Abstract
On Earth, tissue weight generates compressive forces that press on body structures and act on the walls of vessels throughout the body. In microgravity, tissues no longer have weight, and tissue compressive forces are lost, suggesting that individuals who weigh more may show greater effects from microgravity exposure. One unique effect of long-duration microgravity exposure is spaceflight-associated neuroocular syndrome (SANS), which can present with globe flattening, choroidal folds, optic disk edema, and a hyperopic visual shift. To determine whether weight or other anthropometric measures are related to ocular changes in space, we analyzed data from 45 individual long-duration astronauts (mean age 47, 36 male, 9 female, mean mission duration 165 days) who had pre- and postflight measures of disk edema, choroidal folds, and manifest ocular refraction. The mean preflight weights of astronauts who developed new choroidal folds [78.6 kg with no new folds vs. 88.6 kg with new folds (F = 6.2, P = 0.02)] and disk edema [79.1 kg with no edema vs. 95 kg with edema (F = 9.6, P = 0.003)] were significantly greater than those who did not. Chest and waist circumferences were also significantly greater in those who developed folds or edema. The odds of developing disk edema or new choroidal folds were 55% in the highest- and 9% in the lowest-weight quartile. In this cohort, no women developed disk edema or choroidal folds, although women also weighed significantly less than men [62.9 vs. 85.2 kg (F = 53.2, P < 0.0001)]. Preflight body weight and anthropometric factors may predict microgravity-induced ocular changes.
Keywords: anthropometry, body weight, spaceflight-associated neuroocular syndrome
INTRODUCTION
Two of the main effects of microgravity exposure are the removal of hydrostatic gradients throughout the body and the elimination of tissue compressive forces produced by the weight of tissues (3). On Earth, tissue compressive forces increase with body weight, and hydrostatic pressures grow with the height of the fluid-filled structure (e.g., blood vessel) (3). This leads to the hypothesis that changes due to microgravity will also be proportionally larger for individuals with a greater preflight weight and body size, because the changes in tissue and vascular pressures will be greater. If this is true, then preflight body weight might be predictive of microgravity-related changes.
One area where this may be particularly relevant is spaceflight-associated neuroocular syndrome (SANS). This syndrome is occurring in a subset of long-duration astronauts and includes ocular structural changes, such as globe flattening, choroidal folds, and optic disk edema (9, 10). These structural changes are also associated with a hyperopic shift in vision (9, 11). It has been difficult to predict who will develop this syndrome. Female sex appears to be protective. Also, some evidence suggests that differences in one-carbon metabolism may be linked to development of SANS in astronauts (2, 8). However, whether development of SANS is related to preflight body weight and body size has not been explored. To test this hypothesis, we used data collected from National Aeronautics and Space Administration (NASA) astronauts compiled by the Lifetime Surveillance of Astronaut Health.
METHODS
Subjects.
Use of the data was approved by the NASA-Johnson Space Center Institutional Review Board, the Lifetime Surveillance of Astronaut Health review board, and the Committee for the Protection of Human Subjects at Dartmouth College. Data from 50 astronauts who had made long-duration flights were analyzed. For the five astronauts who had made repeat long-duration flights, only the first flight was included, yielding 45 individual astronauts in the cohort. The final cohort is described in Table 1.
Table 1.
Characteristics of the astronauts
| Astronauts |
||||
|---|---|---|---|---|
| Male (n = 36) | Female (n = 9) | Total (n = 45) | P Value (Male vs. Female) | |
| Mission duration, days | 166 ± 31 | 160 ± 31 | 165 ± 30 | 0.6 |
| Preflight weight, kg | 85.2 ± 8.7 | 62.9 ± 5.2 | 80.7 ± 12.1 | <0.0001 |
| Height, cm | 176.2 ± 5.8 | 167.8 ± 2.5 | 174.6 ± 6.3 | 0.0001 |
| Circumference, cm | ||||
| Chest | 104.5 ± 6.8 | 89.1 ± 3.5 | 101.4 ± 8.8 | <0.0001 |
| Waist | 89.4 ± 6.5 | 71.1 ± 4.2 | 85.8 ± 9.6 | <0.0001 |
| Head | 58.6 ± 2.3 | 55.5 ± 2.2 | 58.0 ± 2.6 | 0.0006 |
Values are means ± SD.
Data.
The data included mission duration, sex, preflight body weight, and height, as well as pre- and postflight ocular findings, including manifest refraction, presence or absence of disk edema, presence of choroidal folds, and Clinical Practice Guideline (CPG) classification (1). Anthropometric data were provided from the astronaut’s measurements taken when the individual astronaut was fitted for a space suit. Measurements included bitragion-inion arc, axilla height, neck circumference, waist circumference, chest circumference, sagittal arch, head circumference, bitragion coronal arc, head length, and head breadth.
Statistics.
The astronauts were grouped in three ways based on the following factors: 1) whether they had new choroidal folds after the flight (one astronaut had a choroidal fold preflight), 2) whether they had disk edema postflight, or 3) whether they had disk edema and/or new choroidal folds (noted as “edema/folds”). In this cohort, 6 astronauts developed disk edema, 10 developed new choroidal folds, and 11 developed new folds or edema. Only 25 astronauts had a CPG classification, and the main difference between a low-CPG group (levels 0, 1, and 2) and a high-CPG group (levels 3 and 4) was the presence of disk edema. Therefore, CPG group was not used in the analyses. The refraction closest to launch was used as the preflight value, and the first postflight measurement was used as the postflight value. For the refraction measurements, the spherical equivalent was calculated using the following formula: spherical equivalent = sphere + (cylinder/2) (6). The main statistical analysis for the anthropometric data was a one-way ANOVA for each anthropometric measure (e.g., weight and height), with each individual anthropometric measure as the continuous variable and the presence or absence of edema, new folds, or edema/folds as categorical variables. In this cohort, none of the women had disk edema or new choroidal folds, nor did any of the women have a CPG classification >2. The women also weighed significantly less than the men. Therefore, to ensure that the results did not solely reflect the weight differences between men and women, the analysis described above was also performed within the male cohort only. A bidirectional (forward/backward) step-wise logistic regression (MATLAB function “stepwiseglm”) was done on the anthropometric data with the presence of either folds or edema as the response variable and the anthropometric variables that were shown to be statistically significant as predictor variables. The refraction data were analyzed by multiple linear regression, with change in refraction as the response variable and preflight weight and sex as predictor variables. To assess the odds of developing folds or edema by weight, the cohort was divided into quantiles by weight using the probability intervals of 0.25, 0.5, and 0.75. The odds of having either folds or edema in each quantile were calculated. The analyses were carried out using MATLAB version R2017b.
RESULTS
Table 2 summarizes the main results for the anthropometric measures with the presence of either disk edema or new choroidal folds used as the categorical (grouping) variable. For the overall cohort, preflight weight, waist circumference, and chest circumference were significantly greater in those who developed disk edema or choroidal folds (edema/folds). This was still true when only the male cohort was analyzed. When the data were analyzed using disk edema or new choroidal folds separately as individual grouping variables, the results were similar. For disk edema alone, weight, waist circumference, and chest circumference were significantly greater in those who developed edema (F = 9.6, P = 0.003 for weight; F = 6.6, P = 0.014 for waist circumference; F = 5.1, P = 0.03 for chest circumference), which was also true for new choroidal folds (F = 6.2, P = 0.017 for weight; F = 4.3, P = 0.04 for waist circumference; F = 6.3, P = 0.016 for chest circumference). When the men alone were analyzed, the results were similar, although the difference for chest circumference was no longer significant for edema alone. The pre- to postflight refraction data showed a positive correlation between weight and refractive change (t = 2.6, P = 0.012) but no relationship to sex. Regression analysis on the other anthropometric variables did not show any other relationships, except a tendency for larger head circumference to be related to greater refractive change (t = 1.9, P = 0.07).
Table 2.
Overall results from the study
| Entire Cohort |
Men Only |
||||
|---|---|---|---|---|---|
| Measure | Edema/folds | No edema/folds | F, P value | No edema/folds | F, P value |
| Preflight weight, kg | 89.5 ± 10.5 | 77.9 ± 11.4 | 9.0, 0.005 | 83.3 ± 7.3 | 4.2, 0.05 |
| Height, cm | 177.1 ± 5.5 | 173.7 ± 6.4 | 2.5, 0.12 | 175.8 ± 6.0 | 0.4, 0.54 |
| Axilla height, cm | 132.7 ± 3.8 | 126.7 ± 21.8 | 0.4, 0.51 | 126.6 ± 26.3 | 0.3, 0.58 |
| Circumference, cm | |||||
| Waist | 92.6 ± 8.1 | 83.6 ± 9.1 | 8.8, 0.005 | 88.0 ± 5.3 | 4.1, 0.05 |
| Chest | 107.9 ± 6.7 | 99.4 ± 8.5 | 9.3, 0.004 | 103.1 ± 6.4 | 4.3, 0.05 |
| Head | 59.0 ± 1.7 | 58.0 ± 2.8 | 1.9, 0.17 | 58.5 ± 2.5 | 0.3, 0.60 |
| Neck | 40.6 ± 2.9 | 38.9 ± 3.6 | 2.2, 0.15 | 40.5 ± 2.2 | 0.02, 0.90 |
| Arc, cm | |||||
| Bitragion-coronal | 32.5 ± 2.2 | 32.1 ± 4.2 | 0.05, 0.82 | 32.5 ± 4.8 | 0.0, 0.98 |
| Bitragion-inion | 22.2 ± 1.7 | 23.0 ± 5.5 | 1.3, 0.26 | 24.3 ± 5.6 | 1.4, 0.25 |
| Sagittal arch, cm | 35.1 ± 3.5 | 36.5 ± 4.0 | 1.1, 0.31 | 36.4 ± 2.0 | 2.0, 0.17 |
| Head breadth, cm | 15.7 ± 0.8 | 15.5 ± 0.5 | 0.8, 0.38 | 15.6 ± 0.4 | 0.05, 0.82 |
| Head length, cm | 20.4 ± 0.7 | 20.0 ± 1.3 | 1.2, 0.29 | 20.4 ± 1.3 | 0.02, 0.89 |
Values are means ± SD. Body weight, waist circumference, and chest circumference were significantly greater in astronauts who developed disk edema or choroidal folds. This was still true for male astronauts when their data were analyzed separately.
The bidirectional step-wise logistic regression analysis was used to assess whether there were any interactions between the variables that had been shown to be significant or nearly significant (head circumference) in the ANOVA and regression analyses. The presence of new choroidal folds or edema was used as the response variable. Weight, waist circumference, chest circumference, head circumference, and sex were included as candidate predictor variables for building the step-wise model. The final model included only weight (t = 3.0, P = 0.004), suggesting that addition of other variables cannot significantly increase the likelihood of the logistic regression model.
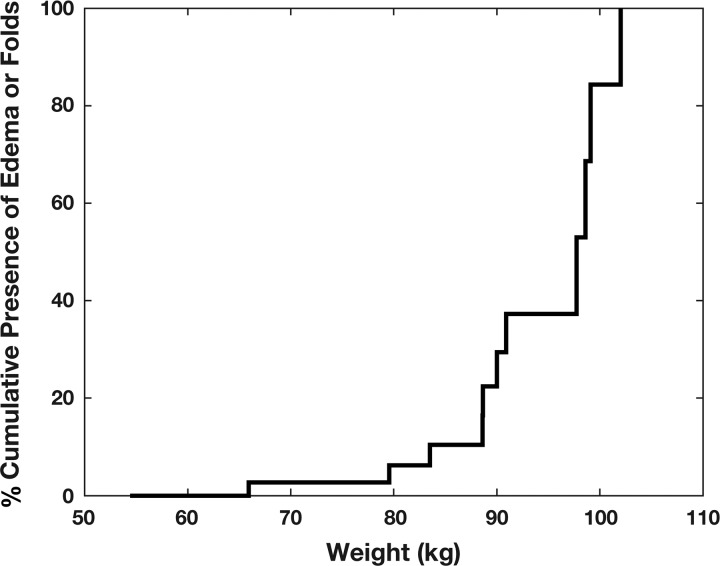
Figure 1 shows the cumulative presence of either disk edema or new choroidal folds by weight in those who developed those ocular changes. The results when the cohort was divided into quantiles by weight are shown in Table 3. The odds of developing either disk edema or ocular folds were >50% in the highest-weight quantile. In this overall cohort, no women developed either disk edema or choroidal folds. When only the men in the cohort were analyzed, however, this was still true. The women weighed significantly less than the men [62.7 vs. 85 kg (F = 53.2, P < 0.0001)] on average.
Fig. 1.
Cumulative presence of disk edema or new choroidal folds as a function of body weight. Development of eye findings increased markedly at ~90 kg.
Table 3.
Odds of disk edema or new choroidal folds by weight quantile for the entire cohort and for men only
| Odds |
||
|---|---|---|
| Quantile | Entire cohort | Men only |
| 1st (lowest) | 0.09 | 0.13 |
| 2nd | 0.09 | 0.20 |
| 3rd | 0.25 | 0.33 |
| 4th (highest) | 0.55 | 0.56 |
DISCUSSION
The removal of all tissue compressive forces is a unique effect of microgravity, and this effect is greater the more a person weighs (5). The ocular changes during long-duration spaceflight are also unique to microgravity (i.e., these changes have not been seen in any ground-based analog of microgravity exposure), and it is reasonable to postulate that these ocular changes might be related to body weight or body size. The results from this study show a strong relationship between body weight and development of ocular changes in space.
Microgravity has been shown to produce unique physiological effects that cannot be replicated in ground-based models. One example is the reduction in central and peripheral venous pressures that occurs in microgravity (3, 4). Before central venous pressure was measured directly in space, a common assumption was that central venous pressure would be increased due to the fluid shift that occurs in microgravity. When central venous pressure was measured directly, however, it did not increase and was actually reduced below supine levels. The most likely explanation was that, without the compressive forces provided by the tissue weight on the walls of veins and venules, vascular capacity was increased and unstressed volume (i.e., the volume of blood contained at zero pressure) increased. The loss of tissue weight increased the compliance of the vascular system. Also, any compression caused by the weight of the chest wall would be lost in microgravity.
The possibility exists that the loss of tissue weight and hydrostatic gradients that occur in space may also be very relevant to SANS. Although SANS shares some characteristics with the terrestrial idiopathic elevated intracranial pressure syndrome, it differs in some fundamental ways: 1) direct measurements of intracranial pressure in short-term microgravity do not show increases in intracranial pressure; and 2) there is no evidence that head-down-tilt bedrest produces ocular changes consistent with SANS (7). Other hypotheses that consider the effects of the loss of tissue compressive forces are needed for SANS.
These data also suggest that body size may be one reason why fewer women develop ocular changes. On average, women weigh less than men, and this was true in this cohort. Nevertheless, even when the analysis was done with only the men in the cohort, the effect of body weight was still significant.
Limitations.
Although body weight was determined before each astronaut’s flight in this data set, the other anthropometric measures were not. Although many of these measurements are unlikely to change significantly over time (e.g., head circumference), other measures, such as waist and chest circumference, could change, and there was no control for these effects in this study. Also, although cycloplegic refraction measurements would be preferred for the refraction analysis, this was not available on a sufficient number of subjects. Nevertheless, the refractive changes showed the same trends and results as the other measures (i.e., disk edema and new choroidal folds).
In conclusion, body weight shows a strong relationship to the subsequent development of ocular changes in space.
GRANTS
This work was supported by Grant NNX13AD35A to the New Hampshire NASA Experimental Program to Stimulate Competitive Research and by the National Space Biomedical Research Institute through Grant NCC 9-58.
DISCLAIMERS
The funding organizations had no role in the design or conduct of this research.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the authors.
AUTHOR CONTRIBUTIONS
J.C.B. conceived and designed research; J.C.B., S.D.P., A.P.A., and J.G. analyzed data; J.C.B., S.D.P., A.P.A., A.B.C., and V.A.-L. interpreted results of experiments; J.C.B. drafted manuscript; J.C.B., S.D.P., A.P.A., A.B.C., V.A.-L., J.G., and A.M.F. edited and revised manuscript; J.C.B., S.D.P., A.P.A., A.B.C., V.A.-L., J.G., and A.M.F. approved final version of manuscript.
ACKNOWLEDGMENTS
The authors thank Wafa Taiym and Sara Mason (Lifetime Surveillance of Astronaut Health Program, NASA Johnson Space Center) for gathering and providing data for this study.
REFERENCES
- 1.Alexander DJ, Gibson CR, Hamilton DR, Lee SMC, Mader TH, Otto CA, Oubre CM, Pass AF, Platts SH, Scott JM, Smith SM, Stenger MB, Westby CM, Zanello SB. Risk of Spaceflight-Induced Intracranial Hypertension and Vision Alterations (12 July 2012). Houston, TX: NASA, 2012. [Google Scholar]
- 2.Anderson AP, Babu G, Swan JG, Phillips SD, Knaus DA, Toutain-Kidd CM, Zegans ME, Fellows AM, Gui J, Buckey JC. Ocular changes over 60 minutes in supine and prone postures. J Appl Physiol 123: 415–423, 2017. doi: 10.1152/japplphysiol.00687.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buckey JC. Central venous pressure. In: Gravity and the Lung: Lessons from Microgravity edited by Prisk GK, West JB, Paiva M. New York: Marcel Dekker, 2001. doi: 10.1201/b15295-11. [DOI] [Google Scholar]
- 4.Buckey JC Jr, Gaffney FA, Lane LD, Levine BD, Watenpaugh DE, Wright SJ, Yancy CW Jr, Meyer DM, Blomqvist CG. Central venous pressure in space. J Appl Physiol (1985) 81: 19–25, 1996. doi: 10.1152/jappl.1996.81.1.19. [DOI] [PubMed] [Google Scholar]
- 5.Buckey JC, Phillips SD, Anderson AP, Chepko AB, Archambault-Leger V, Masterova KS, Fellows AM, Cowan DR. The importance of tissue weight and tissue compressive forces in human spaceflight. In: 68th International Astronautical Congress. Adelaide, Australia: International Astronautical Federation, 2017. [Google Scholar]
- 6.Kolker RJ. Subjective refraction and prescribing glasses, the number one (or number two). In: Guide to Practical Techniques and Principles. St. Paul, MN: Joint Commission on Allied Health Personnel in Ophthalmology, 2014. [Google Scholar]
- 7.Lawley JS, Petersen LG, Howden EJ, Sarma S, Cornwell WK, Zhang R, Whitworth LA, Williams MA, Levine BD. Effect of gravity and microgravity on intracranial pressure. J Physiol 595: 2115–2127, 2017. doi: 10.1113/JP273557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee AG, Tarver WJ, Mader TH, Gibson CR, Hart SF, Otto CA. Neuro-ophthalmology of space flight. J Neuroophthalmol 36: 85–91, 2016. doi: 10.1097/WNO.0000000000000334. [DOI] [PubMed] [Google Scholar]
- 9.Mader TH, Gibson CR, Pass AF, Kramer LA, Lee AG, Fogarty J, Tarver WJ, Dervay JP, Hamilton DR, Sargsyan A, Phillips JL, Tran D, Lipsky W, Choi J, Stern C, Kuyumjian R, Polk JD. Optic disc edema, globe flattening, choroidal folds, and hyperopic shifts observed in astronauts after long-duration space flight. Ophthalmology 118: 2058–2069, 2011. doi: 10.1016/j.ophtha.2011.06.021. [DOI] [PubMed] [Google Scholar]
- 10.Otto C, Ploutz-Snyder R, Samuels B, Gibson C, Sargsyan A, Patel N, Riascos R, Garcia K, Kramer L, Alexander D, Lee S. The prospective observational study of ocular health in International Space Station (ISS) sstronauts: the visual impairment intracranial pressure risk (VIIP). In: NASA Human Research Program Investigator's Workshop Galveston, TX: NASA, 2016. [Google Scholar]
- 11.Taibbi G, Cromwell RL, Kapoor KG, Godley BF, Vizzeri G. The effect of microgravity on ocular structures and visual function: a review. Surv Ophthalmol 58: 155–163, 2013. doi: 10.1016/j.survophthal.2012.04.002. [DOI] [PubMed] [Google Scholar]