Abstract
Persistent pupillary membranes (PPMs) are a common congenital anomaly seen in 95% of neonates. Extensive PPMs, occluding the visual axis and resulting in reduced visual acuity, are relatively uncommon. We describe a case of bilateral total PPM in a 36-year-old female who presented with complaints of blurred vision in both the eyes. Dense pupillary membranes obscuring the visual axis need early surgical treatment. It is essential that the lens status remains clear along the visual axis both before and after pupilloplasty.
Keywords: Accessory iris membrane, persistent pupillary membrane, pupilloplasty, stimulus deprivation amblyopia
Persistent pupillary membrane (PPM) represents a common congenital ocular anomaly seen in 95% of neonates and 20% of adult population[1] that appears as fine iris strands along the pupil, which are remnants of anterior tunica vasculosa lentis that supplies nutrition to the lens in the first 6 months of fetal life. Rarely, it can present as a total dense membrane and we present a case-based approach to removal of the membrane in a 36-year-old female.
Case Report
This study conforms to the principles outlined in the Declaration of Helsinki and was conducted after obtaining approval from the Institutional Ethics Committee on Human Research and informed written consent from the patient.
A 36-year-old female presented to our outpatient department with complaints of blurred vision in both eyes since childhood. On ophthalmic examination, unaided visual acuity was Snellen 6/18 not improving further in both eyes. Anterior segment examination revealed clear corneas, deep, and quiet anterior chambers, and a dense membrane covering the pupillary area continuous with the collarette suggestive of PPM was seen [Figs. 1 and 2]. Lens status and fundus evaluation of both eyes was hindered by the pupillary membrane and could not be commented. B scan was within normal limits. Intraocular pressure in both eyes was 16 mm Hg. Gonioscopy did not reveal any abnormality. Systemic examination revealed no association. A clinical diagnosis of PPM was made and it was planned to excise the membrane. She has been further advised and counseled regarding the options available for the condition such as laser membranectomy and surgical removal. Furthermore, the risk of loss of pinhole effect and need of wearing glasses after any intervention to remove the membrane were explained to the patient.
Figure 1.

Dense pupillary membrane in the left eye seen preoperatively
Figure 2.

Dense pupillary membrane in the right eye seen preoperatively
Procedure
A superior clear corneal incision was made using a 2.8-mm keratome. Then a viscoelastic material (viscoat consisting of chondroitin sulfate and sodium hyaluronate) was injected into the anterior chamber and behind the iris to separate the PPM from the anterior lens capsule. After which the strands were excised at the collarette with a curved iris scissors [Figs. 3 and 4], and the tissue was sent for histopathological examination. Next, viscoelastic was removed completely by irrigation and aspiration, after which hydration of the superior corneal wound was done with sterile balanced salt solution. Histopathological examination of the excised tissue revealed typical features of normal iris tissue in the excised membranes; each specimen consisted of a thin fibrovascular membrane containing small vessels, fibrocytes, and stromal melanocytes. Postoperatively, the pupils were round and central in both eyes, and no remnants of PPM were seen [Figs. 5 and 6]. Fundus was seen clearly and the periphery was normal. There were no intraoperative and postoperative surgical complications. At 6 weeks postoperatively, uncorrected visual acuity was 6/60. Best-corrected refraction was Snellen acuity 6/9 with +5.0Ds/+1.5Dc at 140. Lens remained clear.
Figure 3.
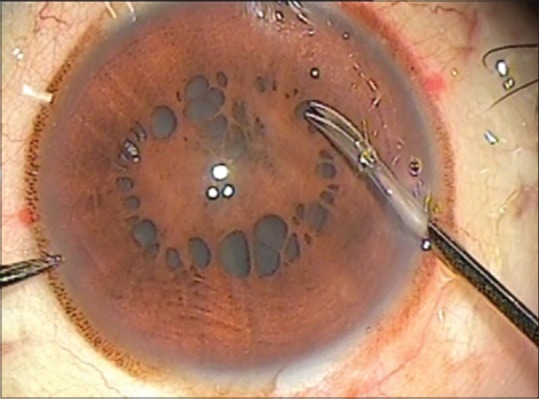
Intraoperative picture of persistent pupillary membrane after maximal pupil dilatation
Figure 4.
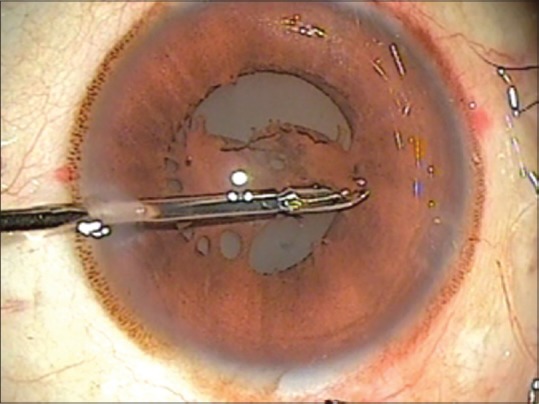
Intraoperative picture of excision of persistent pupillary membrane at the collarette
Figure 5.
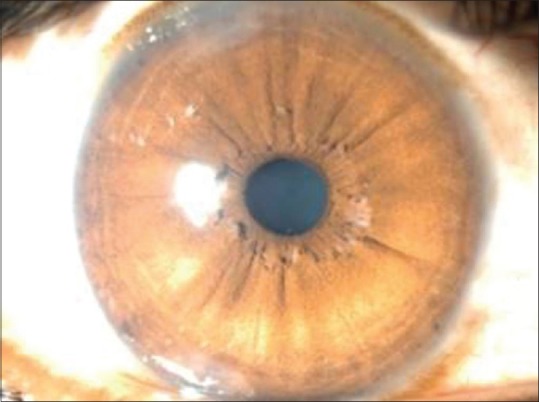
Central round pupil post pupilloplasty in the right eye
Figure 6.
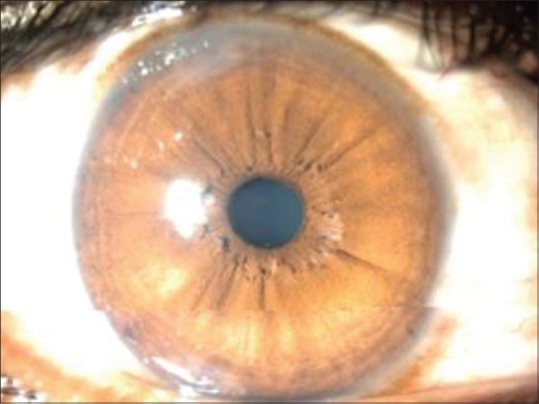
Central round pupil post pupilloplasty in the left eye
Discussion
PPM represents a common congenital ocular anomaly that appears as fine iris strands along the pupil, which are remnants of anterior tunica vasculosa lentis that supplies nutrition to the lens in the first 6 months of fetal life.[1]
PPM can be unilateral or bilateral and can be variable in appearance, size, configuration, and density. Most of the times, it can be seen as thin lacy strands of iris tissue running from the collarette, but a bilateral total persistent membrane is a rare occurrence and is associated with vision deprivation.
Embryologically, the iris forms as a solid sheet of mesodermal tissue known as the pupillary membrane.[2] It is composed of vessels derived from anterior ciliary arteries and mesenchyme ventral to the lens. On the dorsal part of the lens, the hyaloid vessels form a network around the posterior lens capsule. These posterior hyaloid vessels extend anteriorly to anastmose with the network of vessels in the pupillary membrane. This membrane surrounding the fetal lens is known as tunica vasculosa lentis.[2] The pupillary membrane itself begins to regress in the sixth month and disappears completely by the eighth month of gestation. There is some more recent evidence that intrauterine stress, particularly from chronic maternal hypertension, may accelerate the disappearance of these membranes.[3]
A failure of cellular activities that result in regression of pupillary membrane leads to PPM.[4] Conversely, a failure in the involution of the posterior hyaloid system leads to the development of a persistent hyperplasic primary vitreous.
Another entity that is often confused for PPM is accessory iris membrane (AIM) which represents a rare congenital ocular anomaly and appears as iris tissue strands arising from the iris collarette and covers the pupillary area. AIM closely resembles the normal iris tissue in color, pattern, and thickness. It also presents a virtual second pseudopupil aperture in the center with no muscular activity. PPM can be unilateral or bilateral and can be quite variable in appearance, size, configuration, and density while AIM seems to appear always bilateral. Dens AIM can be associated with PPM, amblyopia, anterior polar cataract, coloboma, strabismus, and anterior segment abnormalities.[5]
PPMs should be distinguished from congenital idiopathic microcoria which results from underdevelopment of the dilator pupillae as noted in the literature.[6] However, it can be differentiated by looking at the iris tissue connected to the collarette in case of PPM.
Most cases with PPMs are not significant enough to have visual complaints and so might go undetected. Pupillary apertures of less than 1.5 mm may obscure the light to reach the retina.[7] A small opening affects visual acuity due to the decreased retinal illumination and diffraction. In our case, despite being a thick and large membrane, the patient had good vision probably due to the staenopic effect that was induced by the tiny apertures. In one study of PPMs, 39 cases were followed up. Of these, only five were found to develop poor visual acuity. Four had unilateral deprivational amblyopia, while one case had bilateral anisometropic amblyopia.[8]
Management of persistent papillary membranes
Management of PPMs depends on the extent of the membrane, and consequently the size of the pupillary opening. Small PPMs can be managed conservatively. Mydriatics, refractive correction, and patching for amblyopia have been used successfully in some cases.[9]
Nd:YAG laser membranectomy has been shown to effectively remove the membrane. However, a number of reports have shown the presence of blood vessels, and photo disruption of these membranes can lead to hyphema; the procedure also carries the risk of cataract formation, iritis, and pigment dispersion.[10,11]
Finally, PPMs can be excised surgically. However, surgical management is fraught with risks of anesthesia, intraoperative bleeding, intraocular infection, and cataract formation. Some authors believe that there is no visual advantage to be gained by removing these membranes after the sensitive period for visual development is over although modest improvements have been reported in teenagers.[11,12]
This case illustrates that a total dense pupillary membrane can be safely and effectively removed surgically. However, residual refractive error and the loss of pin hole effect need to be explained to the patient.
To our knowledge, this is the first of its kind of presentation to be reported so far in the literature
Conclusion
Although a bilateral total dense PPM is rare, ophthalmologists may encounter a situation to decide the appropriate management of the condition whether conservative or surgical approach is apt. We believe pupilloplasty is a safe option available with no intraoperative and postoperative complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Tasman W, Jaeger E. Duane's Ophthalmology. Philadelphia: Lippincott Williams & Wilkins; 2007. pp. 24–258. [Google Scholar]
- 2.Matsuo N, Smelser GK. Electron microscopic studies on the pupillary membrane: The fine structure of the white strands of the disappearing stage of this membrane. Invest Ophthalmol. 1971;10:108–19. [PubMed] [Google Scholar]
- 3.Hadi HA, Hobbs CL. Effect of chronic intrauterine stress on the disappearance of tunica vasculosa lentis of the fetal eye: A neonatal observation. Am J Perinatol. 1990;7:23–5. doi: 10.1055/s-2007-999438. [DOI] [PubMed] [Google Scholar]
- 4.Mandal AK, Netland PA. The Pediatric Glaucomas. Maryland Heights, MO: Elsevier, Butterworth Heinemann; 2006. p. 16. [Google Scholar]
- 5.Bhatti SM, Kapoor HK. Bilateral accessory iris membrane. Indian J Ophthalmol. 1998;46:110–1. [PubMed] [Google Scholar]
- 6.Lambert SR, Amaya L, Taylor D. Congenital idiopathic microcoria. Am J Ophthalmol. 1988;106:590–4. doi: 10.1016/0002-9394(88)90592-2. [DOI] [PubMed] [Google Scholar]
- 7.Miller D, Johnson R. Quantification of the pinhole effect. Surv Ophthalmol. 1977;21:347–50. doi: 10.1016/0039-6257(77)90114-x. [DOI] [PubMed] [Google Scholar]
- 8.Lee SM, Yu YS. Outcome of hyperplastic persistent pupillary membrane. J Pediatr Ophthalmol Strabismus. 2004;41:163–71. doi: 10.3928/0191-3913-20040501-09. [DOI] [PubMed] [Google Scholar]
- 9.Miller SD, Judisch GF. Persistent pupillary membrane: Successful medical management. Arch Ophthalmol. 1979;97:1911–3. doi: 10.1001/archopht.1979.01020020359015. [DOI] [PubMed] [Google Scholar]
- 10.Kumar H, Sakhuja N, Sachdev MS. Hyperplastic pupillary membrane and laser therapy. Ophthalmic Surg. 1994;25:189–90. [PubMed] [Google Scholar]
- 11.Gupta R, Kumar S, Sonika, Sood S. Laser and surgical management of hyperplastic persistent pupillary membrane. Ophthalmic Surg Lasers Imaging. 2003;34:136–9. [PubMed] [Google Scholar]
- 12.Brusini P, Beltrame G. Spontaneous hyphaema from persistent remnant of the pupillary membrane. A case report. Acta Ophthalmol (Copenh) 1983;61:1099–103. doi: 10.1111/j.1755-3768.1983.tb01497.x. [DOI] [PubMed] [Google Scholar]


