Abstract
Purpose:
To assess major causes of severe visual impairment (SVI)/blindness (BL) in children studying in schools for the blind in western Uttar Pradesh, India and the extent of inappropriate enrolment of children in blind schools.
Methods:
Students of five schools for the blind were examined in a tertiary care eye hospital. The anatomical sites and etiology for SVI/BL were recorded using the World Health Organization/Prevention of Blindness standard reporting form. Categorical variable were summarized using frequencies and percentages.
Results:
A total of 93 students were examined. Male/Female ratio was 3.4:1. The most common anatomical sites of SVI/BL were the whole globe (40.3%) and the cornea (26.4%). Postnatal or childhood causes were noted in 13.8% cases. Forty-one (56.9%) students had hereditary diseases which was most likely caused by chromosomal abnormalities. Three students were having an associated disability, one was deaf and mute, one was physically handicapped, and one was intellectually challenged. Fifty-four (58%) children were blind and 21 (22.6%) children had no visual impairment but were studying in schools for the blind.
Conclusion:
Schools for the blind should be screened routinely to reduce the incidence of misdiagnosed visual impairment. This will prevent inappropriate enrolment and will definitely help in reducing the social and economic burden of society and of the schools of blind too.
Keywords: Childhood blindness, congenital anomalies, India, schools for the blind, visual impairment
Prevention of childhood blindness is a priority of the World Health Organization's Vision 2020: The Right to Sight.[1] In India, the prevalence of blindness in children under 16 years of age is estimated to be approximately 0.8/1,000.[2] It is estimated that at least 200,000 to 300,000 children in India have severe visual impairment or blindness and approximately 15,000 are in schools for the blind.[2,3] This is significant in terms of total number of disability-adjusted life years lost, social and functional challenges, and lifelong burden on the child and caregivers.[4] Many causes of severe visual impairment and blindness (SVI/BL) in children are avoidable, either preventable or treatable. There are geographical variations in the major causes of childhood blindness.[5]
According to the State Census 2011, the most populated state in India is Uttar Pradesh (UP) with a population of 199.6 million.[6] The State of UP has the highest number of disabled persons (16% of the total disabled in India).[6] Over 4 million people in UP are suffering from some kind of disability.[6] Out of them 0.7 million people are visually impaired.[6] Nearly one-third of blind people lose their eyesight before 20 years of age and many of them are less than 5 when they become blind.[7] Data on causes of visual impairment in children are limited. Screening of schools for the blind provides valuable information on causes of childhood blindness. This can help us to plan and evaluate appropriate resources towards the prevention and cure of children with visual impairment.[7,8]
Children with certain degree of visual impairment can learn to read print with appropriate training and simple visual aids. This may allow them to attend normal schools and be integrated into society, which has lifelong benefits. Yet, many visually impaired children are enrolled in schools for the blind and are taught only Braille. The purpose of this study was to assess the causes of SVI/BL among students of schools for the blind and the extent of inappropriate enrolment of visually impaired children in schools for the blind in western UP.
Methods
This cross-sectional study was carried out in five schools for the blind in western UP, India from September 2015 to December 2015. One district of western UP was identified as the study area by convenient sampling. There are five schools for the blind in the study area, all of which were included in the study. All identified schools for the blind are funded and managed by the government. The required permission for screening of the children was obtained from the principal of each school. The concerned authorities of each school were briefed about the aims and objectives of the study. The school authorities were requested to inform the parents of the children regarding the time and day of screening. UNICEF defines childhood as 0–16 years inclusive. All students under the age of 16 years at the time of the study and aged 16 years and above where onset of visual impairment was before the age of 16 years were included. Vision screening and all other ophthalmic assessment of all children were performed at a tertiary care eye hospital. All students of identified schools for the blind were brought to the tertiary eye care hospital in a phased manner for comprehensive eye examination.
A team comprising a pediatric ophthalmologist and two trained optometrists undertook the examination. Demographic details including age, gender, religion, family history, age of onset of visual loss, previous eye surgery, and medical intervention were collected for each child. The information on additional disabilities such as hearing impairment and speech impairment was also collected.
Distance visual acuity was measured by using a Snellen E chart 3 m, testing each eye separately and then with both eyes open. Children with profound visual loss were assessed for counting finger (at 3 m, 2 m, 1 m, and 0.5 m distance), hand movement, light projection, and perception of light. Near vision were assessed using figures equivalent to N.
Functional vision was determined by (1) child's ability to navigate without assistance between chairs set 2 m apart in a well-lit room; (2) child's ability to recognize someone known to them at a distance of 10 ft; (3) child's ability to recognize the shape of three 2 cm symbols at any near distance equivalent to N-60; and (4) children believed to have useful residual vision (defined as sufficient vision for at least independent mobility, for making social contacts or for near vision, if formal testing of visual acuity is not possible).[9]
Refraction and low vision aid assessment were performed in all students who were able to perform the tests of functional vision. Anterior segments examination was done using slit lamp microscope, and posterior segment examination was performed by direct and/or indirect ophthalmoscopy after dilating the pupils with tropicamide 1% eye drops when possible. B Scan ultrasonography was done if the posterior segment was not visible.
The WHO classification system was used to categorize the cause of SVI/BL using definitions in the coding instructions.[10] Accordingly, the children had no visual impairment if their best corrected visual acuity was greater or equal to 6/18 in better eye, moderate visual impairment (MVI) if their best corrected visual acuity was between <6/18 to ≥6/60 in better eye, severe visual impairment if the best corrected visual acuity was less than 6/60 but better or equal to 3/60 in better eye, and blind if their best corrected visual acuity was less than 3/60. This was irrespective of whether the child could or could not perceive the presence of light. WHO/PBL eye examination forms for children with blindness and low vision were used for data collection.[11]
Etiology of visual loss was assessed based on history and ophthalmic examination. The etiology was categorized under one of the five categories including hereditary disease, intrauterine factor, perinatal/neonatal factor, postnatal/infancy/childhood factor, and unknown.
The anatomical site of abnormality leading to visual loss was also determined. Possibility of optical corrections using spectacles or low vision aids (LVA) was assessed. The need for surgical or medical interventions were recorded and the visual prognosis was assessed. In addition to providing surgical intervention where indicated, low vision aids and spectacles were provided when required.
Statistical analysis was performed using SPSS software (Statistical Package for Social Sciences [IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp]). Significance was defined as P < 0.05. Demographics and baseline characteristics were summarized using descriptive statistics. Categorical variable were summarized using frequencies and percentages. To compare the categorical variables between groups Chi-square test was used to assess if differences exist. If the cells of contingency table had expected count of less than five, Fisher's exact test was used to assess the statistical difference.
Results
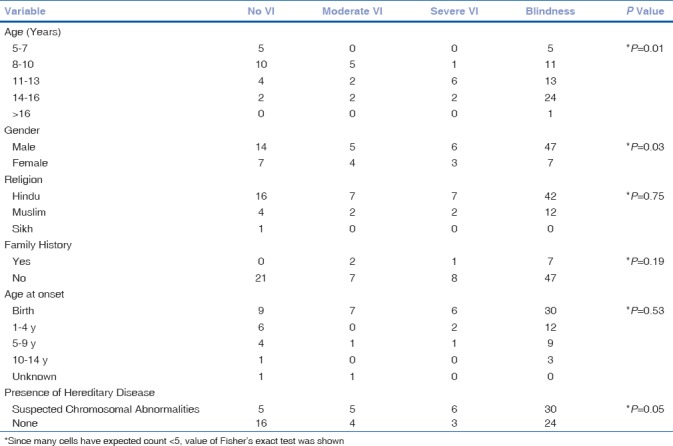
A total of 93 students were studying in the identified schools (A-E) for the blind. Total number of students studying in each school was: 30 in school A, 25 in school B, 22 in school C, 13 in school D, and 3 in school E. All students were brought to the tertiary eye care hospital for comprehensive examination. Of the 93, 10 (10.7%) students were aged between 5 and 7 years, 27 (29%) were between 8 and 10 years, 25 (26.9%) were between 11 and 13 years, 30 (32.3%) were between 14 and 16 years. One student (1.1%) was more than 16 years of age. He was included in the study as the onset of his VI was at eight years of age. Seventy-two students (77.4%) were male and 21 (22.6%) were female, with male/female ratio of 3.4:1. Seventy-two students (77.4%) were Hindu, 20 (21.5%) were Muslim, and 1 (1.1%) was Sikh.
Three students had an associated disability, one was deaf and mute, one physically handicapped, and one was intellectually challenged. Ten (10.7%) students gave history of blindness among family members and the rest 83 (89.2%) did not give history of blindness among family members.
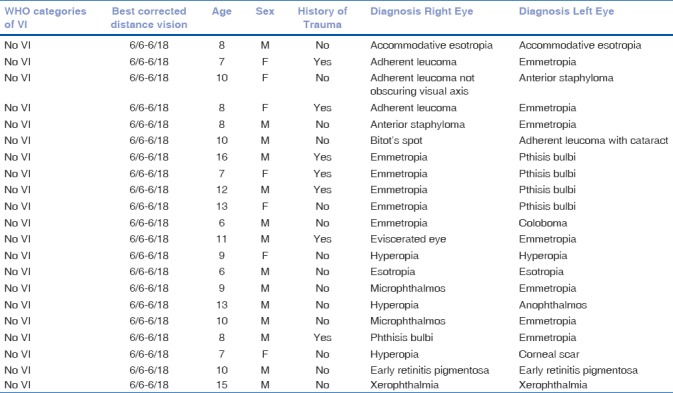
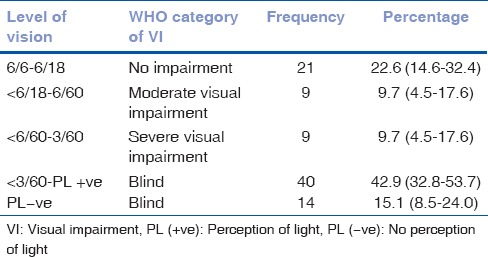
According to WHO criteria, 54 (58%) students were blind, 9 (9.7%) students had SVI, 9 (9.7%) had moderate visual impairment, and 21 (22.6%) had no visual impairment. Of all 72 students who were either BL/SVI/MVI, 51 (70.8%) had no vision, 15 (20.8%) had functional vision, and 6 (8.3%) had residual vision. Seven (33.4%) out of the 21 children diagnosed with no visual impairment had history of trauma in one eye. Characteristics of children diagnosed with no visual impairment is shown in Table 1.
Table 1.
Characteristics of children with no VI
Out of the 43 students who had visual impairment since birth, 30 (69.7%) were blind, 6 (13.9%) had SVI, and 7 (16.2%) had MVI. No statistically significant association was found between the category of visual impairment and religion (P = 0.75), family history (P = 0.18), or the age at onset of visual impairment (P = 0.53) [Table 2]. In 56% of the children, there was vision loss in both eyes.
Table 2.
Comparison between variables with type of visual impairment among blind school students
Out of the 7 students who used LVA, five used distance LVA and two used near LVA. The best corrected visual acuity of the children is shown in Table 3.
Table 3.
WHO categories of visual loss, using best corrected visual acuity (BCVA)
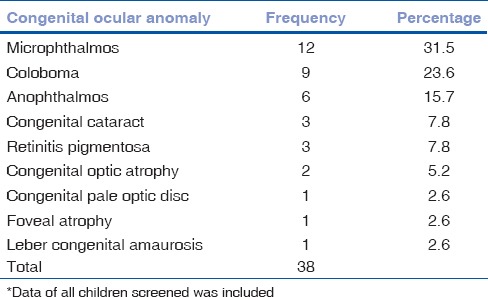
Whole globe (29, 40.3%; N = 72), cornea (19, 26.4%; N = 72), uvea (8, 11.1%; N = 72), lens (5, 6.9%; N = 72), retina (6, 8.3%; N = 72), and optic nerve (3, 4.2%; N = 72) were the anatomical site causing vision loss in BL/SVI/MVI children [Table 4]. Congenital ocular anomalies, mainly microphthalmos, coloboma, and anophthalmos, accounted for visual loss in 38 (40.86%; N = 93) children studying in schools for the blind. [Table 5]. Two children of no visual impairment category (N = 21) had microphthalmos in one eye (other eye was emmetropic in both children), one child had coloboma in one eye (other eye emmetropic), and one child had anophthalmos in one eye (other eye had hyperopia) [Table 1].
Table 4.
Anatomical site of lesion leading to BL/SVI/MVI in the 72 children
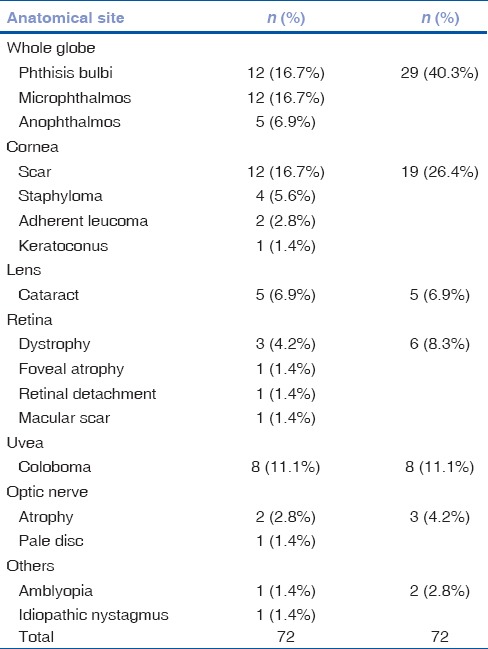
Table 5.
Frequency and percent distribution of congenital ocular anomalies in 93 children*
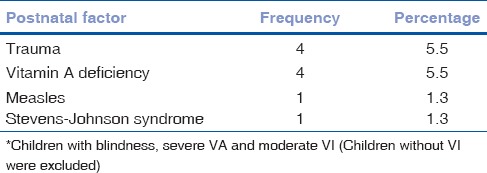
Forty-one (56.9%; N = 72) students had hereditary diseases which was most likely due to chromosomal abnormalities, postnatal causes were present in 10 (13.8%; N = 72) children, and in 21 (29.1%; N = 72) children cause of vision loss was undetermined [Table 6]. Trauma during childhood (4, 5.6%; N = 72) and vitamin A deficiency (4, 5.6%; N = 72) was the most common postnatal cause of the visual impairment [Table 7].
Table 6.
Etiological classification (n=72)*
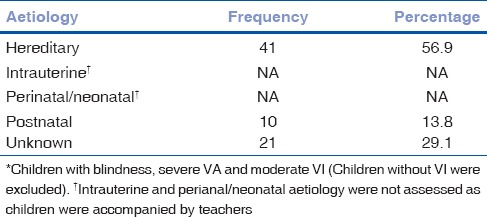
Table 7.
Frequency and percent distribution of postnatal factors in children*
Seventeen students were advised either medical or surgical interventions. Spectacles for vision correction were prescribed for twenty students. Polycarbonate spectacles were prescribed to nine students. Low vision aid was prescribed to one student.
Discussion
In this study, whole globe (40.3%) and cornea (26.4%) were the most common anatomical site of vision loss in children. Phthisis bulbi (16.7%), microphthalmos (16.7%), and corneal scar (16.7%) were the most common cause of childhood blindness. Higher rates of microphthalmos and anophthalmos have been reported in many previous studies from India conducted on visually impaired children.[11,12,13,14,15,16] In this study, hereditary factors such as chromosomal abnormalities were suspected in 56.9% of total VI/BL children. Similar findings have been reported by previous studies from India.[7,16] Kuntla et al. reported 10.3% prevalence of consanguinity in UP.[17] Consanguinity was not assessed in this study, and chromosomal abnormalities were suspected in 56.9% children on the basis of etiology in children who had visual loss or blindness at birth. The higher rate of consanguineous marriages in the study area is presumed to be a cause of higher rate of chromosomal abnormalities among children.
In the present study, avoidable causes of visual loss such as trauma, vitamin A deficiency, measles, Steven–Johnson syndrome, and harmful traditional practices accounted for 24.8% of all the children studying in schools for blind. Previous Indian studies reported avoidable causes of vision loss in children ranged from 30% to 50%.[7,13,14,15,18]
Congenital ocular anomalies such as microphthalmos, coloboma, anophthalmos, congenital cataract, retinitis pigmentosa, foveal atrophy, and leber congenital amaurosis accounted for 40.8% of all visual impairments. This finding is similar to previous studies reported by Bhalerao et al. (52.2%),[7] Gogate et al. (41.3%),[14] Krishnaiah et al. (41.4%),[19] and Bhattacharjee et al. (36.1%).[18] Congenital anomalies may be due to genetic diseases or intrauterine factors. Intrauterine factors could not be assessed in this study because all students were accompanied by their teachers. In this study, three (3.23%) children had additional deformities, which is similar to other studies by Titiyal et al. and Gogate et al.[14,15] Because children with multiple disabilities often do not get admitted into schools for the blind in India,[7] it is likely that causes of visual impairment in children with other disabilities were under-represented in this study.
This study revealed that 21 (22.6%) children who had no visual impairment has been enrolled in schools for the blind. Rahi et al. in 1995 reported that 0.9% of all children studying in schools of blind had no visual impairment.[8] Gogate et al. also reported that 6 (0.3%) out of 1795 children studying in schools for the blind had no visual impairment.[15] These percentages are much less as compared to present study. Another study with sample size similar to present study, i.e. 90 students, also had 2 (2.2%) students with no visual impairment.[7] One reason could be the definition used for determination of “no VI.” A child is said to have no visual impairment if the visual acuity in the better eye is better than or equal to 6/18.[12] Seven children diagnosed with no visual impairment actually had visual impairment in one eye due to trauma and had no visual impairment in the better eye. The diagnosis in the affected eyes in these children was phthisis bulbi in 4 eyes, adherent leucoma in 2 eyes, and anophthalmic socket (status post evisceration). In this study, the diagnosis of better eye in children who had no visual impairment were emmetropia (12 eyes), hyperopia (3 eyes), esotropia (2 eyes), early retinitis pigmentosa (1 eye), xeropthalmia (1 eye), adherent leucoma not obscuring visual axis (1 eye), and Bitot's spot (1 eye). These children with visual acuity of better than and equal to 6/18 in the better eye might have been enrolled in schools for the blind because of the controversy regarding inclusion of one-eyed person under the category of blindness.
This study screened and treated such children who could be rehabilitated with spectacles and those who could live a normal school life after such intervention. Present study contributed to this in terms of reducing the incidence of misdiagnosed visual impairment and inappropriate enrolment in schools for the blind. This in turn contributed to better quality of life for these children, reducing the social and economic burden of the society and definitely the burden of the schools for the blind too.
Conclusion
Each school for the blind should be screened routinely to identify and treat the avoidable causes of blindness and to reduce the incidence of misdiagnosed visual impairment/inappropriate enrolment of children in these schools. Routine screening can save many children from living in exile of such schools and will definitely help in reducing the social and economic burden of society by complementing such children with a good quality of life.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organization. Global Initiative for the Elimination of Avoidable Blindness: action plan. 2006-2011 [Google Scholar]
- 2.Deccan Herald. India accounts for 20 per cent of global blind population [Internet] New Delhi: The Printers (Mysore) Private Ltd; c2014. [cited 2016 Jan 18, last update 2012 Apr 06, Last assessed on 2017 Dec 01]. Available from: http://www.deccanherald.com/content/240119/india-accounts-20-per-cent.htm . [Google Scholar]
- 3.Switzerland: World Health Organization; ©2016; [Last accessed on 2016 Mar 18]. World Health Organization. Prevention of Blindness and Visual Impairment: Priority eye diseases [Internet] Available from: http://www.who.int/blindness/causes/priority/en/index3.htm . [Google Scholar]
- 4.Saxena R, Vashist P, Singh D, Tandon R. Preventing childhood blindness: Synergy between ophthalmology and community medicine. Indian J Community Med. 2015;40:149–51. doi: 10.4103/0970-0218.158841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gilbert C, Foster A. Childhood blindness in the context of VISION 2020: The right to sight. Bull World Health Organ. 2001;79:227–32. [PMC free article] [PubMed] [Google Scholar]
- 6.Census 2011/Disabled persons in India. A statistical profile 2016. Ministry of statistics and programme implementation. [Last assessed on 2017 Dec 01]. Available from: http://mospi.nic.in/sites/default/files/publication_reports/Disabled_persons_in_India_2016.pdf .
- 7.Bhalerao S, Tandon M, Singh S, Dwivedi S, Kumar S, Rana J. Visual impairment and blindness among the students of blind schools in Allahabad and its vicinity: A causal assessment. Indian J Ophthalmol. 2015;63:254–8. doi: 10.4103/0301-4738.156930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rahi JS, Sripathi S, Gilbert CE, Foster A. Childhood blindness in India: Causes in 1318 blind school students in nine states. Eye (Lond) 1995;9(Pt 5):545–50. doi: 10.1038/eye.1995.137. [DOI] [PubMed] [Google Scholar]
- 9.Pal N, Titiyal JS, Tandon R, Vajpayee RB, Gupta S, Murthy GV. Need for optical and low vision services for children in schools for the blind in North India. Indian J Ophthalmol. 2006;54:189. doi: 10.4103/0301-4738.27071. [DOI] [PubMed] [Google Scholar]
- 10.Geneva: WHO; 2016. [Last assessed on 2017 Dec 01]. World Health Organization (WHO). International Statistical Classification of Diseases and Related Health Problems 10th Revision. ICD-10 Version. Available from: http://apps.who.int/classifications/icd10/browse/2016/en#/H53-H54 . [Google Scholar]
- 11.Gilbert C, Foster A, Négrel AD, Thylefors B. Childhood blindness—a new form for recording causes of visual loss in children. Bull World Health Organ. 1993;71:485–9. [PMC free article] [PubMed] [Google Scholar]
- 12.Rahi JS, Gilbert CE, Foster A, Minassian D. Measuring the burden of childhood blindness. Br J Ophthalmol. 1999;83:387–8. doi: 10.1136/bjo.83.4.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hornby SJ, Adolph S, Gothwal VK, Gilbert CE, Dandona L, Foster A. Evaluation of children in six blind schools of Andhra Pradesh. Indian J Ophthalmol. 2000;48:195–200. [PubMed] [Google Scholar]
- 14.Titiyal JS, Pal N, Murthy GVS, Gupta SK, Tandon R, Vajpayee RB, et al. Causes and temporal trends of blindness and severe visual impairment in children in schools for the blind in North India. Br J Ophthalmol. 2003;87:941–5. doi: 10.1136/bjo.87.8.941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gogate P, Deshpande M, Sudrik S, Taras S, Kishore H, Gilbert C. Changing pattern of childhood blindness in Maharashtra, India. Br J Ophthalmol. 2007;91:8–12. doi: 10.1136/bjo.2006.094433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sil AK, Gilbert C. Childhood blindness in India. J Indian Med Assoc. 2001;99:557–60. [PubMed] [Google Scholar]
- 17.Kuntla S, Goli S, Sekher TV, Doshi R. Consanguineous marriages and their effects on pregnancy outcomes in India. Int J Sociol Soc Policy. 2013;33:437–52. [Google Scholar]
- 18.Bhattacharjee H, Das K, Borah RR, Guha K, Gogate P, Purukayastha S, et al. Causes of childhood blindness in the northeastern states of India. Indian J Ophthalmol. 2008;56:495–9. [PMC free article] [PubMed] [Google Scholar]
- 19.Krishnaiah S, Subba Rao B, Lakshmi Narasamma K, Amit G. A survey of severe visual impairment in children attending schools for the blind in a coastal district of Andhra Pradesh in South India. Eye (Lond) 2012;26:1065–70. doi: 10.1038/eye.2012.88. [DOI] [PMC free article] [PubMed] [Google Scholar]


