Enucleation was the standard of care for the management of uveal melanoma until the 1970s, while plaque brachytherapy was strongly emerging as a possible conservative alternative. Zimmerman, et al.'s hypothesis that “enucleation of eyes with uveal melanoma hastened metastatic death by disseminating the tumor cells” caused much concern when it was published 40 years ago.[1,2,3] The hypothesis was based on their astute observation of a peak in mortality in 2–3 years following enucleation.[1,2,3] Manschot and van Strik added to the confusion by emphasizing that radiotherapy of uveal melanoma was unjustifiable because histology frequently demonstrated viable melanoma cells in irradiated eyes.[4]
The “Zimmerman–Manschot debate” ignited a major controversy about both the available choices of treatment of uveal melanoma and the outcomes. Survival data of patients treated with plaque brachytherapy compared with historical series of patients treated with enucleation indicated that enucleation and plaque brachytherapy were equally effective.[5,6] However, due to the retrospective nature of the studies and differences in the baseline characteristics of patients included for comparison, the evidence was not readily accepted, the uncertainty remained, and the debate lingered on. Meanwhile, the tumor size came to be identified as the major prognostic factor for mortality in patients with choroidal melanoma. A meta-analysis of patients with choroidal melanoma treated by enucleation from 1966 to 1988 confirmed that tumor size correlated strongly with mortality – 16% for small tumors, 32% for medium tumors, and 53% for large tumors.[7]
A consensus gradually emerged in favor of conducting a prospective randomized clinical trial to settle the ongoing debate about the treatment of uveal melanoma. The Collaborative Ocular Melanoma Study (COMS) in its final shape consisted of two prospective randomized multicenter clinical trials designed to compare the outcome of therapies for large and medium choroidal melanomas and a third arm to assess the natural history of small choroidal melanomas.[8,9,10] Patients with large choroidal melanomas were randomized to enucleation alone or enucleation preceded by external-beam radiation (20 Gy).[8,9,10] Patients with medium choroidal melanomas were randomized to enucleation or iodine-125 plaque brachytherapy.[8,9,10] Patients with small choroidal melanomas were enrolled and observed.[8,9,10] The primary outcome measure was time to death from all-cause mortality. Secondary outcome measures included metastasis-free survival, cancer-free survival, and years of useful vision.[8,9,10]
COMS was the largest study ever to be performed in ocular oncology, initially funded by the National Eye Institute from 1985, and also by the National Cancer Institute from 1991. With 43 participating centers, more than 2000 patients, 28 numbered publications, and numerous collateral publications generated by its findings, the knowledge produced and disseminated by the COMS is immense.[8,9,10] The major derivates of COMS that have had significant impact on the management of choroidal melanoma are as follows:
The trial of enucleation alone versus pre-enucleation radiotherapy included 1003 patients with large choroidal melanoma (>10 mm in apical height and >16 mm in basal diameter) and concluded that there was no difference between the two treatment arms (the 5-year all-cause mortality was 43% and 38%; 5-year tumor-related mortality was 28% and 26%; and 10-year tumor-related mortality was 40% and 45% in the groups enucleation and enucleation with preoperative radiation, respectively), thus contradicting Zimmerman's hypothesis and reassuring that primary enucleation does not accelerate death from metastatic melanoma.[11,12]
In 1317 patients with medium-sized choroidal melanoma (2.5–10 mm in apical height and ≤16 mm in basal diameter), mortality with histopathologically confirmed melanoma metastasis after brachytherapy with iodine-125 was no worse than that following enucleation.[13] By 12 years, cumulative all-cause mortality was 43% in the brachytherapy arm and 41% in the enucleation arm.[14] The 5-, 10-, and 12-year mortality with histopathologically confirmed melanoma metastasis was 10%, 18%, and 21%, respectively, in the brachytherapy arm, and 11%, 17%, and 17%, respectively, in the enucleation arm.[13,14] These data provided reassurance that brachytherapy is at least as safe as enucleation.
COMS observational study of 204 small melanomas (1.5–2.4 mm in apical height and 5–16 mm in basal diameter) reported 2- and 5-year Kaplan–Meier estimates of tumor growth of 21% and 31%, respectively. The clinical risk factors associated with tumor growth included increased tumor thickness, presence of orange pigmentation, absence of drusen, absence of retinal pigment epithelial changes surrounding the tumor, and presence of pinpoint hyperfluorescence on fluorescent angiography. The 5-year all-cause mortality was 6% and tumor-related mortality was 1% in patients with small choroidal melanomas under observation.[15]
It is 12 years since the last official report of COMS was published. Some of the new knowledge about the biology and prognosis of uveal melanoma has raised pertinent questions about our understanding of and treatment implications based on COMS results. COMS used only the tumor size to categorize the treatment and assess the outcome. We now understand that the measures of prognosis are multifactorial. Damato et al. have developed an online neural network to generate personalized survival curves using demographic, clinical, histological, and genetic predictors (http://www.ocularmelanomaonline.com).[16] Such multifactorial analysis will possibly enhance the reliability of prognostication for metastasis in patients with uveal melanoma.
Following are some of the currently recognized prognostic factors for systemic metastasis:[17,18]
Anatomic predictors: Largest basal tumor diameter, tumor thickness, ciliary body involvement, and extraocular extension. American Joint Committee on Cancer uses all these anatomical factors to prognosticate and it may be more precise than just using the tumor dimensions.
Histopathological predictors: Epithelioid cells, closed loops vascular patterns, macrophages and lymphocytes, HLA expression, high microvascular density, high mitotic count, loss of nuclear immunostaining for BAP1, and so on.
Genetic predictors: Chromosome 3 deletion (partial or total), BAP1 loss, chromosome 8q gain, chromosome 1p loss, and chromosome 9q loss are associated with poor prognosis. Disomy 3 and chromosome 6p gain are associated with a good prognosis. Based on gene expression profiles (GEPs), uveal melanoma is now classified into three prognostic categories for metastasis – low risk (Class 1A), intermediate risk (Class 1B), or high risk (Class 2), with 2%, 21%, and 72% risk, respectively, for systemic metastasis at 5 years.[19,20,21,22]
Damato has postulated that there are three groups of uveal melanoma: (1) metastasizing melanomas, which have already metastasized by the time of ocular treatment even though the metastases may not be detectable; (2) pre-metastasizing melanomas, which develop metastatic capability and disseminate if treatment is delayed, and (3) non-metastasizing melanomas, which do not metastasize even if never treated.[18] With the currently available diagnostic techniques, it is difficult to precisely predict which melanoma might metastasize, but there may soon be a set of reliable molecular markers and their clinical surrogates to predict the same.
The current belief is that the risk for metastasis is governed by GEP and not by the treatment.[19,20,21,22] The correlation between tumor size and increased mortality is attributed to the higher prevalence of monosomy-3 in large tumors rather than to any therapeutic effect.[23,24] Genetic alteration within the tumor seems to be an ongoing evolutionary process, and the concept is supported by the demonstration of intratumoral genetic heterogeneity[25] – it is possible that melanoma may remain small and slowly growing over several years but may acquire Class 2 genetic changes over time (so-called “crescendo malignancy”) that predisposes it to grow and metastasize.[18]
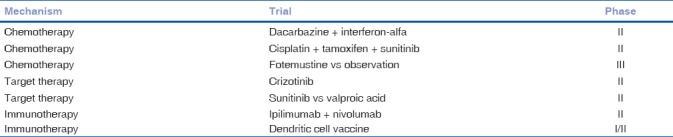
The new knowledge does not, however, imply that the ocular treatment of uveal melanoma is ineffective. Straatsma et al. compared 43 untreated patients with historical controls and reported a trend toward higher mortality in patients who were not immediately treated.[26,27] Estimates of tumor doubling time prompted the hypothesis that lethal melanomas metastasize when they are very small,[28] which supports the concept that small melanomas should be promptly treated at the point of detection, before they metastasize or acquire genetic changes that predispose to metastasis. Similarly, medium and large melanomas also deserve to be locally treated by an appropriate modality to minimize the risk of metastasis, preserve the eye, and optimize vision. Identification of patients at high risk of metastasis by multifactorial prognostication and GEP, personalized risk-based surveillance, and effective adjuvant therapy seems to be a logical approach beyond local treatment.[29] Fine needle aspiration biopsy to acquire sample for GEP in every case of conservatively treated uveal melanoma may soon become the standard of care. Patients with Class 2 risk profile need aggressive protocol-based surveillance for systemic metastasis. New knowledge has improved our ability to risk-stratify patients and identify distinct subsets for possible individualized adjuvant therapy.[29] Although several studies are in progress [Table 1], there is no agreement yet on the precise role and benefit of adjuvant therapy to minimize the risk of systemic metastasis.[29]
Table 1.
Current adjuvant therapy clinical trials in uveal melanoma[29]
COMS was indeed the burning need of the hour when it was designed and conducted, and its results have had tremendous positive impact on the standardization and accuracy of diagnosis and the clinical care of uveal melanoma. The new knowledge is, however, groundbreaking in suggesting that it is the genetic profile that governs prognosis and not just the modality of treatment. Based on the evidence available currently, it would be logical to continue to locally treat uveal melanoma optimally to conserve the eye and vision when possible, risk-stratify patients based on the established clinical profile, histopathological characteristics, and GEP, and consider patients at high risk for systemic metastasis for adjuvant therapy when its beneficial role becomes well-established.
References
- 1.Zimmerman LE, McLean IW, Foster WD. Does enucleation of the eye containing a malignant melanoma prevent or accelerate the dissemination of tumour cells. Br J Ophthalmol. 1978;62:420–5. doi: 10.1136/bjo.62.6.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zimmerman LE, McLean IW. An evaluation of enucleation in the management of uveal melanomas. Am J Ophthalmol. 1979;87:741–60. doi: 10.1016/0002-9394(79)90348-9. [DOI] [PubMed] [Google Scholar]
- 3.McLean IW, Zimmerman LE, Foster WD. Survival rates after enucleation of eyes with malignant melanoma. Am J Ophthalmol. 1979;88:794–7. [PubMed] [Google Scholar]
- 4.Manschot WA, van Strik R. Is irradiation a justifiable treatment of choroidal melanoma? Analysis of published results. Br J Ophthalmol. 1987;71:348–52. doi: 10.1136/bjo.71.5.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gass JDM. Comparison of prognosis after enucleation vs cobalt 60 irradiationof melanomas. Arch Ophthalmol. 1985;103:916–923. [PubMed] [Google Scholar]
- 6.Augsburger JJ, Gamel JW, Sardi VF, Greenberg RA, Shields JA, Brady LW. Enucleation vs cobalt plaque radiotherapy for malignant melanomas of the choroid and ciliary body. Arch Ophthalmol. 1986;104:655–61. doi: 10.1001/archopht.1986.01050170045019. [DOI] [PubMed] [Google Scholar]
- 7.Diener-West M, Hawkins BS, Markowitz JA, Schachat AP. Review of mortality from choroidal melanoma, part II, a meta-analysis of five-year mortality rates following enucleation, 1966 through 1988. Arch Ophthalmol. 1992;110:245–50. doi: 10.1001/archopht.1992.01080140101036. [DOI] [PubMed] [Google Scholar]
- 8.Margo CE. The Collaborative Ocular Melanoma Study: An overview. Cancer Control. 2004;11:304–9. doi: 10.1177/107327480401100504. [DOI] [PubMed] [Google Scholar]
- 9.Fine SL, Hawkins BS. The investigators’ perspective on the collaborative ocular melanoma study. Arch Ophthalmol. 2007;125:968–71. doi: 10.1001/archopht.125.7.968. [DOI] [PubMed] [Google Scholar]
- 10.Straatsma BR. Golden Jubilee Lecture. Randomised clinical trials of choroidal melanoma treatment. Indian J Ophthalmol. 2003;51:17–23. [PubMed] [Google Scholar]
- 11.The Collaborative Ocular Melanoma Study (COMS) randomized trial of pre-enucleation radiation of large choroidal melanoma, II: Initial mortality findings. COMS report no.10. Am J Ophthalmol. 1998;125:779–96. doi: 10.1016/s0002-9394(98)00039-7. [DOI] [PubMed] [Google Scholar]
- 12.Hawkins BS Collaborative Ocular Melanoma Study Group. The Collaborative Ocular Melanoma Study (COMS) randomized trial of pre-enucleation radiation of large choroidal melanoma: IV. Ten-year mortality findings and prognostic factors. COMS report number 24. Am J Ophthalmol. 2004;138:936–51. doi: 10.1016/j.ajo.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 13.Collaborative Ocular Melanoma Study Group: The COMS randomized trial of iodine 125 brachytherapy for choroidal melanoma. III. Initial mortality findings. COMS Report No. 18. Arch Ophthalmol. 2001;119:969–82. doi: 10.1001/archopht.119.7.969. [DOI] [PubMed] [Google Scholar]
- 14.Collaborative Ocular Melanoma Study Group. The COMS randomized trial of iodine125 brachytherapy for choroidal melanoma, V: Twelve-year mortality rates and prognostic factors. COMS Report No. 28. Arch Ophthalmol. 2006;124:1684–93. doi: 10.1001/archopht.124.12.1684. [DOI] [PubMed] [Google Scholar]
- 15.Collaborative Ocular Melanoma Study Group: Mortality in patients with small choroidal melanoma. COMS Report No.4. Arch Ophthalmol. 1997;115:886–93. [PubMed] [Google Scholar]
- 16.Damato B, Eleuteri A, Fisher AC, Coupland SE, Taktak AF. Artificial neural networks estimating survival probability after treatment of choroidal melanoma. Ophthalmology. 2008;115:1598–607. doi: 10.1016/j.ophtha.2008.01.032. [DOI] [PubMed] [Google Scholar]
- 17.Berus T, Halon A, Markiewicz A, Orlowska-Heitzman J, Romanowska-Dixon B, Donizy P. Clinical, histopathological and cytogenetic prognosticators in uveal melanoma – A comprehensive review. Anticancer Res. 2017;37:6541–9. doi: 10.21873/anticanres.12110. [DOI] [PubMed] [Google Scholar]
- 18.Damato B. Does ocular treatment of uveal melanoma influence survival? Br J Cancer. 2010;103:285–90. doi: 10.1038/sj.bjc.6605765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Onken MD, Worley LA, Ehlers JP, Harbour JW. Gene expression profiling in uveal melanoma reveals two molecular classes and predicts metastatic death. Cancer Res. 2004;64:7205–9. doi: 10.1158/0008-5472.CAN-04-1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Onken MD, Worley LA, Tuscan MD, Harbour JW. An accurate, clinically feasible multi-gene expression assay for predicting metastasis in uveal melanoma. J Mol Diagn. 2010;12:461–8. doi: 10.2353/jmoldx.2010.090220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Onken MD, Worley LA, Char DH, Augsburger JJ, Correa ZM, Nudleman E, et al. Collaborative ocular oncology group report number 1: Prospective validation of a multi-gene prognostic assay in uveal melanoma. Ophthalmology. 2012;119:1596–603. doi: 10.1016/j.ophtha.2012.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Plasseraud KM, Wilkinson JK, Oelschlager KM, Poteet TM, Cook RW, Stone JF, et al. Gene expression profiling in uveal melanoma: Technical reliability and correlation of molecular class with pathologic characteristics. Diagn Pathol. 2017;12:59–69. doi: 10.1186/s13000-017-0650-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Augsburger JJ, Correa ZM, Trichopoulos N. An alternative hypothesisfor observed mortality rates due to metastasis after treatment of choroidal melanomas of different sizes. Trans Am Ophthalmol Soc. 2007;105:54–9. [PMC free article] [PubMed] [Google Scholar]
- 24.Damato B, Coupland SE. A reappraisal of the significance of largest basal diameter of posterior uveal melanoma. Eye. 2009;23:2152–60. doi: 10.1038/eye.2009.235. [DOI] [PubMed] [Google Scholar]
- 25.Dopierala J, Damato BE, Lake SL, Taktak AF, Coupland SE. Genetic heterogeneity in uveal melanoma assessed by multiplex ligation-dependent probe amplification. Invest Ophthalmol Vis Sci. 2010;51:4898–905. doi: 10.1167/iovs.09-5004. [DOI] [PubMed] [Google Scholar]
- 26.Straatsma BR, Diener-West M, Caldwell R, Engstrom R Collaborative Ocular Melanoma Study Group. Mortality after deferral of treatment or no treatment for choroidal melanoma. Am J Ophthalmol. 2003;136:47–54. doi: 10.1016/s0002-9394(02)02270-5. [DOI] [PubMed] [Google Scholar]
- 27.Straatsma BR, Diener-West M, Caldwell R, Engstrom RE., Jr Mortality after deferral of treatment or no treatment for choroidal melanoma. Indian J Ophthalmol. 2018;66:1395–400. doi: 10.4103/ijo.IJO_1499_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eskelin S, Pyrhönen S, Summanen P, Hahka-Kemppinen M, Kivela T. Tumor doubling times in metastatic malignant melanoma of the uvea: Tumor progression before and after treatment. Ophthalmology. 2000;107:1443–9. doi: 10.1016/s0161-6420(00)00182-2. [DOI] [PubMed] [Google Scholar]
- 29.Yang J, Manson DK, Marr BP, Carvajal RD. Treatment of uveal melanoma: Where are we now? Ther Adv Med Oncol. 2018;21:10. doi: 10.1177/1758834018757175. [DOI] [PMC free article] [PubMed] [Google Scholar]


