Sir,
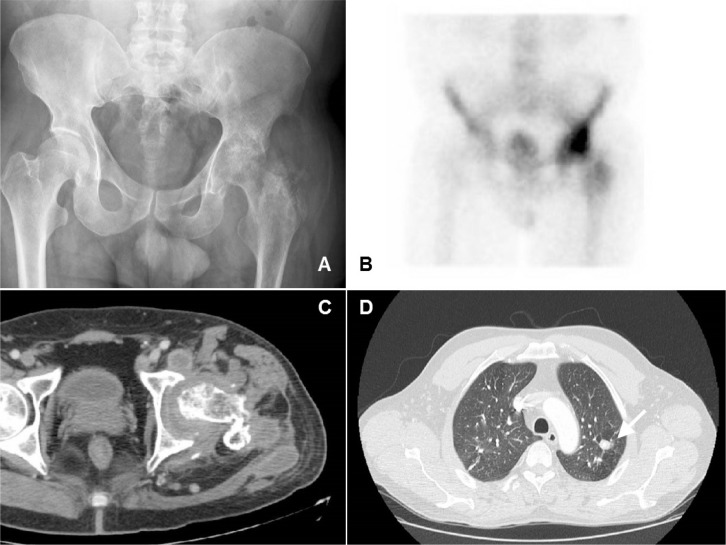
A 54 year-old male patient, born in Ecuador, without any previous disease had been suffering from left hip pain and lameness that did not allow him to do his job as a farmer. Three cutaneous fistulas were persistently suppurating a caseous material, whose samples had been initially sent for bacterial culture and had yielded a coagulase-negative Staphylococcus that was treated with several antibiotics including fluoroquinolones. He had no fevers, sweats or gain loss. Three years after his initial consult, the patient was re-evaluated with a hip X-ray, hip CT-scan and Tc99m-scintigraphy. They showed a destructive infectious process affecting the left femur and acetabular cavity with loss of bone substance and collections in the thigh root (figure 1A, B, and C). A surgical biopsy was performed and sent for bacterial culture (negative) and mycobacterial culture. This last study allowed highlighting the presence of acid alcohol fast bacilli (AAFB) in the Ziehl-Neelsen (ZN) method and detection of the presence of DNA of Mycobacterium tuberculosis through nucleic acid amplification test (NAAT) (Fluorotype MTB, Hain Lifescience). Mutations of resistance to isoniazid and rifampicin were not detected by the technique Genotype MTBDRplus (Hain Lifescience). The antibiogram performed in the system BD Bactec MGIT 960 (Becton Dickinson) showed sensitivity for the five antibiotics tested: streptomycin (STR), isoniazid (INH), rifampin (RIF), ethambutol (EMB), and pyrazinamide (PZA).
Figure 1.
(A) Hip X-ray indicating destruction of the left proximal femur and loss of the joint space. (B) Tc99m-scintygraphy revealing chronic inflammation in acetabulum and femoral head. (C) Destruction with loss of bone density in the left proximal femur and collections in the thigh root in a hip CT-scan. (D) Chest CT-scan revealing an upper left lobe 15 mm nodule with central calcification, consistent with a tuberculous granuloma (arrow).
The patient started to be treated with 4 first-line antituberculosis drugs (INH, RIF, PZA and EMB). A chest-CT scan was performed and a 15 mm upper-left lobe nodule with central calcification was found, consistent with a tuberculous granuloma (figure 1D). The patient had no respiratory symptoms so no sputum for culture could be collected. An aggressive surgery was performed: resection arthroplasty and surgical debridement of abscesses. The patient is still under antituberculosis treatment with rifampicin and isoniazid (27 months to day). Antituberculosis treatment has not yet been stopped because there was a delay in surgical treatment, all caseous material could not be removed and osteomyelitis focuses could have remained after surgery. Despite a positive clinical, analytical and radiological evolution after surgery, it has not been so fast as to ensure the microbiological cure with a standard treatment course.
Osteoarticular tuberculosis accounts for 10-11% of all extrapulmonary tuberculosis and 1-3% of all tuberculosis diagnoses [1]. Tuberculous arthritis is the second cause of osteoarticular tuberculosis after vertebral tuberculosis. Tuberculous arthritis usually affects joints that support large weight such as the hip or knee, and is usually a monoarticular condition. The delay in the diagnosis can be related to the assumption that the skin fistula colonizer is a colonizing fungus or bacteria, as in our case. In these cases a biopsy is mandatory in order to send samples for mycobacterial culture and PCR, in addition to routine bacterial cultures [2]. Diagnostic of osteoarticular tuberculosis can be challenging so a high index of suspicion is necessary and using deep biopsies not only for bacterial cultures, but also for mycobacterial cultures and PCR could help reducing delays in diagnosis [3]. Despite major advances in the diagnosis of mycobacterial infections, microscopic examination for AAFB remains a primary tool because it identifies infections with positive-AAFB smear cases. However, it is of less utility for paucibacillary disease such as in pediatric patients, HIV and those with extrapulmonary disease. Mycobacterial culture has a high sensitivity and is the test of choice for the microbiological diagnosis of tuberculosis. Although the specificity of NAAT is very high, sensitivities vary widely and depend on both the AAFB smear status of the specimen (positive or negative) and the origin of the sample. The results take 1-2 days. Its use is indicated when the degree of suspicion is moderate to high [4]. A few studies have shown the effectiveness of NAAT in the diagnosis of extrapulmonary tuberculosis, in which the reported sensitivities ranged from 87.3% to 97 % (positive ZN) to 68% (negative ZN) and the specificity was over 97% [4]. Early determination of the identity and sensitivy of the mycobacteria is very important not just from a public health and epidemiological perspective, but also to guide the treatment and management [5].
Current Spanish consensus document about the treatment of tuberculosis recommend a 9-month standard treatment for tuberculous spondylitis and there is no specific pattern for tuberculous osteoarthritis of other location [6]. In addition, there is no optimal duration of therapy for patients with bone and soft tissue tuberculosis in which all caseous material cannot be removed with surgery and all studies about antituberculous treatment duration for osteoarticular tuberculosis have been performed in spinal tuberculosis. Some authors recommend to extent antituberculous treatment beyond the recommended 6-9 months in patients with a significant burden of disease, like in our case [2,7]. A logical approach would be to assess the effectiveness of the treatment by periodic blood tests and a CT-scan. PET-CT could be a useful tool to monitor the effectiveness of the treatment, and there is an increasing evidence about it [8–10]. In any case, it is not usually necessary to use such a long treatment pattern and most cases could benefit from a shorter treatment.
We believe that this may be an illustrative case of this extrapulmonary manifestation of tuberculosis, with serious consequences in terms of severity of infection and subsequent physical disability.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest
FUNDING
None to declare
REFERENCES
- 1.Malaviya AN, Kotwal PP. Arthritis associated with tuberculosis. Best Pract Res Clin Rheumatol 2003;17:319–43. PMID: . [DOI] [PubMed] [Google Scholar]
- 2.Watts HG, Lifeso RM. Tuberculosis of bones and joints. J Bone Joint Surg Am 1996;78:288–98. PMID: . [DOI] [PubMed] [Google Scholar]
- 3.Broderick C, Hopkins S, Mack DJF, Aston W, Pollock R, Skinner JA, et al. . Delays in the diagnosis and treatment of bone and joint tuberculosis in the United Kingdom. Bone Joint J 2018;100–B:119–24. PMID: . [DOI] [PubMed] [Google Scholar]
- 4.Forbes BA, Hall GS, Miller MB, Novak SM, Rowlinson M-C, Salfinger M, et al. . Practice Guidelines for Clinical Microbiology Laboratories: Mycobacteria. Clin Microbiol Rev 2018;31. PMID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO | WHO endorses new rapid tuberculosis test . WHO. 2010. Available at: hppt:// www.who.int/mediacentre/news/releases/2010/tb_test_20101208/en/ [Google Scholar]
- 6.González-Martín J, García-García JM, Anibarro L, Vidal R, Esteban J, Blanquer R, et al. . Documento de consenso sobre diagnóstico, tratamiento y prevención de la tuberculosis. Arch Bronconeumol 2010;46:255–74. PMID: . [DOI] [PubMed] [Google Scholar]
- 7.Hogan JI, Hurtado RM, Nelson SB. Mycobacterial Musculoskeletal Infections. Infect Dis Clin North Am 2017;31:369–82. PMID: . [DOI] [PubMed] [Google Scholar]
- 8.Cho YS, Chung DR, Lee EJ, Kim BT, Lee KH. 18F-FDG PET/CT in a case of multifocal skeletal tuberculosis without pulmonary disease and potential role for monitoring treatment response. Clin Nucl Med 2014;39:980–3. PMID: . [DOI] [PubMed] [Google Scholar]
- 9.Stelzmueller I, Huber H, Wunn R, Hodolic M, Mandl M, Lamprecht B, et al. . 18F-FDG PET/CT in the Initial Assessment and for Follow-up in Patients With Tuberculosis. Clin Nucl Med 2016;41:E187–94. PMID: . [DOI] [PubMed] [Google Scholar]
- 10.Montes Ruiz-Cabello M, Guirao Arrabal E, Caminero Luna JA. PET/CT for evaluation of the response to therapy and follow-up of patients with tuberculosis. Med Clin (Barc) 2017;149. PMID: . [DOI] [PubMed] [Google Scholar]