Introduction
Although arthroscopically-assisted treatments continue to be explored and analyzed for their effectiveness, the use of diagnostic wrist arthroscopy as an adjunct to a careful history and physical examination remains the reference standard in the patient with pain thought to be originating from within the wrist.
When examined by an experienced hand surgeon, wrist problems in general and carpal instability are diagnosed nearly 75% of the time by history and physical alone.[1, 2] Pertinent history regarding wrist pathology includes: mechanism of injury, exacerbating hand and wrist maneuvers, pain relieving hand and wrist positions/splints, prior corticosteroid injections that had either a positive impact or no impact on symptoms, and prior surgical interventions.
Arthroscopy should be considered in the setting where a patient’s pain has persisted despite non-operative treatment with splinting and/or occupational therapy delivered by a certified hand therapist. A differential diagnosis should be established prior to arthroscopy to increase the probability of identifying a problem that is contributing to a patient’s pain. A clinical scenario where this is best illustrated is the patient with dorsal wrist pain, exacerbated by loading and extension of the wrist. Physical examination, including provocative maneuvers, increase the probability that further diagnostic adjuncts will unveil a problem that can be acted upon clinically. Using advanced imaging or arthroscopy as a screening tool may not have the same clinical impact. Furthermore, although degenerative changes may be apparent upon intra-articular examination, treatment may not improve the patient’s symptoms. History and focused physical examination remain essential in determining whether or not a patient might predictably benefit from therapeutic intervention.
Indications:
Clinically-relevant anatomy:
A systematic approach to evaluation of the wrist by arthroscopy starts with a thorough knowledge of the three-dimensional anatomy of the region. Traditionally, the workhorse arthroscopic portals are positioned over the dorsal wrist, avoiding the risk of injury to the neurovascular structures of the volar wrist. More recently, authors have described volar arthroscopic portals that can be used to examine and repair dorsal soft-tissue structures. [3–8]
The dorsal arthroscopic portals are named for their relation to the extensor compartments: 3–4, 4–5, 6R, 6U, radial midcarpal, and ulnar midcarpal portals. Table 1 describes the anatomic structures that can be seen with each associated portal.
Table 1:
Anatomic structures by portal location (adapted from print Slutsky DJ, Nagle DJ (eds): Techniques in Hand and Wrist Arthroscopy, Philadelphia, Elsevier, 2006.
| Location | |||||
|---|---|---|---|---|---|
| Portal | Radial | Central | Volar | Dorsal/Distal | Ulnar |
| 1–2 Portal | Scaphoid and lunate fossa, dorsal rim of radius | Proximal and radial scaphoid, proximal lunate | Oblique views of the RSC, LRL | Oblique views of the DRC | TFCC poorly visualized |
| 3–4 Portal | Scaphoid and lunate fossa, volar rim of radius | Proximal scaphoid and lunate, dorsal and membranous SLIL | RSC, RSL, LRL, ULL | Oblique views of DRCL insertion onto dorsal SLIL | TFCC radial insertion, central disk, ulnar attachment, PRUL, DRUL, PTO, PSR |
| 4–5 Portal | Lunate fossa, volar rim of radius | Proximal lunate, triquetrum, dorsal and membranous LTIL | RSL, LRL, ULL | Poorly visualized | TFCC radial insertion, central disk, ulnar attachment, PRUL, DRUL, PTO, PSR |
| 6-R Portal | Poorly visualized | Proximal lunate, triquetrum, dorsal and membranous LTIL | UL, ULT | Poorly visualized | TFCC radial insertion, central disk, ulnar attachment, PRUL, DRUL, PTO, PSR |
| 6U Portal | Sigmoid notch | Proximal triquetrum, membranous LTIL | Oblique views of the UL, ULT | Oblique views of DRCL | TFCC oblique views of radial insertion, central disk, ulnar attachment, PRUL, DRUL |
| VR Portal | Scaphoid and lunate fossa, dorsal rim of radius | Scaphoid and lunate fossa, dorsal rim of radius | Palmar scaphoid and lunate, palmar SLIL | Oblique views of RSL, LRL, UL | Oblique views of radial insertion, central disk, ulnar attachment, PRUL, DRUL |
| VU portal | volar and palmar surfaces of the triquetrum and lunate | palmar and proximal portions of the LT ligament | the volar TFCC | Ulnocarpal ligamentous complex | Ulnar wrist capsule |
| Volar midcarpal portal | Proximal capitate articular surface | Capitohamate articulation, capitohamate ligament | Palmar scapholunate and lunotriquetral ligaments | Dorsal radiocarpal, dorsal intercarpal ligaments | Triquetrohamate ligament, triquetrocapitate ligament, ulnar wrist capsule |
| Radial midcarpal portal | STT joint, distal scaphoid pole | SLIL, SL joint, distal scaphoid, distal lunate | Radial limb of radioscaphocapitate ligament | Proximal capitate, CHIL, oblique views of proximal hamate | LTIL joint, partial triquetrum |
| Ulnar midcarpal portal | Distal articular surface of scaphoid | Distal lunate | Volar limb of RSC | Oblique views of proximal capitate, CHIL, proximal hamate | LTIL, LT joint, triquetrum |
| Dorsal DRUJ portal | Sigmoid notch, radial attachment of TFCC | Ulnar head | Palmar radioulnar ligament | Proximal surface of articular disk | Limited view of deep DRUL |
| Volar DRUJ portal | Sigmoid notch, radial attachment of TFCC | Ulnar head | Dorsal radioulnar ligament | Proximal surface of articular disk | Foveal attachment of deep fibers of TFCC |
RSC – radioscaphocapitate ligament, LRL – long radiolunate ligament, DRC – dorsal radiocarpal ligament, TFCC – triangular fibrocartilage complex, SLIL – scapholunate interosseous ligament, RSL – radioscapholunate ligament, UL – ulnolunate ligament, PRUL – palmar radioulnar ligament, DRUL – dorsal radioulnar ligament, PTO – pisotriquetral orifice, PSR – pre-styloid recess, LTIL – lunotriquetral interosseous ligament, ULT ulnotriquetral ligament, CHIL – capitohamate interosseous ligament
Wrist arthroscopy technique:
The correct instrumentation and arthroscopy setup must be confirmed prior to initiating the delivery of anesthesia. Arthroscopy can be performed either with general anesthetic or regional anesthetic and sedation.
The patient is placed in the supine position with the shoulder abducted and elbow flexed at 90 degrees. A tourniquet is placed above the elbow and the arm is padded in preparation for traction. The arm is secured to the hand table using a soft, gauze wrap. Traction is applied through appropriately-sized finger traps to gently distract the wrist.
If the pulley system is positioned correctly, the fingers will be directly collinear with the forearm.
The surgeon is seated on the side of the side of the hand table toward the feet of the patient. The arthroscopy viewing tower should be placed across from the surgeon. The assistant, important for stabilizing the forearm and wrist, can be seated on either side of the hand table. (Figure 1)
Figure 1.
Patient positioning
Standard equipment includes a 2.7 mm, 30 degree angled arthroscope, a 3-mm hook probe, and overhead traction. Instruments that are used in the treatment of intra-articular pathology include a radiofrequency ablation probe and a mechanical shaver. The shaver may be necessary to clear the wrist of synovitis or degenerative soft tissue changes in order to perform a comprehensive diagnostic evaluation of the wrist.
Traditionally, arthroscopy has been performed using fluid for articular distension and visualization and “wet” arthroscopy has been considered reference standard. Recently, surgeons have challenged this paradigm and have elected to perform “dry” arthroscopy where no fluid is injected into the wrist. Proponents of the dry technique believe that fluid can disrupt normal tissue planes, making conversion to open surgery more difficult. Dry arthroscopy may also have a role in intra-articular fracture reduction and bone grafting. [9, 10] This article will focus on “wet” arthroscopy.
Dorsal Portals: 3–4 portal
The 3–4 portal is used to gain entry into the radiocarpal joint. Found at approximately 1 cm distal to the Lister tubercle, the 3–4 portal exists in the soft-tissue concavity between the extensor pollicis longus (EPL) tendon and the extensor digitorum communis (EDC) tendons. After exsanguinating the extremity, the tourniquet is inflated to 100 mgHg above the most recent systolic blood pressure. (Figure 1)
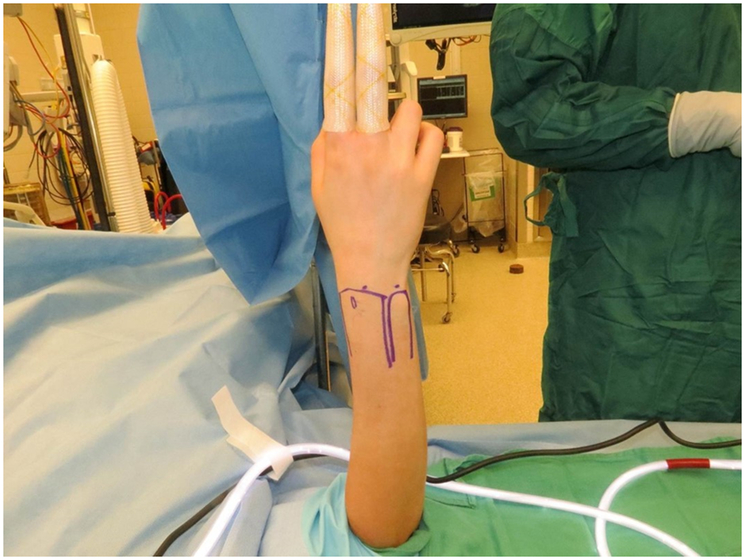
An 18-gauge needle attached to a 10-cc saline-filled syringe is inserted into the 3–4 portal at approximately 10 degrees of inclination toward the hand. This assumes that there is normal volar tilt of the radius (11 degrees). (Figure 2)
Careful inspection and palpation of the surface anatomy avoids inadvertent tendon injury. The bevel of the needle should be positioned parallel to the extensor tendons to reduce the risk of tendon laceration.
If the needle does not enter the portal in perfect position, it may be difficult to place or manipulate the position of the arthroscope, resulting in poor visualization of wrist structures.
Figure 2.
Entering the 3–4 portal
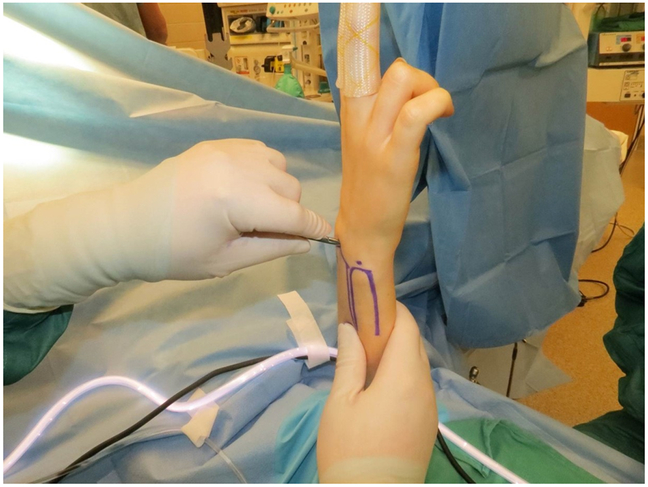
Entry into the joint will be felt by a loss of resistance and a distinct “pop” through the dorsal capsule. The radiocarpal joint can be distended with 5 cc of saline to confirm needle placement. An 11-blade scalpel is then used to increase the size of the skin incision. (Figure 3)
The blade should be placed along the needle, parallel to the extensor tendons, and used to cut skin only.
Figure 3.
Making Skin incision
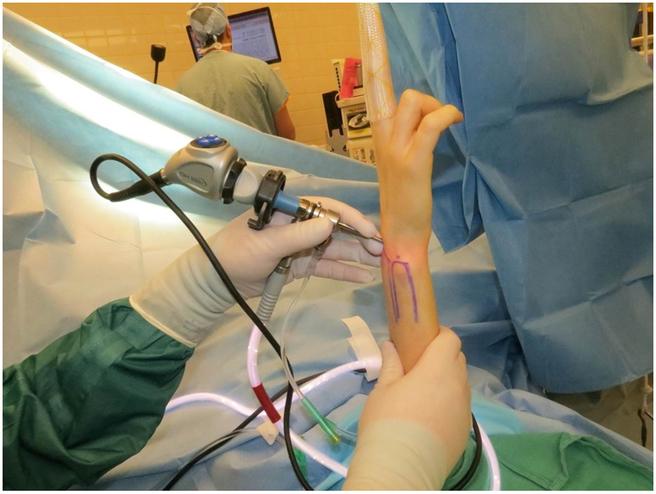
After removing the needle, a mosquito or narrow hemostat is directed along the same path into the radiocarpal joint. Gentle spreading of the mosquito will enlarge the capsular opening and permit entry of the arthroscope. (Figure 4) A blunt cannula is used to position the 2.7 mm arthroscope within the radiocarpal joint.
The arthroscope should be directed along the path that has been created by the mosquito. If slightly off, the trocar will not pass into the joint and may damage the articular surfaces of the distal radius, scaphoid, or lunate. (Figure 5)
Figure 4.
Enlarging the skin incision
Figure 5.
Placing the arthroscope within the radiocarpal joint
4–5, 6U, and 6R portal:
If wet arthroscopy is desired, gravity-driven inflow can be provided by the 6R or 6U portal or via the arthroscopic cannula. Outflow can be directed through the cannula or through the ulnar-sided portals, depending on the direction of inflow.
Periodic irrigation and outflow of arthroscopic fluid will clear debris such as blood, clot, and loose cartilage bodies.
The 4–5 portal is accessed similar to the 3–4 portal. The point of entry is the interval between the EDC and extensor digiti minimi (EDM) tendons, over the radiocarpal joint.
Remembering that the normal inclination of the radius is approximately 22 degrees, the entry point for the 4–5 portal is slightly more proximal than the 3–4 portal.
Needle placement within the radiocarpal joint can be confirmed by direct arthroscopic visualization.
The 6R and 6U portals are designated by their relationship, radial (R) or ulnar (U), to the extensor carpi ulnaris tendon (ECU). The arthroscope can be used to triangulate and identify a safe entry point on either side of the tendon. Entry into the joint is again directly visualized.
Systematic dorsal, radiocarpal evaluation:
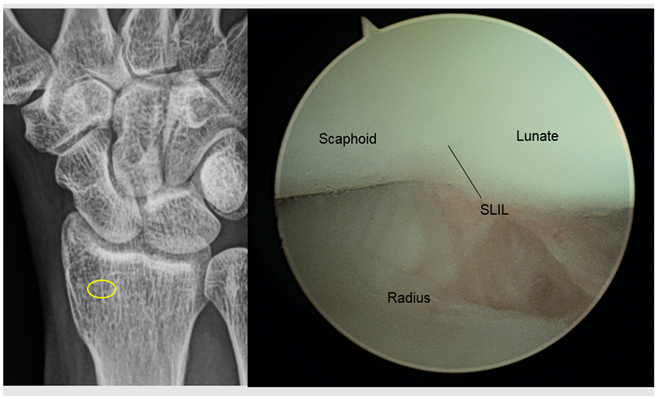
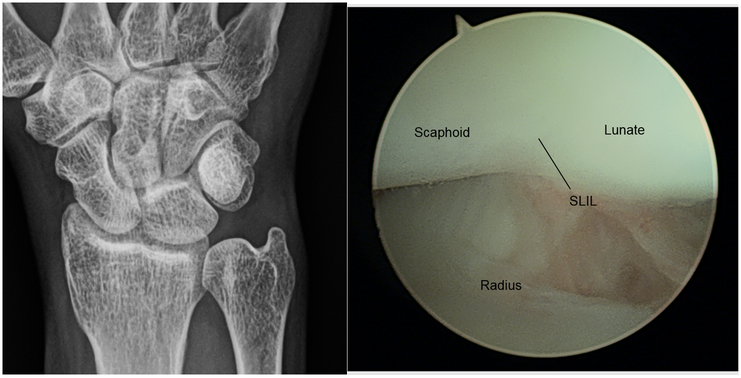
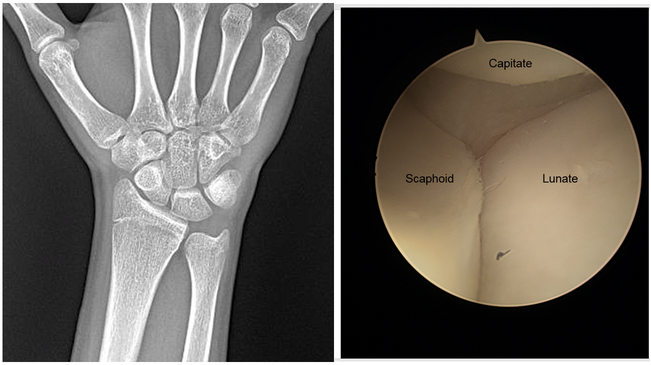
When the arthroscope is placed correctly into the 3/4 portal, the surgeon should be able to view the proximal scaphoid, scapholunate ligament, lunate, and scaphoid fossa of the distal radius. Evaluation should begin from radial to ulnar. If outflow is needed, a 6R portal can be placed via arthroscopic guidance. (Figure 6)
Figure 6.
Radiocarpal view via 3–4 portal
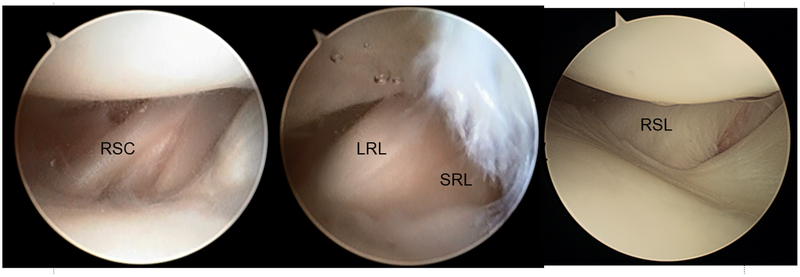
The arthroscope is directed radially along the dorsal wrist capsule to view the radial styloid, proximal scaphoid articular cartilage, and scaphoid fossa. Volar soft-tissue structures, from radial to ulnar are: radioscaphocapitate ligament (RSC), long radiolunate ligament (LRL), short radiolunate ligament (SRL), and the radioscapholunate ligament (RSL) or ligament of Testut. (Figure 7)
Care should be taken to document articular wear, synovitis, and volar capsular injury or attrition.
Figure 7.
Volar/radial extrinsic ligaments. SRL, short radiolunate ligament
The proximal membranous portion of the scapholunate (SL) ligament, and the dorsal scapholunate ligament can be visualized centrally, at the top of the arthroscopic image. Attenuation or hemorrhage represent at least a Geissler grade 1 injury. Geissler grade 2 injury represents gapping between bones of less than a 1 mm. Grade 3 injury exists where gapping exceeds 1 mm. Geissler grade 4 injury is noted when the 2.7 mm arthroscope can be passed freely between bones, suggesting complete ligamentous disruption. Geissler grade 2 – 4 SL injury can be diagnosed via the midcarpal portals.
Moving ulnarly, the proximal articular cartilage of the lunate should be evaluated for wear. The lunate fossa can be appreciated on the distal radius. Staying within the joint but angling the scope toward the dorsal, ulnar wrist, the dorsal radio-carpal ligament can be inspected for injury. Volar radial and ulnar portals can be used to evaluate the full extent of the palmar intercarpal ligaments and the dorsal capsular structures including the dorsal radiocarpal ligament. [5]
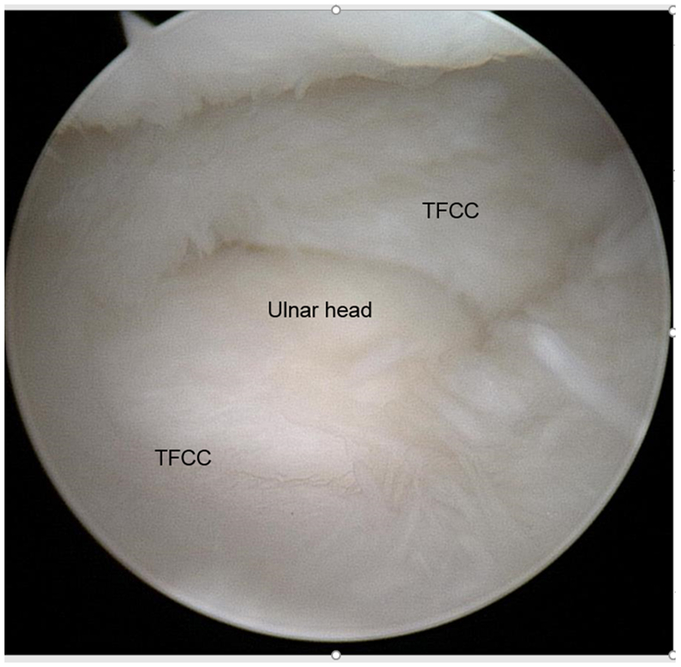
Advancing the scope ulnarly, the surgeon can appreciate the radial insertion of the triangular fibrocartilage complex (TFCC), the central disk, ulnar attachments, the palmar and dorsal radioulnar ligaments, the pisotriquteral orifice, and the prestyloid recess. (Figure 8)
Small, controlled movements will prevent inadvertent withdrawal of the scope from the joint and avoid trauma upon scope reinsertion.
Figure 8.
TFCC and prestyloid recess
Any injury to the TFCC apparent via the 3–4 portal should be further investigated. A central perforation may be seen in the setting of ulnocarpal abutment. (Figure 9) A hook probe can be used via a 6R or 6U portal examine the integrity of the TFCC. (Figure 10) [11, 12] This will cue the surgeon in to detachment of the TFCC from the radius or, more commonly, the ulnar, foveal attachments. Although a peripheral TFCC tear may be the source of ulnar-sided wrist pain, further evaluation may necessary to determine the cause of wrist instability, where present. Foveal attachments may appear to be intact by radiocarpal arthroscopy, where the deep fibers of the palmar and dorsal radiocarpal ligaments are not visualized. [13] When instability is present in the setting of intact superficial PRUL, DRUL foveal attachments, DRUJ arthroscopy or arthrography may be warranted.
Figure 9.
Central perforation of the TFCC.
Figure 10.
Normal TFCC trampoline sign
The 4–5 portal, entered similarly to the 3–4 portal, and confirmed via direct visualization, can be used to confirm the presence of lunate fossa articular wear, changes of the proximal lunate, and injury/degeneration of the TFCC. Importantly, the 4–5 portal is used to better visualize the proximal membranous and dorsal lunotriquetral interosseous ligament. Hemorrhage or attrition will cue the surgeon in to further evaluation from the midcarpal joint.
Midcarpal evaluation:
Placement of the midcarpal portals should be performed after a thorough evaluation of all structures via the radiocarpal portal. Injuries to the scapholunate or lunotriquetral ligaments can be further classified via this approach. Midcarpal instability can be assessed and may be amenable to treatment by thermal capsular skrinkage. [14]
To enter the midcarpal joint, an 18-gauge needle, directed perpendicularly to the forearm axis, is inserted 1 cm distal to the 3–4 portal. The entry site should be just distal to the scapholunate ligament and proximal to the capitate articular surface.
The needle should be gently inserted into the joint to prevent injury to the SLIL or articular cartilage.
If there is return of arthroscopy fluid upon entering the joint, this suggests disruption of the interosseous ligaments of the proximal carpal row where fluid is inappropriately communicating between the radiocarpal and midcarpal joints.
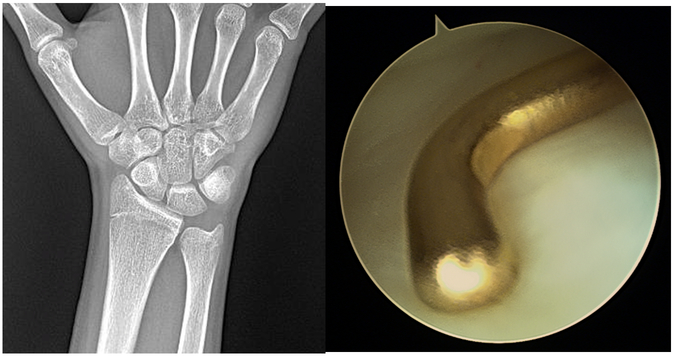
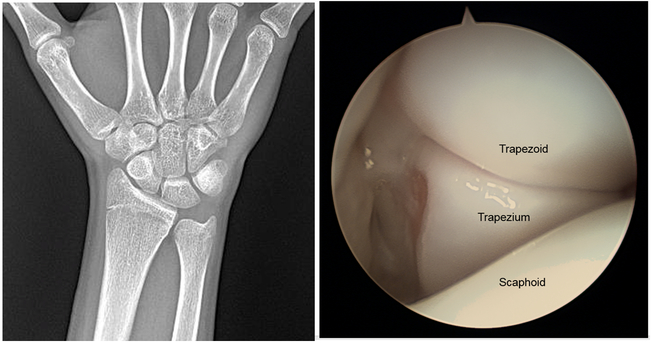
When the scope is oriented correctly, the surgeon should see the proximal capitate at the top of the image. The scaphocapitate joint and capitolunate joints can be seen radially and ulnarly. As the scope is directed radially, the surgeon can evaluate the scapho-trapezio-trapezoid joint and the distal scaphoid pole for articular changes. (Figure 11,12)
Figure 11.
Normal view of SL interval via midcarpal portal.
Figure 12.
Scaphotrapeziotrapezoid articulation
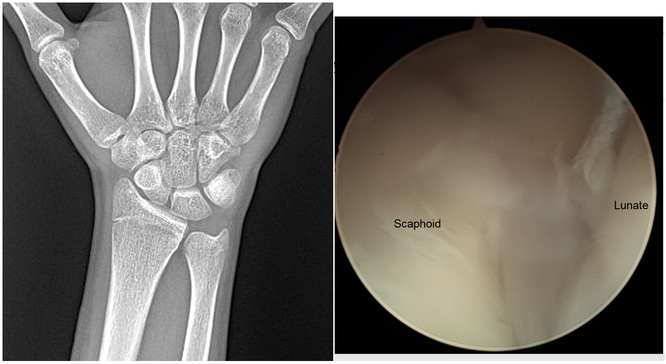
Moving centrally and proximally, the scapholunate articulation is assessed for ligamentous injury and instability. Gross instability can be estimated by one’s ability create a gap between the bones when directing the scope proximally toward the scapholunate interval. If the scope does not easily pass between the bone (>2.7mm gap, Geissler Grade IV instability) then the distance between the two bones should be estimated by using the hook probe. Gapping less than a probe width (1mm) or greater than a probe width signifies Geissler Grade II and III instability, respectively. (Figure 13)
Figure 13.
Grade IV SL instability via midcarpal portal
Volarly, the radial limb of the RSC ligament can be inspected for injury or attritional changes. Moving ulnarly, the proximal capitate, capitohamate articulation, and lunotriquetral joint can be appreciated.
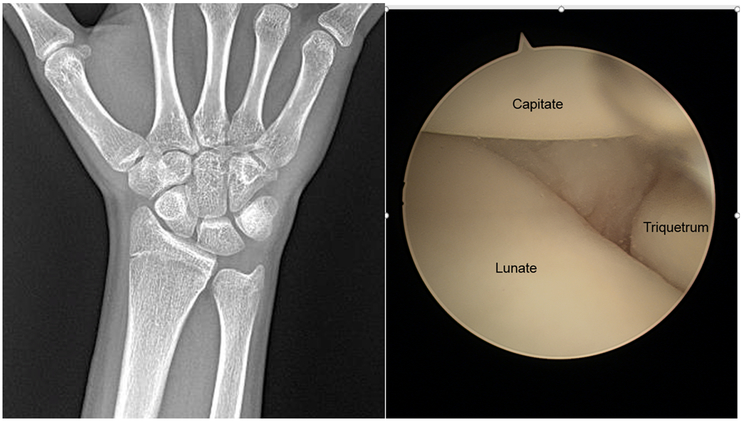
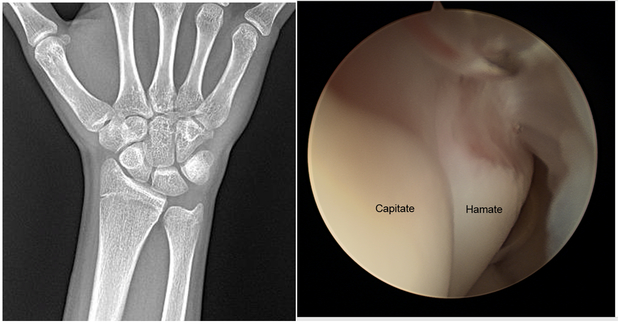
The ulnar midcarpal portal is entered in similar fashion, approximately 1 cm distal to the 4–5 portal. The articular surfaces of the distal scaphoid, lunate, and triquetrum, and proximal capitate, and hamate can again be inspected for articular wear. (Figure 14, 15) Positioned directly distal to the lunotriquetral (LT) interval, this portal can be used to estimate LT instability where distal to proximal pressure is applied via the scope while directly visualizing the joint for gapping.
Figure 14.
LT interval via midcarpal portal
Figure 15.
Capitohamate interval via midcarpal portal.
Advanced arthroscopic techniques:
Volar radial, ulnar, and midcarpal portals:
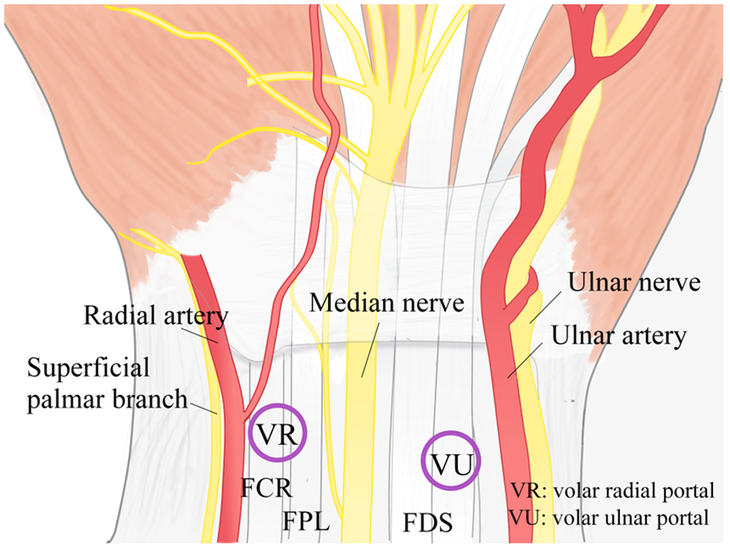
Though the use of volar portals in wrist arthroscopy had been described over a decade ago, their application has not gained widespread acceptance. [7, 15–17] Although technically unfamiliar, the volar radial and ulnar portals have a unique advantage over dorsal portals when visualizing the palmar component of interosseous ligaments, the dorsal wrist capsule, and associated extrinsic ligaments. [5–7]
The safety of the volar radial portal has been examined by Slutsky.[5] The author used a combination of anatomic studies in which lead oxide and India ink preparations highlighted critical neurovascular anatomy. Important to placement of the volar radial portal is the ability to reproducibly locate and avoid the palmar cutaneous branch of the median nerve.
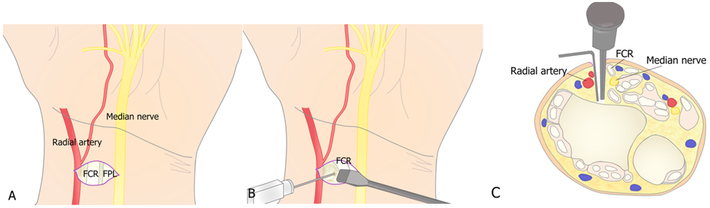
The volar radiocarpal portal is located at the level of the proximal wrist crease in the floor of the flexor carpi radialis (FCR) tendon sheath. After marking the proximal wrist crease on the skin, a 2-cm longitudinal incision over the FCR tendon is centered on the proximal wrist crease. The tendon sheath is incised and the FCR tendon is retracted ulnarly. A 22-gauge needle is directed perpendicular to the forearm axis at the intersection of the proximal wrist crease and mid-point of the FCR tendon sheath. This corresponds to the interval between the RSC and LRL. Injection of the 5 cc of saline to distend the wrist can be used to confirm entry into the radiocarpal joint.
In his anatomic studies, Slutsky identified a safe zone of at least 3 mm around the volar radial portal trocar. Care should be taken to avoid imprecise placement of the trocar, which may result in injury to the palmar cutaneous branch of the median nerve or the palmar radiocarpal arch, which lie ulnar to the FCR tendon sheath and at the distal border to the pronator quadratus, respectively. (Figure 16, 17)
Figure 16.
Relative positions of the volar radial and volar ulnar portal.
(Courtesy of N. Fujihara, MD, Nagoya, Aichi, Japan.)
Figure 17.
Technique for volar radial portal placement.
(Courtesy of N. Fujihara, MD, Nagoya, Aichi, Japan.)
The volar midcarpal portal can be identified and entered at approximately 11mm (range 7–12 mm) distal to the volar radial portal. [5] The superficial palmar branch of the radial artery is avoided after direct visualization and protection. [18] From this portal, the surgeon may visualize the capitohamate ligament, which has been shown to minimize translational motion and stabilize the transverse carpal arch, [19, 20] the palmar portion of the scapholunate ligament, and the palmar aspects of the capitate and hamate for the presence of osteochondral fractures.
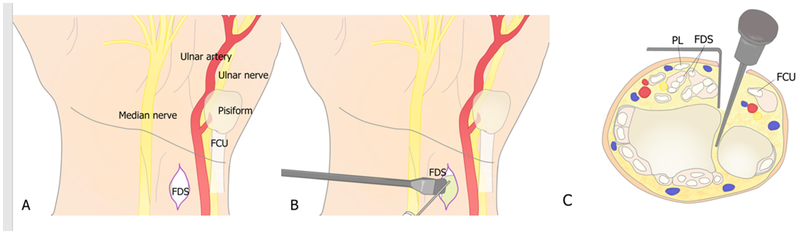
The volar ulnar portal may be used to evaluate and treat causes of ulnar-sided wrist pain, including LT ligament tears, dorsal radioulnar ligament, tears in the extensor carpi ulnaris (ECU) subsheath and ulnar collateral ligamentous complex, and TFCC injuries. This portal is entered via a 2-cm longitudinal incision, beginning at the distal wrist crease and extending proximally along the ulnar border of the flexor digitorum superficialis tendons. After retracting the tendons radially, a 22-gauge needle is used to identify the radiocarpal joint. This may be confirmed with direct arthroscopic visualization or by injection of saline into the joint. Blunt dissection of the volar capsule should precede trocar placement. If the portal is positioned correctly, the trocar should enter the volar wrist through the ulnolunate ligament. The surgeon should visualize the palmar region of the lunotriquetral (LT) ligament, distal and radial to the scope. The volar ulnar portal permits the surgeon to directly visualize the palmar and proximal portions of the LT ligament, the volar TFCC, volar and palmar surfaces of the triquetrum and lunate. (Figure 18)
Figure 18.
Technique for volar ulnar portal placement.
(Courtesy of N. Fujihara, MD, Nagoya, Aichi, Japan.)
In his anatomic study, Slutsky noted that the ulnar nerve and artery were more than 5mm from the entry point of the trocar, though the palmar cutaneous branch of the ulnar nerve (nerve of Henle) was highly variable and at risk during portal placement. [5, 6, 21, 22]
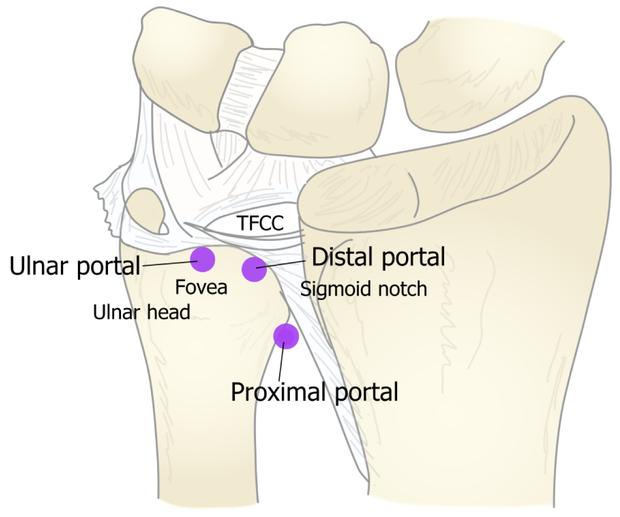
Distal radioulnar joint arthroscopy:
The integrity of the deep attachments of the TFCC establishes the stability of the DRUJ. Studies have shown that the dorsal radioulnar ligament (DRUL) confers stability both palmarly and dorsally. [23] [24, 25] Additionally, it is known that the ECU subsheath is an important stabilizer of the wrist and has been implicated as a pain generator in the patient with ulnar-sided wrist pain.
DRUJ arthroscopy permits a minimally invasive direct evaluation of the soft-tissue stabilizers of the joint, articular cartilage of the sigmoid notch and ulnar head, and the proximal surface of the TFCC.
With respect to the articular cartilage of the sigmoid notch, arthroscopy can reliably detect shear injuries that may not be appreciated on CT or MRI. [25] These injuries are known to cause pain with rotation and compression of the wrist but may be clinically indistinguishable from other pain-generating pathology.
Synovitis of the DRUJ can be caused by a variety of disorders including rheumatoid arthritis, gout, or pigmented villonodular synovitis. This can lead to swelling and pain over the ulnar head. DRUJ arthroscopy will permit direct evaluation and/or debridement of the joint without disruption of the stabilizing ligamentous complex.
Perhaps the most important indication for DRUJ arthroscopy is the evaluation of the proximal attachments of the TFCC where there is concern for wrist instability. Arthrography of the radiocarpal joint will not detect deep palmar or dorsal radioulnar ligament disruption that could be responsible for DRUJ instability. By passing the arthroscope over the ulnar head via the DRUJ, the central disk and proximal radioulnar ligaments can be directly visualized and assessed for integrity.
Three diagnostic portals and a working portal have been described for DRUJ arthroscopy. [25] The proximal DRUJ portal is the point just proximal to the sigmoid notch, along the flare of the ulnar metaphysis. With the wrist in supination, the dorsal DRUJ capsule is relaxed, facilitating entry into the joint. An 18-gauge needle, directed slightly distally, is passed into the joint. Gentle blunt dissection is performed with a mosquito, following the path created by the needle. A blunt trocar, filled with arthroscopy fluid, is introduced after enlarging the dorsal capsulotomy. (Figure 19)
Figure 19.
Relative positions of dorsal DRUJ portals
A systematic assessment of the DRUJ can be performed via the proximal DRUJ portal. One should assess the cartilage of the proximal ulnar head and sigmoid notch for the presence of articular wear, shearing injuries, or loose bodies.
Relaxing the axial directed traction may permit easier view of the DRUJ as the space widens
The wrist should be taken through a complete range of motion in pronation and supination to assess the entire joint surface
The distal DRUJ portal is located between the fifth and sixth extensor compartments, just distal to the ulnar head. A 22-gauge needle can be directed into the DRUJ between the TFCC central disk and cartilage of the ulnar head. Perfect placement is essential to avoid articular trauma upon scope placement.
Entry into the distal DRUJ portal should be performed under direct arthroscopic visualization
The arthroscope can be repositioned to the distal DRUJ portal once precise entry and position have been confirmed. This portal provides the best view of the proximal radioulnar ligamentous attachments into the base of the ulnar styloid.
A working portal, for a grasper or articular shaver, can be introduced 6 to 8 mm distal to the proximal DRUJ portal. This should be performed under direct visualization and care must be taken to avoid cartilage shearing upon instrumentation.
The volar DRUJ portal, as described by Slutsky, may also be used to directly visualize the deep fibers of the radioulnar ligaments. [3] To access the DRUJ via a volar approach, a 2-cm longitudinal incision is designed along the ulnar border of the flexor digitorum superficialis tendons, centered over the proximal wrist crease. The finger flexor tendons are retracted radially and the ulnocarpal joint in entered with a 22-gauge needle. Entry into the DRUJ via the volar capsule is performed 5 – 10 mm proximal to the ulnocarpal joint. With flow of arthroscopy fluid, the joint space expands and will permit passage of a 2.7mm arthroscope. From this portal, the surgeon can directly visualize the foveal attachments of the radioulnar ligaments.
Summary:
Diagnostic arthroscopy is a useful adjunct in the diagnosis and treatment of intra-articular wrist pathology, following careful history and physical examination. A thorough understanding of the three-dimensional anatomy of the wrist is essential to optimize efficiency and to minimize complications associated with improper instrument placement.
Volar arthroscopic portal placement should be approached with caution. Cadaver dissection and trial portal placement may be necessary to prevent or minimize complications.
KEY POINTS.
Following a careful history and physical examination, wrist arthroscopy is the reference standard for identifying and characterizing intra-articular pathology.
Wrist arthroscopy may be used to confirm the presence of articular wear, capsular and interosseous ligamentous pathology, and triangular fibrocartilage complex (TFCC) changes.
Arthroscopy is a useful adjunct when determining whether or not a patient would benefit from soft tissue repair, reconstruction, or salvage procedure.
Degenerative changes may be identified during arthroscopy that may or may not be contributing to a patient’s complaints.
Findings on wrist arthroscopy must be used in context of specific patient complaints and systematic physical exam findings to ensure that the correct treatment is selected.
Synopsis:
After reviewing this article, the reader should have a comprehensive understanding of the indications for diagnostic arthroscopy, technical considerations in performing a systematic evaluation of the wrist, and limitations of this technique.
Acknowledgements:
Supported in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (Midcareer Investigator Award in Patient-Oriented Research (2 K24-AR053120–06) (to Dr. Kevin C. Chung).
The authors would like to acknowledge Nasa Fujihara for her work on the illustrations included in this manuscript.
Footnotes
Conflicts of Interest:
The authors have no conflicts of interest
Financial Disclosure:
None
References
- 1.Rhee PC, et al. , Examination of the wrist: ulnar-sided wrist pain due to ligamentous injury. J Hand Surg Am, 2014. 39(9): p. 1859–62. [DOI] [PubMed] [Google Scholar]
- 2.Sauve PS, et al. , Examination of the wrist: radial-sided wrist pain. J Hand Surg Am, 2014. 39(10): p. 2089–92. [DOI] [PubMed] [Google Scholar]
- 3.Slutsky DJ, Distal radioulnar joint arthroscopy and the volar ulnar portal. Tech Hand Up Extrem Surg, 2007. 11(1): p. 38–44. [DOI] [PubMed] [Google Scholar]
- 4.Slutsky DJ, The incidence of dorsal radiocarpal ligament tears in patients having diagnostic wrist arthroscopy for wrist pain. J Hand Surg Am, 2008. 33(3): p. 332–4. [DOI] [PubMed] [Google Scholar]
- 5.Slutsky DJ, Clinical applications of volar portals in wrist arthroscopy. Tech Hand Up Extrem Surg, 2004. 8(4): p. 229–38. [DOI] [PubMed] [Google Scholar]
- 6.Slutsky DJ, The use of a volar ulnar portal in wrist arthroscopy. Arthroscopy, 2004. 20(2): p. 158–63. [DOI] [PubMed] [Google Scholar]
- 7.Slutsky DJ, Wrist arthroscopy through a volar radial portal. Arthroscopy, 2002. 18(6): p. 624–30. [DOI] [PubMed] [Google Scholar]
- 8.Slutsky DJ and Nagle DJ, Wrist arthroscopy: current concepts. J Hand Surg Am, 2008. 33(7): p. 1228–44. [DOI] [PubMed] [Google Scholar]
- 9.Jones CM, Grasu BL, and Murphy MS, Dry wrist arthroscopy. J Hand Surg Am, 2015. 40(2): p. 388–90. [DOI] [PubMed] [Google Scholar]
- 10.del Pinal F, et al. , Dry arthroscopy of the wrist: surgical technique. J Hand Surg Am, 2007. 32(1): p. 119–23. [DOI] [PubMed] [Google Scholar]
- 11.Ruch DS, Yang CC, and Smith BP, Results of acute arthroscopically repaired triangular fibrocartilage complex injuries associated with intra-articular distal radius fractures. Arthroscopy, 2003. 19(5): p. 511–6. [DOI] [PubMed] [Google Scholar]
- 12.Atzei A, et al. , Arthroscopic foveal repair of triangular fibrocartilage complex peripheral lesion with distal radioulnar joint instability. Tech Hand Up Extrem Surg, 2008. 12(4): p. 226–35. [DOI] [PubMed] [Google Scholar]
- 13.Slutsky DJ, Arthroscopic evaluation of the foveal attachment of the triangular fibrocartilage. Hand Clin, 2011. 27(3): p. 255–61. [DOI] [PubMed] [Google Scholar]
- 14.Mason WT and Hargreaves DG, Arthroscopic thermal capsulorrhaphy for palmar midcarpal instability. J Hand Surg Eur Vol, 2007. 32(4): p. 411–6. [DOI] [PubMed] [Google Scholar]
- 15.Levy HJ and Glickel SZ, Arthroscopic assisted internal fixation of volar intraarticular wrist fractures. Arthroscopy, 1993. 9(1): p. 122–4. [DOI] [PubMed] [Google Scholar]
- 16.Tham S, Coleman S, and Gilpin D, An anterior portal for wrist arthroscopy. Anatomical study and case reports. J Hand Surg Br, 1999. 24(4): p. 445–7. [DOI] [PubMed] [Google Scholar]
- 17.Abe Y, et al. , Arthroscopic assessment of the volar region of the scapholunate interosseous ligament through a volar portal. J Hand Surg Am, 2003. 28(1): p. 69–73. [DOI] [PubMed] [Google Scholar]
- 18.Omokawa S, et al. , Vascular and neural anatomy of the thenar area of the hand: its surgical applications. Plast Reconstr Surg, 1997. 99(1): p. 116–21. [DOI] [PubMed] [Google Scholar]
- 19.Ritt MJ, Berger RA, and Kauer JM, The gross and histologic anatomy of the ligaments of the capitohamate joint. J Hand Surg Am, 1996. 21(6): p. 1022–8. [DOI] [PubMed] [Google Scholar]
- 20.Garcia-Elias M, et al. , Stability of the transverse carpal arch: an experimental study. J Hand Surg Am, 1989. 14(2 Pt 1): p. 277–82. [DOI] [PubMed] [Google Scholar]
- 21.McCabe SJ and Kleinert JM, The nerve of Henle. J Hand Surg Am, 1990. 15(5): p. 784–8. [DOI] [PubMed] [Google Scholar]
- 22.Balogh B, et al. , The nerve of Henle: an anatomic and immunohistochemical study. J Hand Surg Am, 1999. 24(5): p. 1103–8. [DOI] [PubMed] [Google Scholar]
- 23.Haugstvedt JR, et al. , An analysis of the constraint properties of the distal radioulnar ligament attachments to the ulna. J Hand Surg Am, 2002. 27(1): p. 61–7. [DOI] [PubMed] [Google Scholar]
- 24.Taleisnik J, The ligaments of the wrist. J Hand Surg Am, 1976. 1(2): p. 110–8. [DOI] [PubMed] [Google Scholar]
- 25.Whipple TL, Arthroscopy of the distal radioulnar joint. Indications, portals, and anatomy. Hand Clin, 1994. 10(4): p. 589–92. [PubMed] [Google Scholar]