Background
Xanthogranulomatosis (XG) is a granulomatous dermatitis defined as multiple eruptive xanthogranuloma. Although it is commonly observed in children and most of the time regresses over several months or years, it is less common during adulthood and generally tends to then persist. It is well known that XG in adults classically goes along with hematologic disorders such as leukemia, lymphoma, myeloproliferative diseases, and, more rarely, myelodysplastic syndromes. To date, it has not been possible to find any treatment or to explain the underlying molecular mechanisms, hence the need for further research. We report a case of an adult patient with multiple xanthogranuloma and a 2-year history of a rare hypereosinophilic myelodysplasia. This is the first case, to our knowledge, in which improvement has been achieved with thalidomide (50 mg/d) showing its efficacy in this granulomatous disease.
Case report
A 51-year old white man came to our dermatology department, as he had been suffering from a symptomatic nodular eruption for 3 weeks (Fig 1). Originally, the nodules were bilateral and symmetrically located on the extensor surfaces, but they generalized after 3 weeks with no ophthalmologic or mucosal involvement. They were slightly itchy and painful. Tiredness, night sweats, and inflammatory arthralgia of proximal joints concomitantly began and increased over time. No other systemic involvement was noted.
Fig 1.
Skin examination finds well-demarcated, orange-reddish nodules of 0.5 to 1 cm with a firm to elastic consistency.
This man was currently under the care of the hematology department for a rare myelodysplastic syndrome which appeared 2 years prior. Chromosomal analysis on medullar biopsy found a karyotype 45 X-Y with a rare translocation of t(9;12)(q22;p13). Initially, the myelodysplasia was successfully controlled with hydroxyurea and methylprednisolone. However, biological analysis showed an increased eosinophilia (1150/mm3) accompanying the dermatologic disorder with a slight inflammatory syndrome (C-reactive protein, 46.40 mg/L). There was no other significant biological disruption.
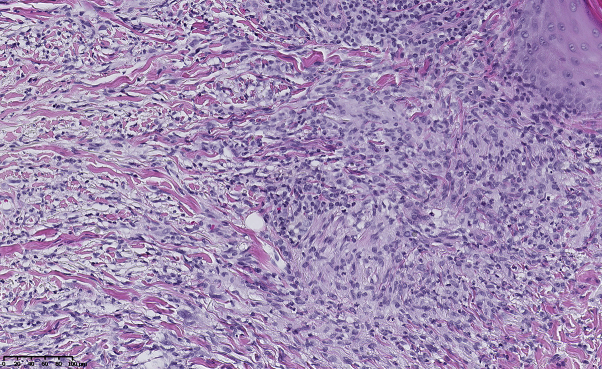
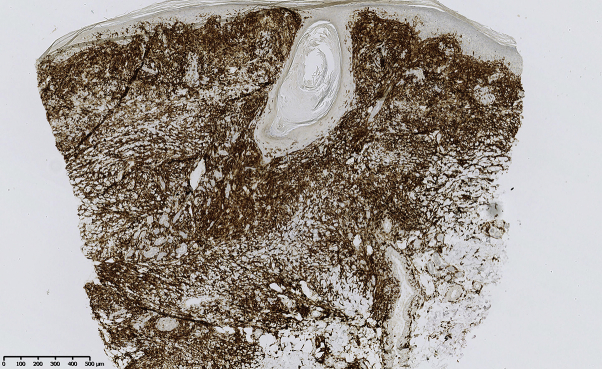
The histopathologic examination of a nodule found a dense granulomatosis infiltrate mainly composed of histiocytes intermingled with collagen bundles, few neutrophils, eosinophils, and lymphocytes (Fig 2, eSlide: VM04937). The infiltrate was perivascular and mostly interstitial and reached the reticular dermis. Immunohistochemistry found a strong positive reaction to CD163 (Fig 3, eSlide: VM04938) and negative reactions to the S100 protein and CD1a. A diagnosis of eruptive xanthogranuloma was thereby established on the basis of clinicopathologic correlation.
Fig 2.
Punch biopsy result shows dense granulomatosis infiltrate composed mainly of histiocytes intermingled with collagen bundles, few neutrophils, eosinophils, and lymphocytes. (Hematoxylin-eosin stain; original magnification: ×20.)
Fig 3.
Strong positive reaction to CD163.
The patient had to be admitted to the hematologic department for pain management. Upon admission, bone marrow biopsies did not show any evolution into an acute leukemia or myelodysplasia worsening.
In coordination with the hematologist, interferon-α2a and methylprednisolone (64 mg) were initiated. Eventually, the general condition of the patient improved with a decrease of the pain scale and a flattening of the skin lesions. However, systemic corticotherapy had to be progressively stopped because of side effects (Cushing face, headache, increased anxiety, and depressive syndrome) which predominantly triggered a relapse of both the nodules and the systemic symptoms. Topical corticotherapy and photochemotherapy (ultraviolet A) failed to show any clinical benefit, whereas thalidomide (50 mg/d) successfully improved the patient's quality of life, resolving cutaneous lesions, and stabilizing the hematologic disease after 3 weeks on thalidomide (Fig 4). The patient still remains stable after 2 years of treatment.
Fig 4.
Complete clearance of the skin lesions 3 weeks after the beginning of the treatment based on thalidomide (50 mg once a day), leaving only hyperpigmented macules.
Discussion
XG represents a common non-Langerhans histiocytosis affecting mainly children and is known as juvenile xanthogranuloma. The first adult case was described by Gartmann and Tritsch in 1963.1 Since then, at least 30 cases have been described in the literature with lesions tending to have a more chronic course.2, 3, 4, 5
Extracutaneous lesions have been only observed with juvenile xanthogranuloma but never in the adult form. Despite their differences, the 2 forms seem to bear many similarities. The clinical presentation is identical: multiple eruptive yellow-brownish and firm papules or nodules diffusely distributed over the body. Biopsy specimens typically show dermal granulomatous infiltrate of numerous histiocytes, Touton giant cells, and various other inflammatory cells. They might also share an increased risk of association with malignancy, although this seems to be more common during adulthood.3
In literature, we have identified 34 cases of adult XG, of which, 11 cases were associated with malignancies: leukemias (4), lymphomas (3), myelodysplastic syndrome (1), monoclonal gammapathy (1), essential thrombocythemia (1), and gastrointestinal stromal tumor (1).2, 3, 4, 5
The exact pathogenesis of XG associated with hematologic disorders still remains to be elucidated. As suggested in previous reports,6, 7 CD163+ M2 macrophages, CD4+ regulatory T cells, and interleukin-17–producing cells seem to be implicated in the mechanism of granulomatous dermatitis associated with the myelodysplastic syndrome. Overall, their proportions are also correlated with hematologic progression. Indeed, the prognosis is directly correlated to the T-helper 17 and regulatory T cell ratio. These studies also mentioned that, in granuloma, regulatory T cells were predominant, whereas T-helper 17 cells were scattered. CD163+ M2 macrophages might be inducers of these regulatory T cells, but the molecular mechanism is still unknown, and further analyses remain to be conducted.
There are no guidelines for the treatment of multiple xanthogranuloma, neither in adults, nor in children. Treatment is mandatory if systemic involvement is observed. It can be necessary if lesions are disfiguring or symptomatic.
This dermatitis is not a real paraneoplastic feature because the oncologic treatment has various results on the skin lesions and does not automatically show cutaneous improvement as observed in our case.2, 3
In our patient, a treatment was necessary because of a decreased quality of life. Systemic steroids have been efficient, but side effects forced us to stop using them. Systemic steroids could therefore be used to quickly control the disease activity for a few weeks, but XG requires a safer long-term treatment. Other immunosuppressive drugs are not recommended to treat such cutaneous diseases because of their potential association with malignancies.
Thalidomide and its analogs are interesting immunomodulatory drugs for patients suffering from XG associated with hematologic diseases. Overall, these treatments are currently being used in the hematology department, in combination with other chemotherapies to stop the growth of malignant cells, especially in the cases of multiple myeloma and myelodysplastic syndromes.
The efficacy of these treatments is also well known in the case of granulomatous diseases such as sarcoidosis and erythema nodosum leprosum.8 Their efficacy on granulomatous diseases has been demonstrated in vitro, where they prevented the formation of multinucleated giant cells by inhibiting stimulated macrophages and modulating production of chemokines.9
In our case, thalidomide has been used successfully to improve the patient's quality of life, resolve cutaneous lesions, and stabilize the hematologic disease.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Gartmann H., Tritsch H. Heln- and grobknotigens naevoxanthoendotheliom. Dermatologica. 1963;215:409–421. [Google Scholar]
- 2.Chiou C.C., Wang P.N., Yang L.C., Kuo T.T., Hong H.S. Disseminated xanthogranulomas associated with adult T-cell leukaemia/lymphoma: a case report and review the association of haematologic malignancies. J Eur Acad Dermatol Venereol. 2007;21:532–535. doi: 10.1111/j.1468-3083.2006.02013.x. [DOI] [PubMed] [Google Scholar]
- 3.Shoo B.A., Shinkai K., McCalmont T.H., Fox L.P. Xanthogranulomas associated with hematologic malignancy in adulthood. J Am Acad Dermatol. 2008;59(3):488–493. doi: 10.1016/j.jaad.2008.03.046. [DOI] [PubMed] [Google Scholar]
- 4.Narváez-Moreno B., Pulpillo-Ruiz A., De Zulueta-Dorado T., Conejo-Mir J. Disseminated juvenile xanthogranuloma associated with follicular lymphoma in an adult: successful treatment with chemotherapy and rituximab. A review of the literature. Actas Dermosifiliogr. 2013;104:242–246. doi: 10.1016/j.ad.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 5.Vadeboncoeur S., Provost N. Multiple xanthogranulomas in an adult. J Cutan Med Surg. 2016;20(5):474–477. doi: 10.1177/1203475416640795. [DOI] [PubMed] [Google Scholar]
- 6.Namiki T., Miura K., Yokozeki H. Multiple CD163+ adult xanthogranuloma associated with myelodysplastic syndrome. J Dermatol. 2015;42(11):1106–1107. doi: 10.1111/1346-8138.13052. [DOI] [PubMed] [Google Scholar]
- 7.Agiwara A., Fujimura T., Furudate S. Generalized granulomatous dermatitis accompanied by myelodysplastic syndrome. Acta Derm Venereol. 2014;94:223–224. doi: 10.2340/00015555-1656. [DOI] [PubMed] [Google Scholar]
- 8.Chen M., Doherty S.D., Hsu S. Innovative uses of thalidomide. Dermatol Clin. 2010;8(3):577–586. doi: 10.1016/j.det.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Yasui K., Yashiro M., Nagaoka Y. Thalidomide prevents formation of multinucleated giant cells (Langhans type cells) from cultured monocytes: possible pharmaceutical applications for granulomatous disorders. Int J Immunopathol Pharmacol. 2009;22(3):707–714. doi: 10.1177/039463200902200316. [DOI] [PubMed] [Google Scholar]