Abstract
The goal of this study was to genotypically characterize extended-spectrum β-lactamase-producing Escherichia coli isolates from the western region of Saudi Arabia and to identify active antibiotics against these isolates using phenotypic and molecular modeling. In total, 211 ESBL-producing E. coli isolates recovered from heterogeneous clinical specimens were identified by MALDI-TOF. Thirty-two sequence types (STs) were identified from a multilocus sequence typing (MLST) analysis of ESBL-producing E. coli, including a novel ST (ST8162). The most common ST in the Saudi and expatriate population was ST131, followed by ST38. All the isolates were multidrug resistant (MDR), and >95% of the isolates were resistant to third-generation (ceftriaxone and ceftazidime) and fourth-generation (cefepime) cephalosporins. The ESBL-positive E. coli isolates primarily harbored the blaCTX-M and blaTEM genes. No resistance was observed against the carbapenem antibiotic group. All the ESBL-producing E. coli isolates were observed to be susceptible to a ceftazidime/avibactam combination. Molecular interaction analyses of the docked complexes revealed the amino acid residues crucial for the binding of antibiotics and inhibitors to the modeled CTX-M-15 enzyme. Importantly, avibactam displayed the most robust interaction with CTX-M-15 among the tested inhibitors in the docked state (∆G = −6.6 kcal/mol). The binding free energy values for clavulanate, tazobactam and sulbactam were determined to be −5.7, −5.9 and −5.2 kcal/mol, respectively. Overall, the study concludes that ‘ceftazidime along with avibactam’ should be carefully used as a treatment option against only carbapenem-resistant MDR ESBL-producing E. coli in this region.
Introduction
Antimicrobial resistance is indiscriminate and is growing across different bacterial groups and against all antibiotic classes, impacting every region and country in the world. Particularly in the present infectious disease era, multidrug-resistant Gram-negative bacteria are a major therapeutic challenge in both hospital1,2 and community settings3,4. Out of 6 ESKAPE pathogens (recognized as particularly troubling), four are Gram-negative bacteria5. Thus, the attention of the scientific community has shifted to studying antibiotic-resistant Gram-negative bacteria6. Members of the family Enterobacteriaceae commonly produce extended-spectrum β-lactamases (ESBLs) that confer resistance to the advanced generation of cephalosporins and may lead to therapeutic dead ends. ESBLs are of great concern because they are often plasmid-associated. These plasmids often carry antimicrobial resistance genes for other antibiotics, such as fluoroquinolones, aminoglycosides, tetracyclines, sulfamethoxazole-trimethoprim and chloramphenicol. Importantly, there is a potential risk of cross-species dissemination of these plasmids, resulting in multiple antibiotic resistance genes being spread to different bacterial species7. Infections from extended-spectrum β-lactamase-producing E. coli are often preceded by asymptomatic carriage8. Moreover, hospital acquired infections due to ESBL-producing E. coli are common, and several nosocomial outbreaks have been reported in different geographical regions9. Recently, several studies from Saudi Arabia have reported the ESBL-producing Enterobacteriaceae Klebsiella pneumoniae and E. coli, primarily from Riyadh10,11. However, very limited data are available regarding the genetic background and clonal type of invasive E. coli from this region.
With respect to ESBLs, blaCTX-M have become the most commonly detected ESBL genotype in different geographical locations worldwide12. In a recent study, Bindayna et al. identified blaCTX-M as the predominant genotype among ESBL-producing bacteria in Saudi Arabia13. The change in the enzymatic activities of blaCTX-M that have led to the evolution of additional variants may be due to point mutations within or outside the active site omega loop, i.e., amino acid positions 161 to 17914. Identification of the amino acid residues that are crucial to the interaction between blaCTX-M variants (the enzymes produced by resistant bacteria) and target drugs (the drug hydrolyzed by these bacterial enzymes) is a problem of deep scientific interest. Information on this subject would be useful for the development of blaCTX-M-resistant antibiotics in the future. Variants of this bacterial enzyme are emerging at a fast pace. Up to 172 blaCTX-M variants have already been reported (http://www.lahey.org/studies/other.asp#table1; accessed on 27/03/2018). Thus, there is an urgent need to design a versatile blaCTX-M inhibitor that can inhibit most of the emerging variants of this enzyme, if not all. Moreover, continuous surveillance is needed because the evolution of newer blaCTX-M enzyme variants with altered and expanded substrate (antibiotic) profiles has now become an everyday phenomenon15.
In this study, ESBL-producing E. coli isolates collected from one of the major territory hospitals of the King Abdulaziz University, which serves Jeddah and the peripheral area, were screened for antimicrobial susceptibility and blaCTX-M genotypes. A multilocus sequence typing (MLST) analysis was performed to identify the common sequence types (STs) of ESBL-producing E. coli circulating in this region, as approximately half of the population are expatriates from developing countries in addition to natives of Jeddah, which is the primary entry point for 30 million pilgrims every year from all over the world. In addition, modeling studies were performed to allow the best therapy against blaCTX-M-producing bacteria to be suggested to local health care facilities.
Results
Demographic and Clinical Data Analysis
A total of 211 nonduplicate ESBL-producing E. coli clinical isolates that were collected during 2014–2015 and identified by MALDI-TOF were characterized in this study. The isolates were obtained at a relatively highly percentage from inpatients (75.4%) followed by outpatients (24.6%). No significant difference (p > 0.05) was observed in the gender of patients, with 115 (54.5%) and 96 (45.5%) being female and male, respectively (Table 1). The average age of the patients was 48 years, ranging from 0.1–96 years with a median age of 55 years. A relatively higher percentage of isolates was obtained from patients older than 50 years of age (54.9%), among whom 85 were inpatients (55.6%). Importantly, 10% of the ESBL-producing E. coil isolates were from neonates <1 year of age (Table 1). The strains were primarily isolated from Saudi patients (42.7%), as well as Yemeni (22.7%), Sudanese (6.2%), Palestinian (4.7%) and Pakistani (4.7%) expatriates, with the remaining 13.3% isolates recovered from patients of 13 other nationalities. The strains were cultured from heterogeneous clinical specimens, mostly from urine (36.5%) and urine catheters (27.9%), followed by wound swabs (10.4%) and blood samples (9%) (Table 1). The results of a chi-square test revealed an association between patient and specimen types (p = 0.001).
Table 1.
Distribution of ESBL-positive E. coli isolates according to demographic and clinical data.
| Source | Total No. | Inp n = 159 (75.4%) | Outp n = 52 (24.6%) | p-value | HA n = 88 (41.7%) | CA n = 123 (58.3%) | p-value | |
|---|---|---|---|---|---|---|---|---|
| Gender | Male | 96 | 83 (52.2) | 13 (25.0) | 0.001 | 46 (52.3) | 50 (40.7) | 0.095 |
| Female | 115 | 76 (47.8) | 39 (75.0) | 42 (47.7) | 73 (59.3) | |||
| Age | ≤1 | 21 | 20 (12.6) | 1 (1.9) | 0.015 | 11 (12.5) | 10 (8.6) | 0.438 |
| 2–11 | 14 | 11 (6.9) | 3 (5.8) | 5 (5.7) | 9 (7.3) | |||
| 12–18 | 2 | 1 (0.6) | 1 (1.9) | 0 | 2 (1.6) | |||
| 19–50 | 58 | 36 (22.6) | 22 (42.3) | 22 (25.0) | 36 (29.3) | |||
| >50 | 116 | 91 (57.2) | 25 (48.1) | 50 (56.8) | 66 (53.7) | |||
| Nationality | Saudi | 90 | 65 (40.9) | 25 (48.1) | 0.057 | 40 (45.5) | 50 (40.7) | 0.227 |
| Yemeni | 48 | 34 (21.4) | 14 (26.9) | 17 (19.3) | 31 (25.2) | |||
| Sudanese | 13 | 13 (8.2) | 0 | 7 (8.0) | 6 (4.9) | |||
| Palestinian | 10 | 7 (4.4) | 3 (5.8) | 2 (2.3) | 8 (6.5) | |||
| Pakistani | 10 | 9 (5.7) | 1 (1.9) | 6 (6.8) | 4 (3.3) | |||
| Ethiopian | 6 | 4 (2.5) | 2 (3.8) | 3 (3.4) | 3 (2.4) | |||
| Somalian | 6 | 6 (3.8) | 0 | 3 (3.4) | 3 (2.4) | |||
| Others | 28 | 21 (13.2) | 7 (13.5) | 17 (19.3) | 24 (19.5) | |||
| Specimens Type | Urine-midstream | 77 | 40 (25.1) | 37 (71.2) | 0.001 | 27 (30.7) | 50 (40.7) | 0.034 |
| Urine-catheter | 59 | 50 (31.4) | 9 (17.3) | 19 (21.6) | 40 (32.5) | |||
| Wound swab | 22 | 20 (12.6) | 2 (3.8) | 14 (15.9) | 8 (6.5) | |||
| Blood | 19 | 18 (11.3) | 1 (1.9) | 9 (10.2) | 10 (8.1) | |||
| Others | 34 | 31 (19.5) | 3 (5.8) | 29 (33.0) | 15 (12.2) |
Inp, Inpatient; Outp, Outpatient; HA, Hospital acquired; CA, Community acquired.
The majority of the ESBL-positive E. coli infections were of community-onset (58.3%), and 41.7% were likely nosocomial infections acquired by the patients during three-day admissions in different hospital units; such infections were primarily identified from patients in male and female medical and surgical wards and pediatric wards. Among the patients with nosocomial infections, 25.6% were cancer patients. ESBL-positive E. coli isolates from nosocomial infections were primarily identified from midstream urine samples (30.7%), urine catheters (21.6%) and wound swabs (15.9%) (Table 1). The community-onset patients were primarily outpatients (42.3%) from the emergency room (26.8%). In more than 85% of patients, an ESBL-positive E. coli infection was not the primary diseases. Among these patients, ESBL positive E. coli were primarily isolated from the malignancy, sepsis, urinary tract infection (UTI) and other renal diseases of patients (Supplementary Fig. S1).
Antimicrobial Susceptibility Analysis
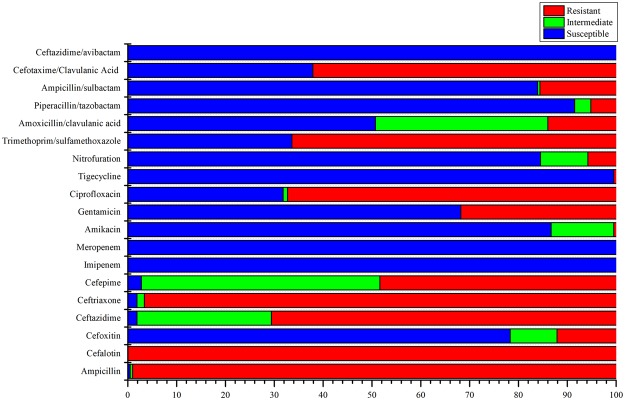
All of the tested E. coli isolates were determined to be multidrug resistant (MDR), and >60% isolates were revealed as extensively drug-resistant (XDR). None of the isolates were recorded as pan-drug resistant (PDR) in this study. In total, 97.6% of isolates were resistant to ≥5 of the tested antibiotics. Among them, 16 isolates were resistant to ≥10 antibiotics. The isolates Ec51 and Ec128, which were recovered from urine catheter and blood samples from Pakistani and Sudanese sepsis patients, respectively, were resistant to the 12 tested antibiotics. Ampicillin resistance was detected in the 99.5% of isolates, with observed MICs of ≥32 µg/ml (Fig. 1). All the tested isolates were resistant to the first-generation cephalosporin cefalotin (8 to ≥64 µg/ml), while >95% of isolates were resistant or intermediately resistant to ceftriaxone, ceftazidime and cefepime. Only 21.3% isolates were resistant or intermediately resistant to the second-generation cephalosporin cefoxitin, with observed MICs of 16–64 µg/ml. All the isolates were susceptible to carbapenem antibiotics (imipenem and meropenem). Other than β-lactam antibiotics, the highest resistance was observed against ciprofloxacin (68.2%) and trimethoprim/sulfamethoxazole (66.4%), with observed MICs of ≥4 and ≥320 µg/ml, respectively (Fig. 1). The lowest antibiotic resistance was observed against amikacin and nitrofurantoin. One ESBL-positive E. coli isolate was resistant to tigecycline, with an MIC of ≥8 µg/ml. No specific association was observed among the disease types and resistances to particular antibiotics in the ESBL-producing E. coli isolates. However, resistance to trimethoprim/sulfamethoxazole was increased to 79% in the cancer patients. In total, 70 different patterns of antibiotic resistance were observed in the 211 isolates, which included 30 groups and 40 unique patterns. The dominant antibiotype pattern (P1) was observed for 26 ESBL-positive E. coli isolates that exhibited resistance to 7 antibiotics and sensitivity to 9 antibiotics (Supplementary Fig. S2). The second antibiotype pattern (P2) was identified in 17 isolates that were resistant to 5 antibiotics and susceptible to 11 antibiotics. The third antibiotype pattern (P3) was identified in 15 isolates that were resistant to 9 antibiotics (Supplementary Fig. S2). The dominant antibiotypes were primarily identified in the inpatients from the >50 years old age group. The other antibiotype patterns were observed in ≤10 isolates. Most importantly, all the ESBL-producing E. coli isolates were determined to be susceptible to the ceftazidime/avibactam combination (Fig. 1).
Figure 1.
Antimicrobial resistance and sensitivity profile of the tested antibiotics among the studied ESBL-positive E. coli isolates. The x-axis values are expressed in percentage.
β-lactamase Resistance Genes Genotyping
The ESBL-positive E. coli isolates primarily harbored the blaCTX-M (95.3%) and blaTEM (83.9%) genes. The blaOXA and blaSHV genes were only detected in 6.6 and 5.2% isolates, respectively (Supplementary Fig. S3). In total, 82.5% isolates carried more than one β-lactamase gene. The combination of blaCTX-M and blaTEM (79.1%) was frequently observed in the ESBL-positive E. coli isolates. The combination of blaCTX-M, blaTEM and blaSHV was observed in only 2.4% of isolates. The blaCTX-M isolates primarily belonged to the group blaCTX-M-1 (74.6%), followed by blaCTX-M-9 (20.4%). The groups blaCTX-M-8/25 and blaCTX-M-2 were detected only in 2.5 and 1.5% of isolates respectively.
MLST Analysis and Identification of Clonal Complex Groups
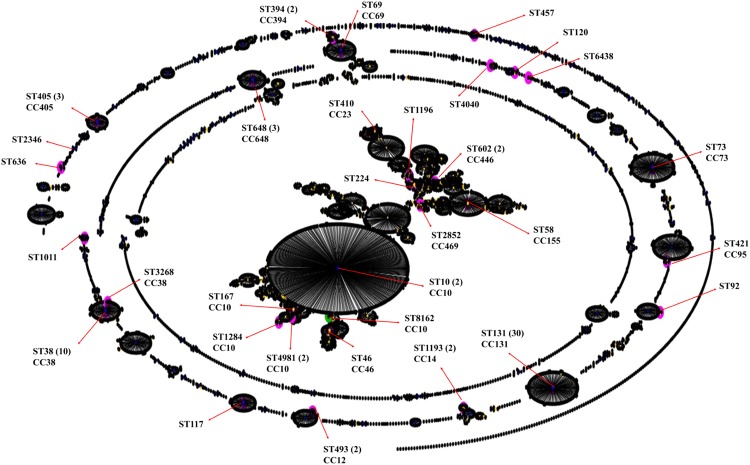
ERIC-PCR produced varying amplification products according to molecular weights observed by gel electrophoresis. The amplicons were between 150 and 7,000 bp, with multiple bands (between 2 to 12 bands) observed for each isolate (Supplementary Fig. S4). The isolates were divided to 80 clusters at distance of 0.5, and a representative isolate from each clade was processed for MLST. Overall, 32 unique STs were detected among the 80 isolates using the allelic profile of the seven housekeeping genes, including a novel ST8162 (Fig. 2). In addition, 16 E. coli STs were identified in this study that were not previously reported from Saudi Arabia. The predominant ST identified was ST131 (37.5%, n = 30), followed by ST38 (12.5%, n = 10). Other identified STs were detected in ≤3 of ESBL-positive E. coli isolates, while 22 identified STs were comprised of a single isolate. eBURST resolve the 32 unique allelic profiles of the isolates into 3 groups and 26 singletons with a single locus variant and 4 groups and 20 singletons with a double locus variant (Fig. 3). In contrast, the BLAST analysis with the EnteroBase database grouped the 32 STs into 14 clonal complexes (CC), including the major CCs CC131 and CC38. The allelic profiles of 6 STs linked with 4 different CCs with a single locus variant, such as ST4981, ST1284 and ST8162, which were linked with CC10 with a single locus variant. The allelic profile of the 11 STs were identified as singletons.
Figure 2.
Regional distribution of E. coli STs detected in Saudi Arabia. The blue labeled STs from Jeddah were detected in this study. *Indicates the STs were previously recovered from food samples and their location in Saudi Arabia was not reported. The map in the figure was obtained from Map data@2018 Google.
Figure 3.
eBURST analysis of multilocus sequence typed ESBL-positive E. coli isolates. The pink nodes indicate the STs detected in this study that were present in the MLST database. The green node indicates the novel ST detected in this study.
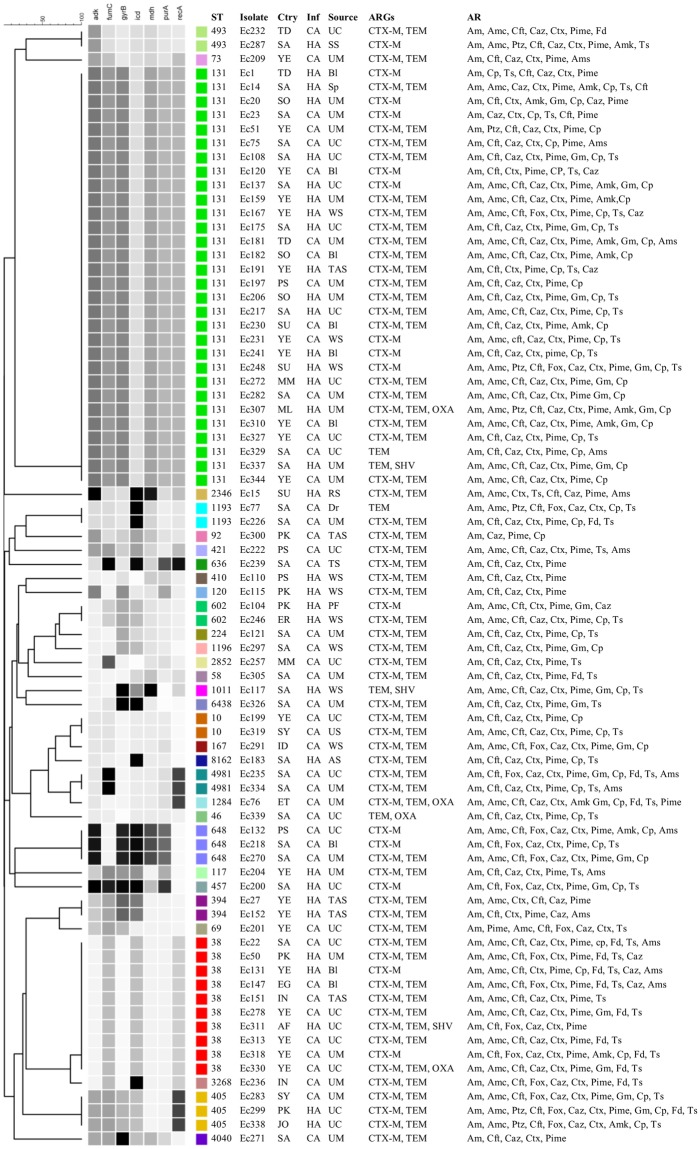
The predominantly identified CC131 and CCT38 were significantly recovered from the inpatients. However, no significant association was observed for these CCs with either community acquired or hospital acquired infections or with disease type (Fig. 4). The CC131 isolates were primarily cultured from midstream urine samples or urine catheters followed by blood specimens (Fig. 4). The two CC394 isolates were specifically recovered from tracheal aspirates of intensive care patients who acquired nosocomial infections of ESBL-positive E. coli, whereas the isolates associated with CC10 were associated with the community acquired infections. CC648 was observed in the CA cases and CC405 was observed in both HA and CA cases. The same STs, such as ST131, ST394, ST405 and ST648, were recovered from multiple hospital wards and intensive care units and patient with different diseases. No specific association was observed between clinically significant CCs and clinical specimens. In total, 14 different STs, primarily ST131 (44%), were identified from the midstream urine samples. In the urine catheter specimens, 12 different STs were identified, including the 5 STs detected in the midstream urine samples. In addition, 3 different STs were identified in blood specimens, and ST131 was primarily identified in blood. No specific association was observed for the other clinically significant CCs and clinical specimens. The 32 STs were identified from patients of 17 different nationalities, and the same ST was observed in patients of different nationalities, suggesting the diversity and cotransfer of the STs among patients from different nationalities in the health care system of Saudi Arabia. The new ST (ST8162) was recovered from a Saudi patient.
Figure 4.
UPGMA dendrogram from the pattern of pairwise differences in alleles that revealed the genetic relationships of STs among the ESBL-positive E. coli isolates, along with the country (Ctry), infection (Inf), specimen source, antimicrobial resistance genes (ARGs) and antibiotic resistances (AR) information. HA, hospital acquired; CA, community acquired; UC, urine-catheter; UM, urine-midstream; SS, skin swab; Bl, blood; Dr, drain; Sp, sputum; WS, wound swab; TAS, tracheal aspirate; TS, tissue swab; RS, rectal swab; AS, ascitic fluid; PF, peritoneal fluid.
All the isolates associated with CC131 and CC10 were resistant to ampicillin, cefalotin, ceftazidime, ceftriaxone, cefepime and ciprofloxacin and were sensitive to imipenem, meropenem and tigecycline (Fig. 4). In addition, all the CC131 isolates were sensitive to nitrofurantoin. In contrast to CC131 and CC10, the majority of isolates associated with CC38 were sensitive to ciprofloxacin and resistant to nitrofurantoin and trimethoprim/sulfamethoxazole. The blaCTX-M gene was present in 93.3% of the ST131 isolates, and this group primarily harbored blaCTX-M-1 (60.3%), whereas 66.6% of ST131 isolates contained both the blaCTX-M and blaTEM genes (Fig. 4). None of the ST131 isolates contained the blaCTX-M-8/2 and blaCTX-M-2 group genes. All the isolates associated with CC38 carried blaCTX-M genes, primarily blaCTXM-1, followed by blaCTX-M-9 genes. All the isolates associated with CC10 carried both blaCTX-M and blaTEM genes.
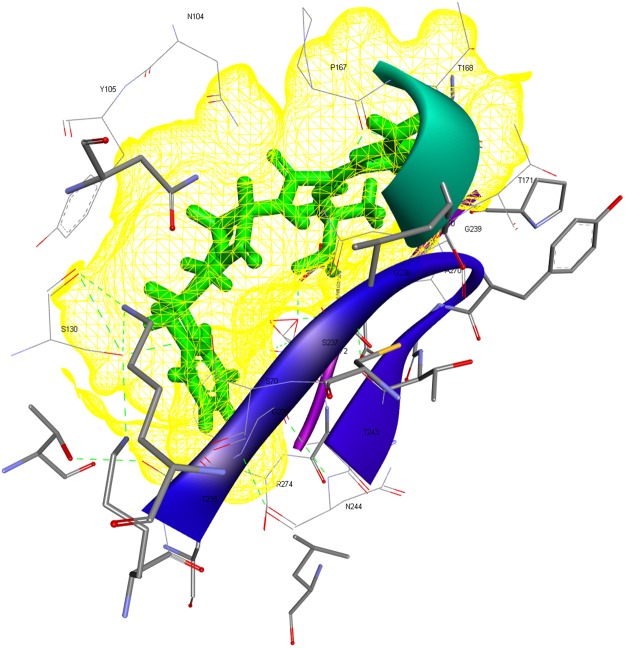
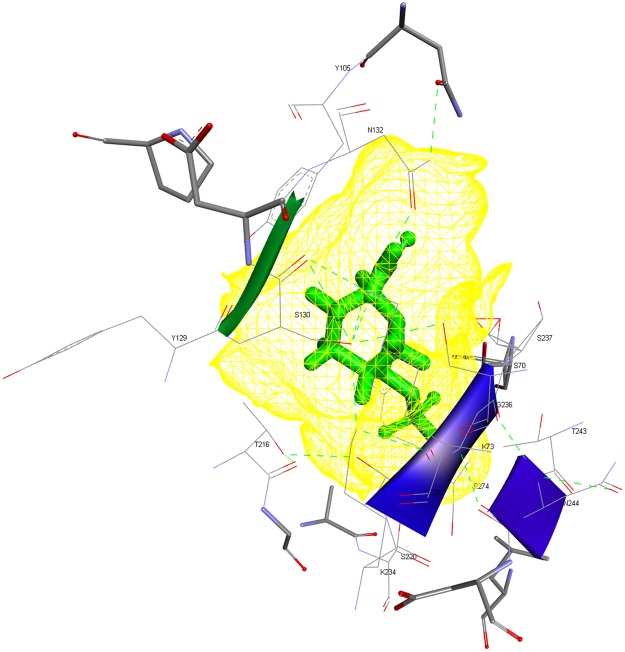
Molecular Modeling and Docking
The results of the BLAST analysis revealed that CTX-M-15 was the most prevalent variant in our study. In addition, a multiple sequence alignment by CLUSTALW indicated that within the CTX-M-15 variants, there was no noteworthy difference in the amino acid residues, particularly in those residues which constituted the “active site omega loop”. Thus, we randomly picked a CTX-M-15 sequence for molecular modeling, with the bacteria harboring this sequence having displayed significant resistance to advanced generation cefalosporins in the MIC and susceptibility tests. Briefly, the results of model validation programs indicated the CTX-M-15 model to be of ‘Good quality’ (Supplementary Figs S5 and S6). Molecular interaction analyses of the docked complexes revealed the amino acid residues crucial to the binding of antibiotics and inhibitors to the modeled CTX-M-15. Figure 5 represents the docking pose and the interacting amino acid residues for the CTX-M-15-ceftazidime-complex (Fig. 5). In contrast, avibactam displayed the most robust interaction with CTX-M-15 among the inhibitors in the docked state (ΔG = −6.6 kcal/mol). The corresponding pose and interacting amino acid residues are shown in Fig. 6. The binding free energy values for clavulanate, tazobactam and sulbactam were determined to be −5.7, −5.9 and −5.2 kcal/mol, respectively.
Figure 5.
Wire-mesh representation of the ceftazidime-CTX-M-15 docked complex. Interacting amino acid residues of the binding pocket are labeled.
Figure 6.
Wire-mesh representation of the avibactam-CTX-M-15 docked complex. Interacting amino acid residues of the binding pocket are labeled.
Discussion
In this study, we provide comprehensive antimicrobial resistance and molecular epidemiological profiles of ESBL-producing E. coli from the Jeddah region of Saudi Arabia. Previous studies from this region have investigated selected antibiotics and clonal groups, limiting their capacity to establish a broad profile. In this study, the majority of isolates were resistant to ampicillin and cephalosporin antibiotics (except cefoxitin), followed by fluoroquinolone and trimethoprim/sulfamethoxazole, which may be associated with self-medication and the common use of β-lactam antibiotics by humans in this region, and this is a trend in the surrounding countries and in the countries of origin of the expatriates. However, we did not detect any carbapenem resistant ESBL-producing E. coli, and low resistance was observed against amikacin, which could be used to combat E. coli infections in this region. Other studies from Saudi Arabia observed comparable levels of resistance in ESBL-producing E. coli recovered from UTI patients and other clinical specimens11,16. However, Al-Agamy recently reported the isolation of carbapenem-resistant E. coli from Riyadh hospitals, including blaNDM-1- and blaOXA-48-positive isolates17. The findings of this study show for the first time that the primary incidence of ESBL-producing E. coli infection in this area are community-onset infections.
Importantly, a marked diversity of clones was observed in the E. coli isolates from Saudi Arabia, and 32 distinct STs from 80 isolates were processed for MLST in this study. Consistent with worldwide reports, ST131 was the predominant ST identified, followed by ST38 and the isolates associated with CC1011,18. In the United States, 53% of ESBL-producing E. coli are associated with ST13119. Similarly, in the United Kingdom and France, 64 and 25% of community-acquired infections from E. coli belonged to ST131, respectively20,21. In previous studies, apart from ST131, STs, ST69, ST73 and ST95 were predominantly identified in a large collection of E. coli and accounted for 40–60% of UTI isolates22,23. In contrast to the previous local reports and studies from the western world, ST38 was the second dominant ST detected in this study. These results, together with those of published studies from Saudi Arabia, suggest the existence of variation in the range of ST131 in the eastern and western regions of Saudi Arabia and indicate a high percentage of ST131 in the Makkah region (≥30%) and in Riyadh (17.3%)10,11. Similarly, variation was observed in the relative percentage distribution of other commonly identified STs in the studies from the eastern and western regions of Saudi Arabia, such as ST73, which was detected at a relatively higher abundance in the eastern region of Saudi Arabia10. Prior to this study, 16 STs, including ST1284, ST92, ST120 and ST46, had not been previously reported from Saudi Arabia and were previously reported from pathogenic strains associated with different diseases worldwide. In addition, we identified a novel ST (ST8162) from a Saudi patient. However, caution should taken in applying the current finding of E. coli clonal distribution to the different geographical regions of Saudi Arabia, as the analysis is based on a limited number of available data. Thus, additional studies are required to understand the distribution of E. coli sequence types in Saudi Arabia. The high diversity in the E. coli clones may have arisen because approximately half of the population of Saudi Arabia are expatriates from developing countries, including Pakistan, India, Bangladesh, the Philippines and African countries where self-medication in patients is evident24.
The antibiotic resistance observed in this study with respect to the different STs were general patterns, with multidrug resistance particularly observed against ampicillin, cephalosporins, ciprofloxacin and trimethoprim/sulfamethoxazole, and the majority of isolates were sensitive to carbapenems. All the ST131-associated isolates were resistant to ciprofloxacin and were sensitive to imipenem, tigecycline and nitrofurantoin. In contrast, low resistance to ciprofloxacin and high resistance to nitrofurantoin was observed in the ST38 isolates. A disproportionate susceptibility to ciprofloxacin in ST131 isolates has been observed in different studies in various geographical regions. In North America, a 23–28% resistance to fluoroquinolone was reported in ST131 isolates, and background resistance was 27% in E. coli25. Similarly, a recent study from Australia observed a 21% fluoroquinolone resistance rate in ST131 isolates from a selected patient population with UTIs, with an estimated 41% of fluoroquinolone-resistant E. coli within the studied population26,27. Overall, the background ciprofloxacin resistance is high in our region compared to other countries where low rates of fluoroquinolone resistance in E. coli have been achieved through regulatory control of fluoroquinolone use in humans and animals28. We observed that the ST405, ST1284 and ST648 isolates were resistant to ≥nine antibiotics. However, the association between ST and the prospective resistance reasonably suggests that rapid identification of E. coli sequence types by molecular techniques might allow treatment to be optimized before the conventional antibiogram could be completed. This would be particularly important in the case of the commonly resistant ST131, as it would allow treatment to be switched, e.g., to a carbapenem in life-threatening infections, or to nitrofurantoin in uncomplicated UTI cases in Saudi Arabia.
The results of this study suggest that the ESBL genes, primarily blaCTX-M and blaTEM, are widely scattered into the 32 STs, which has been confirmed by other reports10,11. The ST131 and ST38 isolates were mainly comprised of the blaCTX-M group blaCTX-M-1 genes, followed by blaCTC-M-9. Recent studies have revealed a substantial increase in the number of blaCTX-M-producing E. coli, which is probably due to the central mechanisms of clonal expansion of E. coli ST13129. We have analyzed all ESBL-positive isolates for blaCTX-M genes by a PCR assay. The results showed that almost all the isolates (99.5%) carried blaCTX-M. Our results, together with those of previous studies, indicates that the blaCTX-M type is the most common ESBL resistance gene in Saudi Arabia; the rate is higher than that reported from Europe and is consistent with that of China10,20,30. At the same time, the primary blaCTX-M group was blaCTX-M-1, which was confirmed by several other local studies10. In China, the primary blaCTX-M-14 and blaCTX-M-15 gene types were reported from blaCTX-M, and differences were observed in the distribution of blaCTX-M-1 and blaCTX-M-9, highlighting the existence of regional epidemiological features. The assay results for the blaTEM, blaSHV and blaOXA genes showed that blaTEM-positive E coli strains were also very common in the ESBL-producing E. coli, while the others were relatively rare, which is consistent with the results from previous studies conducted in China31. In addition, the positive rates of the blaTEM, blaSHV and blaOXA genes exhibited some differences among areas, indicating that there are some regional epidemiological characteristics. As the different ESBL resistance genes encode β-lactams with different hydrolysis capabilities, the different ESBL distributions should be considered with respect to antibacterial use.
Studies at the interface of clinical microbiology and bioinformatics are increasingly being used to address the problem of multiple antibiotic resistance in bacteria. The ensuing battle, i.e., antibiotics versus bacteria, has been acknowledged by the scientific community32,33. Consequently, we suggest that a combination of “ceftazidime and avibactam” could be the best therapy to tackle infections caused by carbapenems resistant Gram-negative bacteria among Saudi patients. This suggestion is supported by the findings of Flamm et al.34, where the authors reported that all of the screened ESBL-positive and meropenem-nonsusceptible E. coli and K. pneumoniae isolates displayed a ceftazidime-avibactam MIC of ≤4 μg/mL34. Furthermore, Castanheira et al.35 tested the activity of a ceftazidime-avibactam combination against Enterobacteriaceae from US hospitals and observed that it displayed commendable activity against the studied strains, including multiresistant KPC-producers35. We therefore implore and encourage the scientific community to recommend the judicious use of antibiotics to help restore bacterial susceptibility to agents such as bactrim and fluoroquinolones. If need be, the first-line agent for ESBL-producing E. coli should be a carbapenem such as ertapenem. It is suggested that ceftazidime-avibactam should be reserved for cases of Carbapenem-Resistant Enterobacteriaceae (CRE). Even in this situation, caution must be exercised, as there are reports of the emergence of ceftazidime-avibactam resistance among CRE with the increasing use of this novel agent36.
Conclusion
The threat of multidrug resistant ESBL-producing E. coli is steadily increasing in Saudi Arabia. A markedly diverse clonal composition of the ESBL-producing E. coli isolates was observed in the western region of Saudi Arabia. A potential factor contributing to this observation may be the large expatriate population working in the metropolitan city of Jeddah and its surroundings. ST38 was identified as an emerging clone following ST131, and blaCTX-M was identified as the primary genotype. The results obtained by microbiological and computational approaches reinforce the conclusion of the present study. Overall, the study concludes that ‘ceftazidime along with avibactam’ and carbapenems could be two promising treatment options against MDR ESBL-producing E. coli in this region. Carbapenems may be used as a first-line option against E. coli isolates resistant to cephalosporins, ciprofloxacin and gentamycin from this region. Furthermore, the results described herein may be useful to update the empirical antibiotic regimens in the health care facilities of Saudi Arabia. An effective antibiotic stewardship program and regular antibiotic resistance surveillance studies are required to avoid complications in the future management of clinical isolates of E. coli-producing ESBLs.
Materials and Methods
Sample collection
This study was conducted at the special infectious agent unit (SIAU) of King Fahd Medical Research Center (KFMRC) with the collaboration of the infection control unit and the clinical and molecular microbiology laboratory of King Abdulaziz University hospital (KAUH) in Jeddah. KAUH is an 845-bed teaching hospital of the King Abdulaziz University that primarily serves the western region of Saudi Arabia. This study was approved by the ethical research committee of the Faculty of Medicine at King Abdulaziz University under the reference number (148–14). The participants provided informed consent, and all the methods were performed in accordance with the approved guidelines. In total, 211 ESBL-producing E. coli isolates were analyzed from 2014–2015.
Identification and Antimicrobial Susceptibility Screening
The purified isolates were freshly cultured on blood agar plates at 37 °C for 18–20 hrs using a biosafety level-2 cabinet. The identity of the purified isolates was determined by MALDI-TOF (MALDI Biotyper Bruker Daltonics, USA) according to the manufacturer’s instructions as described in our previous study37. The calibration was performed using E. coli ATCC 8739 as a standard to validate the run. All the isolates were run in duplicate, and identity score of ≥1.9 with database spectra was considered as a correct identification. All the isolates were initially tested for antimicrobial susceptibility using an automated VITEK-2 (BioMérieux, France) system with a specific AST-N291 card for ESBL-producing Gram-negative bacteria. The results were interpreted according to the guidelines of the CLSI38. The criteria of Magiorakos et al. was used to defined MDR, XDR and PDR isolates39.
ERIC PCR, MLST and Whole Genome Sequencing
The study isolates were typed by Enterobacterial repetitive intergenic consensus (ERIC) PCR to identify genetic relatedness and to limit the number of strains for further investigations. ERIC PCR was performed in 25 µl volumes containing 1 µl (10 µM) of each primer (Table 1), 12.5 µl Go Taq® Green Master Mix (Promega, USA), 1.5 µl DNA template and 9 µl nuclease free water (Promega, USA) following the PCR conditions described by Versalovic et al.40. As previously described, an Achtman MLST scheme based on the internal fragment amplification of housekeeping genes was used to type the ESBL-producing E. coli isolates with slight modification of the annealing temperature41. The allelic profiles and sequence types (STs) were retrieved from the BLAST search of amplified genes in the EnteroBase database (https://enterobase.warwick.ac.uk/species/index/ecoli).
Whole genome sequence was performed for the isolates were STs were not defined from the Achtman scheme. Genomic DNA of the isolates was sequenced on a MiSeq platform (Illumina, USA) with the paired-end strategy using a Nextera XT library kit (Illumina, USA) as described previously42. The ID and allelic profile of the novel ST was obtained from the EnteroBase after uploading the raw read files connected with the metadata.
PCR of β-lactamase Genes
PCR and sequence analyses were performed to determine the genes responsible for the ESBL-phenotype in the ESBL-producers. PCRs for the blaTEM, blaSHV, blaCTX-M and blaOXA genes were conducted using previously described multiplex PCR primers and conditions43. The full-length blaCTX-M gene was amplified from the ESBL-producing isolates using the primers and conditions described by Pfeifer et al.44 and was sequenced with an ABI prism sequencer 3730 (Applied Biosystems, USA). The major groups (blaCTX-M-1, blaCTX-M-2, blaCTX-M-9 and blaCTX-M-8/25) were amplified from the blaCTX-M-positive isolates using group-specific primers according to Xu et al.45.
Molecular Modeling and Docking
Once confirmed as blaCTX-M gene sequences by BLAST, the different blaCTX-M nucleotide sequences were translated to corresponding amino acid sequences using the ‘EXPASY translate tool’. Subsequently, the CTX-M amino acid sequences were subjected to multiple sequence alignments using CLUSTALW to detect any possible mutations, particularly in the active site Ω-loop, which is known to affect the substrate profile of CTX-M enzymes. Modeling was performed using the Swiss Model Server. The modeled structure (prior to docking) was verified using multiple validation programs, including VADAR, GeNMR and PROSESS. PDB structures of drugs/inhibitors were retrieved from Drug bank. The ligands (drugs/inhibitors) were docked into the active crevice of the modeled CTX-M-15 enzyme using AUTODOCK4.246 with the aid of the ‘CLICK-BY-CLICK’-protocol47. The ligands included beta-lactam antibiotics (cefepime, cefotaxime and ceftazidime) as well as inhibitors (avibactam, clavulanate, tazobactam and sulbactam). All of the ligand structures were energy-minimized employing an MMFF94 force field. “Gasteiger charges” were added to the ligand atoms. Rotatable bonds were defined and nonpolar hydrogens were added. “Kollman charges”, essential hydrogens, and other relevant solvation parameters were also added. AUTOGRID was used to construct a grid of 40 Å3 with a spacing of 0.375 Å to target the active crevice of the CTX-M-15 enzyme model. The values of x, y, and z grid coordinates used to target the CTX-M-15 binding pocket were −4.1755, −2.4075, and 8.8905, respectively. Docking experiments used the ‘Solis & Wets local search method’ and a Lamarckian genetic-algorithm (LGA) and incorporated 100 runs each. Each run was programmed to perform 2.5 million “energy-evaluations” prior to termination. Discovery Studio (BIOVIA, San Diego) was used for molecular visualization of the docked complexes and the preparation of figures. Docking energies (ΔG, kcal/mol) were calculated for each of the binding pairs. Accordingly, we narrowed the observations down to few very efficient drugs and CTX-M-inhibitors with reference to the Saudi setting.
Phylogenetic and Statistical Analysis
BioNumerics (V 7.6.0) from Applied Maths was used to analyze the ERIC PCR fingerprinting results, and a dendrogram was constructed using unweighted pair group with arithmetic mean (UPGMA). The default parameters of a 1% tolerance and an 85% similarity index were considered for clustering the isolates based on fingerprinting data. Pearson chi-square or likelihood ratio were used with a significance threshold of p < 0.05.
Electronic supplementary material
Acknowledgements
This project was funded by the National Plan for Science, Technology and Innovation (MAARIFAH) - King Abdulaziz City for Science and Technology - the Kingdom of Saudi Arabia - award number (11-BIO2026-03). The authors also acknowledge with thanks the Science and Technology Unit, King Abdulaziz University for their technical support.
Author Contributions
M.Y., A.A. and S.S. contributed to the experimental work, data analysis and manuscript writing. M.F., Z.B. and R.B. contributed to the experimental work. M.A., N.A. and H.S. contributed to the sample collection. A.J., S.A., N.I. and E.A. contributed to the study design and reviewed the article.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-33093-8.
References
- 1.Shakil S, Khan AU. Infected foot ulcers in male and female diabetic patients: a clinico-bioinformative study. Ann Clin Microbiol Antimicrob. 2010;9:2. doi: 10.1186/1476-0711-9-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shakil S, Ali SZ, Akram M, Ali SM, Khan AU. Risk factors for extended-spectrum beta-lactamase producing Escherichia coli and Klebsiella pneumoniae acquisition in a neonatal intensive care unit. J Trop Pediatr. 2010;56:90–96. doi: 10.1093/tropej/fmp060. [DOI] [PubMed] [Google Scholar]
- 3.Meier S, Weber R, Zbinden R, Ruef C, Hasse B. Extended-spectrum beta-lactamase-producing Gram-negative pathogens in community-acquired urinary tract infections: an increasing challenge for antimicrobial therapy. Infection. 2011;39:333–340. doi: 10.1007/s15010-011-0132-6. [DOI] [PubMed] [Google Scholar]
- 4.Shakil S, Khan AU. Detection of CTX-M-15-producing and carbapenem-resistant Acinetobacter baumannii strains from urine from an Indian hospital. J Chemother. 2010;22:324–327. doi: 10.1179/joc.2010.22.5.324. [DOI] [PubMed] [Google Scholar]
- 5.Rice LB. Federal funding for the study of antimicrobial resistance in nosocomial pathogens: no ESKAPE. J Infect Dis. 2008;197:1079–1081. doi: 10.1086/533452. [DOI] [PubMed] [Google Scholar]
- 6.Bush K. Alarming beta-lactamase-mediated resistance in multidrug-resistant Enterobacteriaceae. Curr Opin Microbiol. 2010;13:558–564. doi: 10.1016/j.mib.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 7.Shakil S, Akram M, Ali SM, Khan AU. Acquisition of extended-spectrum beta-lactamase producing Escherichia coli strains in male and female infants admitted to a neonatal intensive care unit: molecular epidemiology and analysis of risk factors. J Med Microbiol. 2010;59:948–954. doi: 10.1099/jmm.0.020214-0. [DOI] [PubMed] [Google Scholar]
- 8.Ny S, et al. Community carriage of ESBL-producing Escherichia coli is associated with strains of low pathogenicity: a Swedish nationwide study. J Antimicrob Chemoth. 2017;72:582–588. doi: 10.1093/jac/dkw419. [DOI] [PubMed] [Google Scholar]
- 9.Shi H, et al. Epidemiology of CTX-M-type extended-spectrum beta-lactamase (ESBL)-producing nosocomial -Escherichia coli infection in China. Ann Clin Microbiol Antimicrob. 2015;14:4. doi: 10.1186/s12941-015-0063-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alghoribi MF, et al. Antibiotic-resistant ST38, ST131 and ST405 strains are the leading uropathogenic Escherichia coli clones in Riyadh, Saudi Arabia. J Antimicrob Chemother. 2015;70:2757–2762. doi: 10.1093/jac/dkv188. [DOI] [PubMed] [Google Scholar]
- 11.Alyamani EJ, et al. The occurrence of ESBL-producing Escherichia coli carrying aminoglycoside resistance genes in urinary tract infections in Saudi Arabia. Ann Clin Microbiol Antimicrob. 2017;16:1. doi: 10.1186/s12941-016-0177-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ruiz, S. J. et al. First characterization of CTX-M-15-producing Escherichia coli ST131 and ST405 clones causing community-onset infections in South America. J Clin Microbiol49, 1993–1996, doi:JCM.00045-11 (2011). [DOI] [PMC free article] [PubMed]
- 13.Bindayna K, Khanfar HS, Senok AC, Botta GA. Predominance of CTX-M genotype among extended spectrum beta lactamase isolates in a tertiary hospital in Saudi Arabia. Saudi Med J. 2010;31:859–863. [PubMed] [Google Scholar]
- 14.Bonnet R, et al. Novel cefotaximase (CTX-M-16) with increased catalytic efficiency due to substitution Asp-240 ->Gly. Antimicrob Agents Ch. 2001;45:2269–2275. doi: 10.1128/Aac.45.8.2269-2275.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Canton R, Coque TM. The CTX-M beta-lactamase pandemic. Curr Opin Microbiol. 2006;9:466–475. doi: 10.1016/j.mib.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 16.Somily AM, et al. ESBL-producing Escherichia coli and Klebsiella pneumoniae at a tertiary care hospital in Saudi Arabia. J Infect Dev Ctries. 2014;8:1129–1136. doi: 10.3855/jidc.4292. [DOI] [PubMed] [Google Scholar]
- 17.Al-Agamy, M. H., Aljallal, A., Radwan, H. H. & Shibl, A. M. Characterization of carbapenemases, ESBLs, and plasmid-mediated quinolone determinants in carbapenem-insensitive Escherichia coli and Klebsiella pneumoniae in Riyadh hospitals. J InfectPublic Health11, 64–68, doi:S1876-0341(17)30102-8 (2018). [DOI] [PubMed]
- 18.Rogers, B. A., Sidjabat, H. E. & Paterson, D. L. Escherichia coli O25b-ST131: a pandemic, multiresistant, community-associated strain. J Antimicrob Chemother66, 1–14, doi:dkq415 (2011). [DOI] [PubMed]
- 19.Doi Y, et al. Community-associated extended-spectrum beta-lactamase-producing Escherichia coli infection in the United States. Clin Infect Dis. 2013;56:641–648. doi: 10.1093/cid/cis942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lau SH, et al. UK epidemic Escherichia coli strains A-E, with CTX-M-15 beta-lactamase, all belong to the international O25:H4-ST131 clone. J Antimicrob Chemother. 2008;62:1241–1244. doi: 10.1093/jac/dkn380. [DOI] [PubMed] [Google Scholar]
- 21.Arpin C, et al. Nationwide survey of extended-spectrum {beta}-lactamase-producing Enterobacteriaceae in the French community setting. J Antimicrob Chemother. 2009;63:1205–1214. doi: 10.1093/jac/dkp108. [DOI] [PubMed] [Google Scholar]
- 22.Horner C, et al. Escherichia coli bacteraemia: 2 years of prospective regional surveillance (2010-12) J Antimicrob Chemother. 2014;69:91–100. doi: 10.1093/jac/dkt333. [DOI] [PubMed] [Google Scholar]
- 23.Manges AR, Tabor H, Tellis P, Vincent C, Tellier PP. Endemic and epidemic lineages of Escherichia coli that cause urinary tract infections. Emerg Infect Dis. 2008;14:1575–1583. doi: 10.3201/eid1410.080102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang G, Wang W. Present situation of residents recognition and medication behaviors of antibiotics and the influencing factors. Chin Gen Pract. 2013;16:819–822. [Google Scholar]
- 25.Banerjee R, et al. Escherichia coli sequence type 131 is a dominant, antimicrobial-resistant clonal group associated with healthcare and elderly hosts. Infect Control Hosp Epidemiol. 2013;34:361–369. doi: 10.1086/669865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kudinha T, et al. Escherichia coli sequence type 131 as a prominent cause of antibiotic resistance among urinary Escherichia coli isolates from reproductive-age women. J Clin Microbiol. 2013;51:3270–3276. doi: 10.1128/JCM.01315-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rogers BA, et al. Sequence type 131 fimH30 and fimH41 subclones amongst Escherichia coli isolates in Australia and New Zealand. Int J Antimicrob Agents. 2015;45:351–358. doi: 10.1016/j.ijantimicag.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 28.Cheng AC, et al. Control of fluoroquinolone resistance through successful regulation, Australia. Emerg Infect Dis. 2012;18:1453–1460. doi: 10.3201/eid1809.111515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lavigne JP, et al. Virulence potential and genomic mapping of the worldwide clone Escherichia coli ST131. PLoS One. 2012;7:e34294. doi: 10.1371/journal.pone.0034294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xia S, et al. Dominance of CTX-M-type extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli isolated from patients with community-onset and hospital-onset infection in China. PLoS One. 2014;9:e100707. doi: 10.1371/journal.pone.0100707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang C, et al. Characterization of carbapenemases, extended spectrum beta-lactamases, quinolone resistance and aminoglycoside resistance determinants in carbapenem-non-susceptible Escherichia coli from a teaching hospital in Chongqing, Southwest China. Infect Genet Evol. 2014;27:271–276. doi: 10.1016/j.meegid.2014.07.031. [DOI] [PubMed] [Google Scholar]
- 32.Shakil S, Khan R, Zarrilli R, Khan AU. Aminoglycosides versus bacteria–a description of the action, resistance mechanism, and nosocomial battleground. J Biomed Sci. 2008;15:5–14. doi: 10.1007/s11373-007-9194-y. [DOI] [PubMed] [Google Scholar]
- 33.Shaikh S, Fatima J, Shakil S, Rizvi SM, Kamal MA. Antibiotic resistance and extended spectrum beta-lactamases: Types, epidemiology and treatment. Saudi J Biol Sci. 2015;22:90–101. doi: 10.1016/j.sjbs.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Flamm RK, Sader HS, Farrell DJ, Jones RN. Ceftazidime-avibactam and comparator agents tested against urinary tract isolates from a global surveillance program (2011) Diagn Microbiol Infect Dis. 2014;80:233–238. doi: 10.1016/j.diagmicrobio.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 35.Castanheira M, Mills JC, Costello SE, Jones RN, Sader HS. Ceftazidime-avibactam activity tested against Enterobacteriaceae isolates from U.S. hospitals (2011 to 2013) and characterization of beta-lactamase-producing strains. Antimicrob Agents Chemother. 2015;59:3509–3517. doi: 10.1128/AAC.00163-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shields, R. K. et al. Clinical Outcomes, Drug Toxicity, and Emergence of Ceftazidime-Avibactam Resistance Among Patients Treated for Carbapenem-Resistant Enterobacteriaceae Infections. Clin Infect Dis63, 1615–1618, doi:ciw636 (2016). [DOI] [PMC free article] [PubMed]
- 37.Angelakis E, et al. MALDI-TOF mass spectrometry and identification of new bacteria species in air samples from Makkah, Saudi Arabia. BMC Res Notes. 2014;7:892. doi: 10.1186/1756-0500-7-892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.CLSI. Performance standards for antimicrobial susceptibility testing; 26 ed Clinical and Laboratory Standards Institute, Wayne, PA. (2016).
- 39.Magiorakos AP, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–281. doi: 10.1111/j.1469-0691.2011.03570.x. [DOI] [PubMed] [Google Scholar]
- 40.Versalovic J, Koeuth T, Lupski JR. Distribution of repetitive DNA sequences in eubacteria and application to fingerprinting of bacterial genomes. Nucleic Acids Res. 1991;19:6823–6831. doi: 10.1093/nar/19.24.6823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wirth T, et al. Sex and virulence in Escherichia coli: an evolutionary perspective. Mol Microbiol. 2006;60:1136–1151. doi: 10.1111/j.1365-2958.2006.05172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lagier JC, et al. Non contiguous-finished genome sequence and description of Clostridium jeddahense sp. nov. Stand Genomic Sci. 2014;9:1003–1019. doi: 10.4056/sigs.5571026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fang H, Ataker F, Hedin G, Dornbusch K. Molecular epidemiology of extended-spectrum beta-lactamases among Escherichia coli isolates collected in a Swedish hospital and its associated health care facilities from 2001 to 2006. J Clin Microbiol. 2008;46:707–712. doi: 10.1128/JCM.01943-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pfeifer Y, Matten J, Rabsch W. Salmonella enterica serovar Typhi with CTX-M beta-lactamase, Germany. Emerg Infect Dis. 2009;15:1533–1535. doi: 10.3201/eid1509.090567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xu G, An W, Wang H, Zhang X. Prevalence and characteristics of extended-spectrum beta-lactamase genes in Escherichia coli isolated from piglets with post-weaning diarrhea in Heilongjiang province, China. Front Microbiol. 2015;6:1103. doi: 10.3389/fmicb.2015.01103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Morris GM, et al. AutoDock4 and AutoDockTools4: Automated docking with selective receptor flexibility. J Comput Chem. 2009;30:2785–2791. doi: 10.1002/jcc.21256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rizvi SM, Shakil S, Haneef M. A simple click by click protocol to perform docking: AutoDock 4.2 made easy for non-bioinformaticians. EXCLI J. 2013;12:831–857. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.