Abstract
The classic entity of autosomal dominant Blau syndrome (BS) consists of arthritis, dermatitis, and uveitis, occurring as a result of mutations in the NOD2 gene pattern recognition receptor. Sporadic cases are those in which no known gene mutation is identifiable. Uveitis in BS can be refractory to conventional therapy. We report a case of sporadic Blau uveitis managed with adalimumab monotherapy after failing to respond to topical steroids, systemic steroids, methotrexate, and infliximab therapy sequentially. Uveitis resolved completely with adalimumab and the patient has had a disease-free period over a 2-year follow-up with bi-monthly injections for arthritis control.
Keywords: Adalimumab, Blau syndrome, uveitis
Uveitis can be associated with a myriad of systemic disorders and is often a challenging entity to manage. The management becomes even more challenging when it is refractory to conventional pharmacotherapy. We report a case of refractory uveitis in sporadic Blau syndrome (BS), treated with adalimumab monotherapy.
Case Report
A 5-year-old immunocompetent male child presented with sudden onset of pain, redness, and diminution of vision in both eyes for 1 week. He was born of a second-degree consanguineous marriage. His best-corrected visual acuity (BCVA) was 6/36, N18 in the right eye and 6/24, N12 in the left eye. Ocular examination revealed circumcorneal congestion, mutton fat keratic precipitates, grade 3 anterior chamber cells and flare. The irides in both eyes were studded with Busacca nodules and had broad posterior synechiae [Fig. 1]. Indirect ophthalmoscopy revealed grade 1 vitreous haze and optical coherence tomography revealed cystoid macular edema (CME) [Fig. 2] in both eyes. On systemic examination, he had swelling of proximal and distal interphalangeal joints in both hands [Fig. 3a]. An opinion was sought from the rheumatologist who reported it as a non-tender arthritis with no mobility restriction. The attendant gave a history of diffuse rash involving the face, trunk [Fig. 3b] and extremities when the patient was 2 years of age. A differential diagnosis of juvenile idiopathic arthritis, sarcoidosis and tuberculosis was considered and the patient was accordingly investigated. Laboratory investigations revealed elevated erythrocyte sedimentation rate and lymphocytosis. Mantoux test was negative. Chest imaging, QuantiFERON-TB Gold test, serum angiotensin converting enzyme and serum lysozyme assay were within normal limits. Rheumatoid arthritis factor, anti-nuclear antibodies and anti-neutrophilic cytoplasmic antibodies were negative. The diagnosis of BS was provisionally made and blood samples from the child and his mother were tested for known genetic mutations associated with BS, which turned out negative. It was then concluded that the patient had sporadic BS. He was started on 2-hourly prednisolone and twice-daily homatropine eye drops. However, the condition worsened with appearance of new keratic precipitates with increase in the number of Busacca nodules. Oral Prednisolone (1 mg/kg body weight) was added in addition to topicals after a week due to non-satisfactory response. At 1 month follow-up, the condition was status quo, and hence methotrexate (7.5 mg/kg weekly) was added, but this too failed to achieve a satisfactory response. After 1 month, in conjunction with rheumatologist, a decision to start the patient on intravenous injection of infliximab (5 mg/kg body weight: three injections – first injection on day 1, second injection after 2 weeks and third injection after 6 weeks) was made. Uveitis failed to respond and the patient also developed systemic hypertension after 2 months of infliximab therapy. The patient was then switched over to adalimumab monotherapy (20 mg subcutaneous injections every 2 weekly). Within a week, uveitis started responding in the form of decreasing anterior chamber inflammation and iris nodules. Within 3 months, not only uveitis [Fig. 4a] and CME but also arthritis resolved completely. The child has been kept on bi-weekly subcutaneous injections of adalimumab for control of arthritis since then. Over the past 2-year-follow up, uveitis has been in remission [Fig. 4b] with a BCVA of 6/6, N6 in both eyes.
Figure 1.
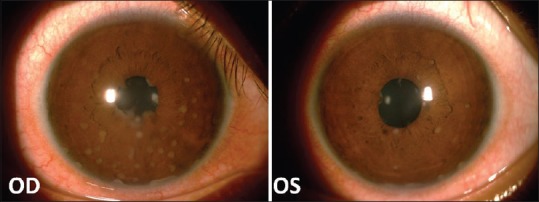
Blau uveitis at presentation. Note the Busacca nodules (more numerous in the right eye) and the posterior synechiaeuveitis
Figure 2.
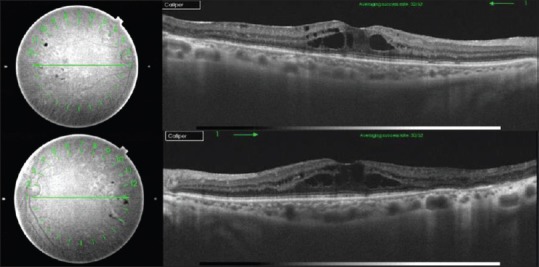
Swept-source optical coherence tomography image at presentation. Note the cystoid macular edema with the corresponding OCT fundus image in the right eye (top) and the left eye (bottom)
Figure 3.

Systemic features at presentation. (a) Arthritis involving interphalangeal joints. (b) Maculopapular dermal rash
Figure 4.
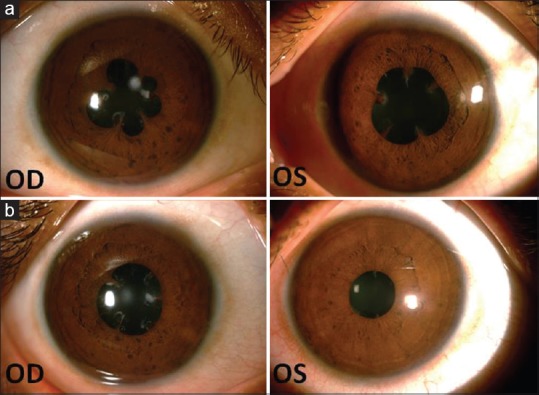
Resolution of Blau uveitis after adalimumab monotherapy: (a) after 3 months and (b) at 2-year follow-up
Discussion
First described in 1985,[1] BS is the prototype of autoimmune disease with autosomal dominant inheritance. The classic triad of BS includes uveitis, arthritis (sometimes associated with camptodactyly) and dermal rash.[2] Till date, 13 NOD2 gene mutations causing BS have been described.[3,4] Those not associated with any known gene mutations have been termed sporadic BS/early-onset sarcoidosis.[5] Uveitis in BS is in the form of progressive panuveitis with multifocal choroiditis.[5] Anterior chamber inflammation may be seen in upto 40% of patients.[6] Complications such as cataracts, glaucoma, vasculitis, macular edema with retinal detachment, optic neuritis and optic atrophy have been reported.[7] The rarity of the disease and the lack of international guidelines pose a challenge to the management of Blau uveitis. Uveitis in BS is known to be resistant to different treatments[8] and is the main cause of visual morbidity.[9] Steroids have been the mainstay for systemic management of BS, and tumor necrosis factor inhibitors have been effective in steroid non-responsive cases.[3] There have been reports of Blau uveitis being refractory to adalimumab therapy too.[8] Interleukin-1 inhibitors have been effective in such cases.[8,9] In our case, uveitis did not respond to topical steroids, systemic steroids, methotrexate, and infliximab. Adalimumab resolved uveitis and systemic features in our patient. However, there are no definite guidelines regarding the dosage, frequency and duration of treatment. It is also not clear when to switch from one agent to the other in such situations.
BS needs to be considered in young children in the first decade of life presenting with uveitis, dermatitis and arthritis. Blau uveitis can have variable severity. It can be refractive to conventional treatment strategies and this can cause considerable ocular morbidity. Biologics such as adalimumab hold promise in such refractory cases. However, lack of prospective large-scale data regarding the efficacy, duration of treatment and cost considerations are major limitations.
Conclusion
To the best of our knowledge, this is the first case of sporadic BS associated uveitis reported from the Indian population that has been successfully treated with adalimumab with a long follow-up of 2 years.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Blau EB. Familial granulomatous arthritis, iritis, and rash. J Pediatr. 1985;107:689–93. doi: 10.1016/s0022-3476(85)80394-2. [DOI] [PubMed] [Google Scholar]
- 2.Wang X, Kuivaniemi H, Bonavita G, Mutkus L, Mau U, Blau E, et al. CARD15 mutations in familial granulomatosis syndromes: A study of the original Blau syndrome kindred and other families with large-vessel arteritis and cranial neuropathy. Arthritis Rheum. 2002;46:3041–5. doi: 10.1002/art.10618. [DOI] [PubMed] [Google Scholar]
- 3.Zeybek C, Basbozkurt G, Gul D, Demirkaya E, Gok F. A new mutation in Blau syndrome. Case Rep Rheumatol 2015. 2015:463959. doi: 10.1155/2015/463959. doi: 10.1155/2015/463959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jain L, Gupta N, Reddy MM, Mittal R, Barik MR, Panigrahi B, et al. A novel mutation in helical domain 2 of NOD2 in sporadic Blau syndrome. Ocular Immunol Inflamm. 2018;26:292–4. doi: 10.1080/09273948.2016.1207789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Priori R, Bombardieri M, Spinelli F, Merlin F, Miceli-Richard C, La Cava M, et al. Sporadic Blau syndrome with a double CARD15 mutation. Report of a case with lifelong follow-up. Sarcoidosis Vasc Diffuse Lung Dis. 2004;21:228–31. [PubMed] [Google Scholar]
- 6.Sarens IL, Casteels I, Anton J, Bader-Meunier B, Brissaud P, Chédeville G, et al. Blau syndrome-associated uveitis: Preliminary results from an international prospective interventional case series. Am J Ophthalmol. 2018;187:158–66. doi: 10.1016/j.ajo.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 7.Kurokawa T, Kikuchi T, Ohta K, Imai H, Yoshimura N. Ocular manifestations in Blau syndrome associated with a CARD15/Nod2 mutation. Ophthalmology. 2003;110:2040–4. doi: 10.1016/S0161-6420(03)00717-6. [DOI] [PubMed] [Google Scholar]
- 8.Simonini G, Xu Z, Caputo R, De Libero C, Pagnini I, Pascual V, et al. Clinical and transcriptional response to the long-acting interleukin-1 blocker canakinumab in Blau syndrome-related uveitis. Arthritis Rheum. 2013;65:513–8. doi: 10.1002/art.37776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aróstegui JI, Arnal C, Merino R, Modesto C, Antonia Carballo M, Moreno P, et al. NOD2 gene-associated pediatric granulomatous arthritis: Clinical diversity, novel and recurrent mutations, and evidence of clinical improvement with interleukin-1 blockade in a Spanish cohort. Arthritis Rheum. 2007;56:3805–13. doi: 10.1002/art.22966. [DOI] [PubMed] [Google Scholar]


