Abstract
Cardiac amyloidosis (CA) describes the pathological process of amyloid protein deposition in the extracellular space of the myocardium. Unfortunately, the diagnosis of CA is often made late and when the disease process is advanced. However, advances in cardiovascular imaging have allowed for better prognostication and establishing diagnostic pathways with high sensitivity and specificity. This review discusses the role of echocardiography, cardiac MRI and nuclear cardiology in current clinical practice for diagnosis and prognosis of CA.
Keywords: cardiac amyloidosis, global longitudinal strain, cardiomyopathy restrictive, cardiac mri, cardio-oncology
Introduction
The term ‘amyloidosis’ describes the pathological process of amyloid deposition in the extracellular space. Amyloid proteins are normally soluble in the plasma and become insoluble after assembling in an abnormal (misfolded) beta-sheet conformation.1 Amyloid may accumulate in multiple organs and cause organ dysfunction.
There are two main types of amyloidosis1: abnormal transthyretin (ATTR) amyloidosis and2 light-chain (AL) amyloidosis, also known as primary systemic amyloidosis.2
ATTR amyloidosis occurs due to an accumulation of abnormal transthyretin protein, a carrier protein for thyroid hormones and vitamin A. Individuals who carry a mutation of the transthyretin protein (TTR) gene produce a variant of this protein, which is synthesised in the liver, and may eventually accumulate in multiple organs throughout their lifetime.3 ATTR amyloidosis is especially prevalent among those of African-American and Afro-Caribbean descent, who often possess a variant known as ‘Val122ll’ in the TTR gene. This variant accounts for nearly one quarter of African Americans with cardiac amyloidosis.4
AL amyloidosis occurs due to an accumulation of the light-chain component of immunoglobulins formed by abnormal B cells (ie, plasma cells) and is often associated with monoclonal gammopathy of undetermined significance or multiple myeloma.5
There may be an accumulation of amyloid proteins in the heart, a condition known as cardiac amyloidosis (CA). CA is a common cause of restrictive cardiomyopathy and should be considered in patients with heart failure with preserved ejection fraction.6 Symptoms may include reduced exercise capacity, fatigue, shortness of breath and oedema of the lower extremities. Cardiac amyloidosis may also affect the conduction system of the heart, leading to arrhythmias and heart blocks. QRS voltages are often diminished, although this may not be appreciable as frequently in ATTR amyloidosis compared with AL amyloidosis.7 8
The gold standard of CA diagnosis is myocardial biopsy.1 However, this procedure is invasive and may fail to detect cardiac amyloidosis if the biopsy sample is taken from a region of the myocardium unaffected by amyloidosis.1 The type of cardiac amyloidosis may be distinguished by taking a sample of the biopsy tissue and analysing it by mass spectrometry.9 The need for tissue diagnosis to characterise the type of amyloidosis is very important as ATTR and AL are treated differently. In clinical practice, most patients have tissue diagnosis from fat pad or kidney biopsies. In few selected cases, where the yield of peripheral biopsies is nil, an endomyocardial biopsy should be considered. Serum-free light-chain assay is a used as part of the work-up, treatment and prognosis of AL amyloidosis; however, its limitations and use are beyond the scope of this review.10 Echocardiography in combination with cardiovascular magnetic resonance (CMR) imaging can be used to diagnose and prognosticate CA.11 12 Additionally, technetium 99m-pyrophosphate (Tc99m-PYP) is a single-photon emission CT (SPECT) agent that is highly sensitive and specific for the diagnosis of ATTR amyloidosis.13 In this review, we discuss echocardiographic, cardiac MRI and nuclear cardiology.
Cardiovascular imaging findings in Cardiac Amyloidosis
Echocardiogram
The hallmark of CA on echocardiogram is increased left ventricular thickness. Cardiac involvement in amyloidosis often presents with >12 mm thickness of the left ventricular wall.8 Increased ventricular wall thickness, left atrial enlargement, and preserved or reduced systolic function are other findings that might be present with CA and may be correlated with clinical congestive heart failure.14 However, these findings may be present in other disorders with increased afterload, such as aortic stenosis, hypertrophic cardiomyopathy, hypertensive heart disease, renal disease and Fabry’s disease. Diastolic function may be significantly affected and tissue Doppler mitral annular velocity values are often less than 6 cm/s. Even though restrictive diastolic dysfunction is seen in advanced stages (see figure 1), there is recent literature by Knight et al that suggests that average E/e′ ratio becomes abnormal in early stages of amyloidosis.12
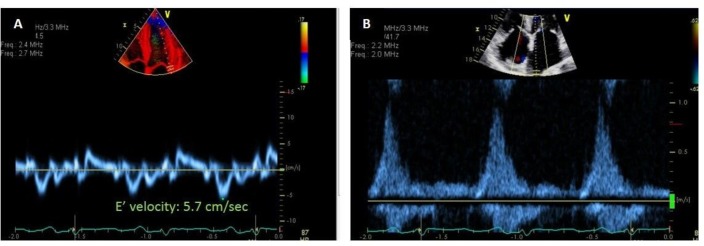
Figure 1.
Diastolic function in cardiac amyloidosis (CA): diastolic parameters tend to be markedly abnormal due to stiffening of the myocardium secondary to amyloid infiltration. Aside from the classical steep deceleration time, which is consistent with restrictive diastolic dysfunction, there are other parameters that are helpful. Tissue Doppler velocity at mitral annulus (E′) are usually <6 cm/s. Also, notice the significant blunting of the systolic component of the pulmonary vein flow, suggesting high filling pressures in the absence of significant mitral regurgitation. Typically, like any other restrictive cardiomyopathy, CA will present with biatrial enlargement, reflecting the chronically elevated filling ventricular pressures.
Another ‘classical’ echocardiographic feature of cardiac amyloidosis is the ‘speckled’ pattern (see figure 2) better characterised in fundamental imaging, which results because amyloid protein is more echogenic than the surrounding myocardial tissue.8
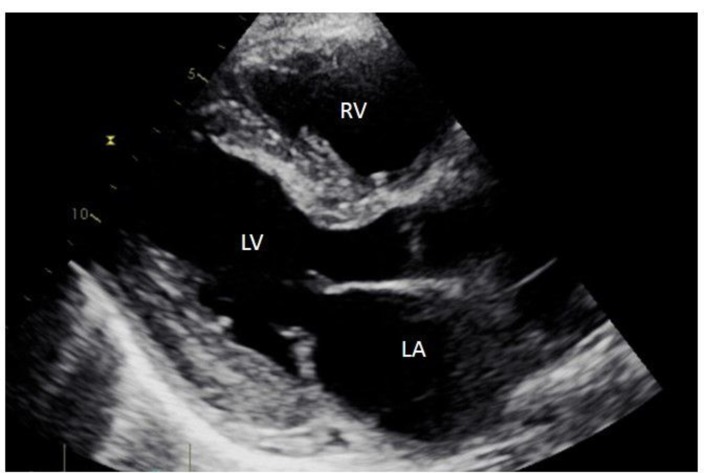
Figure 2.
Speckled pattern in transthoracic echocardiogram: with the advent of harmonic imaging, this is a feature of cardiac amyloidosis that is less reliable due to augmentation of speckles in myocardium and can be seen in harmonic imaging mode. In some echo laboratories, a frame of PLAX using fundamental imaging will be acquired on suspicion. This is a qualitative assessment and should not be used by itself to diagnose cardiac amyloidosis. LA, left atrium; LV, left ventricle; RV, right ventricle.
The global longitudinal strain (GLS) pattern that can be appreciated in CA typically spares the apex of the heart (see figure 3). This is a sensitive and specific finding that can be used to distinguish amyloidosis from other causes of left ventricular hypertrophy (LVH).15 A decrease in GLS can be identified before a decrease in left ventricular ejection fraction (LVEF) in these patients.16
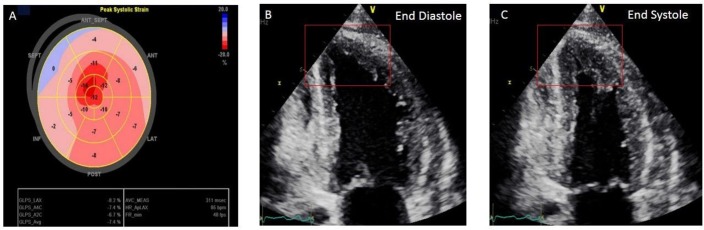
Figure 3.
Apical ‘sparing’ pattern: This is a finding that its helpful in addition to others. The left ventricle apical contractility may be preserved quite commonly in patients with advanced cardiac amyloidosis and can be depicted in a polar map of global longitudinal strain (A). There are other causes of apical ‘sparing’ such as aortic stenosis, hypertension, hypertrophic cardiomyopathy and variant of stress-induced cardiomyopathy. Notice how the basal segments do not contract as robustly as the apex (B, C).
A GLS value equal or less negative than −14.81 has been shown to be a predictor of all-cause mortality among patients with AL amyloidosis with preserved LVEF.17 Additionally, a GLS of −17 or more negative has been shown to be a strong predictor of survival in patients with AL amyloidosis undergoing autologous haematopoietic stem cell transplant.18 The ‘relative regional strain ratio’ (RRSR) has been reported to determine the extent of apical sparing of longitudinal strain in CA, and a median RRSR of greater than 1.19 was associated with increased progression to death or heart transplantation.19 Reduced deformation of the basal segments sparing the apex is not exclusive of CA and can be a less specific technique as other diseases, such as hypertrophic cardiomyopathy, aortic stenosis and hypertension, and even normal subjects can have such pattern.20 It could be the fingerprint of a mechanical response to increased afterload. However, the dissociation between LVEF preservation and GLS reduction expressed as an EF:GLS ratio is a reproducible and precise method to differentiate CA from other causes of LVH.21 Pagourelias et al showed that a value of EF:GLS ratio of more than 4.1 had 89.7% sensitivity and 91.7% of specificity to diagnose CA and distinguish it from other causes of LVH.22
GLS is an independent prognostic marker in patients with AL.16 In a Mayo Clinic study, GLS proved to be an important prognostic marker compared with clinical, echocardiographic and serological markers in patients with light-chain CA.17 Even in the patients who did not have cardiac involvement, GLS predicted all-cause mortality. Compared with the conventional diastolic parameters like E′ and E/E′, speckle tracking imaging-derived diastolic deformation, longitudinal early diastolic strain rate (LSRdias) was superior in predicting outcomes in patients with CA with preserved LVEF (>50%).23 LSRdias <0.85 s−1 alone was associated with fourfold increased mortality in these patients. A low MAPSE (mitral annular plane systolic excursion) value, which indicates the longitudinal ventricular function, is also associated with poor outcomes in patients with heart failure with preserved LVEF.24 Another parameter that is associated with worse outcomes in CA is a higher relative regional strain ratio (average apical longitudinal strain divided by the sum of the average mid and basal longitudinal strain).25
Cardiovascular magnetic resonance
Late gadolinium enhancement
In amyloidosis, the area of the extracellular space often increases due to amyloid deposition. Amyloidosis typically produces a unique pattern of subendocardial myocardial late gadolinium enhancement (LGE) in CMR. However, the area of involvement can also be patchy, diffuse or transmural.26 Transmural enhancement has been associated with a poorer prognosis than other patterns of enhancement.27
Although a very useful technique, a challenge with LGE is to choose an appropriate inversion time (TI) value. This TI value is a baseline where the myocardium is black or ‘nulled’. Incorrect determination of this null point may mask evidence of amyloidosis.27 A technique called ‘phase-sensitive inversion recovery’ allows for the automated determination of an ideal TI time and may prevent user error from incorrectly masking amyloidosis on CMR27 (see figure 4).
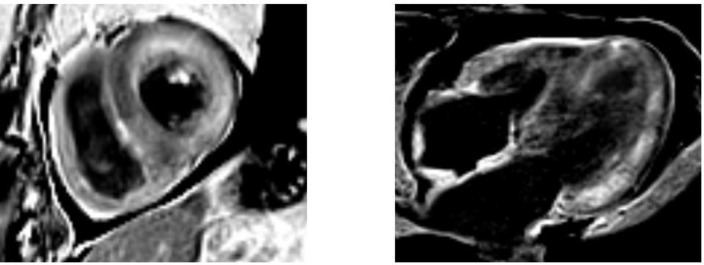
Figure 4.
Late gadolinium enhancement in amyloidosis. Because certain artefacts regarding acquisition timing may occur when acquiring late gadolinium enhancement (LGE), the preferred technique to do LGE in amyloidosis is phase-sensitive inversion recovery (PSIR). PSIR allows to characterise better the segments that have gadolinium enhancement. The characteristic pattern is ‘global endocardial’, which also has been described as having transmural and ‘patchy’ characteristics. This case illustrated above looks mostly transmural and patchy.
Lastly, the administration of a gadolinium contrast agent is contraindicated in patients with a glomerular filtration rate of less than 30 mL/min/1.73 m2 because these patients are at risk of developing nephrogenic systemic fibrosis).28 This poses an especially difficult challenge among patients with amyloidosis, many of whom may have renal dysfunction related to amyloid deposition in the kidneys in addition the myocardium.
There are two CMR techniques29 that have shown prognostic value in patients with CA:
T1 mapping
T1 mapping allows quantifying the relaxivity of the protons in the myocardium in CMR and aids further in tissue characterisation. T1 times were initially described in organs including the liver and spleen among patients with amyloidosis, and changes in T1 times have also been identified in the myocardium of patients with amyloidosis. Myocardial amyloid infiltration and fibrosis can lead to elevated non-contrast or native T1 relaxation times.30 This technique may be especially helpful in diagnosing CA among patients with significant renal involvement of amyloidosis, where gadolinium contrast is not advised.
In a study by Karamitsos et al, elevations in T1 times were appreciated among patients with AL amyloidosis with definite cardiac involvement and also among patients with AL amyloidosis with uncertain or absent cardiac involvement.30 This might suggest that T1 mapping may be more sensitive than other methods of detecting amyloidosis. Also, T1 values were significantly increased among patients with AL amyloidosis and definitive cardiac involvement compared with those with severe aortic stenosis and thickening of the ventricular wall.30 This suggests that T1 mapping may be more specific than other imaging techniques such as echocardiography, which may fail to differentiate amyloidosis from other causes of LVH.
A pre-contrast T1 time of greater than 1044 ms has been associated with a poor prognosis in AL amyloidosis.31 A similar cut-off of greater than 1077 ms has been associated with worse prognosis for ATTR amyloidosis, but not particularly prognostic when separated by familial and wild-type ATTR.32
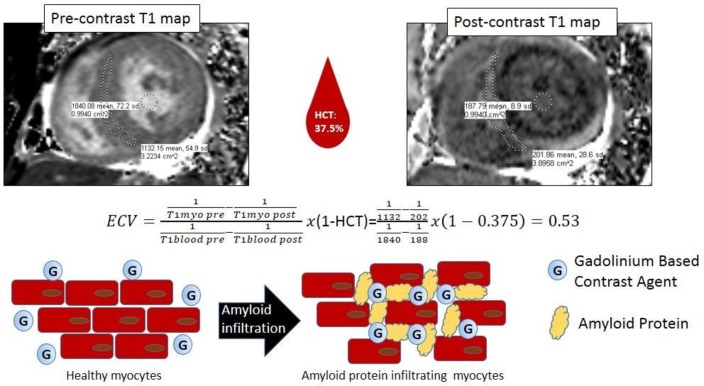
Extracellular volume fraction
T1 mapping can be used to estimate myocardial extracellular volume (ECV) fraction (see figure 5). Extracellular volume fraction can be used as a surrogate to quantify amyloid burden.33 Accurate measurement of the ECV requires a haematocrit performed at the time of the study and can be estimated using the equation: ECV=(1−haematocrit)×(ΔR1myocardium/ΔR1blood).33 In a study by Banypersad et al, extracellular volume fraction progressively increased among those with none versus probable versus definite cardiac involvement. ECV also correlated with echocardiographic parameters including left ventricular mass, septal thickness, end systolic volume and left atrial area. Furthermore, ECV has good correlation with N-terminal pro-BNP levels and troponin T levels, which are strong prognostic indicators of cardiac amyloidosis. Additionally, ECV correlated with smaller QRS voltages and poor performance with 6 min walk test.33
Figure 5.
Extracellular volume fraction in amyloidosis: T1 mapping can be used to estimate myocardial extracellular volume (ECV) fraction, a surrogate to quantify amyloid burden in extracellular space. Accurate measurement of the ECV requires a haematocrit (HCT) performed at the time of study and can be estimated using the equation above; values were taken from the region of interest–derived values, pre-contrast (native) and post-contrast T1 maps. ECV at equilibrium of greater than 0.45 has been shown to portend a poor prognosis in light-chain amyloidosis.
Perhaps most surprisingly, ECV was also found to be increased in cases where hypertrophy was not present on echocardiography, as well as where LGE did not demonstrate evidence of amyloidosis.33 This implies that ECV might be a very sensitive test, which may allow for earlier detection of CA than other methods of diagnosis. ECV at equilibrium of greater than 0.45 has been shown to portend a poor prognosis in AL amyloidosis.31
Other MRI techniques
More recently, the study by Knight et al showed that each increment in the left atrial indexed area by 1.8 cm2/m2, the decrement of indexed stroke volume by 5 mL/m2 and decrement of tricuspid annular plane systolic excursion by 3.6 mm have an independent correlation with mortality in patients with amyloidosis.12
Nuclear cardiology
Another challenge in the diagnosis of CA is differentiating AL from ATTR amyloidosis by non-invasive imaging. Tc99m-PYP SPECT imaging has been proven to be a very sensitive and specific method (about 90% both) for detecting ATTR amyloidosis,13 but not AL amyloidosis. Thus, it can be useful in distinguishing the two types of CA. Evidence of radiotracer uptake and increase in counts within myocardium can be diagnostic of ATTR CA.
Tc99m-PYP is effective in making the diagnosis of ATTR CA and can also be used to determine prognosis. A specific region within the myocardium can be compared with a contralateral area of the chest on Tc99m-PYP cardiac imaging. The ratio of the points of interest in the area of the myocardium relative to the points of interest in the contralateral area of the chest provides what is known as the ‘H:CL ratio’. An H:CL ratio equal or greater than 1.6 predicts increased mortality in ATTR amyloidosis.13 Tc99m-PYP SPECT has shown an uptake distribution of an apical sparing pattern in myocardial segments, with greater uptake in basal and mid than apical LV segments.34 This is comparable with the base to apex gradient in GLS polar map seen by echocardiography. An apical sparing ratio (ASR) of myocardial uptake, which is calculated by adding base and mid segment counts and dividing it by apical counts, has been recently shown to predict survival better than echo-derived GLS.34 An ASR of more than 2.75 is associated with a better prognosis in patients with ATTR CA.34
Tc99m-Hydroxymethylene diphosphonate (Tc99m-HMDP) SPECT as well has shown promising results of good sensitivity and specificity to differentiate between AL and ATTR CA.35 Also, Tc99m-HMDP has shown an apical sparing pattern as well in myocardial uptake distribution.36 Another SPECT tracer that can robustly differentiate TTR from AL CA is Tc99m 3,3-diphosphono-1,2-propanodicarboxylic acid (DPD). Perugini et al demonstrated that using a semiquantitative visual scoring of myocardial uptake (Perugini grading), ATTR CA can be differentiated from AL with Tc99m-DPD SPECT.37 With a well-established sensitivity and specificity, Perugini grading in Tc99m DPD did not show prognostic value in a more recent study in patients with ATTR CA.38 Recently, Tc99m-PYP was compared with Tc99m-DPD in patients with established diagnosis of ATTR CA.39 The latter was shown to have significant skeletal muscle uptake, and this could obscure cardiac uptake and cause some false-negative results.39 PET has fewer literature representation than SPECT techniques mentioned above in CA.40 Dorbala et al showed that 18F-florbetapir PET shows uptake in both ATTR and AL CA and could be used to quantify amyloid myocardial burden.40 41 In clinical practice, the use of PET is not widespread in CA and remains in the realm of research, but this continues to be an exciting and emerging field for these diseases.
Conclusion
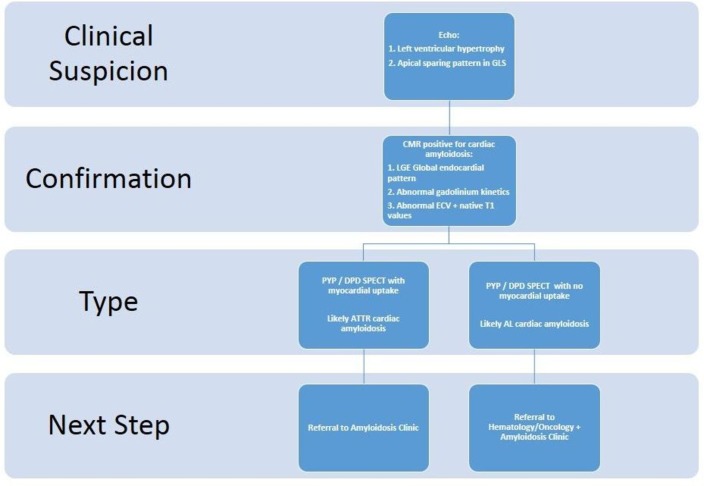
Historically, echocardiography has allowed for the possible identification of cardiac amyloidosis, but findings are relatively non-specific and may present late in the disease process. CMR has allowed for significant improvement in the diagnosis of CA. LGE has proven to be a very useful tool to make CMR an important part of the diagnostic pathway.26 However, gadolinium-based contrasts may be contraindicated in some patients with CA with renal involvement. T1 mapping and measurements of extracellular volume fraction have contributed significantly in making CMR a robust prognostic tool in CA. A non-invasive cardiac imaging algorithm using sequentially CMR and Tc99m-PYP can be suggested to differentiate AL from TTR CA and tailor work-up and clinical pathway accordingly (see figure 6). Despite advancements in cardiac imaging for the diagnosis and prognosis of CA, there is still a need for earlier detection of CA.
Figure 6.
Suggested algorithm for cardiac imaging diagnosis and stratification of cardiac amyloidosis. AL, light-chain amyloidosis; ATTR, abnormal transthyretin; CMR, cardiovascular magnetic resonance; DPD, 3,3-diphosphono-1,2-propanodicarboxylic acid; ECV, extracellular volume; GLS, global longitudinal strain; PYP, pyrophosphate; SPECT, single-photon emission CT.
Footnotes
Contributors: JL-M planned the manuscript. JL-M, AMA and PP developed the manuscript. JL-M, SH, AMA, PP, AG, CAI, PYK, JBD, NLP and GG helped draft the manuscript. JL-M submitted the manuscript and is responsible as guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1. Mollee P, Renaut P, Gottlieb D, et al. . How to diagnose amyloidosis. Intern Med J 2014;44:7–17. 10.1111/imj.12288 [DOI] [PubMed] [Google Scholar]
- 2. Guan J, Mishra S, Falk RH, et al. . Current perspectives on cardiac amyloidosis. Am J Physiol Heart Circ Physiol 2012;302:H544–H552. 10.1152/ajpheart.00815.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sekijima Y, Transthyretin SY. Transthyretin (ATTR) amyloidosis: clinical spectrum, molecular pathogenesis and disease-modifying treatments. J Neurol Neurosurg Psychiatry 2015;86:1036–43. 10.1136/jnnp-2014-308724 [DOI] [PubMed] [Google Scholar]
- 4. Jacobson DR, Alexander AA, Tagoe C, et al. . Prevalence of the amyloidogenic transthyretin (TTR) V122I allele in 14 333 African-Americans. Amyloid 2015;22:171–4. 10.3109/13506129.2015.1051219 [DOI] [PubMed] [Google Scholar]
- 5. Falk RH, Alexander KM, Liao R, et al. . AL (Light-Chain) cardiac amyloidosis: a review of diagnosis and therapy. J Am Coll Cardiol 2016;68:1323–41. 10.1016/j.jacc.2016.06.053 [DOI] [PubMed] [Google Scholar]
- 6. Gertz MA, Dispenzieri A, Sher T. Pathophysiology and treatment of cardiac amyloidosis. Nat Rev Cardiol 2015;12:91–102. 10.1038/nrcardio.2014.165 [DOI] [PubMed] [Google Scholar]
- 7. Grogan M, Dispenzieri A. Natural history and therapy of AL cardiac amyloidosis. Heart Fail Rev 2015;20:155–62. 10.1007/s10741-014-9464-5 [DOI] [PubMed] [Google Scholar]
- 8. Mohty D, Damy T, Cosnay P, et al. . Cardiac amyloidosis: updates in diagnosis and management. Arch Cardiovasc Dis 2013;106:528–40. 10.1016/j.acvd.2013.06.051 [DOI] [PubMed] [Google Scholar]
- 9. Vrana JA, Theis JD, Dasari S, et al. . Clinical diagnosis and typing of systemic amyloidosis in subcutaneous fat aspirates by mass spectrometry-based proteomics. Haematologica 2014;99:1239–47. 10.3324/haematol.2013.102764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bhole MV, Sadler R, Ramasamy K. Serum-free light-chain assay: clinical utility and limitations. Ann Clin Biochem 2014;51(Pt 5):528–42. 10.1177/0004563213518758 [DOI] [PubMed] [Google Scholar]
- 11. Cariou E, Bennani Smires Y, Victor G, et al. . Diagnostic score for the detection of cardiac amyloidosis in patients with left ventricular hypertrophy and impact on prognosis. Amyloid 2017;24:101–9. 10.1080/13506129.2017.1333956 [DOI] [PubMed] [Google Scholar]
- 12. Knight DS, Zumbo G, Barcella W, et al. . Cardiac structural and functional consequences of amyloid deposition by cardiac magnetic resonance and echocardiography and their prognostic roles. JACC Cardiovasc Imaging 2018. 10.1016/j.jcmg.2018.02.016 [DOI] [PubMed] [Google Scholar]
- 13. Castano A, Haq M, Narotsky DL, et al. . Multicenter study of planar technetium 99m pyrophosphate cardiac imaging: predicting survival for patients with ATTR cardiac amyloidosis. JAMA Cardiol 2016;1:880–9. 10.1001/jamacardio.2016.2839 [DOI] [PubMed] [Google Scholar]
- 14. Cueto-Garcia L, Reeder GS, Kyle RA, et al. . Echocardiographic findings in systemic amyloidosis: spectrum of cardiac involvement and relation to survival. J Am Coll Cardiol 1985;6:737–43. 10.1016/S0735-1097(85)80475-7 [DOI] [PubMed] [Google Scholar]
- 15. Phelan D, Collier P, Thavendiranathan P, et al. . Relative apical sparing of longitudinal strain using two-dimensional speckle-tracking echocardiography is both sensitive and specific for the diagnosis of cardiac amyloidosis. Heart 2012;98:1442–8. 10.1136/heartjnl-2012-302353 [DOI] [PubMed] [Google Scholar]
- 16. Buss SJ, Emami M, Mereles D, et al. . Longitudinal left ventricular function for prediction of survival in systemic light-chain amyloidosis: incremental value compared with clinical and biochemical markers. J Am Coll Cardiol 2012;60:1067–76. 10.1016/j.jacc.2012.04.043 [DOI] [PubMed] [Google Scholar]
- 17. Barros-Gomes S, Williams B, Nhola LF, et al. . Prognosis of light chain amyloidosis with preserved LVEF: added value of 2D speckle-tracking echocardiography to the current prognostic staging system. JACC Cardiovasc Imaging 2017;10:398–407. 10.1016/j.jcmg.2016.04.008 [DOI] [PubMed] [Google Scholar]
- 18. Pun SC, Landau HJ, Riedel ER, et al. . Prognostic and added value of two-dimensional global longitudinal strain for prediction of survival in patients with light chain amyloidosis undergoing autologous hematopoietic cell transplantation. J Am Soc Echocardiogr 2018;31:64–70. 10.1016/j.echo.2017.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Senapati A, Sperry BW, Grodin JL, et al. . Prognostic implication of relative regional strain ratio in cardiac amyloidosis. Heart 2016;102:748–54. 10.1136/heartjnl-2015-308657 [DOI] [PubMed] [Google Scholar]
- 20. Carstensen HG, Larsen LH, Hassager C, et al. . Basal longitudinal strain predicts future aortic valve replacement in asymptomatic patients with aortic stenosis. Eur Heart J Cardiovasc Imaging 2016;17:283–92. 10.1093/ehjci/jev143 [DOI] [PubMed] [Google Scholar]
- 21. Pagourelias ED, Duchenne J, Mirea O, et al. . The relation of ejection fraction and global longitudinal strain in amyloidosis: implications for differential diagnosis. JACC Cardiovasc Imaging 2016;9:1358–9. 10.1016/j.jcmg.2015.11.013 [DOI] [PubMed] [Google Scholar]
- 22. Pagourelias ED, Mirea O, Duchenne J, et al. . Echo parameters for differential diagnosis in cardiac amyloidosis: a head-to-head comparison of deformation and nondeformation parameters. Circ Cardiovasc Imaging 2017;10:e005588 10.1161/CIRCIMAGING.116.005588 [DOI] [PubMed] [Google Scholar]
- 23. Liu D, Hu K, Störk S, et al. . Predictive value of assessing diastolic strain rate on survival in cardiac amyloidosis patients with preserved ejection fraction. PLoS One 2014;9:e115910 10.1371/journal.pone.0115910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hu K, Liu D, Herrmann S, et al. . Clinical implication of mitral annular plane systolic excursion for patients with cardiovascular disease. Eur Heart J Cardiovasc Imaging 2013;14:205–12. 10.1093/ehjci/jes240 [DOI] [PubMed] [Google Scholar]
- 25. Liu D, Hu K, Niemann M, et al. . Effect of combined systolic and diastolic functional parameter assessment for differentiation of cardiac amyloidosis from other causes of concentric left ventricular hypertrophy. Circ Cardiovasc Imaging 2013;6:1066–72. 10.1161/CIRCIMAGING.113.000683 [DOI] [PubMed] [Google Scholar]
- 26. Selvanayagam JB, Hawkins PN, Paul B, et al. . Evaluation and management of the cardiac amyloidosis. J Am Coll Cardiol 2007;50:2101–10. 10.1016/j.jacc.2007.08.028 [DOI] [PubMed] [Google Scholar]
- 27. Fontana M, Pica S, Reant P, et al. . Prognostic value of late gadolinium enhancement cardiovascular magnetic resonance in cardiac amyloidosis. Circulation 2015;132:1570–9. 10.1161/CIRCULATIONAHA.115.016567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yang L, Krefting I, Gorovets A, et al. . Nephrogenic systemic fibrosis and class labeling of gadolinium-based contrast agents by the Food and Drug Administration. Radiology 2012;265:248–53. 10.1148/radiol.12112783 [DOI] [PubMed] [Google Scholar]
- 29. Patel AR, Kramer CM. Role of cardiac magnetic resonance in the diagnosis and prognosis of nonischemic cardiomyopathy. JACC Cardiovasc Imaging 2017;10(10 Pt A):1180–93. 10.1016/j.jcmg.2017.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Karamitsos TD, Piechnik SK, Banypersad SM, et al. . Noncontrast T1 mapping for the diagnosis of cardiac amyloidosis. JACC Cardiovasc Imaging 2013;6:488–97. 10.1016/j.jcmg.2012.11.013 [DOI] [PubMed] [Google Scholar]
- 31. Banypersad SM, Fontana M, Maestrini V, et al. . T1 mapping and survival in systemic light-chain amyloidosis. Eur Heart J 2015;36:244–51. 10.1093/eurheartj/ehu444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Martinez-Naharro A, Kotecha T, Norrington K, et al. . Native T1 and extracellular volume in transthyretin amyloidosis. JACC Cardiovasc Imaging 2018. 10.1016/j.jcmg.2018.02.006 [DOI] [PubMed] [Google Scholar]
- 33. Banypersad SM, Sado DM, Flett AS, et al. . Quantification of myocardial extracellular volume fraction in systemic AL amyloidosis: an equilibrium contrast cardiovascular magnetic resonance study. Circ Cardiovasc Imaging 2013;6:34–9. 10.1161/CIRCIMAGING.112.978627 [DOI] [PubMed] [Google Scholar]
- 34. Sperry BW, Vranian MN, Tower-Rader A, et al. . Regional variation in technetium pyrophosphate uptake in transthyretin cardiac amyloidosis and impact on mortality. JACC Cardiovasc Imaging 2018;11(2 Pt 1):234–42. 10.1016/j.jcmg.2017.06.020 [DOI] [PubMed] [Google Scholar]
- 35. Galat A, Van der Gucht A, Guellich A, et al. . Early phase 99Tc-HMDP scintigraphy for the dnosis and typing of cardiac amyloidosis. JACC Cardiovasc Imaging 2017;10:601–3. 10.1016/j.jcmg.2016.05.007 [DOI] [PubMed] [Google Scholar]
- 36. Van Der Gucht A, Cottereau AS, Abulizi M, et al. . Apical sparing pattern of left ventricular myocardial 99mTc-HMDP uptake in patients with transthyretin cardiac amyloidosis. J Nucl Cardiol 2017. 10.1007/s12350-017-0894-z [DOI] [PubMed] [Google Scholar]
- 37. Perugini E, Guidalotti PL, Salvi F, et al. . Noninvasive etiologic diagnosis of cardiac amyloidosis using 99mTc-3,3-diphosphono-1,2-propanodicarboxylic acid scintigraphy. J Am Coll Cardiol 2005;46:1076–84. 10.1016/j.jacc.2005.05.073 [DOI] [PubMed] [Google Scholar]
- 38. Hutt DF, Fontana M, Burniston M, et al. . Prognostic utility of the Perugini grading of 99mTc-DPD scintigraphy in transthyretin (ATTR) amyloidosis and its relationship with skeletal muscle and soft tissue amyloid. Eur Heart J Cardiovasc Imaging 2017;18:1344–50. 10.1093/ehjci/jew325 [DOI] [PubMed] [Google Scholar]
- 39. Sperry BW, Gonzalez MH, Brunken R, et al. . Non-cardiac uptake of technetium-99m pyrophosphate in transthyretin cardiac amyloidosis. J Nucl Cardiol 2018. 10.1007/s12350-017-1166-7 [DOI] [PubMed] [Google Scholar]
- 40. Bravo PE, Dorbala S. Targeted nuclear imaging probes for cardiac amyloidosis. Curr Cardiol Rep 2017;19:59 10.1007/s11886-017-0868-4 [DOI] [PubMed] [Google Scholar]
- 41. Dorbala S, Vangala D, Semer J, et al. . Imaging cardiac amyloidosis: a pilot study using ¹⁸F-florbetapir positron emission tomography. Eur J Nucl Med Mol Imaging 2014;41:1652–62. 10.1007/s00259-014-2787-6 [DOI] [PubMed] [Google Scholar]