Abstract
Thermosensitive polymeric delivery system (PLA-PEG-PLA) loaded with chitosan-zinc-insulin complex was designed for continuous in vivo insulin delivery at basal level for prolonged period after a single subcutaneous injection. Chitosan-zinc-insulin complex was optimized to restrict the diffusion of insulin from the delivery system by forming large complexes and thereby reducing the initial burst release. The in vivo absorption and bioactivity of insulin released from the delivery systems were studied in streptozotocin-induced diabetic rat model. The amount of insulin released in vivo was quantified using Enzyme Linked Immunosorbent Assay (ELISA), and its bioactivity was determined by its ability to reduce the blood glucose levels in diabetic rats. An indirect ELISA was performed to determine the immunogenic potential of insulin released from the formulations. Furthermore, the in vitro and in vivo biocompatibility of the delivery system was studied using an MTT assay, and by studying the histology of skin samples, respectively. Chitosan-zinc-insulin complex significantly (P<0.05) reduced the initial burst release of insulin from the polymeric delivery system in comparison to zinc-insulin or insulin alone. The delivery system released insulin for ~3 months in biologically active form with corresponding reduction in blood glucose levels in diabetic rats. The insulin released from the delivery systems did not provoke any immune response. The delivery systems demonstrated excellent biocompatibility both in vitro and in vivo and were non-toxic. The results indicate that the chitosan-zinc-insulin complex incorporated in the thermosensitive polymeric delivery system can be used as an alternative to the conventional daily basal insulin therapy.
Keywords: Protein delivery, insulin, chitosan-zinc-insulin complex, controlled release, biocompatibility, in vivo release and bioactivity
GRAPHICAL ABSTRACT
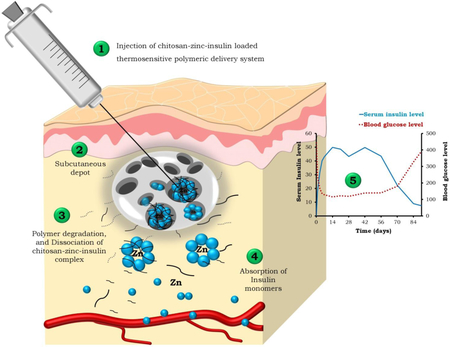
Events following subcutaneous administration of chitosan-zinc-insulin complex loaded thermosensitive delivery system in vivo
INTRODUCTION
Diabetes mellitus is cited as one of the most challenging health problems in the 21st century. It is characterized by absolute or relative (type 1 or 2) deficiency in insulin secretion/response resulting in hyperglycemia. In healthy individuals, physiological insulin secretion has two phases; basal secretion, wherein the pancreas secrete a constant low level of insulin into the circulation throughout the day, and stimulated secretion, where the pancreas respond to food intake by secreting large bolus of insulin to maintain normoglycemia [1]. The basal insulin which is secreted at a rate of 0.5-1U/h throughout the day and between meals, accounts for ~50% of the total daily insulin output, and plays a major role in preventing long-term diabetic complications [2,3]. Therefore, type 1 diabetic patients with absolute deficiency of insulin completely rely on basal-bolus insulin regimen for maintaining their blood glucose levels. This regimen attempts to replicate the normal insulin secretion profile and comprises of multiple injections of rapid acting insulin before each meal to mimic prandial insulin secretion, and an additional injection of intermediate/long acting insulin before bedtime to mimic basal insulin secretion. This repeated insulin administration gives rise to numerous complications and the pain from multiple daily injections adversely affects the quality of life of patients. Therefore, from a patient compliance perspective, to avoid the discomfort and inconvenience associated with multiple daily injections, alternate administration routes have been explored.
Various inhalation insulin preparations (Exubera®, AERx® insulin) [4,5], nasal sprays (Nasulin™) [6], and oral insulin spray (Oralin™) [7] have been used to relieve pain and discomfort experienced by patients due to repeated injections. However, due to the absence of the controlled delivery feature, these systems do not offer a prolonged insulin release. Insulin pumps are extensively tried due to their ability to offer improved glycemic control as compared to daily injections [8]. Almost every feasible route for insulin administration has been tested with limited success and the subcutaneous route still remains the principal route of administration. The two long acting basal insulin analogues, Lantus® (Insulin Glargine), and Levemir® (Insulin detemir) have become available in recent years to achieve adequate glycemic control [9-11]. Though these analogues are known to achieve good glycemic control, and lower the incidence of fasting hypoglycemia efficiently [12]; they do not completely eliminate the risk of nocturnal/fasting hypoglycemia [13]. In view of these shortcomings, attempt have been made to fabricate an ideal basal insulin therapy, which will essentially provide a constant, peak-free, prolonged and continuous insulin supply after subcutaneous administration, eliminating the risk of fasting hypoglycemia.
Controlled delivery of insulin using in situ gel forming delivery systems can be an effective strategy which could provide continuous low basal insulin level, and partly alleviate the pain felt by multiple injections [14]. Such insulin delivery is also critical in reducing the long-term micro and macro vascular complications of diabetes [15].
Several researchers have focused on the development of injectable thermosensitive polymeric delivery systems for the delivery of insulin at a controlled rate and in response to the physiological need [14,16,17]. These delivery systems with varying hydrophilic/hydrophobic content can alter the rate of insulin release. The major advantage of these delivery systems is absence of organic phase which hampers the delicate protein structure [18]. Additionally, the biodegradable and biocompatible nature of the copolymers, as well as simplicity of administration of the delivery system makes them attractive for sustained drug delivery. Zinc has been employed in number of pharmaceutical preparations of insulin for prolonging the release period, and enhancing its stability by protecting from unfolding/misfolding [19]. Literature also indicates that human body stores insulin in its zinc-based hexameric form [20]. Upon secretion into bloodstream, hexamers dissociate into dimers and finally to monomers which is the active form of insulin. Increasing evidence suggests that insulin/chitosan polyelectrolyte complexes can be efficiently used for insulin delivery [21-26]. Though chitosan, zinc, and thermosensitive polymeric delivery systems have been individually used for controlling insulin delivery, a combination approach is not yet fully explored.
In our previous work, we have demonstrated the ability of chitosan-zinc-insulin complex incorporated in thermosensitive copolymer poly(D,L-lactide)-poly(ethylene glycol)-poly(D,L-lactide) (PLA-PEG-PLA, 4500 Da) based delivery system to control the release of insulin for prolonged period while maintaining its structural integrity in vitro [27]. It was observed that the complex formation played an important role in reducing the initial burst release of insulin from the polymer gel matrix, due to increased size and slow dissociation from chitosan-zinc-insulin complex, and also helped to stabilize insulin during release and storage. The complex formation between chitosan and zinc-insulin also protected insulin from the acidic degradation products formed during copolymer degradation and stabilized insulin inside the delivery system without aggregation or degradation during entire release period.
In present study, the ability of the delivery system to provide basal level of insulin for three months after a single subcutaneous injection was investigated in vivo using streptozotocin-induced diabetic rat model. The biocompatibility of the delivery system containing thermosensitive polymer incorporated chitosan was tested in vitro and in vivo. Furthermore, the immunogenic potential of released insulin was also investigated.
MATERIALS
Human recombinant insulin (Incelligent® SG) was obtained from Millipore Corporation (Norcross, GA). Chitosan (50 kDa) was procured from Sigma Aldrich Co. (St. Louis, MO). Human Embryonic Kidney (HEK293) cells were obtained from American Type Culture Collection (ATCC, VA). Sprague Dawley rats were purchased from Harlan Laboratories Inc. (IN, USA). Streptozotocin was procured from Enzo Life Sciences (NY, USA). Human insulin ELISA Kit was obtained from Mercodia, Uppsala, Sweden. Nembutal (Pentobarbital sodium) and Ketoprofen were procured from Lundbeck Inc. (IL, USA), and Medisca Inc. (NY, USA), respectively. Rat Immunoglobulin G (IgG) were purchased from Santa Cruz Biotechnology (CA, USA).
METHODS
Preparation of the delivery systems:
The thermosensitive triblock copolymer PLA-PEG-PLA (molecular weight 4500 Da) was synthesized by ring-opening polymerization and characterized by 1H and 13C-NMR for structural composition, and gel permeation chromatography (GPC) for molecular weight distribution. The details about the synthesis and characterization procedures are discussed earlier [14]. Chitosan-zinc-insulin complexes were designed, characterized, optimized, and incorporated into the triblock copolymer based delivery systems as described in our earlier publication [27]. Briefly, the delivery system was prepared by dissolving the triblock copolymer (30% w/w) in water at 4°C under continuous stirring. Insulin alone, zinc-insulin or chitosan-zinc-insulin complexes were mixed with the aqueous copolymer solutions at room temperature to get the final formulations. All formulations were tested for their injectability by passing through a 25 G needle.
In vivo insulin release and bioactivity:
The North Dakota State University Institutional Animal Care and Use Committee (IACUC) approved the animal study protocol and experiments. Eight weeks old male Sprague-Dawley rats weighing 180-200 g were used to study the in vivo absorption and bioactivity of the recombinant human insulin (rH) released from the delivery systems. Rats were housed in a temperature controlled facility maintained at 12 h light-dark cycle, and allowed free access to food and water. The rats were acclimatized to the housing conditions one week before the study initiation. A single dose of freshly prepared streptozotocin (STZ, 55 mg/kg body weight) dissolved in ice cold citrate buffer (pH 4.5) was injected intraperitoneally to the rats to induce diabetes. Post-injection, rats were provided with 5% sucrose solution to counteract the potential risk of hypoglycemia caused by massive insulin release under the influence of STZ. Rats were monitored daily, and one week after STZ injection, blood glucose levels were measured. The rats with fasting blood glucose levels >200 mg/dl were considered diabetic and retained in the study. The diabetic rats were divided into 8 different groups (6 animals/group), and assigned to the treatments randomly. An additional group of non-diabetic rats was used as control. The formulations were injected as a single subcutaneous dose at the back neck region of rats using 25 G needle. The treatment groups were injected with the polymeric delivery systems containing either insulin alone, zinc-insulin or and chitosan-zinc-insulin complexes at two different doses. Assuming the daily basal insulin requirement of ~18-24 IU (~0.4-0.5 IU/kg/day; total dose: ~30 and 45 IU/kg for 90 days), two doses were selected to provide a continuous basal level of insulin. Groups I and II were injected with the thermosensitive delivery system containing insulin alone at a dose of 30 and 45 IU/kg, groups III and IV with zinc-insulin (30 and 45 IU/kg), and group V and VI with chitosan-zinc-insulin complex at a dose of 30 and 45 IU/kg. Group VII was treated with single dose of insulin (2 IU/kg) dissolved in PBS (pH 7.4) subcutaneously; while STZ treated animals without treatment (group VIII) were used as a negative control. After the initial week, blood sampling was performed on a weekly basis until three months using tail vein puncture. At the end of the study period, an intravenous injection of pentobarbital (150 mg/kg) was used to euthanize the rats.
Quantification of serum insulin levels using Enzyme Linked Immunosorbent Assay (ELISA): Insulin levels were measured by sampling blood from the tail vein of rats at pre-determined time points after overnight fasting. Serum was collected after centrifuging the blood samples at 4°C at 3000 rpm for 15 min, and stored at −20°C. Mercodia Human Insulin ELISA kit was utilized to determine the of serum insulin (rH) levels [28].
Determination of blood glucose levels: The pharmacodynamic activity of insulin released from the delivery systems was estimated from blood glucose levels. After overnight fasting, blood was withdrawn from tail vein of rats, and the fasting blood glucose levels were measured by the glucose oxidase method using a glucometer (Bayer CONTOUR® blood glucose monitoring system, IN), and expressed in milligrams per deciliter (mg/dl).
Body weight determination: The change in the body weight of rats before and after induction of diabetes, as well as after insulin treatment was noted daily for the first week, and further monitored on weekly basis during entire study duration.
Detection of anti-insulin antibodies: The rat serum samples were collected after 1, 2 and 3 months of treatment and were subjected to ELISA. For detection of anti-human insulin antibodies in rat serum an indirect ELISA was performed [29]. Briefly, ELISA plate was coated with 800 ng/ml insulin in coating buffer (carbonate buffer, 50 mM, pH 9.6, 100 μl/well), and kept overnight at 4°C. Plates were incubated with a blocking agent [3% bovine serum albumin (BSA)], at 37°C for 1 h. The plates were washed with PBS containing 0.02% tween 20 (PBST) followed by addition of diluted rat serum and again incubated at 37°C for 1 h. The plates were washed again with PBST, and 1:5000 diluted goat anti-rat-IgG-Horseradish Peroxidase conjugated secondary antibody was added, followed by incubation at 37°C for 2 h. Substrate solution (tetramethylbenzidine, TMB) was added at the end of incubation, and the plates were further incubated for 20 min at 37°C. Sulfuric acid (0.5 M) was used to stop the reaction, and the optical density was recorded at 450 nm using a microplate reader. Rat IgG were used as a control.
In vitro biocompatibility of the delivery system:
In vitro biocompatibility of the thermosensitive polymeric delivery system with and without chitosan was quantitatively assessed using a standard MTT cell viability assay. This assay was aimed to evaluate the effect of polymer extracts, and their degradation products on the cell viability in vitro. The detailed procedure is described previously [30]. Briefly, the aqueous solutions of thermosensitive polymer (30% w/w, 500μl) with/without chitosan were prepared, injected in a tube, and allowed to form gels by incubating at 37°C in water bath. The polymeric hydrogels were extracted into PBS (10 ml, pH 7.4) at 37 and 70°C by incubating for 10 days. The extracts were diluted with growth medium, added to the Human Embryonic Kidney (HEK293) cells and incubated for 24, 48 and 72 hours. Percent cell viability was calculated considering the cell viability of untreated cells (growth medium only) as 100%. For comparison purposes cells treated with PBS (without polymer), DMSO, and chitosan were used as controls.
In vivo biocompatibility of the delivery system:
The in vivo biodegradability and biocompatibility of the delivery system with and without chitosan was evaluated after injecting 500 μl of the delivery system subcutaneously into the upper neck area of rats. The appearance of gel lump was monitored regularly by visual examination. At 1, 7, 30 and 90 days post-injection, rats were euthanized, and the subcutaneous tissue surrounding the injection site was excised and examined visually for the presence of any delivery system residue. For assessing the biocompatibility of the delivery system, the excised hydrogel-contacting subcutaneous tissue was fixed in 10% neutrally buffered formalin at room temperature, sectioned (5 μm thickness), and processed for histological analysis. The skin sections were stained with hematoxylin eosin (H&E) and examined under the light microscope for any inflammatory reactions. The collagen deposition near the injection site was visualized by staining the skin sections with Gomori’s trichrome stain, and the collagen density and its appearance at the injection site were compared to that of normal skin tissue using ImageJ 1.45 software (NIH, MD).
Statistical analysis:
For statistical analysis, a single factor ANOVA was performed using Minitab 16 statistical software (Minitab Inc., PA). A p-value of less than 0.05 was considered to be significant. Serum insulin levels were plotted against time and the bioavaialability of insulin was determined based on the area under the curve (AUC) data calculated by linear trapezoidal rule [31]. The concentration versus time profile was used to determine maximum serum concentration (Cmax) and corresponding time at which maximum concentration is reached (Tmax) for the solution group (Insulin in PBS: 2 IU/kg SC).
RESULTS
Preparation of the delivery systems:
The optimized chitosan-zinc-insulin complex loaded thermosensitive polymeric delivery systems (PLA-PEG-PLA chain length: 1500-1500-1500, molecular weight 4500 Da) were formulated as described previously [27]. The formulations were injectable through 25 G needle, and formed gel depot quickly after incubation at body temperature.
In vivo absorption and bioactivity of insulin:
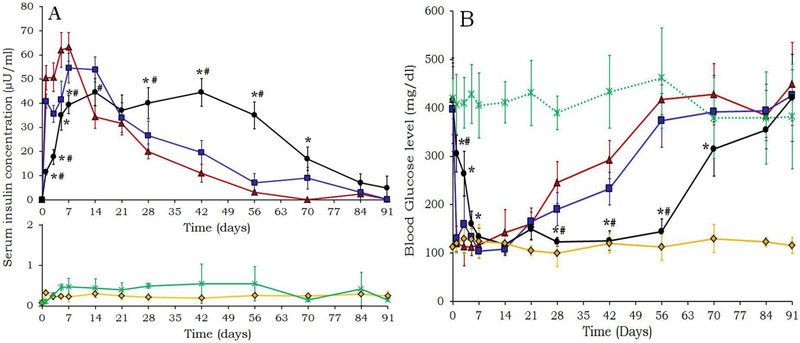
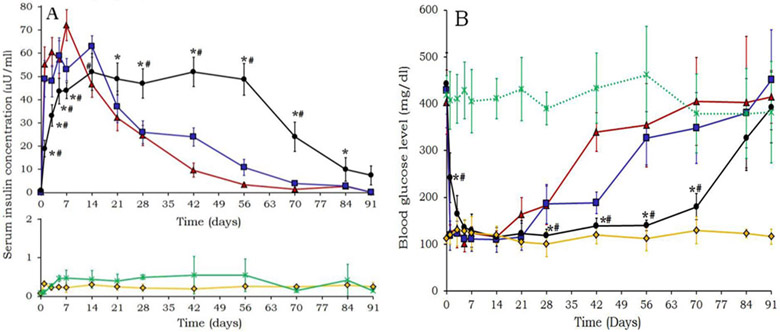
The pharmacokinetic profile of insulin released from the delivery systems and associated pharmacodynamic effects are presented in figures 1 and 2. Additionally, the serum insulin concentration and blood glucose levels of untreated (control), and STZ treated animals are also presented. The fasting blood glucose level of untreated animals remained in between 90-125 mg/dl throughout the study duration; while STZ treated rats showed fluctuating blood glucose levels between 300-550 mg/dl
Figure 1:
A) Serum human insulin and B) Blood glucose levels of rats in treated with (▴) Insulin alone, (■) Zinc-insulin, (●) Chitosan-zinc-insulin complex loaded thermosensitive polymeric delivery systems, (×) Streptozotocin control, and (♦) Untreated control; (insulin loading; 30 IU/kg) [n=6, mean ± SD, *: significantly different than insulin alone, and #: significantly different than zinc-insulin at P<0.05]
Figure 2:
A) Serum human insulin and B) Blood glucose levels of rats in treated with (▴) Insulin alone, (■) Zinc-insulin, (●) Chitosan-zinc-insulin complex loaded thermosensitive polymeric delivery systems, (×) Streptozotocin control, and (♦) Untreated control; (insulin loading; 45 IU/kg) [n=6, mean ± SD, *: significantly different than insulin alone, and #: significantly different than zinc-insulin at P<0.05]
Comparison among the delivery systems at 30 IU/kg insulin dosing:
The release profile of insulin and blood glucose levels of the rats treated with different formulations at 30 IU/kg insulin loading is presented in figure 1A and B, respectively. The animals treated with the delivery system containing insulin alone showed highest initial burst release (52.1±7.6 μU/ml) followed by a continuous release over the period of 42 days, and subsequent rapid reduction in insulin levels. In case of formulation containing zinc-insulin, though the initial burst release was reduced significantly (p<0.05) as compared to the formulation containing insulin alone, after ~14 days, an appreciable decline in the insulin level was observed, and the levels dropped continuously in 21-42 days. The delivery system containing chitosan-zinc-insulin complex showed significantly lower (P<0.05) initial burst release of insulin (11.4±2.1 μU/ml) as compared to the formulations containing insulin alone and zinc-insulin loaded delivery systems. Also, significantly higher (P<0.05) serum insulin levels were maintained for ~63 days, and then declined gradually over the period of 91 days. AUC was used to determine the bioavailability of insulin released, and is presented in table 1. Insulin bioavailability was enhanced in case of chitosan-zinc-insulin complex loaded delivery system, indicated by increase in AUC by 1.5 and 1.85 fold as compared to the formulations containing zinc-insulin and insulin alone, respectively (table 1).
Table 1:
In vivo pharmacokinetic parameters of insulin in rats
| Treatment Groups | Insulin dose (IU/kg) |
AUC(0-t) (μU.day/ml) |
Fold increase in AUC compared to insulin alone |
Fold increase in AUC compared to zinc- insulin |
|---|---|---|---|---|
| Insulin alone | 30 | 1481.36±105.6 | --- | --- |
| Zinc-insulin | 30 | 1886.68±92.2 | 1.27 | --- |
| Chitosan-zinc-insulin | 30 | 2733.08±103.8 | 1.85 | 1.5 |
| Insulin alone | 45 | 1686.79±93.8 | --- | --- |
| Zinc-insulin | 45 | 2073.58±110.1 | 1.23 | --- |
| Chitosan-zinc-insulin | 45 | 3458.79±153.3 | 2.1 | 1.3 |
[Mean ± SD, n=6, t: 90 days for polymeric delivery systems; Solution group (Insulin dispersed in PBS, injected via SC route), Cmax, Tmax, and AUC0-t for solution group: 55.75±6.4 μU/ml, 1 h, and 6.18±0.35 μU.day/ml, respectively]
The physiological effects of released insulin denoted by reduction in blood glucose levels are depicted in figure 1B. The fasting blood glucose levels in rats administered with any of the delivery systems were significantly lower (p<0.05) than the diabetic rats in STZ treated group. In case of delivery systems containing insulin alone, and zinc-insulin it was observed that the blood glucose levels dropped suddenly in response to the large amount of insulin released and remained low until 21 days, and then returned to pretreatment levels (~400 mg/dl) quickly. While, chitosan-zinc-insulin complex helped to maintain the blood glucose levels in the range of 100-150 mg/dl until ~63 days. The blood glucose levels were significantly low as compared to the delivery systems containing insulin alone or zinc-insulin until 63 days suggesting that insulin was released slowly from the chitosan-zinc-insulin complex.
Comparison among delivery systems at 45 IU/kg insulin loading:
The in vivo release profile of insulin released, and blood glucose levels of rats treated with the delivery system containing insulin alone, zinc-insulin, and chitosan-zinc-insulin complex at 45 IU/kg insulin loading are presented in figure 2A and B, respectively. The serum insulin levels of animals treated with the delivery system containing chitosan-zinc-insulin complex were significantly different (P<0.05) as compared to that of insulin alone, and zinc-insulin. Serum insulin levels were maintained above 40 μU/ml over 70 days before gradually returning to baseline levels. Increase in insulin AUC by 1.3 and 2 fold was noticed as compared to zinc-insulin, and insulin alone containing formulations. The pharmacodynamic response reflected the pharmacokinetic profile of released insulin in that reduction in blood glucose was observed until ~70 days, and as the insulin release was reduced, blood glucose levels increased and reached to the pretreatment levels. Animals treated with insulin alone or zinc-insulin containing delivery systems showed a sharp drop in insulin levels after ~10 and 16 days, respectively. In the case of formulations containing chitosan-zinc insulin complex, the fasting blood glucose levels remained significantly (P<0.05) low until ~70 days as compared to insulin alone, or zinc-insulin containing formulations. The blood glucose levels were comparable to that of control (untreated group) up to 63 days, and then increased gradually.
For comparing the insulin release and blood glucose levels, insulin solution (2 IU/Kg in PBS) was administered to the diabetic rats via SC route, and the blood glucose and serum insulin levels were measured at 0.5, 1, 2, 4, 6, 8, 12 and 24 h post-injection. Immediately after subcutaneous administration, serum insulin levels increased rapidly, and the data showed values of Cmax and Tmax of 55.75±6.4 μU/ml and 1 h, respectively (figure S1A, supplementary information). Corresponding sudden decline in blood glucose levels was noticed, and reached to ~20% of the pre-administration levels within 1 h (figure S1B, supplementary information). Insulin levels reduced over the period of 12 h, and reached below the detection limit. Similarly, blood glucose reached to the pretreatment levels after 12 h.
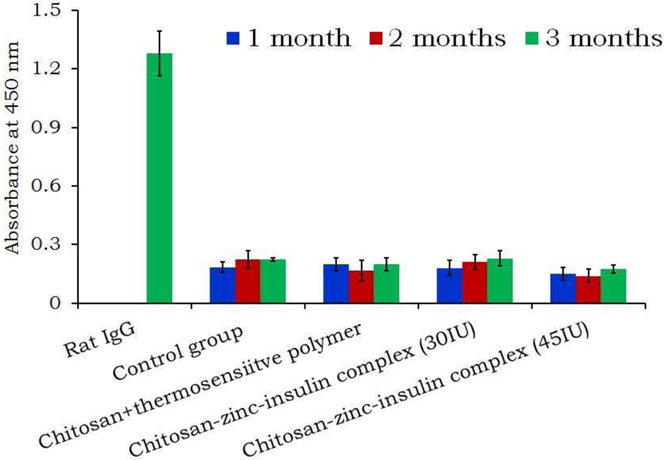
Detection of anti-insulin (rH) antibodies:
The rat serum samples collected at 1, 2 and 3 month time points were screened for the presence of antibodies against insulin released from the delivery systems, and it was observed that no antibodies against human insulin (rH) were developed (figure 3). For comparison purposes, rat IgG were used as control. No antibodies were observed against released insulin initially or after 90 days of treatment and the antibody response was comparable to that of control (untreated) group. It indicated that the released insulin was non-immunogenic in nature.
Figure 3:
Detection of anti-insulin (rH) antibodies in rat serum treated with formulations at different insulin dosing.
Body weight determination:
Initially after STZ injection a marked reduction in the body weight of rats was observed in all treatment groups. The STZ treatment group showed continuous loss of body weight at the end of three months. The rats treated with insulin formulations showed a gradual weight gain, and was significantly (P<0.05) higher than STZ treated animals (figures S2, and S3A-B, supplementary information). Though there was no significant difference observed in the body weights of rats in either of the treatment groups, the chitosan-zinc-insulin complex treated animals showed progressive weight gain and were comparable to that of non-diabetic control.
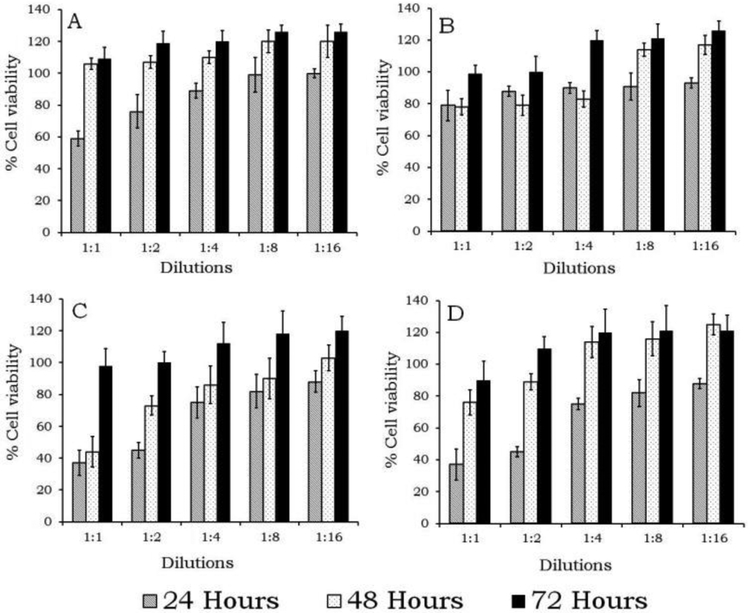
In vitro biocompatibility of the delivery systems:
Figure 4 A-D shows the cell viability quantitatively measured by an MTT assay for thermosensitive polymeric delivery system with and without chitosan incubated at 37 and 70°C, respectively for 10 days. It was observed that the HEK293 cells grew better in the extracts prepared from chitosan containing thermosensitive delivery systems than unmodified (thermosensitive polymer only), and PBS, or DMSO treated cells (Figure S4 A-F, supplementary information). Initially, at 24 h the cell viability was ~60-80% for the concentrated polymeric extracts (1:1 dilution with growth medium), while the extracts diluted to 1:16 ratio showed close to 100% cell growth. At 48 and 72 h, no significant difference (p>0.05) in the cell viability was observed as compared to control (growth medium only), and instead the polymeric delivery system containing chitosan showed higher cell viability as compared to the cells treated with polymeric extracts without chitosan.
Figure 4:
In vitro biocompatibility of the delivery systems containing chitosan + thermosensitive polymer extracts prepared by incubating the delivery systems for 10 days, A) 37, and B) 70°C, and thermosensitive polymer only at C) 37, and D) 70°C determined by MTT cell viability assay [n=6, mean ± SD]
In vivo biocompatibility of the delivery system:
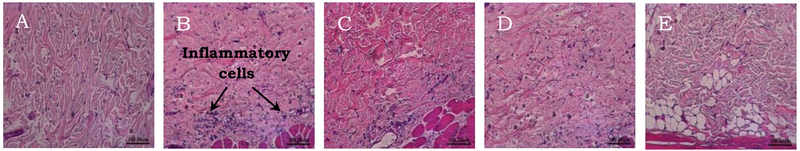
The rats were injected with the polymeric delivery systems containing chitosan, and the inflammatory response to the foreign material was observed, and compared to that of control (untreated), and is presented in figure 5. Histology of untreated skin (control group) is presented in figure 5A. The representative light microscopy images of skin following administration of chitosan containing thermosensitive polymeric delivery system at 1, 7, 30 and 90 days is shown in figure 5B-E. The severity of the response to the foreign material was observed by the presence of leukocytes and fibroblasts near the site of injection. The nuclei of the neutrophils or other inflammatory cells are stained purple after H & E staining, and thus can be easily identified from the surrounding connective tissue. Figures 5B and C represent the clear incidence of acute inflammatory response to the polymeric delivery system containing chitosan, at day 1 and 7, respectively. Large neutrophil infiltration at the site of injection was observed initially. Chronic inflammatory response to the delivery system at day 30 is depicted in figure 5D. However, this response subsided considerably 30 days post-injection, indicated by the presence of few inflammatory cells, and the skin tissue surrounding the delivery system closely resembled to that of control at 90 days (figure 5E). Similar type of inflammatory response was observed in case of rats treated with only thermosensitive polymeric delivery system without chitosan as presented in figure S5 A-D (supplementary information). Thus, it was noticed that the subcutaneous administration of polymeric delivery systems with/without chitosan showed an inflammatory response due to injection and continual presence of polymeric gel in the body. But, at the end of the study no signs of chronic inflammation, or necrosis were observed.
Figure 5:
Light micrographs of rat skin histology after H and E staining: A) Control; and subcutaneous skin tissue sampled after injecting the delivery systems containing chitosan + thermosensitive polymer at B) Day 1, C) Day 7, D) Day 30 and E) Day 90
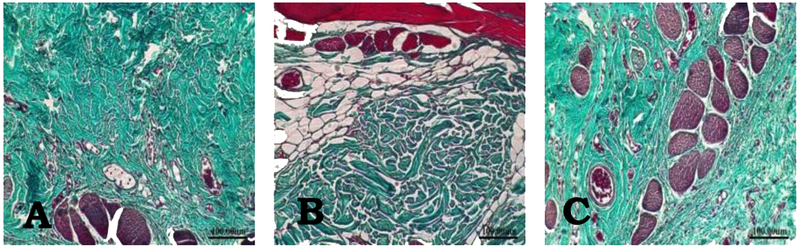
To determine the degree of collagen deposition at the tissue-delivery system interface, the skin samples were also stained with Gomori’s trichome stain which specifically stains collagen (figures 6A-C). The collagen density determined by ImageJ 1.45 software showed that the collagen deposition increased until 30 days (figure 6B), but was comparable to the control at the end of the study (90 days) (figure 6C). The skin histology of animals treated with thermosensitive polymer (without chitosan), is presented in supplementary information (figure S6 A-B supplementary information). The results indicate that the addition of chitosan did not change the biocompatible nature of the thermosensitive polymeric delivery system.
Figure 6:
Light micrographs of rat skin histology after staining with Gomori’s trichrome stain: A) Control; and skin subcutaneous tissue sampled after injecting the delivery systems containing chitosan + thermosensitive polymer at B) Day 30, C) Day 90.
DISCUSSION
Various strategies have been utilized to reduce the initial burst release of insulin, and to preserve its structural integrity during formulation, storage and release from depot forming polymeric delivery systems. In our previously published work [27], we developed a controlled release delivery system to deliver insulin at basal level by incorporating chitosan-zinc-insulin complex into PLA-PEG-PLA (4500 Da) thermosensitive triblock copolymer. A combination approach was employed by utilizing the characteristic properties of insulin, such as self-assembly into hexamers in presence of zinc and their ability to interact with chitosan electrostatically to form chitosan-zinc-insulin complexes. Our in vitro release studies indicated that the increased size of chitosan-zinc-insulin complex helped to reduce complex diffusion from the thermosensitive polymer gel matrix, and prolonged the insulin release in vitro. This slow diffusion of insulin resulted in reduced initial burst release, and further the complex helped to stabilize insulin during release and storage, while providing controlled release over extended duration in vitro [27]. Various analytical techniques such as circular dichroism (CD), differential scanning Calorimetry (DSC), polyacrylamide gel electrophoresis (PAGE)/SDS-PAGE, high-performance liquid chromatography (HPLC), and matrix-assisted laser desorption/ionization-time-of-flight mass spectrometry (MALDI-TOF MS) confirmed the conformational and chemical stability of insulin released from the delivery systems. The complex formation between chitosan and zinc-insulin also protected insulin from the acidic degradation products formed during copolymer degradation, and stabilized insulin inside the delivery system without aggregation or degradation.
The acidic byproducts formed during degradation of the triblock copolymer lead to decrease in pH of microenvironment in the gel matrix, which is the major cause of insulin instability. This acidic microclimate can be reduced by incorporating a basic excipient in the delivery system [32]. Chitosan possesses abundant amino groups on its surface, and hence, acts as proton sponge [33,34]. It also possesses good buffering ability which could resist the major pH change in the microenvironment of during degradation of polymer gel matrix. Our preliminary results indicated that the addition of chitosan to zinc-insulin could have reduced the exposure of protein to the damaging environment resulting from PLA degradation, leading to increased stability. Our studies also demonstrated that the presence of lactic acid residues reduced the thermostability of insulin alone and zinc-insulin, but did not significantly affect insulin in the form of chitosan-zinc-insulin complex determined by DSC (data unpublished). These results further confirmed the stabilizing effect of chitosan on insulin structure.
A single dose STZ induced diabetic rat model is widely accepted experimental model to study the effect of various controlled release insulin formulations. A single dose STZ (55 mg/kg) causes selective toxicity to pancreatic beta cells, and produces type 1 diabetes in the experimental animals [35]. STZ action is manifested via alkylation of DNA, which in turn causes drastic reduction in insulin level affecting overall glucose metabolism in the body, and thereby producing hyperglycemia. The blood glucose levels of rats after STZ treatment increased rapidly, and were hyperglycemic after 5-7 days. As expected, SC injection of insulin solution demonstrated the shortest duration of action and the blood glucose levels reverted to the pretreatment levels within 12 h post treatment. The factors which alter the insulin absorption after subcutaneous administration are its molecular weight, and association state at the administration site [36]. The results showed that after SC administration of insulin solution, insulin being in its monomeric form was absorbed quickly leading to a spike in insulin levels. The polymeric delivery system containing insulin alone also demonstrated a rapid increase in serum insulin concentration, indicating an initial burst release due to the quick escape of unassociated surface-localized insulin monomers after injection. These surface localized insulin monomers being smaller in size might have escaped easily by diffusion, resulting in a spike in insulin levels. Additionally, the delivery system showed a short-term release of insulin which could be due to the aggregation or degradation of insulin in the delivery system. These results were also supported by the reduction in pharmacodynamic response of insulin. Addition of zinc to insulin reduced the initial burst due to the increased size and reduced solubility of insulin. It also helped in relatively sustaining the release of insulin for longer duration as compared to insulin alone. Zinc is known to exhibit fibrillation inhibitory effect on insulin, and stabilizes hexameric assembly [14]. Although zinc-insulin hexamer formation helped to reduce the initial burst release of insulin and prolonged the release duration, there was no appreciable improvement in the bioavailability as compared to the formulations containing insulin alone. The delivery systems containing chitosan-zinc-insulin complex showed marked reduction in the initial burst release, indicated by a gradual and slow rise in serum insulin levels. This might be due to the enlarged size (zinc-insulin hexamer), and the complex formation with chitosan by electrostatic interactions which might have helped in reducing insulin diffusion from the polymer gel matrix.
The initial burst release of insulin is the major cause of hypoglycemia and is a critical aspect which needs to be addressed during the development of controlled delivery systems. The balance between glucose production and its utilization gets altered due to the large variation in plasma insulin levels after its administration [37]. Reduction in peak/trough ratio of insulin i.e. lowering the variability is highly desirable to lower/prevent the occurrence of hypoglycemia-associated complications [38]. Formulations containing chitosan-zinc-insulin showed a gradual increase in serum insulin with very low peak-free levels after administration, and additionally the release was continuous for ~70 days. These formulations also showed increase in AUC by 1.2-2 fold as compared to zinc-insulin and insulin alone containing formulations, respectively. This could be due to the slow dissociation of large chitosan-zinc-insulin complexes, into insulin oligomers and finally to zinc-free insulin monomers. Being a controlled delivery system, the chitosan-zinc-insulin complex loaded thermosensitive polymeric delivery system released small amount of insulin over prolonged period of time leading to higher absorption rates. It has been well documented that the absorption rate of insulin via subcutaneous route is a complex phenomenon, and is inversely related to its concentration [39]. Thus, the slow dissociation of insulin from the chitosan-zinc-insulin complex might have reduced its degradation by the proteases present at the injection site, and thereby improved its absorption [14]. Since chitosan is known to stabilize proteins [40-43], the complex formation might have offered additional stabilizing effect which protected insulin after administration. These results also confirmed our earlier findings showing that chitosan-zinc-insulin containing thermosensitive polymeric delivery system maintained at body temperature preserved the structural integrity of incorporated insulin for prolonged period [27].
The pharmacodynamic effect of insulin released from different delivery systems was evaluated by the regulation of blood glucose levels. The high initial burst release of insulin observed after administration of formulations containing inulin alone caused rapid reduction in blood glucose levels below the normal levels, and suggested that the delivery system containing insulin alone would not be a good choice, since it may lead to a hypoglycemic shock. In case of formulations containing 45IU/kg insulin alone, the Cmax of insulin in rat serum reached to >70 μU/ml, and a quick drop in the blood glucose reaching to ~100mg/dL was observed. But, no severe physical and behavioral symptoms/changes (i.e., tremors/convulsions/hypoglycemic shock) due to hypoglycemia were noticed. These results suggest an initial burst release from the formulation, however, the amount of insulin released was not sufficient enough to cause hypoglycemia. It is also possible that the characteristic coprophagic behavior of rats might have contributed towards the prevention of severe hypoglycemic episodes [44]. Zinc-insulin containing formulations did not show a sharp drop in blood glucose, indicating reduction in initial burst release due to formation of zinc-insulin hexamers (increased size, and reduced solubility), but lowered the blood glucose levels for slightly longer duration as compared to insulin alone. The results suggest that the incorporated insulin might have precipitated/degraded in the delivery system, and failed to elicit the biological response. Chitosan-zinc-insulin containing formulations (insulin loading: 30 and 45 IU/kg) showed gradual and sustained reduction in blood glucose over the period of 7 days, without any sign of hypoglycemia. This is considered as the most important and desirable property of insulin containing controlled delivery systems. The delivery systems containing chitosan-zinc-insulin complexes helped maintaining the blood glucose levels below 200 mg/dl, for prolonged duration as compared to insulin alone or zinc-insulin containing delivery systems. Additionally, the blood glucose levels were comparable to that of control (untreated rats) for considerably longer duration and then increased gradually. The results also showed that there was no significant difference (P>0.05) in blood glucose levels in two consecutive time points until 56-63 days, which can be interpreted as the pharmacodynamic manifestation of the continuous release of insulin at a steady rate. This data also demonstrates that the biological activity of insulin released from chitosan-zinc-insulin complex was preserved during fabrication and maintained during the entire release duration. All the delivery systems released insulin for relatively shorter period in vivo as compared to in vitro release. It has been well documented and also observed in our earlier studies that the in vivo release duration of insulin was shorter as compared to that of observed during in vitro release, which could be as a result of faster degradation of the delivery system in vivo than in vitro [14,45]. But, as far as the biological activity of released insulin is concerned, chitosan-zinc-insulin complex containing delivery systems showed better glycemic control over longer duration as compared to the delivery system containing insulin alone or zinc-insulin.
Some of the macro and micro vascular complications due to diabetes include stroke, neuropathy, amputations, retinopathy, and renal failure, leading to increased disability, reduced life expectancy, and huge health costs [46]. The animals in the streptozotocin treatment group developed not only diabetes as indicated by increased fasting blood glucose values, but also showed signs of cataract which is one of the earlier complications of diabetes mellitus. Similarly, the animals treated with the delivery systems containing insulin alone also showed signs of cataract by the end of study indicating that the delivery system did not release insulin sufficient enough to alleviate the diabetic complications. No signs of retinopathy were observed in rats treated with zinc-insulin or chitosan-zinc-insulin containing formulations indicated that the released insulin helped in preventing the onset of diabetes related microvascular complications. It has been reported that STZ induced diabetes causes reduction in body weight due to the loss/degradation of structural proteins, which mainly contribute to the body weight [47]. Thus, after STZ treatment, a significant and drastic weight loss was observed in all groups. A gradual improvement in body weight was noticed after administering the rats with insulin formulations, while the rats in STZ treatment group showed continuous weight loss. This increase in body weight may be due to the prolonged release and in turn effect of insulin from the delivery system.
Proteins undergo physical degradation like unfolding, misfolding, aggregation, or chemical degradation such as oxidation, deamidation, isomerization, that can result in an immune response [48]. Protein aggregation in the commercially available preparations has reported to be a key factor underlying the unwanted immune responses of therapeutic proteins. Insulin aggregates are known to invoke antibody formation [49], and hence insulin aggregation inside the delivery system could alter its release, stability, activity, safety and overall duration of action after administration. Fineberg et al. [50], have reported that the formulation is one of the crucial factors that alter the immunogenic potential of insulin. Soluble forms of insulin are known to be less allergenic than intermediate or long-acting insulin preparations. The acidic preparations of insulin are reported to be more immunogenic than neutral formulations. Our ELISA results indicated that no immune response against human insulin observed in all treatment groups, which signified that the released insulin was non-immunogenic in nature.
Biocompatibility is an array of complex characteristics and indicates the level of interaction between the implanted delivery system and the host tissue. It is difficult to determine the biocompatibility of a material by a single method, and always require complex set of in vitro and in vivo methods. In our earlier studies we have already demonstrated the biodegradable and biocompatible nature of the thermosensitive polymeric delivery system (PLA-PEG-PLA, Mw: 4500 Da) in vitro [14]. Chitosan, another polymer used in this study is a linear polysaccharide composed of β-(1-4)-linked D-glucosamine and N-acetyl-D-glucosamine units distributed randomly. Chitosan is eliminated from the body by renal clearance, and the degree of acetylation as well as its molecular weight affects the degradation rate. High molecular weight chitosan undergoes degradation by chitinases in the body leading to the formation of smaller chains [51,52]. It is reported as a biocompatible and biodegradable positively charged polymer with minimum immunogenic potential and also possesses low cytotoxic potential [53]. Zinc gets eliminated from body via renal clearance [54]. It is important to consider the potential cytotoxicity of the thermosensitive polymer (PLA-PEG-PLA) with or without chitosan, and its residual degradation products. An indirect cytotoxicity method was used, where the cells were exposed to the polymer extracts prepared at 37 and 70°C which simulated the long-term effects of the injected depot forming delivery systems [55,56]. Prior to the treatment, the extracts were neutralized to disregard the effect of pH, and to emphasize on the effect of polymer degradation products on cell viability. Therefore, the results showed the effect of concentration of polymer and its degradation products only on the cell viability. Growth medium without polymer served as negative control and used to determine the percent cell viability. Our in vitro cytotoxicity study results indicated that the addition of chitosan did not change the biocompatible nature of the delivery system containing thermosensitive polymer. The polymer extracts of thermosensitive copolymer containing chitosan prepared at 70°C showed higher cell viability in comparison to extract prepared at 37°C. Chitosan has been found to exhibit good biocompatibility and extremely low cell toxicity [53]. Chitosan accelerates cell proliferation, and also possesses wound healing property [57]. Since greater amount of chitosan would be extracted in its low molecular weight soluble form at 70°C, which has led to-lesser cell toxicity than the extract prepared at 37°C. In an effort to determine the biocompatible nature of the delivery system in vivo, the subcutaneous tissue surrounding the depot was excised and observed for inflammatory reactions. Tissue healing process is usually initiated through cascade of inflammatory stages including acute inflammation, chronic inflammation, and granular tissue formation at the injection site [58,59]. During in vivo biocompatibility evaluation, it was noticed that the subcutaneous administration of polymeric systems with/without chitosan showed an inflammatory response due to injection and continual presence of polymeric gel in the body. But, at the end of the study no signs of chronic inflammation, or necrosis were observed. Thus, as expected the inflammatory response to the developed delivery systems was short-lived, and the delivery systems were biocompatible.
The extent of fibrosis, organization of collagen fibers and collagen density around the depot are also important in determining the biocompatible nature of the depot forming systems. Gomori’s trichrome stain was used to determine the nature and presence of collagen deposition at the subcutaneous tissue-delivery system interface. Though frequent removal and replacement of the release medium during in vitro release reduces the acidic environment with subsequent reduction in protein degradation, it is difficult to predict whether it reflects in vivo conditions [60]. It has been reported that the fibrous capsule formation around the delivery system possibly retards the effective elimination of the polymer degradation products out of the site [60]. This leads to increased acidic microenvironment near injection site, and in turn reduces the stability of encapsulated protein. It has been reported that usually the collagen fibers are arranged randomly without a specific organization with a sparse density, but in response to injury due to implanted material, collagen become well-defined and increased collagen deposition is usually observed near the site of implantation [61]. In our experiments, it was noted that the collagen deposition at the site of injection was a short-term response. Increased collagen deposition was observed initially, but the its density reduced eventually and the skin tissue observed at the end of the study period showed absence of residual scar tissue indicated the biocompatible nature of the delivery system. Since no scar tissue/fibrous capsule were observed near the gel depot, it allowed us to conclude that polymer degradation products are removed continuously after degradation from the injection site.
CONCLUSIONS
Thus, in vivo studies indicated chitosan-zinc-insulin complex containing delivery systems controlled the release of insulin over 70 days, necessary to maintain the basal insulin levels. The released insulin was in its monomeric and biologically active form which was absorbed in the body indicated by reduced blood glucose levels. The formulations containing insulin did not provoke any immunogenic response, and helped to reduce the diabetic complications. The polymeric delivery system containing chitosan was biodegradable and biocompatible in vivo. This signifies that the chitosan-zinc-insulin complex incorporated in the thermosensitive polymeric delivery system can be used as an alternative to the conventional daily multiple dose basal insulin therapy.
Supplementary Material
ACKNOWLEDGEMENTS
The authors gratefully acknowledge the financial support provided by NIH#HD56053 and Fraternal Order of Eagles grants.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Adhikari S, Adams-Huet B, Wang Y-CA, Marks JF, White PC, Institution of basal-bolus therapy at diagnosis for children with type 1 diabetes mellitus, Pediatrics. 123(4) (2009) e673–e678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guthrie R, Is there a need for a better basal insulin?, Clin. Diabetes 19(2) (2001) 66–70. [Google Scholar]
- 3.Kruszynska YT, Home PD, Hanning I, Alberti KG, Basal and 24-h C-peptide and insulin secretion rate in normal man, Diabetologia. 30(1) (1987) 16–21. [DOI] [PubMed] [Google Scholar]
- 4.Moses RG, Bartley P, Lunt H, O’Brien RC, Donnelly T, Gall M-A, Vesterager A, Wollmer P, Roberts A, Safety and efficacy of inhaled insulin (AERx® iDMS1) compared with subcutaneous insulin therapy in patients with Type 1 diabetes: 1-year data from a randomized, parallel group trial, Diabet Med 26(3) (2009) 260–267. [DOI] [PubMed] [Google Scholar]
- 5.Jani R, Triplitt C, Reasner C, Defronzo RA, First approved inhaled insulin therapy for diabetes mellitus, Expert Opin. Drug. Deliv 4(1) (2007) 63–76. [DOI] [PubMed] [Google Scholar]
- 6.Leary AC, Dowling M, Cussen K, O’Brien J, Stote RM, Pharmacokinetics and pharmacodynamics of intranasal insulin spray (Nasulin™) administered to healthy male volunteers, J. Diabetes. Sci. Technol 2(6) (2008)1054–1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Modi P, Mihic M, Lewin A, The evolving role of oral insulin in the treatment of diabetes using a novel RapidMist System, Diabetes Metab. Res. Rev 18 (2002) S38–S42. [DOI] [PubMed] [Google Scholar]
- 8.Radermecker RP, Renard E, Scheen AJ, Circulating insulin antibodies: influence of continuous subcutaneous or intraperitoneal insulin infusion, and impact on glucose control, Diabetes Metab. Res. Rev 25(6) (2009) 491–501. [DOI] [PubMed] [Google Scholar]
- 9.Robertson KJ, Schoenle E, Gucev Z, Mordhorst L, Gall M-A, Ludvigsson J, Insulin detemir compared with NPH insulin in children and adolescents with Type 1 diabetes, Diabet. Med 24(1) (2007) 27–34. [DOI] [PubMed] [Google Scholar]
- 10.Philips J-C, Scheen A, Insulin detemir in the treatment of type 1 and type 2 diabetes. Vasc. Health Risk Manag 2(3) (2006) 277–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heller S, Koenen C, Bode B, Comparison of insulin detemir and insulin glargine in a basal-bolus regimen, with insulin aspart as the mealtime insulin, in patients with type 1 diabetes: A 52-week, multinational, randomized, open-label, parallel-group, Treat-to-Target noninferiority trial, Clin. Ther 31(10) (2009) 2086–2097. [DOI] [PubMed] [Google Scholar]
- 12.Meneghini LF, Rosenberg KH, Koenen C, Merilainen MJ, Lüddeke H-J, Insulin detemir improves glycaemic control with less hypoglycaemia and no weight gain in patients with type 2 diabetes who were insulin naive or treated with NPH or insulin glargine: clinical practice experience from a German subgroup of the predictive study. Diabetes Obes. Metab 9(3) (2007) 418–427. [DOI] [PubMed] [Google Scholar]
- 13.Hirsch IB, Insulin analogues N Engl. J. Med 352(2) (2005) 174–183. [DOI] [PubMed] [Google Scholar]
- 14.Al-Tahami K, Oak M, Mandke R, Singh J, Basal level insulin delivery: in vitro release, stability, biocompatibility, and in vivo absorption from thermosensitive triblock copolymers, J. Pharm. Sci 100(11) (2011) 4790–4803. [DOI] [PubMed] [Google Scholar]
- 15.Manoharan C, Singh J, Evaluation of polyanhydride microspheres for basal insulin delivery: Effect of copolymer composition and zinc salt on encapsulation, in vitro release, stability, in vivo absorption and bioactivity in diabetic rats, J. Pharm. Sci 98(11) (2009) 4237–4250. [DOI] [PubMed] [Google Scholar]
- 16.Huynh DP, Nguyen MK, Pi BS, Kim MS, Chae SY, Lee KC, Kim BS, Kim SW, Lee DS, Functionalized injectable hydrogels for controlled insulin delivery, Biomaterials. 29(16) (2008) 2527–2534. [DOI] [PubMed] [Google Scholar]
- 17.Choi S, Kim SW, Controlled release of insulin from injectable biodegradable triblock copolymer depot in ZDF rats, Pharm. Res 20(12) (2003) 2008–2010. [DOI] [PubMed] [Google Scholar]
- 18.Al-Tahami K, Singh J, Smart polymer based delivery systems for peptides and proteins. Recent Pat. Drug Deliv. Formul 1(1) (2007) 65–71. [DOI] [PubMed] [Google Scholar]
- 19.Phillips NB, Wan Z, Whittaker L, Hu S-Q, Huang K, Hua QX, Whittaker J, Ismail-Beigi F, Weiss MA, Supramolecular protein engineering, design of zinc-stapled insulin hexamers as a long acting depot. J. Biol. Chem 285(16) (2010) 11755–11759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dunn MF, Zinc-ligand interactions modulate assembly and stability of the insulin hexamer--a review. Biometals 18(4) (2005) 295–303. [DOI] [PubMed] [Google Scholar]
- 21.Luppi B, Bigucci F, Mercolini L, Musenga A, Sorrenti M, Catenacci L, Zecchi V, Novel mucoadhesive nasal inserts based on chitosan/hyaluronate polyelectrolyte complexes for peptide and protein delivery. J. Pharm. Pharmacol 61(2) (2009) 151–157. [DOI] [PubMed] [Google Scholar]
- 22.Jintapattanakit A, Peungvicha P, Sailasuta A, Kissel T, Junyaprasert VB, Nasal absorption and local tissue reaction of insulin nanocomplexes of trimethyl chitosan derivatives in rats. J. Pharm. Pharmacol 62(5) (2010) 583–591. [DOI] [PubMed] [Google Scholar]
- 23.Jintapattanakit A, Junyaprasert VB, Mao S, Sitterberg J, Bakowsky U, Kissel T, Peroral delivery of insulin using chitosan derivatives: a comparative study of polyelectrolyte nanocomplexes and nanoparticles, Int. J. Pharm 342(1–2) (2007) 240–249. [DOI] [PubMed] [Google Scholar]
- 24.Jintapattanakit A, Junyaprasert VB, Kissel T, The role of mucoadhesion of trimethyl chitosan and PEGylated trimethyl chitosan nanocomplexes in insulin uptake, J. Pharm. Sci 98(12) (2009) 4818–4830. [DOI] [PubMed] [Google Scholar]
- 25.Mao S, Bakowsky U, Jintapattanakit A, Kissel T, Self-assembled polyelectrolyte nanocomplexes between chitosan derivatives and insulin. J. Pharm. Sci 95(5) (2006) 1035–1048. [DOI] [PubMed] [Google Scholar]
- 26.Jin Y, Zhou D, Yang H-Y, Zhu X, Wang X-R, Zhang Z-R, Huang Y, Effects of degree of quaternization on the preparation and characterization of insulin-loaded trimethyl chitosan polyelectrolyte complexes optimized by central composite design, Pharm. Dev. Technol (2011) [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 27.Oak M, Singh J, Controlled delivery of basal level of insulin from chitosan-zinc-insulin-complex-loaded thermosensitive copolymer, J. Pharm. Sci 101(3) (2012) 1079–1096. [DOI] [PubMed] [Google Scholar]
- 28.Mercodia-Insulin ELISA kit Manual. 2011. (http://www.mercodia.se/)
- 29.Gupta S, Chattopadhyay T, Pal Singh M, Surolia A, Supramolecular insulin assembly II for a sustained treatment of type 1 diabetes mellitus. Proc. Natl. Acad. Sci. U. S. A 107(30) (2010) 13246–13251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Al-Tahami K, Oak M, Singh J. Controlled delivery of basal insulin from phase-sensitive polymeric systems after subcutaneous administration: in vitro release, stability, biocompatibility, in vivo absorption, and bioactivity of insulin, J. Pharm. Sci 100(6) (2011) 2161–2171. [DOI] [PubMed] [Google Scholar]
- 31.Rowland M, Tozer TN. Clinical Pharmacokinetics and Pharmacodynamics: Concepts and Applications. Fourth ed., Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 32.Shao PG, Bailey LC, Stabilization of pH-induced degradation of porcine insulin in biodegradable polyester microspheres, Pharm. Dev. Technol 4(4) (1999) 633–642. [DOI] [PubMed] [Google Scholar]
- 33.Sajeesh S, Sharma CP, Novel pH responsive polymethacrylic acid-chitosan-polyethylene glycol nanoparticles for oral peptide delivery, J. Biomed. Mater. Res. A 76B(2) (2006) 298–305. [DOI] [PubMed] [Google Scholar]
- 34.Mandke R, Singh J, Effect of acyl chain length and unsaturation on physicochemical properties and transfection efficiency of N-acyl-substituted low-molecular-weight chitosan, J. Pharm. Sci 101(1) (2012) 268–282. [DOI] [PubMed] [Google Scholar]
- 35.Wu KK, Huan Y, Streptozotocin-induced diabetic models in mice and rats, Curr. Protoc. Pharmacol 40 (2008) 5.47.1–5.47.14. [DOI] [PubMed] [Google Scholar]
- 36.Barichello JM, Morishita M, Takayama K, Nagai T, Absorption of insulin from Pluronic F-127 gels following subcutaneous administration in rats. Int. J. Pharm 184(2) (1999) 189–198. [DOI] [PubMed] [Google Scholar]
- 37.Rizza RA, Mandarino LJ, Gerich JE, Dose-response characteristics for effects of insulin on production and utilization of glucose in man, Am. J. Physiol 240(6) (1981) E630–E639. [DOI] [PubMed] [Google Scholar]
- 38.Takenaga M, Yamaguchi Y, Kitagawa A, Ogawa Y, Mizushima Y, Igarashi R, A novel insulin formulation can keep providing steady levels of insulin for much longer periods in-vivo, J. Pharm. Pharmacol 54 (9)(2002) 1189–1194. [DOI] [PubMed] [Google Scholar]
- 39.Li J, Johnson JD, Mathematical models of subcutaneous injection of insulin analogues: A mini-review, 12(2) Discrete Continuous Dyn. Syst. Ser. B (2009) 401–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Calvo P, Remuñan-López C, Vila-Jato JL, Alonso MJ, Chitosan and chitosan/ethylene oxide-propylene oxide block copolymer nanoparticles as novel carriers for proteins and vaccines, Pharm. Res 14(10) (1997) 1431–1436. [DOI] [PubMed] [Google Scholar]
- 41.Calvo P, Remuñan-López C, Vila-Jato JL, Alonso MJ, Novel hydrophilic chitosan-polyethylene oxide nanoparticles as protein carriers, J. Appl. Polym. Sci 63(1) (1997) 125–132. [Google Scholar]
- 42.Vila A, Sánchez A, Janes K, Behrens I, Kissel T, Vila Jato JL, Alonso MJ, Low molecular weight chitosan nanoparticles as new carriers for nasal vaccine delivery in mice, Eur. J. Pharm. Biopharm 57(1) (2004)123–131. [DOI] [PubMed] [Google Scholar]
- 43.Fernández-Urrusuno R, Calvo P, Remuñán-López C, Vila-Jato JL, Alonso M, Enhancement of nasal absorption of insulin using chitosan nanoparticles, Pharm. Res 16(10) (1999) 1576–1581. [DOI] [PubMed] [Google Scholar]
- 44.Leonardi R, Rehg JE, Rock CO, Jackowski S, Pantothenate kinase 1 is required to support the metabolic transition from the fed to the fasted state, PLoS ONE, 5(6) (2010) 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kwon YM, Kim SW, Biodegradable triblock copolymer microspheres based on thermosensitive sol-gel transition. Pharm. Res 21(2) (2004) 339–343. [DOI] [PubMed] [Google Scholar]
- 46.International Diabetes Federation. The Global Burden: Diabetes and Impaired Glucose Tolerance (IGT): Prevalence and Projections IDF Diabetes Atlas, 4th ed. Brussels: International Diabetes Federation; 2011. [Google Scholar]
- 47.Veeramani C, Pushpavalli G, Pugalendi K, Antihyperglycaemic effect of Cardiospermum halicacabum Linn. leaf extract on STZ-induced diabetic rats, J. Appl. Biomed 6(1) (2007) 19–26. [Google Scholar]
- 48.Hermeling S, Crommelin DJA, Schellekens H, Jiskoot W, Structure-immunogenicity relationships of therapeutic proteins. Pharm. Res 21(6) (2004) 897–903. [DOI] [PubMed] [Google Scholar]
- 49.Schernthaner G, Immunogenicity and allergenic potential of animal and human insulins, Diabetes Care. 16 (1993) Suppl 3, 155–165. [DOI] [PubMed] [Google Scholar]
- 50.Fineberg SE, Kawabata TT, Finco-Kent D, Fountaine RJ, Finch GL, Krasner AS, Immunological responses to exogenous insulin, Endocr. Rev 28(6) (2007) 625–652. [DOI] [PubMed] [Google Scholar]
- 51.Riva R, Ragelle H, des Rieux A, Duhem N, Jerome C, Preat V. Chitosan and chitosan derivatives in drug delivery and tissue engineering. Adv. Polym. Sci 244 (2011) 19–44. [Google Scholar]
- 52.Kean T, Thanou M. Biodegradation, biodistribution and toxicity of chitosan. Adv. Drug Deliv. Rev 62(1) (2010) 3–11. [DOI] [PubMed] [Google Scholar]
- 53.Mansouri S, Lavigne P, Corsi K, Benderdour M, Beaumont E, Fernandes JC, Chitosan-DNA nanoparticles as non-viral vectors in gene therapy: strategies to improve transfection efficacy, Eur. J. Pharm. Biopharm 57(1) (2004) 1–8. [DOI] [PubMed] [Google Scholar]
- 54.U.S. Environmental Protection Agency Washington D.C. Toxicological review of zinc and compounds. 2005. CAS No. 7440–66-6.
- 55.Ignatius AA, Claes LE, In vitro biocompatibility of bioresorbable polymers: poly(L, DL-lactide) and poly(L-lactide-co-glycolide). Biomaterials. 17(8) (1996) 831–839. [DOI] [PubMed] [Google Scholar]
- 56.Silva GA, Marques AP, Gomes ME, Coutinho OP, Reis RL. Cytotoxicity screening of biodegradable polymeric systems In: Reis RL, Román JS, Editors. In Biodegradable systems in tissue engineering and regenerative medicine, CRC Press LLC; 2004, p. 339–353. [Google Scholar]
- 57.Nwe N, Furuike T, Tamura H, The mechanical and biological properties of chitosan scaffolds for tissue regeneration templates are significantly enhanced by chitosan from Gongronella butleri. Materials 2(2), (2009), 374–398. [Google Scholar]
- 58.Morais JM, Papadimitrakopoulos F, Burgess DJ, Biomaterials/tissue interactions: possible solutions to overcome foreign body response. 12(2) AAPS J (2010) 188–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Onuki Y, Bhardwaj U, Papadimitrakopoulos F, Burgess DJ, A review of the biocompatibility of implantable devices: current challenges to overcome foreign body response, J. Diabetes Sci. Technol 2(6) (2008)1003–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Park TG, Lu W, Crotts G, Importance of in vitro experimental conditions on protein release kinetics, stability and polymer degradation in protein encapsulated poly (d,l-lactic acid-co-glycolic acid) microspheres, J. Control. Release 33(2) (1995) 211–222. [Google Scholar]
- 61.Daugherty AL, Cleland JL, Duenas EM, Mrsny RJ, Pharmacological modulation of the tissue response to implanted polylactic-co-glycolic acid microspheres. Eur. J. Pharm. Biopharm 44(1) (1997) 89–102. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.