Abstract
Objectives
Pneumonia is a major cause of death among inpatients at psychiatric hospitals. Psychiatric hospital-acquired pneumonia (PHAP) is defined as pneumonia developed in inpatients at psychiatric hospitals. PHAP is a type of nursing and healthcare-associated pneumonia (NHCAP). The purpose of this study was to clarify the risk factors for mortality among PHAP patients.
Methods
We retrospectively reviewed the clinical files of patients transferred to Tokyo Metropolitan Matsuzawa Hospital from psychiatric hospitals for PHAP treatment during the 10-year period from September 2007 to August 2017. We analyzed the clinical differences between the survivors and non-survivors and assessed the usefulness of severity classifications (A-DROP, I-ROAD, and PSI) in predicting the prognosis of PHAP.
Results
This study included a total of 409 PHAP patients, 87 (21.3%) of whom expired and 322 (78.7%) of whom survived. The mortality rates, according to the A-DROP classifications, were 4.9% in the mild cases, 21.6% in the moderate cases, 40.7% in the severe cases, and 47.6% in the very severe cases. The mortality rates, according to the I-ROAD classifications, were 9.5% in group A, 34.7% in group B, and 36.2% in group C. The mortality rates, according to the PSI classifications, were 0% in class II and III, 23.1% in class IV, and 44.9% in class V. The mortality rate increased as the severity increased. We identified 3 factors (age ≥65 years, body mass index ≤18.5 kg/m2, and bilateral pneumonic infiltration) as significant predictors of mortality. We therefore added two factors (body mass index ≤18.5 kg/m2 and bilateral pneumonic infiltration) to the A-DROP classification and established a modified A-DROP classification with a range of 0 to 7. The area under the receiver operation characteristic curves for predicting mortality were 0.699 for the A-DROP classification and 0.807 for the modified A-DROP classification.
Conclusion
The mortality rate in PHAP patients tended to increase with increasing classifications of severity. The modified A-DROP classification may be useful for predicting the prognosis of PHAP patients.
Keywords: pneumonia, psychiatric hospital, hospital-acquired pneumonia, underweight, scoring system
Introduction
In Japan, over 300,000 patients with psychiatric disorders are hospitalized in psychiatric hospitals. The number of psychiatric beds per 100,000 population is 265, the largest in the world (1). One of the major causes of death among inpatients with psychiatric disorders is pneumonia (2). Psychiatric hospital-acquired pneumonia (PHAP) is pneumonia developed among inpatients at psychiatric hospitals and is reported to account for about half of deaths at psychiatric hospitals (3,4).
PHAP is a type of healthcare-associated pneumonia (HCAP). HCAP is defined as pneumonia that develops in patients who have been receiving healthcare, and it has an in-hospital mortality rate that ranges between that observed for community-acquired pneumonia (CAP) and hospital-acquired pneumonia (HAP). The Japan Respiratory Society (JRS) created a Japanese version of the HCAP guideline. The guideline for the treatment of nursing and healthcare-associated pneumonia (NHCAP) was published by the JRS in 2011 (5). According to this guideline, PHAP includes NHCAP.
It is important to assess the disease severity of pneumonia to predict the patient prognosis. The guideline for NHCAP recommended three sets of criteria to help evaluate the severity of the pneumonia itself: 1) the A-DROP classification in the JRS's revised CAP guideline (6); 2) the I-ROAD classification in the JRS's HAP guideline (7); and 3) the pneumonia severity index (PSI) cited in the Infectious Diseases Society of America (IDSA)'s CAP guideline (8). However, to our knowledge, there have been no studies examining the disease severity of PHAP.
While our hospital is a psychiatric hospital, we have a Medical Comorbidity Ward and have accepted patients transferred from other psychiatric hospitals to be treated for medical comorbidities. We therefore performed a retrospective cohort study to elucidate the risk factors for mortality due to PHAP.
Materials and Methods
Study population
The clinical files of the consecutive patients transferred from a psychiatric hospital to Tokyo Metropolitan Matsuzawa Hospital for the treatment of PHAP during the 10-year period from September 2007 to August 2017 were retrospectively reviewed. PHAP was defined as pneumonia developed in patients hospitalized at a psychiatric hospital. This study was approved by the institutional review board of Tokyo Metropolitan Matsuzawa Hospital.
We reviewed each patient's physical characteristics, clinical parameters, laboratory findings, and radiographic findings on admission. The presence of overt symptoms of dysphagia or a medical history of aspiration was determined as a swallowing disorder in each patient. The outcomes were either alive or dead at the time of hospital discharge. In addition, the physical characteristics, clinical parameters, laboratory findings, and radiographic findings were compared between the two patient groups of “alive” or “deceased” at the time of hospital discharge in order to assess the utility of these variables in defining the severity of PHAP. A multivariable analysis was performed to define which prognostic factors were related to mortality due to PHAP.
The A-DROP classification, I-ROAD classification, and PSI were applied to PHAP patients. The mortality rate was determined in accordance with the severity classification of each scoring system. We then added clinical variables that were found to be independent predictors of mortality to the A-DROP classifications and established a modified A-DROP classification. We analyzed the performance characteristics of the scores calculated according to the A-DROP and modified A-DROP classifications.
Statistical analyses
The quantitative data are presented as the mean±standard deviation. The differences between survivors and non-survivors were analyzed using the chi-squared test for categorical variables and Student's t-test for quantitative variables. A multiple logistic regression analysis was used to assess the role of several variables as prognostic factors related to mortality due to PHAP. The contribution of each potential prognostic factor was denoted by an odds ratio and the associated 95% confidence interval (CI). A receiver operating characteristic (ROC) curve was used to analyze the probability of PHAP mortality in dependence on the calculated score. A value of p<0.05 was considered to be significant. A statistical software package (JMP, version 10.0.2; SAS Institute; Cary, USA) was used for the statistical analysis.
Results
A total of 409 patients who were transferred to Tokyo Metropolitan Matsuzawa Hospital from a psychiatric hospital for the treatment of PHAP were included in this study. Of these 409 patients, 87 (21.3%) had expired at the time of hospital discharge, while 322 (78.7%) were still alive. The physical characteristics and clinical parameters of patients with PHAP according to a survival or fatal outcome are summarized in Table 1. The features of non-survivors differed distinctly from those of the survivors. The non-survivors group tended to be older and had a lower body mass index (BMI) than the survivors (72.6±5.5 vs. 62.7±12.4 years, p<0.0001; 14.4±1.5 vs. 17.7±3.9 kg/m2, p<0.0001, respectively). Figs. 1, 2 show the distribution of the patients according to the age and BMI.
Table 1.
Characteristics, Laboratory Findings and Radiographic Findings of the 409 Patients with Psychiatric Hospital-acquired Pneumonia according to the Outcome*.
| Survivors (n=322) |
Non-survivors (n=87) |
p value | ||||
|---|---|---|---|---|---|---|
| Age, years | 62.7±12.4 | 72.6±5.5 | <0.0001 | |||
| Men/women, n | 210/112 | 61/26 | 0.391 | |||
| Psychiatric illness, n (%) | ||||||
| Schizophrenia | 274 (85.1%) | 71 (81.6%) | 0.427 | |||
| Dementia | 20 (6.2%) | 7 (8.0%) | 0.541 | |||
| Mood disorder | 14 (4.3%) | 5 (5.7%) | 0.582 | |||
| Others | 14 (4.3%) | 4 (4.6%) | 0.920 | |||
| Clinical parameters | ||||||
| Height, cm | 164.0±7.3 | 163.0±7.9 | 0.270 | |||
| Body weight, kg | 47.6±11.1 | 36.1±3.7 | <0.0001 | |||
| Body mass index, kg/m2 | 17.7±3.9 | 14.4±1.5 | <0.0001 | |||
| Heart rate, /min | 94.9±21.1 | 90.5±29.5 | 0.117 | |||
| Mean blood pressure, mmHg | 92.8±15.3 | 93.6±13.0 | 0.657 | |||
| Body temperature, °C | 37.4±0.9 | 37.5±0.9 | 0.515 | |||
| SpO2 ≤90% while breathing room air | 148 (46.0%) | 41 (47.1%) | 0.252 | |||
| Oriental disturbance | 56 (17.4%) | 21 (24.1%) | 0.153 | |||
| Probable aspiration | 34 (10.6%) | 11 (12.6%) | 0.581 | |||
| Laboratory findings | ||||||
| White blood cell, ×103/μL | 10.7±5.7 | 10.9±6.6 | 0.742 | |||
| Hematocrit, % | 34.3±5.4 | 33.4±5.6 | 0.176 | |||
| Platelet, ×104/μL | 24.3±9.5 | 25.2±13.1 | 0.433 | |||
| Blood urea nitrogen, mg/dL | 18.2±7.1 | 19.3±6.2 | 0.333 | |||
| Albumin, g/dL | 2.7±1.0 | 2.6±0.9 | 0.299 | |||
| Creatinine mg/dL | 0.6±0.3 | 0.6±0.5 | 0.318 | |||
| Total bilirubin, mg/dL | 0.8±0.4 | 0.9±0.4 | 0.069 | |||
| Sodium, mEq/L | 135.1±6.3 | 135.4±10.8 | 0.770 | |||
| Potassium, mEq/L | 4.0±0.6 | 4.0±0.5 | 0.973 | |||
| C-reactive protein, mg/dL | 9.1±7.9 | 7.8±6.6 | 0.166 | |||
| Radiographic findings | ||||||
| Bilateral pneumonic infiltration | 66 (20.5%) | 56 (64.4%) | <0.001 | |||
| Multilobar pneumonic infiltration | 202 (62.7%) | 60 (69.0%) | 0.282 |
*Data are presented as n (%) or mean±standard deviation.
Figure 1.
The distribution of patients by BMI. The patients were divided into groups according to their survival (A) or a fatal outcome (B).
Figure 2.
The distribution of patients by serum level of albumin. The patients were divided into groups according to their survival (A) or a fatal outcome (B).
The laboratory findings, isolated microorganisms, and radiographic findings were then compared between the two groups (Table 1). Bilateral pneumonic infiltration was more frequently diagnosed by chest X-ray in the non-survivors group than in the survivors (64.4% vs. 20.5%; p<0.001). The types of isolated microorganisms did not differ significantly between the two groups (data not shown).
To identify the prognostic factors related to mortality, we carried out a multivariate analysis (Table 2). Age ≥65 years showed the greatest odds ratio among the predictive factors, followed by BMI ≤18.5 kg/m2 and bilateral pneumonic infiltration diagnosed by chest X-ray.
Table 2.
Prognostic Factors Related to Mortality according to Logistic Regression.
| Risk factors | Odds ratio | 95% CI | p value | |||
|---|---|---|---|---|---|---|
| Age ≥65 years | 77.9 | 10.7-566.0 | <0.001 | |||
| Body mass index ≤18.5 kg/m2 | 65.3 | 9.0-475.5 | <0.001 | |||
| Bilateral pneumonic infiltration on chest X-ray | 7.0 | 4.1-11.7 | <0.01 |
CI: confidence interval
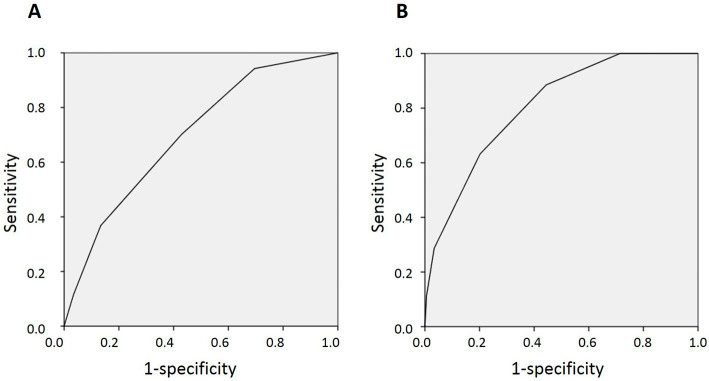
Table 3 shows the results of the three parameters in each scoring system. The mortality rates of PHAP patients increased as the severity increased. Using the A-DROP classification, the mortality rates were 4.9% in the mild cases, 21.6% in the moderate cases, 40.7% in the severe cases, and 47.6% in the very severe cases. With the I-ROAD classification, the mortality rates were 9.5% in group A, 34.7% in group B, and 36.2% in group C. With the PSI classification, the mortality rates were 0% in class II and III, 23.1% in class IV, and 44.9% in class V. We then added two factors (BMI ≤18.5 kg/m2 and bilateral pneumonic infiltration) to the A-DROP classification and established a modified A-DROP classification with scores ranging from 0 to 7. The area under the ROC curve for predicting mortality was 0.699 with the A-DROP classification and 0.807 with the modified A-DROP classification (Fig. 3).
Table 3.
The Distribution of the Outcome Measures in PHAP Patients according to the Risk Classifications.
| n | Mortality (%) | ||||||
|---|---|---|---|---|---|---|---|
| A-DROP | Mild | 103 | 5 (4.9%) | ||||
| Moderate | 231 | 50 (21.6%) | |||||
| Severe | 54 | 22 (40.7%) | |||||
| Very severe | 21 | 10 (47.6%) | |||||
| I-ROAD | Mild | 222 | 21 (9.5%) | ||||
| Moderate | 118 | 41 (34.7%) | |||||
| Severe | 69 | 25 (36.2%) | |||||
| PSI | I | 0 | 0 | ||||
| II | 45 | 0 | |||||
| III | 88 | 0 | |||||
| IV | 169 | 39 (23.1%) | |||||
| V | 107 | 48 (44.9%) |
PHAP: psychiatric hospital-acquired pneumonia
Figure 3.
The ROC curves for predicting mortality in PHAP patients based on the A-DROP and modified A-DROP classifications. The A-DROP classification (A) and modified A-DROP classification (B). The method for calculating the score is shown in the Results section. ROC: receiver operating characteristic, PHAP: psychiatric hospital-acquired pneumonia
Discussion
We showed that the mortality rate in PHAP patients tended to increase in accordance with the severity classifications. Furthermore, we identified significant risk factors for mortality among PHAP patients, including the patient age, BMI, and presence of bilateral pneumonic infiltration on chest X-ray. The modified A-DROP classification developed in the present study utilized the 5 clinical variables of the A-DROP classification with 2 additional factors (BMI ≤18.5 kg/m2 and bilateral pneumonic infiltration). Based on the ROC analysis, the utility of the modified A-DROP classification was superior to the A-DROP classification. The modified A-DROP classification thus seems to be suitable for assessing PHAP.
Many factors, such as an advanced age, dehydration, consciousness disturbance, hypoxemia, low blood pressure, malnutrition, impaired activities of daily living, and complications, have been reported to be risk factors for mortality associated with pneumonia and are included as factors in the severity assessment systems for pneumonia (6-8). The A-DROP classification was developed to classify the disease severity of CAP and contains five clinical factors: advanced age, dehydration, consciousness disturbance, hypoxemia, and low blood pressure (6). Recently, its application in the classification of NHCAP has been reported. Oshitani et al. reported that a very severe A-DROP classification was a risk factor for mortality along with complicated diabetes mellitus, hypoalbuminemia, and extensive pneumonia (9). The present findings showed that the mortality rate in PHAP patients tended to increase in accordance with the severity classification. Advanced age, underweight, and extensive pneumonic infiltration were associated with mortality; no other assumed risk factors were identified in the present study. The heterogeneity of the NHCAP patients might have contributed to the discrepancy between previous studies and our results (5).
Patient age is reported to be a risk factor of mortality due to pneumonia. Many severity assessment systems for pneumonia incorporate the patient age (6-8). The A-DROP classification and the I-ROAD classification each comprise five factors, including the patient age (men >70 years, women >75 years) (6,7). The PSI stratifies pneumonia into five classes for risk of death. If the patient age is more than 50, the patient is not stratified into the lowest risk class (8). The results of our study are consistent with these scoring systems.
Nutrition is one of the most important clinical factors influencing mortality due to infectious disease (10,11). The BMI is widely used to define the baseline nutrition status (12). Several studies have revealed that underweight is associated with a risk of death due to pneumonia (13,14). Underweight is prevalent in Japanese inpatients at psychiatric hospitals. Sugai et al. reported that Japanese inpatients with schizophrenia have a higher prevalence of underweight than the general Japanese population (13.8% vs. 7.9%) (15). We previously reported that being underweight was a risk factor for mortality among psychiatric patients with medical comorbidities (16). In the present study, the prevalence of being underweight was extremely high (90.2%), and underweight showed a high odds ratio on a multivariable analysis for determining the prognostic factors related to mortality from PHAP. Being underweight has also been reported as risk factor for the development of pneumonia (17). Underweight may be an important factor influencing the development and prognosis of pneumonia for both psychiatric and non-psychiatric patients.
The utility of chest X-ray for categorizing the severity of pneumonia has been reported (18,19). A previous meta-analysis revealed that multilobar pneumonic infiltration was an independent prognostic factor of pneumonia-related death (OR 3.1) (17). Furthermore, the severe community-acquired pneumonia (SCAP) score that was developed as a simple method for predicting in-hospital mortality adopts multilobar/bilateral pneumonic infiltration on chest X-ray as a minor criterion (20). We showed that bilateral pneumonic infiltration revealed on chest X-ray was an independent predictor of mortality due to PHAP. The rate of probable aspiration did not differ significantly between the survivors and non-survivors. Thus, bilateral pneumonic infiltration may reflect not aspiration pneumonia but advanced pneumonia. Chest X-ray may be useful not only for diagnosing PHAP but also for defining the severity of PHAP.
The present study was associated with several limitations. First, our subjects were located in the Medical Comorbidity Ward of a psychiatric hospital, which is specialized for the treatment of medical comorbidities and where many patients with severe psychotic symptoms are transferred. Accordingly, the clinical features of PHAP may be biased. Second, we treated only PHAP patients who had been transferred to our facility. As such, mild PHAP patients able to be treated at their local psychiatric hospital might not have been included. This could have influenced treatment outcome. Finally, because this was a retrospective cohort study, a prospective study to validate the modified A-DROP classification is needed.
In conclusion, our findings indicated that the mortality rate of PHAP patients tended to increase as the severity classification increased. The modified A-DROP classification, which is composed of advanced age, dehydration, consciousness disturbance, hypoxemia, low blood pressure, underweight, and extensive pneumonic infiltration, may be useful for managing the treatment of PHAP patients.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Tachimori H, Takeshima T, Kono T, Akazawa M, Zhao X. Statistical aspects of psychiatric inpatient care in Japan: based on a comprehensive nationwide survey of psychiatric hospitals conducted from 1996 to 2012. Psychiatry Clin Neurosci 69: 512-522, 2015. [DOI] [PubMed] [Google Scholar]
- 2. Lim LC, Sim LP, Chiam PC. Mortality among psychiatric inpatients in Singapore. Singapore Med J 32: 130-132, 1991. [PubMed] [Google Scholar]
- 3. Hewer W, Rössler W, Fätkenheuer B, Löffler W. Mortality among patients in psychiatric hospitals in Germany. Acta Psychiatr Scand 91: 174-179, 1995. [DOI] [PubMed] [Google Scholar]
- 4. Polednak AP. Respiratory disease mortality in an institutionalised mentally retarded population. J Ment Defic Res 19: 165-172, 1975. [DOI] [PubMed] [Google Scholar]
- 5. Kohno S, Imamura Y, Shindo Y, et al. . Clinical practice guidelines for nursing- and healthcare-associated pneumonia (NHCAP) [complete translation]. Respir Investig 51: 103-126, 2013. [DOI] [PubMed] [Google Scholar]
- 6. Miyashita N, Matsushima T, Oka M; Japanese Respiratory Society. . The JRS guidelines for the management of community-acquired pneumonia in adults: an update and new recommendations. Intern Med 45: 419-428, 2006. [DOI] [PubMed] [Google Scholar]
- 7. Seki M, Watanabe A, Mikasa K, Kadota J, Kohno S. Revision of the severity rating and classification of hospital-acquired pneumonia in the Japanese Respiratory Society guidelines. Respirology 13: 880-885, 2008. [DOI] [PubMed] [Google Scholar]
- 8. Fine MJ, Auble TE, Yealy DM, et al. . A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 336: 243-250, 1997. [DOI] [PubMed] [Google Scholar]
- 9. Oshitani Y, Nagai H, Matsui H, Aoshima M. Reevaluation of the Japanese guideline for healthcare-associated pneumonia in a medium-sized community hospital in Japan. J Infect Chemother 19: 579-587, 2013. [DOI] [PubMed] [Google Scholar]
- 10. Van den, Broeck J, Eeckels R. Effect of malnutrition on child mortality. Lancet 344: 273, 1994. [DOI] [PubMed] [Google Scholar]
- 11. Beisel WR. History of nutritional immunology: introduction and overview. J Nutr 122: 591-596, 1992. [DOI] [PubMed] [Google Scholar]
- 12. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser 854: 1-452, 1995. [PubMed] [Google Scholar]
- 13. Corrales-Medina VF, Valayam J, Serpa JA, Rueda AM, Musher DM. The obesity paradox in community-acquired bacterial pneumonia. Int J Infect Dis 15: e54-e57, 2011. [DOI] [PubMed] [Google Scholar]
- 14. LaCroix AZ, Lipson S, Miles TP, White L. Prospective study of pneumonia hospitalizations and mortality of U.S. older people: the role of chronic conditions, health behaviors, and nutritional status. Public Health Rep 104: 350-360, 1989. [PMC free article] [PubMed] [Google Scholar]
- 15. Sugai T, Suzuki Y, Yamazaki M, et al. . High prevalence of underweight and undernutrition in Japanese inpatients with schizophrenia: a nationwide survey. BMJ Open 5: e008720, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Haga T, Ito K, Ono M, et al. . Underweight and hypoalbuminemia as risk indicators for mortality among psychiatric patients with medical comorbidities. Psychiatry Clin Neurosci 71: 807-812, 2017. [DOI] [PubMed] [Google Scholar]
- 17. Phung DT, Wang Z. Risk of pneumonia in relation to body mass index in Australian Aboriginal people. Epidemiol Infect 141: 2497-2502, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fine MJ, Smith MA, Carson CA, et al. . Prognosis and outcomes of patients with community-acquired pneumonia. A meta-analysis. JAMA 275: 134-141, 1996. [PubMed] [Google Scholar]
- 19. Leroy O, Santré C, Beuscart C, et al. . A five-year study of severe community-acquired pneumonia with emphasis on prognosis in patients admitted to an intensive care unit. Intensive Care Med 21: 24-31, 1995. [DOI] [PubMed] [Google Scholar]
- 20. España PP, Capelastegui A, Gorordo I, et al. . Development and validation of a clinical prediction rule for severe community-acquired pneumonia. Am J Respir Crit Care Med 174: 1249-1256, 2006. [DOI] [PubMed] [Google Scholar]