Abstract
Background:
African Americans are generally known to have lower heavy drinking prevalence than Whites despite often greater individual and community risk factors. While it is supposed that their protective resources explain this “paradox”, studies have not explicitly examined this.
Objective:
Assess the contribution of protective resources to Black-White differences in heavy drinking, and (secondarily) whether protective resources operate by reducing heavy drinking and/or increasing abstinence.
Methods:
Using data from the 2009–10 U.S. National Alcohol Survey (N=3,133 Whites and 1,040 Blacks ages 18+), we applied Propensity Score (PS) weighting to estimate racial differences in heavy drinking and abstinence under hypothetical conditions in which Whites are similar to Blacks in: 1) age and marital status; 2) socioeconomic position and unfair treatment; 3) neighborhood socioeconomic conditions and alcohol outlet density; and 4) protective resources (proscriptive religiosity, area-level religiosity, “drier” network drinking norms and patterns, and family social support).
Results:
The Black-White gap in male and female drinkers’ baseline heavy drinking increased after weighting adjustments for demographics. In women, this gap was reduced after weighting on disadvantage and eliminated after adjusting for protective resources. In men, adjustment for disadvantage increased the racial gap, and protective resources reduced it. Protective resources had a stronger effect on Black-White differences in men’s abstinence than heavy drinking, but similar effects on these outcomes in women.
Conclusion:
Protective resources help explain Black-White differences in men’s and particularly women’s heavy drinking. Future research is needed to elucidate mechanisms of action and additional factors underlying racial differences in men’s heavy drinking.
Keywords: racial/ethnic disparities, alcohol use, heavy drinking, protective factors, African American, stress, health paradox
INTRODUCTION
U.S. national surveys generally show lower heavy drinking prevalence among African Americans compared to Whites, as well as less intense binge drinking (Centers for Disease Control and Prevention (CDC), 2013). Researchers have been perplexed by this and by African Americans’ lower lifetime rates of substance use and other psychiatric disorders, given their greater exposure to social and economic adversity and well-established links between adversity, psychological distress and heavy drinking (Jones-Webb, Karriker-Jaffe, Zemore, & Mulia, 2016; Mulia, Schmidt, Bond, Jacobs, & Korcha, 2008; Zemore, Karriker-Jaffe, Keithly, & Mulia, 2011). Such findings are considered to be an “epidemiologic paradox” (K. M. Keyes & Cerdá, 2013) in that, similar to the “Hispanic paradox” (Franzini, Ribble, & Keddie, 2002), a disadvantaged group appears to fare not only better than expected but better than the advantaged group.
A recent review suggests African Americans’ lower prevalence of heavy drinking and alcohol use disorder may be due to their more conservative drinking norms, a desire to avoid racially biased and punitive societal reactions to drinking, and (possibly) protective genetic factors affecting alcohol metabolism (Zapolski, Pedersen, McCarthy, & Smith, 2014). The broader “minority paradox” of lower lifetime psychiatric problems in African Americans compared to Whites (Breslau, Kendler, Su, Gaxiola-Aguilar, & Kessler, 2005) also has been attributed to protective sociocultural factors that help foster resilience and mitigate the stress of minority status and economic disadvantage (C. L. Keyes, 2009; Lee, Neblett, & Jackson, 2015). However, these types of social stress-based explanations that invoke stress buffers and effective coping in disadvantaged populations have been critiqued as lacking strong empirical support (Mezuk et al., 2010) due to a lack of between-group studies explicitly assessing whether protective factors account for unexpectedly better health outcomes in disadvantaged (vs. advantaged) groups (Schwartz & Meyer, 2010).
To address this gap, we conducted a between-groups study using Propensity Score (PS) methods to estimate Black-White differences in heavy drinking prevalence under hypothetical conditions in which Blacks and Whites have similar risk and protective factors. Accounting for population-level confounders such as demographic and risk exposure differences between the two groups is important when estimating the impact of protective factors, as neglecting to do so could bias the results. To our knowledge, this is the first study to employ these rigorous analytic methods to assess whether protective factors help explain racial differences in heavy drinking. Our study is informed by a social stress framework recognizing differential exposure to adversity as a key mechanism underlying health disparities (Thoits, 2010), and an assets model highlighting resources that promote health even in the context of adversity (Morgan & Ziglio, 2007).
Understanding African Americans’ lower levels of heavy drinking and other health paradoxes is important for several reasons. First, such reversals of expected health disparities may raise doubts about social determinants of health and the need to address these. Second, these reversals also raise questions about protective factors and resources of disadvantaged groups that support health but go unrecognized. Third, identification of health-enhancing individual and community factors in disadvantaged populations can stimulate research into social, psychological and biological processes through which they may bolster health. This, in turn, can advance our understanding of mechanisms shaping population health and inform the design and targeting of public health interventions.
Risk and Protective Factors for Heavy Drinking
Risk factors.
Several risk factors associated with increased heavy drinking and alcohol problems are more likely to affect African Americans than Whites. At the individual level, these include low socioeconomic position, indicated by lower education (Centers for Disease Control and Prevention (CDC), 2013) and poverty (Mossakowski, 2008), and unfair treatment and perceived discrimination (Martin, Tuch, & Roman, 2003; Zemore et al., 2011). At the community level, risk factors include neighborhood disadvantage (Karriker-Jaffe, 2011) and alcohol outlet density (R. A. Scribner, Cohen, & Fisher, 2000). Exposure to these disadvantages may increase alcohol-related risk by increasing stress and, in turn, drinking to relieve stress (e.g., unfair treatment and poverty); limiting available strategies for addressing stressors and stress (e.g., individual and neighborhood poverty); and influencing health-related knowledge and neighborhood norms that affect drinking and coping responses (e.g., low education and neighborhood alcohol outlet density).
Protective factors.
Protective resources can help sustain behavioral, psychological and physical health in the face of adversity. Churches and faith-based communities have long been recognized as powerful sources of affirmation and support in Black and low-income communities (West, 1994). African Americans evidence higher levels of religiosity than Whites, greater affiliation with religions proscribing alcohol use, and more conservative drinking norms, all of which are associated with less alcohol use (Herd & Grube, 1996; Michalak, Trocki, & Bond, 2007; Wallace, Brown, Bachman, & LaVeist, 2003). In addition, the stress-buffering and health benefits of social support are well documented (Cohen & Syme, 1985), with instrumental and emotional support particularly important in low-income and minority communities (Sarkisian & Gerstel, 2004). As with risk factors, protective resources may work directly to suppress heavy drinking, and indirectly to mitigate stress associated with heavy drinking (Elder et al., 2000; Lindenberg et al., 1999). They might also deter any drinking at all. Indeed, this might explain why abstinence rates are higher among African Americans than Whites (Dawson, Goldstein, Saha, & Grant, 2015), an important difference that must be considered when trying to understand racial differences in heavy drinking prevalence. It raises the question of whether the Black-White gap in heavy drinking is more a function of protective factors that promote abstinence, discourage heavy drinking among drinkers, or both, a question we address by analyzing prevalence of current drinking (or abstinence) and heavy drinking among drinkers. Identifying protective factors that operate on heavy drinking specifically could help inform interventions to address national goals to reduce binge drinking (U.S. Department of Health and Human Services, 2011).
Our study hypotheses are informed by theoretical and empirical work on the adverse health effects of stress, drinking to cope or regulate negative emotion, and the health benefits of protective resources (Cooper, Frone, Russell, & Mudar, 1995; Pearlin & Radabaugh, 1976). We expect that when Whites have similar exposure to risk factors as Blacks, their heavy drinking prevalence will increase and this will widen the racial gap in prevalence; when Whites have protective resources similar to Blacks, their heavy drinking prevalence will decrease, greatly reducing the racial gap. Protective factors will thus partly account for the commonly observed Black-White difference in heavy drinking prevalence. Given African Americans’ significantly higher abstinence rates, our analysis begins by examining racial differences in current drinking under the aforementioned hypothetical conditions. This enables us to assess how protective resources influence racial differences in heavy drinking; that is, by fostering abstinence, discouraging heavy drinking among current drinkers, or both.
METHODS
Data Source
This study utilized data from 1,040 Blacks and 3,133 Whites who completed the 2009–10 U.S. National Alcohol Survey (NAS), a cross-sectional, computer-assisted telephone survey of adults ages 18 and older using random digit dialing with a sampling frame of all 50 states and the District of Columbia. This study received IRB exemption approval per 45 CFR 46.101(b). Figure 1 shows the flow chart and N of subjects from recruitment through analysis.
Figure 1.
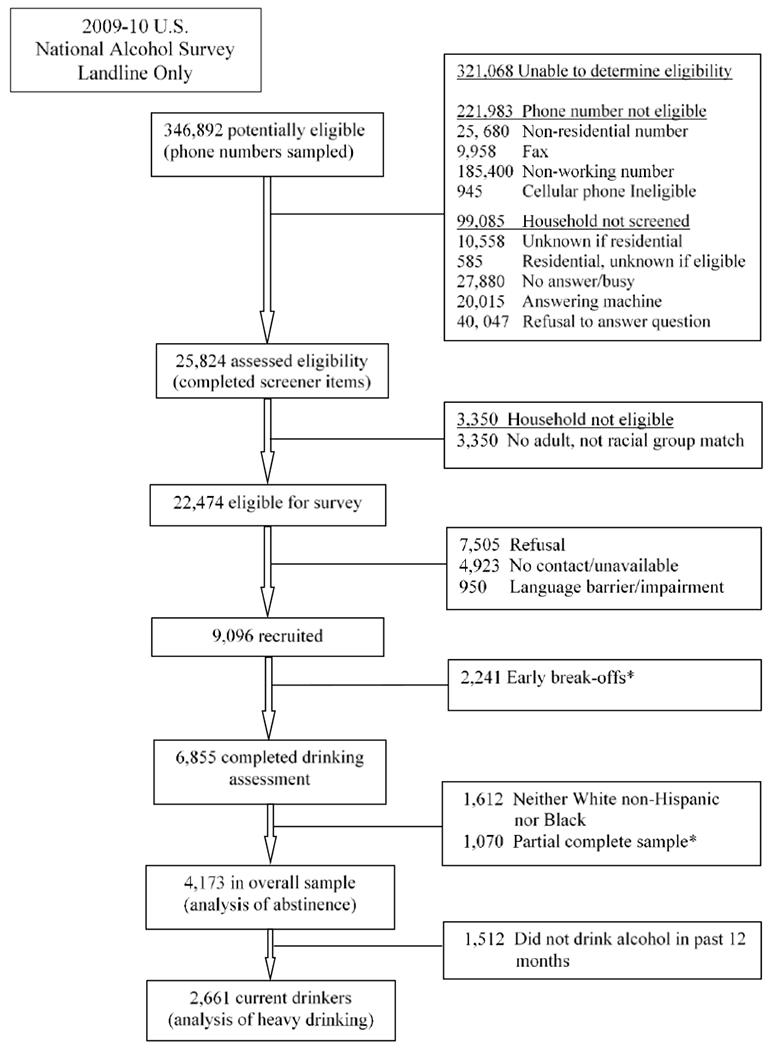
Flow Diagram of Subjects from Potential Eligibility through Inclusion in Analysis
* Insufficient data; case not retained.
The NAS sample included oversamples of Blacks and Latinos, and low-population states, and a dual-frame design that included both landline and cellular phones, providing coverage of 97.5% of the US households (Blumberg & Luke, 2009). The current study used data from landline cases only, as the abridged cell phone survey lacked items on key protective resources examined here. The cooperation rate for the landline sample was approximately 50%, which is respectable for telephone surveys (Pew Research Center, 2012). Because telephone refusals often occur as immediate hang-ups prior to receiving any description of the study, lower response rates from telephone (vs. face-to-face) surveys do not necessarily result in biased population estimates (Groves, 2006). Extensive analysis of the NAS telephone surveys with this level of response rate have shown no significant bias in alcohol estimates when compared with NAS replicate subsamples with differing response rates (e.g., (Midanik & Greenfield, 2003).
Measures
Drinking outcomes.
Current drinking was defined as having drank at least one drink in the past year. Heavy Drinking was defined as 5+ drinks in a given day for men, or 4+ drinks in a day for women, consistent with guidelines issued by the National Institute on Alcohol Abuse and Alcoholism (National Institute on Alcohol Abuse and Alcoholism, 2005). For men, heavy drinking was derived from graduated frequency (GF) questions about how often specific quantities of alcohol were consumed in a single day, starting with “12 or more drinks,” then “at least 8 but less than 12 drinks,” “5, 6 or 7 drinks”, and so forth down to one drink (Greenfield, 2000). While the GF approach is highly effective for capturing heavy drinking (Rehm et al., 1999), the GF asks for frequency of “either 3 or 4 drinks”, and thus could not be used to capture women’s heavy drinking at the 4+ threshold. Women’s heavy drinking was therefore based on the question, “How many times have you had four or more drinks of any alcoholic beverages in one day?” Of note, sensitivity analysis of men’s heavy drinking using an identical single question on 5+ drinking found the pattern of men’s results were very similar to the findings based on the widely-used GF series presented here. To capture multiple occasions of heavy drinking, we used a measure indicating heavy drinking on 7 or more days in the past year for men, and 3 or more days for women. While a monthly frequency threshold is more commonly used in alcohol studies, the monthly prevalence rate was too low for analysis of racial-gender subgroup differences.
Risk factors.
Individual-level confounders and risk factors included age, marital status, poverty (defined as a percentage of the 2008 federal poverty level based on the last year’s household income and family size), employment status, and education (Table 1 shows response categories for variables). Frequency of perceived unfair treatment was based on the question “How often do you feel that you are treated unfairly” (range 1–4, “almost never” to “often”), which is strongly associated with minority status and alcohol problems (Mulia, Ye, Zemore, & Greenfield, 2008; Zemore et al., 2011). We also assessed neighborhood-level risk factors. Neighborhood disadvantage, measured at the census tract level, takes into account proportion of residents with no high school degree, male unemployment, poverty and proportion working class. The Cronbach’s alpha was 0.80, indicating good reliability; proportions were averaged, with higher values indicating greater neighborhood disadvantage (range=0.00–0.86, M=0.322, SD=0.103). Neighborhood advantage, also assessed at the census tract level and associated with drinking beyond NIAAA recommended limits (Karriker-Jaffe, 2013), was indicated by proportion of residents with a 4-year college degree, professional jobs (e.g., management, engineering, education and legal professions), and high income (at least $75,000/year, which was 150% of the U.S. median income in 2010). The Cronbach’s alpha was high (0.92); proportions were averaged, with higher values indicating greater neighborhood advantage (range=0.00–0.87, M=.311, SD=.163). Off-premise alcohol outlet density (density of liquor stores per 1000 population) was measured at the zip code level (range: 0–10, M=0.12, SD=0.30) and has been positively associated with alcohol consumption and alcohol use disorders (Brenner, Borrell, & Barrientos-Gutierrez, 2015). Although alcohol outlet density is measured differently across studies (e.g., by population size, geographic area, or roadway miles), studies have found similar results using these different denominators (R. Scribner, Cohen, Kaplan, & Allen, 1999; R. A. Scribner, Cohen, & Farley, 1998).
Table 1.
Sample Characteristics (2009-10 U.S. National Alcohol Survey)
| Men Total | Male Current Drinkers | Women Total | Female Current Drinkers | |||||
|---|---|---|---|---|---|---|---|---|
| Black n=310 |
White n=1223 |
Black n=170 |
White n=921 |
Black n=730 |
White n=1910 |
Black n=347 |
White n=1223 |
|
| Age: 18-29 | 0.26 | 0.19 | 0.25 | 0.19 | 0.27 | 0.16** | 0.31 | 0.16** |
| 30-39 | 0.18 | 0.17 | 0.23 | 0.19 | 0.16 | 0.16 | 0.20 | 0.18 |
| 40-49 | 0.25 | 0.23 | 0.29 | 0.25 | 0.19 | 0.20 | 0.23 | 0.23 |
| 50-59 | 0.15 | 0.18 | 0.12 | 0.17 | 0.16 | 0.18 | 0.14 | 0.19 |
| 60+ | 0.16 | 0.24* | 0.11 | 0.20** | 0.22 | 0.30** | 0.12 | 0.24*** |
| Marital: married | 0.52 | 0.68** | 0.61 | 0.69 | 0.35 | 0.68*** | 0.36 | 0.72*** |
| Separated/divorce | 0.07 | 0.07 | 0.07 | 0.07 | 0.18 | 0.09*** | 0.17 | 0.08* |
| Widowed | 0.04 | 0.02 | 0.02 | 0.02 | 0.10 | 0.11 | 0.05 | 0.07 |
| Never married | 0.37 | 0.23* | 0.30 | 0.23 | 0.37 | 0.12*** | 0.42 | 0.13*** |
| Education: < HS grad | 0.23 | 0.11* | 0.20 | 0.08 | 0.17 | 0.10** | 0.06 | 0.06 |
| HS grad | 0.36 | 0.32 | 0.32 | 0.29 | 0.36 | 0.30 | 0.33 | 0.24 |
| Some college | 0.24 | 0.28 | 0.29 | 0.29 | 0.22 | 0.30** | 0.25 | 0.32 |
| College grad | 0.17 | 0.30** | 0.18 | 0.33** | 0.24 | 0.29 | 0.36 | 0.38 |
| Employment: Full time | 0.42 | 0.56* | 0.48 | 0.60 | 0.36 | 0.33 | 0.48 | 0.41 |
| Part-time | 0.10 | 0.09 | 0.14 | 0.08 | 0.09 | 0.15** | 0.07 | 0.16*** |
| Unemployed | 0.19 | 0.09* | 0.20 | 0.09 | 0.17 | 0.07*** | 0.17 | 0.06* |
| Retired | 0.13 | 0.18 | 0.09 | 0.15 | 0.15 | 0.22** | 0.05 | 0.17*** |
| Others | 0.16 | 0.09 | 0.09 | 0.08 | 0.24 | 0.23 | 0.23 | 0.20 |
| Income: < 100% Federal Poverty Level (FPL) | 0.22 | 0.07*** | 0.22 | 0.06** | 0.33 | 0.12*** | 0.23 | 0.07*** |
| 100-199% FPL | 0.24 | 0.17 | 0.26 | 0.15 | 0.18 | 0.16 | 0.20 | 0.13 |
| 200-299% FPL | 0.06 | 0.12** | 0.04 | 0.13*** | 0.11 | 0.12 | 0.16 | 0.11 |
| 300-399% FPL | 0.17 | 0.17 | 0.17 | 0.19 | 0.09 | 0.13* | 0.11 | 0.15 |
| 400% + FPL | 0.17 | 0.36*** | 0.22 | 0.39** | 0.17 | 0.31*** | 0.25 | 0.39*** |
| Missing | 0.14 | 0.10 | 0.10 | 0.08 | 0.12 | 0.17 | 0.06 | 0.15** |
| Frequency of unfair treatment (mean; range 1-4) | 2.12 | 1.81** | 2.18 | 1.80** | 2.13 | 1.76*** | 2.15 | 1.75*** |
| Mean NBH disadvantage | 0.36 | 0.29*** | 0.34 | 0.29*** | 0.35 | 0.30*** | 0.34 | 0.28*** |
| Mean NBH advantage | 0.26 | 0.33*** | 0.29 | 0.35*** | 0.28 | 0.33*** | 0.30 | 0.36** |
| Mean liquor store density (per 1000 population) | 0.11 | 0.10 | 0.11 | 0.11 | 0.11 | 0.11 | 0.11 | 0.11 |
| PROTECTIVE RESOURCES | ||||||||
| Religion very important and discourages drinking (1=yes) | 0.38 | 0.20*** | 0.29 | 0.12** | 0.43 | 0.26*** | 0.39 | 0.13*** |
| Network disapproval of drinking (mean; range 0-6) | 3.23 | 2.23*** | 2.41 | 1.58** | 3.93 | 2.73*** | 2.87 | 1.70*** |
| Network disapproval of heavy drinking (mean; range 0-3) | 2.45 | 2.06*** | 2.22 | 1.89* | 2.63 | 2.25*** | 2.47 | 1.99*** |
| Dryness of network based on “regular” drinking (mean; range 0-3) | 1.83 | 1.82 | 1.65 | 1.71 | 2.14 | 1.89*** | 1.98 | 1.65*** |
| Dryness of network based on heavy drinking (mean; range 0-3) | 2.47 | 2.58 | 2.38 | 2.56 | 2.54 | 2.56 | 2.49 | 2.53 |
| Family social support (mean; range 0-12) | 10.16 | 10.54 | 10.33 | 10.56 | 9.70 | 10.51*** | 9.65 | 10.56** |
| Mean area-level religious membership (per 1000 population) | 514.45 | 476.03** | 517.79 | 466.54*** | 520.31 | 482.81*** | 524.62 | 478.24*** |
Notes. Unweighted data,
p<.05
p<.01
p≤.001.
Protective factors.
Proscriptive religiosity was a dichotomous variable based on two items indicating the respondent’s religion is both “very important” to them and discourages alcohol use (yes/no), and has been strongly associated with support for more restrictive alcohol control policies (Mulia, Ye, et al., 2014). Area-level religiosity was a county-level variable indicating the number of members of a religious group per 1000 population based on the 2000 and 2010 Religious Congregations and Membership Study (Grammich et al., 2012), which includes more than 200 different religious bodies, and is correlated with area-level adherence to religions discouraging alcohol use (r=0.42). Social network drinking norms were assessed using three items on injunctive drinking norms (i.e., perceptions about the social approval of drinking): “How many people who are important to you would approve of you…”: 1) drinking alcohol, 2) drinking 1–2 drinks regularly, and 3) occasionally getting drunk (all/most, half, less than half, and none). These were reverse coded (range 0–3), with higher scores representing more pervasive disapproval. Social network drinking was based on two questions on the proportion of persons close to respondents who are “regular drinkers” and, separately, “heavy or problem drinkers” (all/most, half, less than half, and none), also reverse coded (range 0–3); the higher the score, the “drier” the network. Family social support was measured using four items from the family subscale of the Multidimensional Scale of Perceived Social Support (Zimet, Dahlem, Zimet, & Farley, 1988): “I get the emotional help and support I need from my family; I can talk about my problems with my family; My family really tries to help me; My family accepts me the way I am.” Responses ranged from “not at all” to “quite a lot” and were summed, with higher values indicating greater support (range 0–12). This measure has been shown to buffer the effects of severe economic hardship on alcohol problems risk (Murphy, Zemore, & Mulia, 2014).
Analysis Strategy
Propensity score (PS) weighting (Robins, Hernán, & Brumback, 2000) was used to weight the White sample to make it similar to the Black sample in distributions of demographic, risk and protective factors that are theoretically and empirically relevant to racial differences in heavy drinking. PS weighting essentially constructs a hypothetical population in which both groups have equivalent distributions of these factors, allowing us to examine whether population-level differences in protective resources account for racial differences in heavy drinking prevalence. To assess this, the White sample must first be comparable to the Black sample in all confounding factors that could affect the racial gap in heavy drinking; we therefore adjust for demographics and risk factors first. We expect that when Whites have the same demographics (younger and single) and risk factors (poorer, greater unfair treatment, disadvantaged neighborhoods) as Blacks, Whites’ heavy drinking prevalence will increase and the racial gap will widen. When we additionally weight on protective factors (e.g., religious beliefs and social networks that discourage drinking and heavy drinking), we can assess whether the racial gap is reduced or eliminated as we expect it to be. Thus applied, PS weighting enables us to answer the question: what would the Black-White difference in heavy drinking be if Whites, as a group, had the same level of protective factors as Blacks all else being equal (that is, with Whites also similar to Blacks in demographics and risk factors). The process of “equating” the two samples is achieved by “weighting up” Whites who share the same characteristics of Blacks, while “weighting down” Whites who are dissimilar from Blacks.
Multiple steps were involved in PS weighting. The first step was to define the PS by estimating the probability of being Black versus White based on logistic regression using risk and protective factors (confounding variables) as predictors. After this step, at a given PS, distributions of adjusted confounders should no longer be related to race/ethnicity (Rosenbaum & Rubin, 1983). Second, PS weights were constructed by assigning a weight of 1 to the group chosen as the reference sample (Blacks), and assigning to Whites the propensity odds [(, where is the estimated PS)]. The Black sample was the referent, given our interest in whether the racial gap in heavy drinking would decrease if Whites had the same protective factors as Blacks; the study’s much larger White sample facilitated this statistical equivalence. Lastly, the final PS weights were constructed by multiplying the PS weights from the prior step with the survey’s sampling weights. The latter were constructed to make the estimated sample representative of the US adult population accounting for the probability of selection (number of households, multiple phone lines, adult residents in households) and non-response; post-stratification weights were used to map the sample onto the US adult population proportions of race/ethnicity by region, by age, and by gender groups. To check the validity of sampling weights for a landline-only sample, comparisons were made between the landline-only sample and landline-cell combined data on main drinking variables and found their weighted means were very similar (weighted using a different set of sampling weights) (Greenfield, Ye, Karriker-Jaffe, & Kerr, 2013). Through this process, the PS-weighted distributions of confounding and protective variables in the White sample were made similar to the variable distributions in the Black sample, and thus racial/ethnic differences in risk and protective factors apparent in the unweighted sample (Table 1) were removed through PS weighting (Table 1a).
Table 1a.
Sample Characteristics after Propensity Score Weighting (2009-10 U.S. National Alcohol Survey)
| Men Total | Male Current Drinkers | Women Total | Female Current Drinkers | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Black | White | p | Black | White | p | Black | White | p | Black | White | p | |
| Age 18-29 | 0.26 | 0.27 | 0.8737 | 0.25 | 0.22 | 0.7199 | 0.27 | 0.25 | 0.7175 | 0.31 | 0.27 | 0.6614 |
| 30-39 | 0.18 | 0.16 | 0.8400 | 0.23 | 0.23 | 0.9557 | 0.16 | 0.15 | 0.7908 | 0.20 | 0.18 | 0.7185 |
| 40-49 | 0.25 | 0.24 | 0.8177 | 0.29 | 0.31 | 0.8853 | 0.19 | 0.22 | 0.5717 | 0.23 | 0.25 | 0.7683 |
| 50-59 | 0.15 | 0.16 | 0.8179 | 0.12 | 0.13 | 0.7178 | 0.16 | 0.15 | 0.7652 | 0.14 | 0.15 | 0.8104 |
| 60+ | 0.16 | 0.16 | 0.9826 | 0.11 | 0.11 | 0.8541 | 0.22 | 0.23 | 0.6357 | 0.12 | 0.15 | 0.3942 |
| Marital status: married | 0.52 | 0.54 | 0.8495 | 0.61 | 0.69 | 0.3297 | 0.35 | 0.35 | 0.9768 | 0.36 | 0.35 | 0.9303 |
| Separate/divorce | 0.07 | 0.06 | 0.8127 | 0.07 | 0.04 | 0.5515 | 0.18 | 0.17 | 0.7782 | 0.17 | 0.17 | 0.9512 |
| Widowed | 0.04 | 0.04 | 0.9929 | 0.02 | 0.02 | 0.7732 | 0.10 | 0.10 | 0.7801 | 0.05 | 0.05 | 0.8691 |
| Never married | 0.37 | 0.36 | 0.9265 | 0.30 | 0.25 | 0.4903 | 0.37 | 0.38 | 0.8142 | 0.42 | 0.42 | 0.9441 |
| Education: < HS grad | 0.23 | 0.20 | 0.6344 | 0.20 | 0.13 | 0.3002 | 0.17 | 0.21 | 0.5149 | 0.06 | 0.05 | 0.7370 |
| HS grad | 0.36 | 0.40 | 0.6138 | 0.32 | 0.36 | 0.6718 | 0.36 | 0.32 | 0.3606 | 0.33 | 0.28 | 0.4491 |
| Some college | 0.24 | 0.24 | 0.9811 | 0.29 | 0.30 | 0.8771 | 0.22 | 0.20 | 0.6179 | 0.25 | 0.27 | 0.8116 |
| College grad | 0.17 | 0.17 | 0.8640 | 0.18 | 0.21 | 0.6905 | 0.24 | 0.27 | 0.5798 | 0.36 | 0.40 | 0.5823 |
| Employment: Full time | 0.42 | 0.43 | 0.8533 | 0.48 | 0.55 | 0.4316 | 0.36 | 0.35 | 0.7652 | 0.48 | 0.47 | 0.9011 |
| Part-time | 0.10 | 0.13 | 0.6642 | 0.14 | 0.09 | 0.3324 | 0.09 | 0.08 | 0.8125 | 0.07 | 0.06 | 0.5975 |
| Unemployed | 0.19 | 0.16 | 0.6183 | 0.20 | 0.16 | 0.5872 | 0.17 | 0.17 | 0.9784 | 0.17 | 0.21 | 0.5348 |
| Retired | 0.13 | 0.13 | 0.8738 | 0.09 | 0.09 | 0.9855 | 0.15 | 0.17 | 0.5522 | 0.05 | 0.06 | 0.7603 |
| Other | 0.16 | 0.14 | 0.6410 | 0.09 | 0.12 | 0.7386 | 0.24 | 0.24 | 0.9811 | 0.23 | 0.20 | 0.7607 |
| Income: < 100% Federal Poverty Level (FPL) | 0.22 | 0.22 | 0.9700 | 0.22 | 0.15 | 0.4057 | 0.33 | 0.30 | 0.6366 | 0.23 | 0.22 | 0.9151 |
| 100-199% FPL | 0.24 | 0.24 | 0.9288 | 0.26 | 0.28 | 0.8051 | 0.18 | 0.17 | 0.7812 | 0.20 | 0.17 | 0.6145 |
| 200-299% FPL | 0.06 | 0.08 | 0.4620 | 0.04 | 0.07 | 0.4436 | 0.11 | 0.11 | 0.8985 | 0.16 | 0.12 | 0.5316 |
| 300-399% FPL | 0.17 | 0.16 | 0.7394 | 0.17 | 0.19 | 0.8038 | 0.09 | 0.09 | 0.9171 | 0.11 | 0.11 | 0.8941 |
| 400% + FPL | 0.17 | 0.18 | 0.8076 | 0.22 | 0.23 | 0.8097 | 0.17 | 0.18 | 0.7072 | 0.25 | 0.30 | 0.5118 |
| Missing | 0.14 | 0.12 | 0.7434 | 0.10 | 0.09 | 0.9090 | 0.12 | 0.15 | 0.6666 | 0.06 | 0.08 | 0.7118 |
| Frequency of unfair treatment (1-4) | 2.12 | 2.10 | 0.8794 | 2.18 | 2.20 | 0.8906 | 2.13 | 2.18 | 0.7380 | 2.15 | 2.17 | 0.8751 |
| Neighbor disadvantage | 0.36 | 0.36 | 0.9693 | 0.34 | 0.33 | 0.6244 | 0.35 | 0.35 | 0.9721 | 0.34 | 0.32 | 0.2751 |
| Neighbor advantage | 0.26 | 0.26 | 0.8673 | 0.29 | 0.30 | 0.5907 | 0.28 | 0.28 | 0.9617 | 0.30 | 0.33 | 0.4769 |
| Liquor store density (per 1000 population) | 0.11 | 0.12 | 0.7791 | 0.11 | 0.11 | 0.8023 | 0.11 | 0.11 | 0.7100 | 0.11 | 0.09 | 0.2755 |
| PROTECTIVE RESOURCES | ||||||||||||
| Religion very important and discourages drinking (1=yes) | 0.38 | 0.40 | 0.8477 | 0.29 | 0.25 | 0.6023 | 0.43 | 0.45 | 0.7602 | 0.39 | 0.37 | 0.8100 |
| Network disapproval of drinking (mean; range 0-6) | 3.23 | 3.31 | 0.8184 | 2.41 | 2.32 | 0.7936 | 3.93 | 4.07 | 0.4861 | 2.87 | 2.96 | 0.8077 |
| Network disapproval of heavy drinking (mean; range 0-3) | 2.45 | 2.47 | 0.8761 | 2.22 | 2.23 | 0.9619 | 2.63 | 2.61 | 0.7991 | 2.47 | 2.53 | 0.5919 |
| Dryness of network based on “regular” drinking (mean; range 0-3) | 1.83 | 1.91 | 0.5483 | 1.65 | 1.68 | 0.8568 | 2.14 | 2.20 | 0.4193 | 1.98 | 1.98 | 0.9591 |
| Dryness of network based on heavy drinking (mean; range 0-3) | 2.47 | 2.51 | 0.7139 | 2.38 | 2.44 | 0.6817 | 2.54 | 2.55 | 0.9132 | 2.49 | 2.49 | 0.9992 |
| Family social support (mean; range 0-12) | 10.16 | 10.32 | 0.6373 | 10.33 | 10.31 | 0.9738 | 9.70 | 9.56 | 0.7028 | 9.65 | 9.62 | 0.9497 |
| Area religious membership(per 1000 population) | 514.45 | 526.15 | 0.6389 | 517.79 | 505.57 | 0.5655 | 520.31 | 517.14 | 0.8039 | 524.62 | 522.65 | 0.9070 |
Notes. Pairwise tests comparing Whites to Blacks indicated no significant differences.
We present results from analyses of the racial difference in current drinking prevalence in the overall sample (N=4,173) and in heavy drinking prevalence among current drinkers (N=2,661). For each analysis, proportions with the drinking outcome were first compared between Whites and Blacks without adjustment (i.e., the raw estimates applying only the sampling weights). A series of PS weights (in which each subsequent weight adds new factors to those entered in the previous weight) were then created to progressively adjust for: 1) age and marital status, 2) individual-level socioeconomic disadvantage and unfair treatment, and 3) neighborhood-level socioeconomic context and alcohol outlet density. Order of entry was theoretically motivated, beginning with basic demographics and proceeding to individual-level risk factors, followed by (less proximate) area-level risk factors. The final weighting step adjusted for racial differences in all preceding factors and protective resources. For each stage of the PS weighting adjustment, the adjusted White prevalence of current or heavy drinking was compared to the Black prevalence to assess change in the racial difference in the drinking outcome. We tested this difference in proportions in weighted analysis with the PS weights treated as sampling weights, performed by applying the STATA survey command (StataCorp., 2015) which generates robust standard error estimates. To facilitate comparisons across drinking outcomes and groups, we report both absolute and relative changes in the Black-White difference in drinking outcomes.
RESULTS
Racial/Ethnic Differences in Risk and Protective Factors
As expected, the unweighted sample of Blacks tended to be younger than Whites, were less likely to be married, had lower SES, experienced unfair treatment more frequently, and resided in areas of greater disadvantage and less neighborhood advantage (Table 1). However, Black men and women also had higher levels of proscriptive religiosity and area-level religiosity as well as “drier” social network norms; Black women compared to White women also had fewer drinkers among the people they were close to. A similar pattern of racial differences was found in the subsample of current drinkers. As seen in Table 1a, after PS weighting there were no longer differences between Blacks and Whites.
Racial/ethnic Differences in Current Drinking
As shown in Table 2, unadjusted prevalence of current drinking was higher among Whites than Blacks. While this gap increased slightly after adjusting for group differences in age and marital status, the racial gap decreased after weighting on individual- and neighborhood-level risk factors (decreasing by 41% in men and 88% in women). Following subsequent weighting on protective resources, White drinking prevalence fell by an additional 10 percentage points in men and 11 points in women, resulting in comparable abstinence rates in Black and White men and women.
Table 2.
Estimates of Racial/ethnic Differences in Current Drinking Prevalence: Results from Propensity Score Weighting (2009-10 U.S. National Alcohol Survey)
| Weighting Factors a | Black % (SE) |
White % (SE) |
White-Black Difference b (95% CIs) |
|---|---|---|---|
| MEN | |||
| Unadjusted (“baseline”) | 57.1 (5.1) | 75.4 (1.8) | 18.3 (7.7, 28.9)*** |
| Age, marital status | 57.1 (5.1) | 75.9 (2.0) | 18.8 (8.0, 29.6)*** |
| Individual SES, unfair treatment | 57.1 (5.1) | 70.9 (3.2) | 13.8 (2.0, 25.6)* |
| Neighborhood SES, alcohol outlet density | 57.1 (5.1) | 68.1 (3.8) | 11.0 (−1.5, 23.5)† |
| Protective Resources | 57.1 (5.1) | 58.2 (5.7) | 1.1 (−14.0, 16.1) |
| WOMEN | |||
| Unadjusted (“baseline”) | 50.7 (3.4) | 64.4 (1.6) | 13.7 (6.5, 21.0)*** |
| Age, marital status | 50.7 (3.4) | 64.6 (2.6) | 13.9 (5.6, 22.2)** |
| Individual SES, unfair treatment | 50.7 (3.4) | 58.3 (3.2) | 7.6 (−1.6, 16.7) |
| Neighborhood SES, alcohol outlet density | 50.7 (3.4) | 52.4 (4.8) | 1.7 (−9.9, 13.2) |
| Protective Resources c | 50.7 (3.4) | 41.5 (4.1) | −9.2 (−19.5, 1.1)† |
Notes.
PS weighting was performed to weight the White sample to be similar to Black sample on an increasing number of factors introduced at each step, with black as the reference group; factors in each step include the variables in prior steps.
The White-Black difference is calculated as the White % - the Black %.
Protective resources include proscriptive religiosity, social network drinking norms and patterns, family social support, area-level religious membership
p<0.10
p<0.05
p<0.01
p<0.001
Racial/ethnic Differences in Heavy Drinking among Drinkers
Table 3 shows the racial difference in heavy drinking prevalence among current drinkers. We expected that weighting on risk factors would increase the White heavy drinking prevalence (and widen the racial gap), and that adjusting for protective factors would decrease prevalence (and narrow the gap). Among male drinkers, weighting on risk factors increased the age- and marriage-adjusted racial gap in heavy drinking by 35% or 6.3 percentage points (from 18.0 % to 24.3%). Notably, weighting on these same risk factors had the opposite effect on men’s current drinking prevalence in the overall sample, reducing the Black-White gap in current drinking by 41% (from 18.8 to 11.0 points, see Table 2 upper panel). After weighting on protective resources, the racial gap in male drinkers’ heavy drinking was reduced by 5.5 points (or 23%), which is considerably less than the 9.9 point (or 90%) decrease in the racial gap in men’s current drinking prevalence following adjustment for protective factors. The latter thus appear to have a stronger effect on the Black-White difference in men’s abstinence than heavy drinking. Even after adjusting for differences in risk and protective factors, a sizeable racial gap in male drinkers’ heavy drinking prevalence remained.
Table 3.
Estimates of Racial/ethnic Differences in Heavy Drinking Prevalence: Results from Propensity Score Weighting (2009-10 U.S. National Alcohol Survey)
| Men | Women | |||||
|---|---|---|---|---|---|---|
| Weighting Factors a | Black % (SE) |
White % (SE) |
White-Black Difference b (95% CIs) |
Black % (SE) |
White % (SE) |
White-Black Difference b (95% CIs) |
| Unadjusted (“baseline”) | 13.5 (5.0) | 27.9 (2.4) | 14.3 (3.5, 25.1)** | 10.0 (3.5) | 18.0 (1.9) | 8.0 (0.2, 15.7)* |
| Age, marital status | 13.5 (5.0) | 31.5 (2.8) | 18.0 (6.8, 29.1)** | 10.0 (3.5) | 27.2 (3.9) | 17.2 (7.0, 27.4)*** |
| Individual SES, unfair treatment | 13.5 (5.0) | 35.1 (4.2) | 21.5 (8.7, 34.3)*** | 10.0 (3.5) | 24.6 (3.7) | 14.5 (4.6, 24.5)** |
| Neighborhood SES, alcohol outlet density | 13.5 (5.0) | 37.8 (5.0) | 24.3 (10.5, 38.1)*** | 10.0 (3.5) | 22.5 (3.7) | 12.4 (2.4, 22.5)* |
| Protective Resources c | 13.5 (5.0) | 32.3 (5.5) | 18.7 (4.1, 33.3)* | 10.0 (3.5) | 13.0 (3.2) | 3.0 (−6.3, 12.3) |
Notes. Analysis was limited to current drinkers (results for the overall sample including abstainers are available from the authors upon request). Heavy drinking was defined as 5+ drinks/day on at least 7 occasions for men, and 4+ drinks/day on at least 3 occasions for women.
PS weighting was performed to weight the White current drinker sample to be similar to Black current drinker sample on an increasing number of factors introduced at each step, with black as the reference group; factors in each step include the variables in prior steps.
The White-Black difference is calculated as the White % - the Black %.
Protective resources include proscriptive religiosity, social network drinking norms and patterns, family social support, area-level religious membership
p<0.10
p<0.05
p<0.01
p<0.001
Results for female drinkers differed from men’s in that weighting on risk factors reduced the age- and marriage-adjusted racial gap in heavy drinking by 27% (from 17.2 to 12.4 points). After additional weighting on protective resources, the Black-White female gap in heavy drinking decreased by another 9.5 points (76%), which is similar to the 10.9 point decrease in the racial gap in women’s current drinking prevalence (Table 2, bottom panel). Thus, among women, protective resources appear to have similar effects on both reducing current drinking (that is, increasing abstinence) and reducing heavy drinking by drinkers.
DISCUSSION
The current study aimed to shed light on the differential prevalence of heavy drinking in Blacks and Whites generally found in large national surveys. Specifically, we examined whether protective resources previously associated with lower alcohol consumption help to explain the “paradox” of African Americans’ lower heavy drinking prevalence. We implemented a series of PS weighting adjustments to progressively remove racial/ethnic differences in the distribution of both risk and protective factors in the two groups; this balancing of risk factors across groups controls for population-level confounders and is needed to assess the validity of protective resources as an explanation for differential heavy drinking. Doing so altered the Black-White gap in heavy drinking prevalence.
Overall, our results indicate that racial differences in protective resources help to explain the paradox and provide partial support for stated hypotheses. As expected, when male drinkers had similar levels of social and economic risk factors, White men’s heavy drinking increased, widening the racial gap in heavy drinking; and when men had similar levels of protective resources, White men’s heavy drinking decreased. This reduction helped to offset the increase in heavy drinking associated with greater risk exposure, narrowing the Black-White gap considerably, but White men nevertheless had more prevalent heavy drinking. We discuss this below with how protective factors operate.
Our findings for women were different from men’s in that the racial gap in heavy drinking decreased when White and Black female drinkers had similar levels of disadvantage; this gender difference was unexpected and is discussed below. Supporting our second hypothesis, the heavy drinking gap was reduced and virtually eliminated when the racial groups had similar levels of protective resources.
Research from the broader health field has attempted to understand causes of health disparities between Blacks and Whites. A few studies have examined what happens when these groups have similar exposure to adverse individual and environmental conditions, such as the Exploring Health Disparities in Integrated Communities Study (EHDIC) (LaVeist, Pollack, Thorpe, Fesahazion, & Gaskin, 2011), or similar health-promoting resources such as access to health care through the Veterans Health Administration (VA) (Kovesdy et al., 2015). Such studies have found that Black-White disparities are attenuated, erased, or actually reversed compared to national disparity rates. For example, the EHDIC study found that Black-White disparities in hypertension, diabetes, and obesity among women were either smaller than nationally, or even non-existent, in a low-income, racially integrated community in Baltimore (LaVeist et al., 2011). This was because White residents showed much greater health risk than Whites nationally, indicating White residents’ compromised health when exposed to similar socioeconomic and community risk factors as Blacks (LaVeist et al., 2011). Further, a “reverse disparity” in smoking prevalence and intensity was found, with White residents faring worse than both their Black neighbors and Whites nationwide (LaVeist, Thorpe, Mance, & Jackson, 2007). Similarly, in a different study of Black and White VA patients (which is an atypical sample in that Blacks and Whites have similar health care access), a reverse disparity in all-cause mortality and incident coronary heart disease was found, with Black patients showing better health outcomes than Whites (Kovesdy et al., 2015).
Although our study is focused on alcohol outcomes, our results are largely in keeping with these findings of poorer outcomes in Whites with similar risk factor exposure as Blacks (we found increased heavy drinking in White male drinkers after weighting on risk factors), and are also consistent with reduced Black-White health differences given similar protective conditions across groups (the racial difference in heavy drinking decreased after weighting on protective resources). However, one difference concerns the EHDIC finding that the Black-White gap in binge drinking was much smaller than seen nationally (Fesahazion, Thorpe, Bell, & LaVeist, 2012). Unlike the EHDIC study, our analysis was gender-stratified and showed that exposure to similar risk factors reduced the racial gap only in women’s heavy drinking, not men’s.
A secondary aim of our study was to examine how protective resources contribute to Black-White differences in heavy drinking; that is, by increasing abstinence, reducing heavy drinking among drinkers, or both. Study results suggest that both mechanisms are relevant, but to varying degrees in men and women. For women, adjusting protective factors had a very similar effect on the Black-White gap in both current drinking prevalence and heavy drinking prevalence among drinkers, reducing the racial difference by 10.9 and 9.5 percentage points, respectively. In men, protective resources had nearly double the impact on the racial gap in current drinking prevalence as it did on heavy drinking, yielding a 9.9 versus 5.5 point reduction, respectively. Thus, while protective factors affect men’s abstinence and heavy drinking, they appear to have a larger impact on the Black-White difference in abstinence.
There may be several reasons for observed gender differences in the effects of protective resources on the racial gap in heavy drinking. First, because racial differences in protective factors were somewhat greater in female drinkers than male drinkers, weighting resulted in a larger increase in protective resources for White women than White men. Also, the racial gap in women’s baseline heavy drinking was smaller than men’s (8.0 vs. 14.4 percentage points). This may reflect the lower frequency threshold used to operationalize women’s heavy drinking (3+ days in women vs. 7+ days in men), necessitated by the relative rarity of heavy drinking in women. Related to this, it may be that protective resources more effectively inhibit infrequent behaviors that are presumably less habitual; if so, this could help explain the larger impact on White women’s (less frequent) heavy drinking than men’s.
Additionally, men’s heavy drinking might be reinforced by factors not studied here, such as a broad-based drinking culture that is more permissive of men’s heavy drinking than women’s. Research suggests there are gender differences in how stress manifests as mental health problems (Aneshensel, Rutter, & Lachenbruch, 1991), with men more likely to evidence substance use disorders and women more likely to manifest symptoms of affective or anxiety disorders. This is consistent with observed gender differences in the strength of association between stressors and alcohol outcomes (Matheson, White, Moineddin, & Dunn, 2012; Mulia, Zemore, Murphy, Liu, & Catalano, 2014), the relationship between drinking to cope and alcohol problems (Cooper et al., 1995), and mediating pathways from economic stressors to psychological distress and alcohol problems (Brown & Richman, 2012), all of which point to stronger associations among men than women and which could reflect gender differences in culturally acceptable ways of coping with stress (Griffith, 2012). While longitudinal studies demonstrate women’s increased risk for problem drinking following exposure to socioeconomic and environmental stressors (Hill & Angel, 2005; Mulia, Schmidt, et al., 2008), our finding that disadvantage had opposite effects on White men and women’s heavy drinking prevalence suggests that heavy drinking may be a much more pervasive response in men (vs. women) to the types of stressors examined here.
Limitations
The present results should be interpreted in light of several study limitations. First, this study assessed the overall effect of protective resources, recognizing that there may be synergistic effects of protective factors that should be captured when trying to explain African Americans’ lower heavy drinking prevalence. Future studies could strive to identify individual factors underlying this protection, as well as common and powerful combinations of protective resources for each racial group of interest. Second, we lacked data to examine potentially protective genetic factors that may deter heavy drinking among Blacks (Zapolski et al., 2014). Also, our measures of drinking norms and patterns pertain to people “important to you” and might not capture a broad-based drinking culture permissive of men’s heavy drinking. Third, it should not be assumed that protective resources that reduce heavy drinking will also prevent alcohol-related problems among heavy drinkers, as different protective resources such as good health and access to regular health care and high-quality alcohol treatment services may prevent problems. Indeed, compared to Whites, Blacks have lower levels of heavy drinking but elevated risk for alcohol problems. Fourth, a reverse health disparity may reflect differential exposure to protective factors as well as differential effects of such exposure. The PS method addresses the former by balancing protective (and risk) exposures in the two groups. Racial differences in heavy drinking that remain after this adjustment could indicate differential effects of protective (or risk) exposure(s) -- for instance, a stronger protective effect of proscriptive religiosity on Black men’s compared to White men’s heavy drinking as previously reported (Herd, 1994). Finally, the use of PS methods creates a counterfactual scenario for estimating a hypothetical reduction in the Black-White gap in heavy drinking; also, as these data are more than five years old, it is unclear whether these findings would hold in more recent surveys.
Conclusions
Our study suggests that protective resources play a significant role in explaining the “paradox” of Blacks’ lower heavy drinking prevalence relative to Whites, particularly for women. This was less true for men, where PS weighting on protective resources reduced some of the racial difference in heavy drinking prevalence but had a larger impact on abstinence rates. Future research should investigate factors not studied here which may reinforce heavy drinking in White men and/or suppress it in Black men; for instance, cultural norms that may support heavy drinking as a social practice and source of enjoyment in certain contexts, particularly for White men whose heavy drinking has been more strongly associated with social and enhancement motives than Black men’s (Cooper et al., 2008). Identifying and intervening on such influences might reduce alcohol-related morbidity and mortality in these groups.
As discussed, the protective resources examined here could influence heavy drinking in a number of ways. For example, proscriptive religiosity could directly shape drinking attitudes, and reduce drinking to cope to the extent that it increases access to social support from faith-based communities (Murry, Bynum, Brody, Willert, & Stephens, 2001). New research suggests that religiosity might also reduce stress by influencing the body’s neurobiological stress response processes (Holmes & Kim-Spoon, 2016). Studies that can identify the multiple, salutary effects of a given protective factor, and on various theoretically-linked mental health and behavioral outcomes, could yield a more comprehensive understanding of protective resources and how these bolster health. Moreover, research that elucidates the protective resources and other assets of communities that promote health and well-being (Morgan & Ziglio, 2007) can allow us to build on these strengths and actively engage communities in preventing alcohol-related and other health problems.
Acknowledgments
This work was supported by the U.S. National Institute on Alcohol Abuse and Alcoholism (R01AA020474, R01AA022668, and P50AA005595).
Footnotes
DECLARATION OF INTEREST
The authors declare that they have no conflicts of interest.
REFERENCES
- Aneshensel CS, Rutter CM, & Lachenbruch PA (1991). Social structure, stress, and mental health: competing conceptual and analytic models. American Sociological Review, 56(2), 166–178. [Google Scholar]
- Blumberg SJ, & Luke JV (2009). Wireless Substitution: Early Release of Estimates from the National Health Interview Survey, July-December 2008 [Accessed: 2012–06-14 Archived by WebCite® at http://www.webcitation.org/68Q6oLoEC] (pp. 13). Hyattsville, MD: National Center for Health Statistics. [Google Scholar]
- Brenner AB, Borrell LN, & Barrientos-Gutierrez T (2015). Longitudinal associations of neighborhood socioeconomic characteristics and alcohol availability on drinking: results from the Multi-Ethnic Study of Atherosclerosis (Mesa). Social Science and Medicine, 145, 17–25. doi: 10.1016/j.socscimed.2015.09.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Kendler KS, Su M, Gaxiola-Aguilar S, & Kessler RC (2005). Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychological Medicine, 35(3), 317–327. doi: 10.1017/S0033291704003514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RL, & Richman JA (2012). Sex differences in mediating and moderating processes linking economic stressors, psychological distress, and drinking. Journal of Studies on Alcohol and Drugs, 73(5), 811–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2013). CDC Health Disparities and Inequalities Report–United States, 2013. MMWR. Morbidity and Mortality Weekly Report, 62(Suppl. 3), 1–186. [PubMed] [Google Scholar]
- Cohen S, & Syme SL (Eds.). (1985). Social support and health. New York: Academic Press. [Google Scholar]
- Cooper ML, Frone MR, Russell M, & Mudar P (1995). Drinking to regulate positive and negative emotions: a motivational model of alcohol use. Journal of Personality and Social Psychology, 69(5), 990–1005. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Krull JL, Agocha VB, Flanagan ME, Orcutt HK, Grabe S, … Jackson M (2008). Motivational pathways to alcohol use and abuse among black and white adolescents. Journal of Abnormal Psychology, 117(3), 485–501. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Saha TD, & Grant BF (2015). Changes in alcohol consumption: United States, 2001–2002 to 2012–2013. Drug and Alcohol Dependence, 148, 56–61. doi: 10.1016/j.drugalcdep.2014.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder JP, Campbell NR, Litrownik AJ, Ayala GX, Slymen DJ, Parra-Medina D, & Lovato CY (2000). Predictors of cigarette and alcohol susceptibility and use among Hispanic migrant adolescents. Preventive Medicine, 31(2, Pt. 1), 115–123. [DOI] [PubMed] [Google Scholar]
- Fesahazion RG, Thorpe RJ Jr., Bell CN, & LaVeist TA (2012). Disparities in alcohol use: does race matter as much as place? Preventive Medicine, 55(5), 482–484. doi: 10.1016/j.ypmed.2012.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franzini L, Ribble JC, & Keddie AM (2002). Understanding the Hispanic paradox In LaVeist TA (Ed.), Race, Ethnicity, and Health (pp. 280–304). San Francisco, CA: Jossey-Bass. [PubMed] [Google Scholar]
- Grammich C, Hadaway K, Houseal R, Jones DE, Krindatch A, Stanley R, & Taylor RH (2012). 2010 U.S. Religion Census: Religious congregations & membership study. Kansas City, MO: Association of Statisticians of American Religious Bodies. [Google Scholar]
- Greenfield TK (2000). Ways of measuring drinking patterns and the difference they make: experience with graduated frequencies. Journal of Substance Abuse, 12(1–2), 33–49. doi: 10.1016/S0899-3289(00)00039-0 [DOI] [PubMed] [Google Scholar]
- Greenfield TK, Ye Y, Karriker-Jaffe KJ, & Kerr WC (2013). Practical utility of a new propensity score weighting technique for estimates based on landline-only cases in a dual frame landline/mobile telephone US national alcohol survey. Presented at the 141st Annual American Public Health Association Meeting and Exposition Boston, MA: November 2–6. [Google Scholar]
- Griffith DM (2012). An intersectional approach to men’s health. Journal of Men’s Health, 9(2), 106–112. doi: 10.1016/j.jomh.2012.03.003 [DOI] [Google Scholar]
- Groves RM (2006). Nonresponse rates and nonresponse bias in household surveys. Public Opinion Quarterly, 70(5), 646–675. doi: 10.1093/poq/nfl033 [DOI] [Google Scholar]
- Herd D (1994). Predicting drinking problems among black and white men: results from a national survey. Journal of Studies on Alcohol, 55(1), 61–71. doi: 10.15288/jsa.1994.55.61 [DOI] [PubMed] [Google Scholar]
- Herd D, & Grube JW (1996). Black identity and drinking in the US: a national study. Addiction, 91(6), 845–857. doi: 10.1046/j.1360-0443.1996.91684510.x [DOI] [PubMed] [Google Scholar]
- Hill TD, & Angel RJ (2005). Neighborhood disorder, psychological distress, and heavy drinking. Social Science and Medicine, 61(5), 965–975. [DOI] [PubMed] [Google Scholar]
- Holmes C, & Kim-Spoon J (2016). Why are religiousness and spirituality associated with externalizing psychopathology? A literature review. Clinical Child and Family Psychology Review, 19(1), 1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones-Webb R, Karriker-Jaffe KJ, Zemore SE, & Mulia N (2016). Effects of economic disruptions on alcohol use and problems: why do African Americans fare worse? Journal of Studies on Alcohol and Drugs, 77(2), 261–271. doi: 10.15288/jsad.2016.77.261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe KJ (2011). Areas of disadvantage: a systematic review of effects of area-level socioeconomic status on substance use outcomes. Drug and Alcohol Review, 30(1), 84–95. doi: 10.1111/j.1465-3362.2010.00191.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe KJ (2013). Neighborhood socioeconomic status and substance use by U.S. adults. Drug and Alcohol Dependence, 133(1), 212–221. doi: 10.1016/j.drugalcdep.2013.04.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes CL (2009). The black-white paradox in health: flourishing in the face of social inequality and discrimination. Journal of Personality, 77(6), 1677–1706. [DOI] [PubMed] [Google Scholar]
- Keyes KM, & Cerdá M (2013). Racial/ethnic differences in alcohol-related suicide: a call for focus on unraveling paradoxes and understanding structural forces that shape alcohol-related health. Alcoholism: Clinical and Experimental Research, 37(5), 717–719. doi: 10.1111/acer.12083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovesdy CP, Norris KC, Boulware LE, Lu JL, Ma JZ, Streja E, … Kalantar-Zadeh K (2015). Association of race with mortality and cardiovascular events in a large cohort of US veterans. Circulation, 132(16), 1538–1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist TA, Pollack K, Thorpe R Jr., Fesahazion R, & Gaskin D (2011). Place, not race: disparities dissipate in Southwest Baltimore when blacks and whites live under similar conditions. Health Affairs, 30(10), 1880–1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist TA, Thorpe RJ Jr., Mance GA, & Jackson J (2007). Overcoming confounding of race with socio-economic status and segregation to explore race disparities in smoking. Addiction, 102(Suppl. 2), 65–70. [DOI] [PubMed] [Google Scholar]
- Lee DB, Neblett EW Jr., & Jackson V (2015). The role of optimism and religious involvement in the association between race-related stress and anxiety symptomatology. The Journal of Black Psychology, 41(3), 221–246. [Google Scholar]
- Lindenberg CS, Strickland O, Solorzano R, Galvis C, Dreher M, & Darrow VC (1999). Correlates of alcohol and drug use among low-income hispanic immigrant childbearing women living in the U.S.A. International Journal of Nursing Studies, 36(1), 3–11. [DOI] [PubMed] [Google Scholar]
- Martin JK, Tuch SA, & Roman PM (2003). Problem drinking patterns among African Americans: the impacts of reports of discrimination, perceptions of prejudice, and “risky” coping strategies. Journal of Health and Social Behavior, 44(3), 408–425. [PubMed] [Google Scholar]
- Matheson FI, White HL, Moineddin R, & Dunn JR (2012). Drinking in context: the influence of gender and neighbourhood deprivation onalcohol consumption Journal of Epidemiology and Community Health, 66, e4. [DOI] [PubMed] [Google Scholar]
- Mezuk B, Raffety JA, Kershaw KN, Hudson D, Abdou CM, Lee H, … Jackson JS (2010). Reconsidering the role of social disadvantage in physical and mental health: stressful life events, health behaviors, race, and depression. American Journal of Epidemiology, 172(11), 1238–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalak L, Trocki K, & Bond J (2007). Religion and alcohol in the U.S. National Alcohol Survey: how important is religion for abstention and drinking? Drug and Alcohol Dependence, 87(2–3), 268–280. doi: 10.1016/j.drugalcdep.2006.07.013 [DOI] [PubMed] [Google Scholar]
- Midanik LT, & Greenfield TK (2003). Telephone versus in-person interviews for alcohol use: results of the 2000 National Alcohol Survey. Drug and Alcohol Dependence, 72(3), 209–214. doi: 10.1016/S0376-8716(03)00204-7 [DOI] [PubMed] [Google Scholar]
- Morgan A, & Ziglio E (2007). Revitalising the evidence base for public health: an assets model. Promotion and Education, 14(Suppl. 2), 17–22. doi: 10.1177/10253823070140020701x [DOI] [PubMed] [Google Scholar]
- Mossakowski KN (2008). Is the duration of poverty and unemployment a risk factor for heavy drinking? Social Science and Medicine, 67(6), 947–955. [DOI] [PubMed] [Google Scholar]
- Mulia N, Schmidt L, Bond J, Jacobs L, & Korcha R (2008). Stress, social support and problem drinking among women in poverty. Addiction, 103(8), 1283–1293. doi: 10.1111/j.1360-0443.2008.02234.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulia N, Ye Y, Karriker-Jaffe KJ, Kerr WC, Greenfield TK, & Jones-Webb R (2014). Racial/ethnic disparities and attitudes towards alcohol policy in the U.S. 37th Annual Research Society on Alcoholism Scientific Meeting Bellevue, WA: June 21–25. [Google Scholar]
- Mulia N, Ye Y, Zemore SE, & Greenfield TK (2008). Social disadvantage, stress and alcohol use among black, Hispanic and white Americans: findings from the 2005 U.S. National Alcohol Survey. Journal of Studies on Alcohol and Drugs, 69(6), 824–833. doi: 10.15288/jsad.2008.69.824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulia N, Zemore SE, Murphy R, Liu H, & Catalano R (2014). Economic loss and alcohol consumption and problems during the 2008 to 2009 U.S. recession. Alcoholism: Clinical and Experimental Research, 38(4), 1026–1034. doi: 10.1111/acer.12301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy RD, Zemore SE, & Mulia N (2014). Housing instability and alcohol problems during the 2007–2009 US recession: the moderating role of perceived family support. Journal of Urban Health, 91(1), 17–32. doi: 10.1007/s11524-013-9813-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murry VM, Bynum MS, Brody GH, Willert A, & Stephens D (2001). African American single mothers and children in context: a review of studies on risk and resilience. Clinical Child and Family Psychology Review, 4(2), 133–155. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. (2005). Helping patients who drink too much: a clinician’s guide. Updated 2005 Edition, revised October 2015 (NIH Publication No. 07–3769) [Accessed: 2016–08-12 Archived by WebCite® at http://www.webcitation.org/6jiIsTNiY]. Rockville, MD. [Google Scholar]
- Pearlin LI, & Radabaugh CW (1976). Economic strains and the coping function of alcohol. The American Journal of Sociology, 82(3), 652–663. [DOI] [PubMed] [Google Scholar]
- Pew Research Center. (2012). Assessing the representativeness of public opinion surveys [Accessed: 2015–02-09 Archived by WebCite® at http://www.webcitation.org/6WDcTE4P1] (pp. 51). Washington, DC. [Google Scholar]
- Rehm J, Greenfield TK, Walsh G, Xie X, Robson L, & Single E (1999). Assessment methods for alcohol consumption, prevalence of high risk drinking and harm: a sensitivity analysis. International Journal of Epidemiology, 28(2), 219–224. doi: 10.1093/ije/28.2.219 [DOI] [PubMed] [Google Scholar]
- Robins JM, Hernán MÁ, & Brumback B (2000). Marginal structural models and causal inference in epidemiology. Epidemiology, 11(5), 550–560. doi: 10.1097/00001648-200009000-00011 [DOI] [PubMed] [Google Scholar]
- Rosenbaum PR, & Rubin DB (1983). The central role of the propensity score in observational studies for causal effects. Biometrika, 70, 41–55. [Google Scholar]
- Sarkisian N, & Gerstel N (2004). Kin support among blacks and whites: race and family organization. American Sociological Review, 69(6), 812–837. [Google Scholar]
- Schwartz S, & Meyer IH (2010). Metal health disparities research: the impact within and between group analyses on tests of social stress hypotheses. Social Science and Medicine, 70(8), 1111–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scribner R, Cohen D, Kaplan S, & Allen SH (1999). Alcohol availability and homicide in New Orleans: conceptual considerations for small area analysis of the effect of alcohol outlet density. Journal of Studies on Alcohol, 60(3), 310–316. [DOI] [PubMed] [Google Scholar]
- Scribner RA, Cohen DA, & Farley TA (1998). A geographic relation between alcohol availability and gonorrhea rates. Sexually Transmitted Diseases, 25(10), 544–548. [DOI] [PubMed] [Google Scholar]
- Scribner RA, Cohen DA, & Fisher W (2000). Evidence of a structural effect for alcohol outlet density: a multilevel analysis. Alcoholism: Clinical and Experimental Research, 24(2), 188–195. [PubMed] [Google Scholar]
- StataCorp. (2015). Stata Statistical Software: Release 14.0. College Station, TX: Stata Corporation. [Google Scholar]
- Thoits PA (2010). Stress and health: major findings and policy implications. Journal of Health and Social Behavior, 51(Suppl.), S41–S53. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2011). Healthy People 2020 Objectives [Accessed: 2013–01-29 Archived by WebCite® at http://www.webcitation.org/6E2Qk6kB7] (pp. 335). Washington, DC. [Google Scholar]
- Wallace JM, Brown TN, Bachman JG, & LaVeist TA (2003). The influence of race and religion on abstinence from alcohol, cigarettes and marijuana among adolescents. Journal of Studies on Alcohol, 64(6), 843–848. [DOI] [PubMed] [Google Scholar]
- West CP (1994). Race Matters. New York, NY: Vintage Books. [Google Scholar]
- Zapolski TCB, Pedersen SL, McCarthy DM, & Smith GT (2014). Less drinking, yet more problems: understanding African American drinking and related problems. Psychological Bulletin, 140(1), 188–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore SE, Karriker-Jaffe KJ, Keithly S, & Mulia N (2011). Racial prejudice and unfair treatment: interactive effects with poverty and foreign nativity on problem drinking. Journal of Studies on Alcohol and Drugs, 72(3), 361–370. doi: 10.15288/jsad.2011.72.361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet GD, Dahlem NW, Zimet SG, & Farley GK (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30–41. [DOI] [PubMed] [Google Scholar]


