Abstract
Introduction:
The epidemiology of chronic pain in youth has been increasingly documented over the past decade. However, the precipitating events associated with the onset of pediatric chronic pain are not well studied.
Objectives:
Understanding the events that precede the onset of pain, and are reported by patients as germane to the early stages of their pain, may add one piece to the puzzle of the causal etiology of pediatric chronic pain disorders.
Methods:
We conducted a retrospective chart review of 320 young people attending a tertiary care chronic pain clinic with musculoskeletal chronic pain.
Results:
Approximately two-thirds of patients reported a precipitating event for their pain; injury was the most commonly reported event, followed by a chronic disease, then an infection or illness. Surgery was the least commonly reported event. About one-third of patients did not report any precipitating event for their pain. Patients with neuropathic pain were even more likely to report a precipitating event compared to those with localized and diffuse musculoskeletal pain. Patients with localized musculoskeletal pain and neuropathic pain were most likely to report an injury, whereas patients with diffuse musculoskeletal pain were most likely to report a chronic disease. We found little to no evidence that the presence or type of precipitating event was associated with patients' psychological or physical functioning.
Conclusion:
This study adds to the epidemiological evidence base for pediatric chronic pain disorders.
Keywords: Precipitating event, Pediatric chronic pain, Injury, Epidemiology, Child, Adolescent
1. Introduction
The epidemiology of chronic pain in youth has been increasingly documented over the past decade. Population-based cohort studies have revealed that 25% to 37.3% of children and adolescents report chronic pain, and 5.1% report moderate or severe chronic pain, which impacts their psychological, physical, and social functioning.16,27,32 Also, well described are prevalence rates across different chronic pain sites: headache and abdominal pains are common in early childhood, whereas musculoskeletal pains (including limb and back pain) are most common through mid-late childhood and adolescence.27 In one school-based study, musculoskeletal pains accounted for 64% of all the pains that were reported by young people.30 Less studied, however, are the precipitating events associated with the onset of pediatric chronic pain. Here, we define a precipitating event as an incident temporally and conceptually tied to the onset of an individual's pain. Investigating events that precede the onset of chronic pain and are reported by patients as germane to the early stages of their pain may add one piece to the puzzle of the causal etiology of pediatric chronic pain disorders and may be informative for preventive strategies.
Injury, surgery, illness, infection, and chronic disease are commonly recognized as events preceding the chronic pain onset in adults. Evidence for such precipitating events is taken from prospective, retrospective, and disease-cohort studies, mostly in populations with musculoskeletal and neuropathic pain. For example, regarding injury, an early study found that 24% of individuals with fibromyalgia reported experiencing physical trauma in the 6 months before the onset of their disease.1 Regarding surgery, approximately 20% of adults who presented to a chronic pain clinic implicated surgery as one of the causes of their pain, with half of these patients listing it as the sole cause.9 There is also evidence that illness, infection, and chronic disease are associated with chronic pain, and with neuropathic pain in particular. For example, herpes zoster,17 lyme disease,23 HIV infection,14 multiple sclerosis,26 and cancer4 are conditions associated with neuropathic pain problems.
On the other hand, a growing body of data also indicates that, in many cases, there is no identifiable cause for the onset of chronic pain. For example, Almeida et al.2 found that 6% of adults with chronic pelvic pain had no self-identified cause. In the large European survey described above,3 12% of respondents reported that they did not know the cause of their pain. Even for complex regional pain syndrome (CRPS), which is generally considered a neuropathic musculoskeletal condition in which a specific event precedes the onset, a study by de Rooij et al.11 found that 7% of patients report a spontaneous onset of their pain.
Despite this growing evidence base, a number of questions remain outstanding. First, the majority of data is from adult populations. We know very little about those events associated with the onset of chronic pain in youth. Second, little is known about whether experiencing a precipitating event, and whether different types of precipitating events, are associated with differing demographic or clinical characteristics, or with different psychofunctioning profiles in youth. This information could be important for taking a precision-medicine approach to understanding risk in pediatric chronic pain and stratifying care according to individual needs.
The aim of this study was to contribute to the epidemiological evidence base for precipitating events in pediatric chronic pain disorders, focusing on children and adolescents with chronic musculoskeletal pain. Specifically, we conduct a retrospective chart review to examine the prevalence, and clinical and psychofunctional correlates of precipitating events for children and adolescents attending a tertiary care chronic pain clinic.
2. Methods
2.1. Participants
A retrospective chart review was performed on 320 children and adolescents, aged 6 to 18 years, who presented to a tertiary care chronic pain clinic in the northeast United States (see Table 1 for more detailed characterization of the sample). There were 245 girls (76.6%) and 75 boys (23.4%). Three-quarters of patients were accompanied by their mothers (75.0%). All patients included in this chart review were referred to the clinic with a primary musculoskeletal pain complaint. We grouped chronic pain diagnoses into 3 major categories: localized musculoskeletal pain (single limb or joint pain, low back pain, and chest pain), diffuse musculoskeletal pain (widespread musculoskeletal pain, postural orthostatic tachycardia syndrome with musculoskeletal pain, Ehlers–Danlos syndrome, joint hypermobility, and fibromyalgia), and neuropathic pain (CRPS, neuralgia, and pain amplification disorder). We included neuropathic pain conditions such as CRPS within the broader category of musculoskeletal pain to be comparable with other conceptualizations of chronic musculoskeletal pain in youth.7 The median pain duration in the full sample was 12 months (range = 1–209 months). Although a small number of patients reported experiencing pain for less than 3 months (and therefore do not meet commonly accepted criteria for chronic pain), we included these patients to be representative of the cohort of children and adolescents attending the tertiary care clinic.
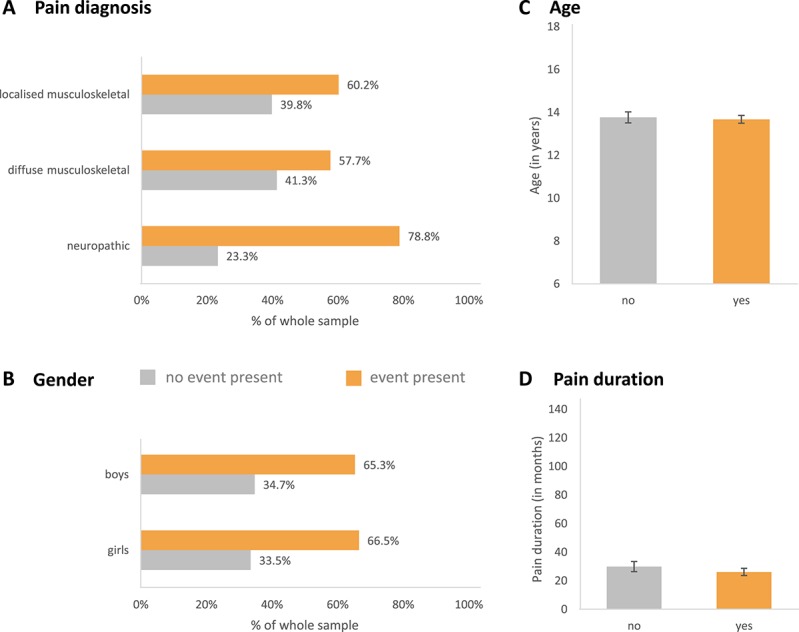
Table 1.
Sample demographics and clinical characteristics.
2.2. Procedures and precipitating event coding
Children and adolescents were evaluated at the tertiary care clinic by a physician, physical therapist, and psychologist before receiving a treatment plan. At the evaluation, patients and a parent (75% mothers) completed a clinical interview in which they were asked to declare any events that they believed precipitated the child's pain, or to declare whether they could not identify any precipitating event for the child's pain. Patients also completed questionnaire measures on pain, psychological, and physical functioning as part of this evaluation. All precipitating events were coded from patients' medical record by the first author (A.J.B.). To ensure coding reliability, 3 research students also acted as secondary coders, coding a portion of the medical records each. Interrater reliability tests were performed for the presence of precipitating event category, as well as for the type of precipitating event category. For the presence of precipitating event category, the observed unweighted kappa value was 0.81 at a 95% confidence interval (0.65–0.97). For the type of precipitating event category, the observed unweighted kappa value was 0.84 at a 95% confidence interval (0.72–0.96). Any discrepancies were discussed, and all final event codes were agreed on by multiple coders as well as the senior author (L.E.S.), who is a registered clinical psychologist working with young people with chronic pain. There were 5 event categories used for the purposes of this study:
(1) Injury (eg, sports-related injuries, automobile accident, and rolled/sprained ankle);
(2) Surgery (eg, cyst removal, gallbladder removal, and knee surgery);
(3) Infection/illness (eg, ear infections, sinus infections, and influenza);
(4) Chronic disease (eg, Ehler–Danlos syndromes, juvenile arthritis, scoliosis, osteomyelitis, and Sever disease);
(5) No event identified.
2.3. Measures
2.3.1. Typical pain intensity
Participants provided their typical pain intensity (in the past week) on a standard 11-point numeric rating scale (0 [no pain] to 10 [worst possible pain]).5
2.3.2. Functional disability
The Functional Disability Inventory6,37 is a 15-item self-report questionnaire that measures perceived difficulty in performing common activities in the domains of school, home, recreation, and social interactions. Participants rate the difficulty they had in performing each activity in the preceding 2 weeks (ranging from 0 [no trouble] to 5 [impossible]). The Functional Disability Inventory consists of 15 items and yields a total score that can range from 0 to 60, with higher scores indicating greater disability.18
2.3.3. General anxiety
The Revised Children's Manifest Anxiety Scale—Second Edition (RCMAS-2)29 is a 49-item self-report questionnaire comprising 40 dichotomous items assessing general anxiety and 9 dichotomous items assessing defensiveness. We used the general anxiety scale for this study; higher scores indicate greater anxiety symptom severity. Items are scored either 0 (No) or 1 (Yes), yielding a total anxiety score ranging from 0 to 40. Raw scores were converted into T scores, accounting for age.
2.3.4. Depressive symptoms
The Children's Depression Inventory (CDI)20 is a 27-item self-report questionnaire that assesses depressive symptoms in children and adolescents. Each item consists of 3 self-report statements increasing in severity. Items are scored from 0 to 2, yielding a total score ranging from 0 to 54, with greater scores indicating a greater level of depressive symptoms. During data collection, the clinic replaced the CDI with the CDI-2,21 a similarly scored measure to the CDI but with 28 items and a maximum total score of 56. To correct for the disparity in total score, raw scores for both the CDI and the CDI-2 were converted into T scores, accounting for age and sex (see Ref. 28 for similar approach).
2.3.5. Children's Somatization Inventory
The Child Somatization Inventory36 is a 24-item self-report questionnaire assessing the severity of nonspecific somatic symptoms (eg, weakness and dizziness). Respondents rate the extent to which they have experienced each of 35 symptoms during the past 2 weeks using a 5-point Likert-type scale (ranging from 0 [not at all] to 4 [a whole lot]). Total scores are computed by summing the items, with a possible range of 0 to 140. Higher scores indicate higher levels of somatic symptoms.
2.3.6. Fear of pain
The Fear of Pain Questionnaire for Children31 is a 24-item self-report questionnaire that assesses young people's pain-related fears and avoidance. There are 2 subscales within the measure: fear of pain (13 items), which is a measure of distress caused by pain, and avoidance of activities (11 items), which evaluates avoidance behavior towards activities as a result of fear of pain. Items are rated on a 5-point scale from 0 to 4 and are summed to obtain a total score; thus, the total score range is 0 to 96. Higher scores indicate greater fear and avoidance of pain.
2.3.7. School functioning
The Pediatric Quality of Life Inventory33,34 is a 23-item questionnaire that assesses young people's physical, emotional, social, and school functioning. The School Functioning subscale (5 items) was used for this study. Items are rated on a 5-point scale from 0 to 4, and raw scores are then transformed into standard scores on a scale of 0 to 100, with higher scores indicating better functioning (less impairment). Child self-reports and parent proxy reports are available for this measure, but the parent report has shown better reliability and validity than the child version. Thus, we used the parent version32 in this study.
2.4. Statistical analyses
First, we examined frequencies of the presence and type of precipitating event across the whole sample. Next, to compare demographic and clinical characteristics across patients with and without a precipitating event, we performed χ2 and t test analyses including the presence of a precipitating event (yes/no) and clinical and demographic factors (the χ2 test: pain diagnosis and sex; the t test: pain duration and age). To compare demographic and clinical characteristics across patients with different types of precipitating events, we performed similar χ2 and 1-way ANOVA analyses but included event type (surgery, injury, infection/illness, and chronic disease) instead of the presence of an event.
Next, to examine psychofunctional correlates of the presence/type of precipitating event, we conducted a series of 1-way ANOVAs. First, we included the presence of a precipitating event (yes/no) as the independent variable, and psychofunctional factors as dependent variables (typical pain intensity, functional disability, school functioning, depression, anxiety, somatization, and fear of pain). Next, we included event type (surgery, injury, infection/illness, and chronic disease) as the independent variable and psychofunctional factors as dependent variables.
An alpha of 0.05 was considered significant. We applied Bonferroni correction for multiple comparisons where applicable. We required each participant to have completed at least 75% of items on each questionnaire to compute total/mean/T scores for those measures (missing data: range = 2%–7%; M = 4% for each measure, no imputation was used).
3. Results
3.1. Incidence of precipitating events
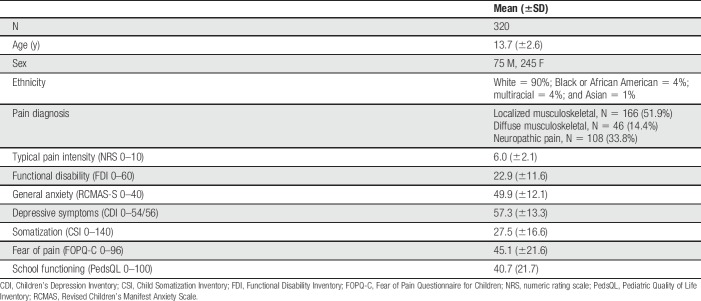
As can be seen in Figure 1, roughly two-thirds of patients (212 patients, 66.3%) reported a precipitating event before their pain onset. Injury was the most commonly reported event (41.9%), followed by chronic disease (14.1%), infection/illness (5.6%), and surgery (4.7%). Roughly one-third of patients (108 patients, 33.8%) did not report any precipitating event for their pain.
Figure 1.
Incidence of precipitating events.
3.2. Demographic/clinical factors: the presence of precipitating event
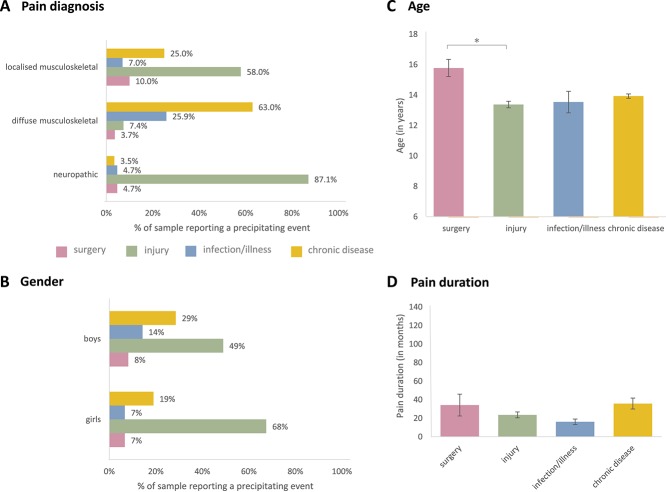
For all 3 pain diagnosis groups, most patients reported a precipitating event (Fig. 2A). There was a significant association between the presence of a precipitating event and diagnosis (χ2(2) = 11.35, P = 0.003). Patients with neuropathic pain were more likely to report a precipitating event compared to patients with localized or diffuse musculoskeletal pain (P < 0.05). The presence of a precipitating event did not differ according to patients' sex (χ2(1) = 0.04, P = 0.85), age (t(318) = −0.27, P = 0.79), or pain duration (t(313) = −0.86, P = 0.39) (Fig. 2B–D).
Figure 2.
Presence of precipitating events across demographic (B and C) and clinical (A and D) groups.
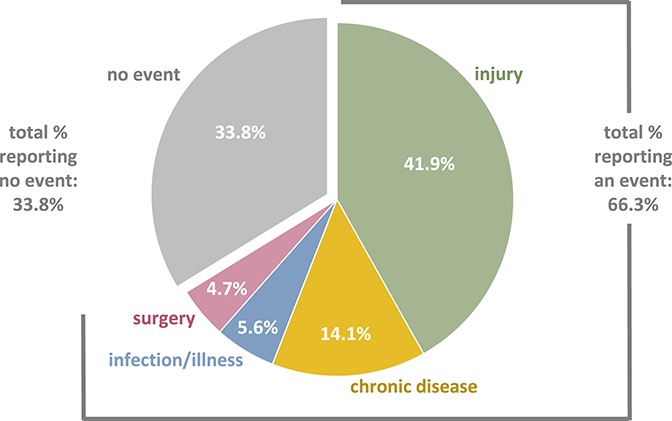
3.3. Demographic/clinical factors: the type of precipitating event
There was a significant association between the type of precipitating event and diagnosis (χ2(6) = 70.43, P < 0.001). Patients with localized musculoskeletal pain and neuropathic pain were most likely to report an injury, whereas patients with diffuse musculoskeletal pain were most likely to report a chronic disease (Fig. 3A). The type of precipitating event was also associated with patients' sex (χ2(3) = 6.29, P = 0.01). Specifically, girls were more likely than boys to report an injury, whereas there was no significant sex difference for infection/illness, surgery, or chronic disease (Fig. 3B). There was also a significant difference in precipitating event type across age (F(3,208) = 4.06, P = 0.008). Specifically, patients who reported surgery as the precipitating event were significantly older (M = 15.78 years, SD = 2.19) than those patients who reported an injury (M = 13.38 years, SD = 2.49; P = 0.005) (Fig. 3C). There was no significant difference in precipitating event type across pain duration (F(3,203) = 1.91, P = 0.13) (Fig. 3D).
Figure 3.
Type of precipitating events across demographic (B and C) and clinical (A and D) groups. *p<.05.
3.4. Psychofunctional factors: the presence of precipitating event
There were no significant effects of the presence of a precipitating event on patients' typical pain intensity (F(1,289) = 0.12, P = 0.73), functional disability (F(1,310) = 3.64, P = 0.06), somatization (F(1,305) = 0.10, P = 0.75), fear of pain (F(1,299) = 0.67, P = 0.41), school functioning (F(1,293) = 0.05, P = 0.82), depressive symptoms (F(1,309) = 0.03, P = 0.86), or anxiety symptoms (F(1,302) = 0.90, P = 0.34).
3.5. Psychofunctional factors: the type of precipitating event
There was a significant effect of the type of precipitating event on patients' typical pain intensity (F(3,188) = 4.89, P = 0.003). Specifically, patients who reported an injury (M = 6.29, SD = 2.09) reported more pain than those patients who reported an infection/illness (M = 4.41, SD = 1.84; P = 0.004). There were no significant effects of the type of precipitating event on patients' functional disability (F(3,202) = 1.48, P = 0.22), somatization (F(3,195) = 1.01, P = 0.39), fear of pain (F(3,192) = 0.51, P = 0.68), school functioning (F(3,192) = 1.27, P = 0.29), depressive symptoms (F(3,202) = 0.47, P = 0.71), or anxiety symptoms (F(3,197) = 0.33, P = 0.81).
4. Discussion
A common question when describing the prevalence of chronic pain in childhood is: “but what happened before the pain?” Anecdotally, this question is more frequently asked about young people than older people, perhaps in part because the pain cannot be attributed to the wear and tear associated with aging. In this study, we aimed to add to the epidemiological evidence base for pediatric chronic pain disorders by providing information regarding the events that precipitate the onset of chronic musculoskeletal pain in childhood and adolescence. We conducted a retrospective chart review of 320 young people attending a tertiary care chronic pain clinic with a primary musculoskeletal (local, diffuse, and neuropathic) pain complaint. We examined both the prevalence and type of various precipitating events that patients reported as causing their pain (injury, infection/illness, surgery, and chronic disease), as well as the absence of a precipitating event. We considered whether the presence or type of precipitating event differed across demographic or clinical characteristics of the patients, and we considered whether the presence or type of precipitating event was associated with certain psychofunctioning profiles.
Approximately two-thirds of patients reported a precipitating event for their pain. Injury was the most commonly reported event, by over 40% of the sample. The next most commonly reported event was a chronic disease, followed by an infection or illness. Surgery was the least commonly reported event (only 4.7% of the sample). About one-third of patients did not report any precipitating event for their pain. Overall, we found some evidence that the presence and/or type of precipitating event varied according to patients' demographic or clinical characteristics. Across all 3 diagnostic categories (diffuse, localized, and neuropathic), patients were more likely to report a precipitating event than not; however, patients with neuropathic pain were even more likely to report a precipitating event compared to those with localized and diffuse musculoskeletal pain. We did not find that patients' age, sex, or diagnosis was associated with whether or not they reported a precipitating event for their pain. With respect to the type of precipitating event, however, a number of differences emerged. First, we found that girls were more likely than boys to report an injury, whereas there was no significant sex difference for infection/illness, surgery, or chronic disease. We also found that patients who reported surgery as the precipitating event were significantly older (∼2.5 years) than those patients who reported an injury. Interestingly, when considering event type, patients with localized musculoskeletal pain and neuropathic pain were most likely to report an injury, whereas patients with diffuse musculoskeletal pain were most likely to report a chronic disease. This is likely due to the fact that certain chronic diseases in young people (eg, Ehlers–Danlos syndromes, juvenile arthritis, and scoliosis) are typically associated with widespread pain, whereas more localized pain is more likely to stem from an initial injury to one body part (eg, a sports-related fracture or sprain). We found little to no evidence that the presence or type of precipitating event was associated with psychological or physical functioning. The only significant finding was that patients who reported an injury reported more pain than those patients who reported an infection/illness (around 6 of 10 compared with 4 of 10).
To the best of our knowledge, this study is one of the first to systematically consider the precipitating events associated with chronic pain in youth, thus providing important epidemiological data for this population. Chronic musculoskeletal pain in childhood and adolescence is a common and disabling problem.7,19,27 For most young people presenting to a tertiary care pain clinic, the experience of chronic pain has often had a large and negative impact on their physical and psychological well-being as well as that of their family.7 Chronic pain in youth is associated with substantial interference in daily life, including interruption in school activities and impairment in physical, social, and emotional functioning.16 It is also associated with substantial financial costs to individual families and to society, resulting in estimated costs of $11,787 per family per year, equating to an annual societal cost of $19.5 billion.12 Thus, understanding the epidemiology of chronic pain in childhood and adolescence, including the events that may have a primary causal role in the onset of the pain, is of great clinical and societal importance.
Our findings provide important information indicating the prevalence of precipitating events in children and adolescents at tertiary care chronic pain clinics. We focused here on musculoskeletal pain disorders as population-based epidemiological studies indicate that although headaches and abdominal pains are most commonly reported in young children, middle childhood and adolescence are most commonly characterized by musculoskeletal (especially back and neck) pain.7,19,27 An outstanding question is whether or not the prevalence and type of precipitating events reported here are similar in samples with nonmusculoskeletal pains and in samples presenting to other (types of) clinics. Indeed, the composition of patients in pediatric chronic pain clinics across the United States and in different countries will depend, in part, on the referral system for these clinics, as well as the availability of other pain- and disease-specific clinics at the hospital and in the geographic area (eg, a headache clinic, or a gastroenterology clinic). Further studies are needed to confirm our findings and to characterize the prevalence of precipitating events in nonmusculoskeletal samples.
The current findings provide preliminary evidence that, for children and adolescents with chronic musculoskeletal pain, reporting a precipitating event for their pain, or reporting a certain type of precipitating event, may not play a large role in subsequent physical or psychological functioning. These findings are especially interesting given that there is some evidence in adult samples that the absence of a precipitating event, that is having no identified cause for the pain, is associated with worse functioning.11 The current findings are thus relevant for a consideration of a precision-medicine approach to pediatric pain. That is, identifying risk factors that predict poor physical or psychological functioning may be useful for screening risk during initial clinical evaluations and subsequently for stratifying care according to risk level. However, a number of future studies are required before determining whether or not precipitating events are important to include in screening practices. For example, we do not know whether the presence or type of precipitating event is associated with health care–seeking behaviors. Our data are from a health care–seeking sample, and thus, we do not know whether or not there would be differences in a non–health care–seeking sample. In adults, there is evidence that attributing physical symptoms such as pain to external and nonbiological factors is associated with not seeking health care.13 Also, relevant is to what extent our findings would apply to patients who would seek but do not have access to tertiary health care services. Future studies could consider how socioeconomic factors impact the reporting and impact of precipitating events in this population. We also do not know whether the presence or type of precipitating event is associated with longer-term functioning over time, or with response to treatment. Longitudinal studies considering the role of precipitating events in patients' psychofunctional trajectories over time, as well as their recovery both within and outside the context of treatment, will be important. It is also important to note that identifying precipitating events that are commonly associated with chronic pain in childhood, even if not associated specifically with the child's functioning when their pain is already chronic, will be important for potentially identifying who may later develop chronic pain, and thus for prevention efforts. Our findings do not contradict the increased understanding that pain in children is multifactorial and that even when there are clear “biological” contributors to the pain (eg, a chronic disease such as arthritis), psychosocial factors are, perhaps separately, important in the child's chronic pain experience.24
Our findings add to the literature on risk factors for pediatric chronic pain. Although few studies have considered specific precipitating events, studies to date have identified a variety of risk factors including demographic factors, psychosocial factors, and previous pain experiences. For example, Coenders et al.8 found that youth with chronic pain was more likely to have individual and parent history of functional pain syndromes (eg, migraine, nonmigraine headaches, functional abdominal pain, and restless leg syndrome) than youth without chronic pain. In a longitudinal study, Kroner-Herwig et al.22 found that previous multiple pain sites, age, sex, internalizing/externalizing symptoms, and time spent with visual media were significant risk factors for the development of multiple pains in childhood and adolescence. A recent review by McKillop and Banez25 also identified a variety of factors that increase the likelihood of transitioning from acute to chronic pain in youth. These include temperament, anxiety, depression, subjective experience of stress, passive coping strategies, sleep problems, and other parent and/or family factors. We add to this literature a recognition of the potential role of specific medical events in contributing to risk of pediatric chronic pain.
Our findings can also be considered within existing theoretical frameworks of risk factors in pediatric chronic pain. One such framework was proposed by von Baeyer and Champion,35 including hypothesized antecedents and consequences of pain vulnerability in children and adolescents. Our findings provide support for antecedent factors such as injury and inflammation, which are included in von Baeyer and Champion's framework as “sensory inputs into the central nervous system.” Taking theoretical models and original studies together, it is clear that a number of intrapersonal and interpersonal biopsychosocial factors, and their complex interactions, likely play a role in increasing risk of pediatric chronic pain. As McKillop and Banez25 suggest, progress on understanding risk of pediatric chronic pain will likely lie in considering how multiple factors, including precipitating medical events, interact to increase relative risk.
This study has limitations, which can be addressed in future research. First, both patients and parents contributed to the initial evaluations, and we were unable to distinguish who reported each precipitating event. It will be interesting in future studies to consider whether the presence or type of precipitating event differs according to whether the patient or parent is the reporter. Second, although our sample was relatively large, some categorical analyses (eg, regarding precipitating event type and diagnosis type) resulted in a relatively small number of participants per cell, so these data should be interpreted with caution. Finally, discussion of precipitating events in patients' initial evaluation focused on physical events, and thus, psychological or emotional trauma could not be coded for in this data set. There is growing recognition that chronic pain can be precipitated by psychological and emotional trauma,38,39 including in childhood.10 Moreover, given preliminary evidence for the cooccurrence of pain and posttraumatic stress symptoms and disorders in youth,15 the prevalence of precipitating psychological and emotional trauma in pediatric chronic pain is an important next question.
In this retrospective chart review, approximately two-thirds of children and adolescents with chronic musculoskeletal pain reported a precipitating physical event for their pain, with injury as the most commonly reported event. One-third of young patients reported no precipitating event for their chronic pain. Although there were some differences in the types of precipitating events reported across different demographic groups and pain diagnoses, we found little to no evidence that the presence or type of precipitating event was associated with patients' psychological or physical functioning. Important next steps will be to better understand the physical events that precipitate nonmusculoskeletal pains such as headaches and abdominal pains in childhood, and to integrate data on physical and psychological traumatic events that precipitate the onset of pediatric chronic pain.
Disclosures
There are no conflicts of interest arising from this work.
Acknowledgments
The authors thank Maggie Ryan, Connie Hsu, Victoria Perron, and Hannah Robins for their assistance with coding precipitating events from medical records.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
A.J. Becker and L.C. Heathcote contributed equally to this article.
References
- [1].Al-Allaf AW, Dunbar KL, Hallum NS, Nosratzadeh B, Templeton KD, Pullar T. A case-control study examining the role of physical trauma in the onset of fibromyalgia syndrome. Rheumatology (Oxford) 2002;41:450–3. [DOI] [PubMed] [Google Scholar]
- [2].Almeida EC, Nogueira AA, Candido dos Reis FJ, Rosa e Silva JC. Cesarean section as a cause of chronic pelvic pain. Int J Gynaecol Obstet 2002;79:101–4. [DOI] [PubMed] [Google Scholar]
- [3].Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006;10:287–333. [DOI] [PubMed] [Google Scholar]
- [4].Caraceni A, Portenoy RK. An international survey of cancer pain characteristics and syndromes. IASP Task Force on Cancer Pain. International Association for the Study of Pain. PAIN 1999;82:263–74. [DOI] [PubMed] [Google Scholar]
- [5].Castarlenas E, Jensen MP, von Baeyer CL, Miro J. Psychometric properties of the numerical rating scale to assess self-reported pain intensity in children and adolescents: a systematic review. Clin J Pain 2017;33:376–83. [DOI] [PubMed] [Google Scholar]
- [6].Claar RL, Walker LS. Functional assessment of pediatric pain patients: psychometric properties of the Functional Disability Inventory. PAIN 2006;121:77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Clinch J, Eccleston C. Chronic musculoskeletal pain in children: assessment and management. Rheumatology (Oxford) 2009;48:466–74. [DOI] [PubMed] [Google Scholar]
- [8].Coenders A, Chapman C, Hannaford P, Jaaniste T, Qiu W, Anderson D, Glogauer M, Goodison-Farnsworth E, McCormick M, Champion D. In search of risk factors for chronic pain in adolescents: a case–control study of childhood and parental associations. J Pain Res 2014;7:175–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Davies HTO, Crombie IK, Macrae WA, Rogers KM. Pain clinic patients in Northern Britain. Pain Clin 1992;5:129–35. [Google Scholar]
- [10].Davis DA, Luecken LJ, Zautra AJ. Are reports of childhood abuse related to the experience of chronic pain in adulthood? a meta-analytic review of the literature. Clin J Pain 2005;21:398–405. [DOI] [PubMed] [Google Scholar]
- [11].de Rooij AM, Perez RS, Huygen FJ, van Eijs F, van Kleef M, Bauer MC, van Hilten JJ, Marinus J. Spontaneous onset of complex regional pain syndrome. Eur J Pain 2010;14:510–13. [DOI] [PubMed] [Google Scholar]
- [12].Groenewald CB, Essner BS, Wright D, Fesinmeyer MD, Palermo TM. The economic costs of chronic pain among a cohort of treatment-seeking adolescents in the United States. J Pain 2014;15:925–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Gulec H. Normalizing attributions may contribute to non–help-seeking behavior in people with fibromyalgia syndrome. Psychosomatics 2008;49:212–17. [DOI] [PubMed] [Google Scholar]
- [14].Hewitt DJ, McDonald M, Portenoy RK, Rosenfeld B, Passik S, Breitbart W. Pain syndromes and etiologies in ambulatory AIDS patients. PAIN 1997;70:117–23. [DOI] [PubMed] [Google Scholar]
- [15].Holley AL, Wilson AC, Noel M, Palermo TM. Post-traumatic stress symptoms in children and adolescents with chronic pain: a topical review of the literature and a proposed framework for future research. Eur J Pain 2016;20:1371–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Huguet A, Miro J. The severity of chronic pediatric pain: an epidemiological study. J Pain 2008;9:226–36. [DOI] [PubMed] [Google Scholar]
- [17].Jung BF, Johnson RW, Griffin DR, Dworkin RH. Risk factors for postherpetic neuralgia in patients with herpes zoster. Neurology 2004;62:1545–51. [DOI] [PubMed] [Google Scholar]
- [18].Kashikar-Zuck S, Flowers SR, Claar RL, Guite JW, Logan DE, Lynch-Jordan AM, Palermo TM, Wilson AC. Clinical utility and validity of the Functional Disability Inventory among a multicenter sample of youth with chronic pain. PAIN 2011;152:1600–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, MacDonald AJ. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. PAIN 2011;152:2729–38. [DOI] [PubMed] [Google Scholar]
- [20].Kovacs M. The Children's Depression Inventory (CDI). Psychopharmacol Bull 1985;21:995–8. [PubMed] [Google Scholar]
- [21].Kovacs M. Children's Depression Inventory (CDI and CDI 2). The encyclopedia of clinical psychology. Hoboken, NJ: John Wiley & Sons, Inc, 2014. [Google Scholar]
- [22].Kroner-Herwig B, Gassmann J, van Gessel H, Vath N. Multiple pains in children and adolescents: a risk factor analysis in a longitudinal study. J Pediatr Psychol 2011;36:420–32. [DOI] [PubMed] [Google Scholar]
- [23].Logigian EL, Kaplan RF, Steere AC. Chronic neurologic manifestations of Lyme disease. N Engl J Med 1990;323:1438–44. [DOI] [PubMed] [Google Scholar]
- [24].Malleson P, Clinch J. Pain syndromes in children. Curr Opin Rheumatol 2003;15:572–580. [DOI] [PubMed] [Google Scholar]
- [25].McKillop HN, Banez GA. A broad consideration of risk factors in pediatric chronic pain: where to go from here? Children (Basel) 2016;3:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Osterberg A, Boivie J, Thuomas KA. Central pain in multiple sclerosis–prevalence and clinical characteristics. Eur J Pain 2005;9:531–42. [DOI] [PubMed] [Google Scholar]
- [27].Perquin CW, Hazebroek-Kampschreur AA, Hunfeld JA, Bohnen AM, van Suijlekom-Smit LW, Passchier J, van der Wouden JC. Pain in children and adolescents: a common experience. PAIN 2000;87:51–8. [DOI] [PubMed] [Google Scholar]
- [28].Rabner JA, Kaczynski KJ, Simons LE, LeBel A. Pediatric headache and sleep disturbance: a comparison of diagnostic groups. Headache 2018;58:217–228. [DOI] [PubMed] [Google Scholar]
- [29].Reynolds CR, Richmond BO. Revised Children's Manifest Anxiety Scale, second edition (RCMAS-2), manual. Los Angeles, CA: Western Psychological Services, 2008. [Google Scholar]
- [30].Roth-Isigkeit A, Thyen U, Stöven H, Schwarzenberger J, Schmucker P. Pain among children and adolescents: restrictions in daily living and triggering factors. Pediatrics 2005;115:e152–e162. [DOI] [PubMed] [Google Scholar]
- [31].Simons LE, Sieberg CB, Carpino E, Logan D, Berde C. The Fear of Pain Questionnaire (FOPQ): assessment of pain-related fear among children and adolescents with chronic pain. J Pain 2011;12:677–86. [DOI] [PubMed] [Google Scholar]
- [32].Varni JW, Limbers CA, Burwinkle TM. Parent proxy-report of their children's health-related quality of life: an analysis of 13,878 parents' reliability and validity across age subgroups using the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes 2007;5:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 2001;39:800–12. [DOI] [PubMed] [Google Scholar]
- [34].Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the Pediatric Quality of Life Inventory. Med Care 1999;37:126–39. [DOI] [PubMed] [Google Scholar]
- [35].von Baeyer CL, Champion GD. Commentary: multiple pains as functional pain syndromes. J Pediatr Psychol 2011;36:433–7. [DOI] [PubMed] [Google Scholar]
- [36].Walker LS, Garber J, Greene JW. Somatization symptoms in pediatric abdominal pain patients: relation to chronicity of abdominal pain and parent somatization. J Abnorm Child Psychol 1991;19:379–94. [DOI] [PubMed] [Google Scholar]
- [37].Walker LS, Greene JW. The Functional Disability Inventory: measuring a neglected dimension of child health status. J Pediatr Psychol 1991;16:39–58. [DOI] [PubMed] [Google Scholar]
- [38].Yavne Y, Amital D, Watad A, Tiosano S, Amital H. A systematic review of precipitating physical and psychological traumatic events in the development of fibromyalgia. Semin Arthritis Rheum 2018. 10.1016/j.semarthrit.2017.12.011. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- [39].Young Casey C, Greenberg MA, Nicassio PM, Harpin RE, Hubbard D. Transition from acute to chronic pain and disability: a model including cognitive, affective, and trauma factors. PAIN 2008;134:69–79. [DOI] [PubMed] [Google Scholar]