioning factor of persons with dementia with the intercepts for negative caregiving aspects. The second row presents regressions of rate of change for each negative aspect of caregiving on the baseline physical functioning factor of the persons with dementia. Subsequent rows provide model-estimated mean levels and rates of change in each exposure and outcome. For factor scores representing physical functioning of persons with dementia, caregiver burden, and caregiver depressive symptoms, higher scores indicate greater impairment, more burden, and more depressive symptoms, respectively.
Associations by spousal relationship of caregiver
More impaired physical functioning of persons with dementia was associated at baseline with greater caregiver burden among spousal (β=8.77, 95% CI: 8.52, 9.02) caregivers and less caregiver burden among non-spousal caregivers (β=−0.75, 95% CI: −1.35, −0.16) (Table 3). Physical functioning of persons with dementia predicted slower worsening in caregiver burden among both spousal (β=−0.22, 95% CI: −0.37, −0.08) and non-spousal (β=−0.24, 95% CI: −0.40, −0.08) caregivers. Physical functioning was associated with more depressive symptoms among non-spousal caregivers (β=4.73, 95% CI: 4.35, 5.11) and faster declines in depressive symptoms among spousal caregivers (β=−0.16, 95% CI: −0.33, −0.05) (Table 3).
Table 3.
Associations of Summary Physical Functioning of Persons with Dementia and Negative Caregiving Aspects by Spousal Group (N=1,211)
| Parameter | Caregiver burden | Depressive symptoms of the caregiver |
||||
|---|---|---|---|---|---|---|
| Estimate | Standard Error |
95% Confidence Interval |
Estimate | Standard Error |
95% Confidence Interval |
|
| Spousal caregivers, n=616 | ||||||
| Residual baseline covariance | 8.77* | 0.25 | (8.52, 9.02) | 1.80 | 3.64 | (−1.84, 5.44) |
| Regression of slope on PWD physical functioning |
−0.22* | 0.08 | (−0.37, −0.08) | −0.16* | 0.07 | (−0.33, −0.05) |
| Non-spousal caregivers, n=595 | ||||||
| Residual baseline covariance | −0.75* | 0.60 | (−1.35, −0.16) | 4.73* | 0.38 | (4.35, 5.11) |
| Regression of slope on PWD physical functioning |
−0.24* | 0.08 | (−0.40, −0.08) | −0.08 | 0.09 | (−0.27, 0.09) |
p<0.05, PWD = persons with dementia
Note: The first row under each subgroup presents associations of the intercept of the summary physical functioning factor of persons with dementia with the intercepts for negative caregiving aspects. The second row under each subgroup presents regressions of rate of change for each negative aspect of caregiving on the baseline physical functioning factor of persons with dementia. For factor scores representing physical functioning of persons with dementia, caregiver burden, and caregiver depressive symptoms, higher scores indicate greater impairment, more burden, and more depressive symptoms, respectively.
Associations by race of caregivers
At baseline, more impaired physical functioning in persons with dementia was associated with more depressive symptoms (β=4.21, 95% CI: 0.83, 7.59) among non-white caregivers (Table 4). Greater impairment in physical functioning of persons with dementia was associated with slower worsening in caregiver burden among both non-white (β=−0.14, 95% CI: −0.28, −0.01) and white (β=−0.27, 95% CI: −0.40, −0.14) caregivers, as well as with changes in depressive symptoms in white caregivers (β=−0.12, 95% CI: −0.24, −0.02) (Table 4).
Table 4.
Associations of Summary Physical Functioning Factor of Persons with Dementia and Negative Caregiving Aspects by Caregiver Race (N=1,211)
| Parameter | Caregiver burden | Depressive symptoms of the caregiver |
||||
|---|---|---|---|---|---|---|
| Estimate | Standard Error |
95% Confidence Interval |
Estimate | Standard Error |
95% Confidence Interval |
|
| Non-white Caregivers (n=481) | ||||||
| Residual baseline covariance | 1.84 | 1.89 | (−0.04, 3.73) | 4.21* | 3.38 | (0.83, 7.59) |
| Regression of slope on PWD physical functioning |
−0.14* | 0.07 | (−0.28, −0.01) | −0.04 | 0.10 | (−0.22, 0.18) |
| White Caregivers (n=730) | ||||||
| Residual baseline covariance | 2.63 | 5.45 | (−2.82, 8.08) | −0.09 | 0.85 | (−0.94, 0.75) |
| Regression of slope on PWD physical functioning |
−0.27* | 0.07 | (−0.40, −0.14) | −0.12* | 0.06 | (−0.24, −0.02) |
p<0.05, PWD = persons with dementia
Note: The first row under each subgroup presents associations of the intercept of the summary physical functioning factor of persons with dementia with the intercepts for negative caregiving aspects. The second row under each subgroup presents regressions of rate of change for each negative aspect of caregiving on the baseline physical functioning factor of persons with dementia. For factor scores representing physical functioning of persons with dementia, caregiver burden, and caregiver depressive symptoms, higher scores indicate greater impairment, more burden, and more depressive symptoms, respectively.
Sensitivity analyses
Excluding one dataset at a time from the pooled analysis yielded results similar to Table 2 (Supplementary Table 2). One notable except was that after excluding REACH II, there was an inverse association between baseline physical functioning of persons with dementia and change in caregiver depressive symptoms.
Associations by age group of physical functioning with caregiver burden and depressive symptoms among caregivers followed a similar pattern as for associations by spousal status (Supplementary Table 3).
Among participants in control groups, associations between physical functioning and rates of change in caregiver burden and depressive symptoms were similar (Supplementary Table 4). Several baseline associations varied in magnitude while a few differed in direction, but we did not consider them meaningfully different, since 95% confidence intervals overlapped with 0. Specifically, among non-white caregivers from control groups, more impaired physical functioning of persons with dementia was associated with greater caregiver burden (β=4.53, 95% CI: 1.21, 7.85) at baseline, but more impaired physical functioning of persons with dementias was no longer associated with slower worsening of caregiver burden (β=−0.27, 95% CI: −0.51, 0.03), although the direction was similar to that of the main finding. Among white caregivers from control groups, more impaired physical functioning of persons with dementia was associated with decreases in depressive symptoms (β=−10.51, 95% CI: −13.20, −7.82) at baseline, but not with slower worsening of depressive symptoms (β=−0.09, 95% CI: −0.25, 0.10). Among spousal caregivers from control groups, more impaired physical functioning of persons with dementia was no longer associated with greater caregiver burden at baseline (β=1.06, 95% CI: −0.84, 2.96). More impaired physical functioning of persons with dementia was associated with decreases in depressive symptoms (β=−6.80, 95% CI: −7.56, −6.03), but not with slower worsening of depressive symptoms (β=−0.14, 95% CI: −0.38, 0.03). Among non-spousal caregivers from control groups, more impaired physical functioning of persons with dementia was no longer associated with slower worsening in caregiver burden (β=−0.24, 95% CI: −0.54, 0.12), although the direction remained the same as that of the main finding.
Discussion
In this integrative data analysis of four behavioral intervention trials of support for dementia caregivers seeking intervention, we sought to characterize associations between levels of impairment in physical functioning of persons with dementia and measures of caregiver burden and depressive symptoms among their caregivers. The overall findings suggest effects of physical functioning of persons with dementia on their caregivers are associated with both increased caregiver burden and general depressive symptoms. Associations of physical functioning impairment with rates of change in caregiver burden and with depressive symptoms were present but not consistent overall and by group.
Associations at baseline of physical functioning impairment of persons with dementia and elevated caregiver burden are consistent with other studies. Given et al. (1993) reported that caregivers feel burdened when care demands increase. In our study, worse physical functioning of persons with dementia at baseline was associated with less worsening in caregiver burden. This pattern suggests that caregivers of persons with dementia grow to cope with the demands of caregiving as the person with dementia becomes more physically impaired (Sherwood, Given, Given, & Eye, 2005). Alternatively, increased physical impairment may lead dementia caregivers to seek more support in caregiving, i.e., from family, friends, and support groups, thereby leading to less worsening in caregiver burden.
We examined the effects of caregiver relationship and race on the association of the levels of physical impairment of persons with dementia with caregiver burden and general depressive symptoms. Among spousal caregivers, more impaired physical functioning was associated with more caregiver burden among spousal caregivers but less caregiver burden among non-spousal caregivers at baseline. The association with caregiver burden did not differ by race of a caregiver. Pinquart and Sörensen (2003) reported that spousal caregivers tend to have fewer financial, physical, and psychological resources, as well as fewer stress-buffering roles and activities. Contributing to increased perceptions of burden, older caregivers also may be less likely than younger caregivers to use formal support such as nursing assistants (Hooker, Monahan, Bowman, Frazier, & Shifren, 1998).
Baseline levels of impairment in physical functioning of persons with dementia led to less worsening of depressive symptoms particularly among spousal and white caregivers. This finding suggests that spousal and white caregivers may adjust to the level of impairment. Among both non-spousal and non-white caregivers, level of impairment in physical functioning of persons with dementia was associated with increased depressive symptoms, which mirrors the main findings.
There are several strengths of this study. Strengths of composite factors derived from item response theory (IRT) include greater sensitivity to differences in physical functioning of persons with dementia and caregiver characteristics and greater precision, as compared to individual scales for ADLs, IADLs, depressive symptoms, and caregiver burden (Armstrong et al., 2017; Gross et al., 2014). Individual scales use their own scale for measurement, and it is difficult to relate these measures to others on a common underlying continuum. Moreover, larger sample sizes in the pooled sample facilitated stratified analyses by caregiver demographic characteristics, which would not have been feasible in any of the individual datasets with the same level of statistical power. Additionally, while many studies of the association between physical functioning in people with dementia and aspects of caregiving have been cross-sectional in design, we examined longitudinal relationships between physical functioning of persons with dementia and negative aspects of caregiving. Lastly, the results of main analysis with random assignment adjustment were similar to those when restricting the sample to only those in the control arm of intervention trials. This suggests that the intervention did not affect the direction of the relationship between physical functioning of persons with dementia and caregiver characteristics.
This study has limitations. First, the length of follow-up in all behavioral intervention studies was less than one year and although we had more than two timepoints on average for most people, there may not have been enough time to observe longitudinal associations between physical functioning of persons with dementia and changes in outcomes. Second, physical functioning of persons with dementia was reported by the caregiver, which may result in same source bias when examining caregiver characteristics such as caregiver burden and depressive symptoms. A third limitation is that the pooled sample in this study came from convenience samples of caregivers who may report more physical health conditions and depressive symptoms, as compared to non-caregivers (Pinquart & Sörensen, 2003; Pruchno et al., 2008). Fourth, a potential limitation is undue influence from a single study. We conducted sensitivity analyses to see if our results were affected by one or more datasets. When excluding REACH II data, there was an inverse association of level of physical impairment of persons with dementia with depressive symptoms. Since REACH II contributed 53.0% of the overall sample, this dataset was influential on this association. Additionally, depressive symptoms in each study were measured using different versions of the CES-D. We were able to use item-level data to derive a continuum for depressive symptoms to address this limitation. Finally, regional differences may affect some findings; most of the sample is from randomized trials conducted in one Northeastern U.S. city.
Our findings from this study that integrated data across four intervention studies suggest that efforts to assist dementia caregivers to meet the physical impairment needs of the persons with dementia should be focused particularly among older, spousal caregivers. In this study, we found overall that greater physical functioning impairment was associated with greater caregiver burden and more depressive symptoms. While not entirely surprising, this finding underscores the importance of physical functioning for negative aspects of caregiving. When we stratified by caregiver relationship and race, much of the baseline association between physical functioning impairment and caregiver burden is due to spousal caregivers. Much of the baseline association between physical functioning impairment and caregiver depressive symptoms, however, is attributable to non-spousal and non-white caregivers. This pattern of results is consistent with the hypothesis that different groups of caregivers may report burden and others may experience depression, but not all caregivers in a given sample will necessarily have difficulties with both despite worsen impairment of persons with dementia for whom they are caring.
Supplementary Material
Acknowledgments
Funding: This work was supported by a Pilot Award from the Johns Hopkins Center for Innovative Care in Aging, School of Nursing (PI: Gross) and T32AG000247 (Epidemiology and Biostatistics of Aging Training Program, Johns Hopkins Center on Aging and Health) (Armstrong). ACT was funded by the National Institute on Aging and the National Institute on Nursing Research (Grant Number: R01AG22254). COPE was funded by the Pennsylvania Department of Health and Tobacco Funds (Grant Number: SAP#41000272). REACH II was funded by the National Institute on Aging and the National Institute on Nursing Research (AG13305, AG13289, AG13313, AG20277, AG13265, NR004261). TAP was funded by the National Institute of Mental Health (Grant Number: R21MH069425). The contents do not necessarily represent views of the funding entities. Funders had no deciding roles in the design and conduct of the study.
Footnotes
Conflicts of Interest: The authors report no conflicts of interest.
References
- Alzheimer’s Association. (2016). 2016 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia, 12(4), 459–509. 10.1016/j.jalz.2016.03.001 [DOI] [PubMed] [Google Scholar]
- Armstrong NM, Gitlin LN, Parisi JM, Carlson MC, Rebok GW, & Gross AL (2017).E pluribus unum: harmonization of physical functioning across intervention studies of older adults. PLoS One 12(7): e0181746 10.1371/journal.pone.0181746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bédard M, Molloy DW, Squire L, Dubois S, Lever JA, & O’Donnell M (2001). The Zarit Burden interview: a new short version and screening version. The Gerontologist, 41(5), 652–657. 10.1093/geront/41.5.652 [DOI] [PubMed] [Google Scholar]
- Beeson RA (2003). Loneliness and depression in spousal caregivers of those with Alzheimer’s disease versus non-caregiving spouses. Archives of Psychiatric Nursing, 17(3), 135–143. 10.1016/S0883-9417(03)00057-8 [DOI] [PubMed] [Google Scholar]
- Belle SH, Burgio L, Burns R, Coon D, Czaja SJ, Gallagher-Thompson D, . . . Resources for Enhancing Alzheimer’s Caregiver Health (REACH) II Investigators. (2006). Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: a randomized, controlled trial. Annals of Internal Medicine, 145(10), 727–738. 10.7326/0003-4819-145-10-200611210-00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell CM, & Gibson GD (1997). Racial, ethnic, and cultural differences in dementia caregiving: review and analysis. The Gerontologist, 37(3), 355–364. 10.1093/geront/37.3.355 [DOI] [PubMed] [Google Scholar]
- Connell CM, Janevic MR, & Gallant MP (2001). The costs of caring: impact of dementia on family caregivers. Journal of Geriatric Psychiatry and Neurology,14(4), 179–187. 10.1177/089198870101400403 [DOI] [PubMed] [Google Scholar]
- Dilworth-Anderson P, Brummett BH, Goodwin P, Williams SW, Williams RB, & Siegler IC (2005). Effect of race on cultural justifications for caregiving. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 60, S257–S262. 10.1093/geronb/60.5.S257. [DOI] [PubMed] [Google Scholar]
- Dracup K, Westlake C, Erickson VS, Moser DK, Caldwell ML, & Hamilton MA (2003). Perceived control reduces emotional stress in patients with heart failure. The Journal of Heart and Lung Transplant, 22(1), 90–93. 10.1016/S1053-2498(02)00454-0 [DOI] [PubMed] [Google Scholar]
- Eloniemi-Sulkava U, Notkola I, Hämäläinen K, Rahkonen T, Viramo P, Hentinen M, Sulkava R (2002). Spouse caregivers’ perceptions of influence of dementia on marriage. International Psychogeriatrics, 14(01), 47–58. 10.1017/S104161020200827X [DOI] [PubMed] [Google Scholar]
- Gallagher-Thompson D, Dal Canto PG, Jacob T, & Thompson LW (2001). A comparison of marital interaction patterns between couples in which the husband does or does not have Alzheimer’s disease. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 56(3), S140–S150. 10.1093/geronb/56.3.S140 [DOI] [PubMed] [Google Scholar]
- Gitlin LN, Winter L, Dennis MP, Corcoran M, Schinfeld S, & Hauck WW (2006). A randomized trial of a multi-component home intervention to reduce functional difficulties in older adults. Journal of the American Geriatrics Society, 54(5), 809–816. 10.1111/j.1532-5415.2006.00703.x [DOI] [PubMed] [Google Scholar]
- Gitlin LN, Winter L, Dennis MP, Hodgson H, & Hauck WW (2010). A biobehavioral home-based intervention and the well-being of patients with dementia and their caregivers: the COPE randomized trial. JAMA, 304(9), 983–991. 10.1001/jama.2010.1253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gitlin LN, Winter L, Earland TV, Herge EA, Chernett NL, Piersol CV, & Burke JP (2009). The Tailored Activity Program to reduce behavioral symptoms in individuals with dementia: feasibility, acceptability, and replication potential. The Gerontologist, 49(3), 428–439. 10.1093/geront/gnp087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Given C, Stommel M, Given B, Osuch J, Kurtz M, & Kurtz J (1993). The influence of cancer patients’ symptoms and functional states on patients’ depression and family caregivers’ reaction and depression. Health Psychology, 12(4), 277–285. 10.1037/0278-6133.12.4.277 [DOI] [PubMed] [Google Scholar]
- Glymour MM, & Manly JJ (2008). Lifecourse social conditions and racial and ethnic patterns of cognitive aging. Neuropsychology Review, 18(3), 223–254. [DOI] [PubMed] [Google Scholar]
- Gross AL, Jones RN, & Inouye SK (2014). Development of an expanded measure of physical functioning for older persons in epidemiologic research. Research on Aging, 37(7), 671–694. 10.1177/0164027514550834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haley WE, Roth DL, Coleton MI, Ford GR, West CA, Colllins RP, & Isobe TL (1996). Appraisal, coping, and social support as mediators of well-being in black and white family caregivers of patients with Alzheimer’s disease. Journal of Consulting and Clinical Psychology, 64(1), 121 10.1037/0022-006X.64.1.121 [DOI] [PubMed] [Google Scholar]
- Hebert LE, Weuve J, Scherr PA, & Evans DA (2013). Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology, 80(19), 1778–1783. 10.1212/WNL.0b013e31828726f5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooker K, Monahan DJ, Bowman SR, Frazier LD, & Shifren K (1998). Personality counts for a lot: Predictors of mental and physical health of spouse caregivers in two disease groups. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 53(2), P73–P85. 10.1093/geronb/53B.2.P73 [DOI] [PubMed] [Google Scholar]
- Hooker K, Bowman SR, Coehlo DP, Lim SR, Kaye J, Guariglia R, & Li F (2002). Behavioral change in persons with dementia: relationships with mental and physical health of caregivers. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 57(5), P453–P460. [DOI] [PubMed] [Google Scholar]
- Janevic MR, & Connell CM (2001). Racial, ethnic, and cultural differences in the dementia caregiving experience: recent findings. The Gerontologist, 41(3), 334–347. 10.1093/geront/41.3.334 [DOI] [PubMed] [Google Scholar]
- Kasper JD, Freedman VA, Spillman BC, & Wolff JL (2015). The disproportionate impact of dementia on family and unpaid caregiving to older adults. Health Affairs, 34(10), 1642–1649. 10.1377/hlthaff.2015.0536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King RB, Hartke RJ, & Houle TT (2010). Patterns of relationships between background characteristics, coping, and stroke caregiver outcomes. Topics in Stroke Rehabilitation, 17(4), 308–317. 10.1310/tsr1704-308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight BG, Robinson GS, Longmire CVF, Chun M, Nakao K, & Kim JH (2002). Cross-cultural issues in caregiving for persons with dementia: do familism values reduce burden and distress? Aging International, 27, 70–95. 10.1007/s12126-003-1003-y [DOI] [Google Scholar]
- Lee M, & Kolomer SR (2005). Caregiver burden, dementia, and elder abuse in South Korea. Journal of Elder Abuse & Neglect, 17, 61–74. 10.1300/J084v17n01_04 [DOI] [PubMed] [Google Scholar]
- Mendez-Luck C, Kennedy D, & Wallace S (2008). Concepts of burden in giving care to older relatives: a study of female caregivers in Mexico City neighbourhood. Journal of Crosscultural Gerontology, 23, 265–282. 10.1007/s10823-008-9058-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moser DK, & Dracup K (1995). Psychosocial recovery from a cardiac event: the influence of perceived control. Heart & Lung: The Journal of Acute and Critical Care, 24(4), 273–280. 10.1016/S0147-9563(05)80070-6 [DOI] [PubMed] [Google Scholar]
- Narayan S, Lewis M, Tornatore J, Hepburn K, & Corcoran-Perry S (2001). Subjective responses to caregiving for a spouse with dementia. Journal of Gerontological Nursing, 27(3), 19–28. 10.3928/0098-9134-20010301-05 [DOI] [PubMed] [Google Scholar]
- National Alliance for Caregiving & AARP Public Policy Institute. Caregiving in the U.S 2015. Retrieved May 3, 2017, from http://www.aarp.org/content/dam/aarp/ppi/2015/caregivers-of-older-adults-focused-look.pdf
- Nordahl H, Hvidtfeldt UA, Diderichsen F, Rod NH, Osler M, Frederiksen BL, Andersen I (2014). Cohort profile: the social inequality in cancer (SIC) cohort study. International Journal of Epidemiology, 43(6), 1750–1758. 10.1093/ije/dyu003 [DOI] [PubMed] [Google Scholar]
- Ory MG, Hoffman RR, Yee JL, Tennstedt S, & Schulz R (1999). Prevalence and impact of caregiving: a detailed comparison between dementia and nondementia caregivers. The Gerontologist, 39(2), 177–186. 10.1093/geront/39.2.177 [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, & Skaff MM (1990). Caregiving and the stress process: an overview of concepts and their measures. The Gerontologist, 30(5), 583–594. 10.1093/geront/30.5.583 [DOI] [PubMed] [Google Scholar]
- Pinquart M, & Sörensen S (2003). Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychology and Aging, 18(2), 250 10.1037/0882-7974.18.2.250 [DOI] [PubMed] [Google Scholar]
- Pinquart M, & Sörensen S (2005). Ethnic differences in stressors, resources, and psychological outcomes of family caregiving: a meta-analysis. The Gerontologist, 45(1), 90–106. 10.1093/geront/45.1.90 [DOI] [PubMed] [Google Scholar]
- Pruchno RA, Brill JE, Shands Y, Gordon JR, Genderson MW, Rose M, & Cartwright F (2008). Convenience samples and caregiving research: how generalizable are the findings? The Gerontologist, 48(6), 820–827. DOI: 10.1093/geront/48.6.820 [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Reid J, & Hardy M (1999). Multiple roles and well-being among midlife women: testing role strain and role enhancement theories. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 54(6), S329–S338. 10.1093/geronb/54B.6.S329 [DOI] [PubMed] [Google Scholar]
- Roth DL, Dilworth-Anderson P, Huang J, Gross AL, & Gitlin LN (2015). Positive aspects of family caregiving for dementia: differential item functioning by race. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 70(6), 813–819. 10.1093/geronb/gbv034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth DL, Fredman L, & Haley WE (2015). Informal caregiving and its impact on health: a reappraisal from population-based studies. The Gerontologist, 55(2), 309–319. 10.1093/geront/gnu177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samejima F (1969). Estimation of latent ability using a response pattern of graded scores. Psychometrika monograph supplement 10.1007/BF02290599 [DOI]
- Schneider J, Murray J, Banerjee S, & Mann A (1999). EUROCARE: a cross‐national study of co‐resident spouse carers for people with Alzheimer’s disease: I—factors associated with carer burden. International Journal of Geriatric Psychiatry, 14(8), 651–661. [DOI] [PubMed] [Google Scholar]
- Schulz R, McGinnis K, Zhang S, et al. Dementia patient suffering and caregiver depression. Alzheimer Disease and Associated Disorders 2008;22(2):170–176. 10.1097/WAD.0b013e31816653cc [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherwood PR, Given CW, Given BA, & von Eye A (2005). Caregiver burden and depressive symptoms: analysis of common outcomes in caregivers of elderly patients. Journal of Aging and Health, 17(2), 125–147. 10.1177/0898264304274179 [DOI] [PubMed] [Google Scholar]
- Stephens MAP, Franks MM, & Townsend AL (1994). Stress and rewards in women’s multiple roles: the case of women in the middle. Psychology and Aging, 9(1), 45–52. 10.1037/0882-7974.9.1.45 [DOI] [PubMed] [Google Scholar]
- Välimäki TH, Martikainen JA, Hallikainen IT, Väätäinen ST, & Koivisto AM (2015). Depressed spousal caregivers have psychological stress unrelated to the progression of Alzheimer disease: a 3-year follow-up report, Kuopio ALSOVA Study. Journal of Geriatric Psychiatry and Neurology, 28(4), 272–280. 10.1177/0891988715598229 [DOI] [PubMed] [Google Scholar]
- Zarit SH, Orr NK, & Zarit JM (1985). The Hidden Victims of Alzheimer’s Disease: Families under Stress New York, NY: New York University Press; 10.1093/hsw/12.3.236 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


