Abstract
Inflammatory bowel disease (IBD) is a known medical burden in most developed countries and a significant cause of morbidity. The IBD label includes Crohn’s disease (CD) and ulcerative colitis (UC). Pharmacological and surgical intervention are the two main management approaches for IBD. Some drugs have been developed for IBD therapy, but accessibility is limited due to high costs. Furthermore, these agents have demonstrated inactivity over long-term treatment courses. Therefore, an urgent need is present for new treatment options that are safe, able to sustain clinical remission, and improve mucosal gut healing. Seaweed has received much attention in the pharmacological field owing to its various biomedical properties, including the prolongation of blood clotting time, as well as antitumor, anti-inflammation, and antioxidant effects. This study therefore aimed to examine the effects of a dietary polysaccharide-rich extract obtained from Eucheuma cottonii (EC) on a model of colitis. Colitis was induced in male BALB/c mice by the administration of 2.5% (w/v) dextran sulfate sodium (DSS) for 7 days. DSS-induced mice were treated with either one of three different doses of EC extracts (0.35, 0.70, and 1.75 g/kg body weight) or curcumin as a positive control (0.10 g/kg). Mice were sacrificed post-treatment and blood samples were collected. The disease activity index (DAI) and inflammatory cytokine levels (tumor necrosis factor (TNF)-α, interleukin (IL)-1β, IL-6, IL-10) were measured. After treatment for 7 days, EC extract administration protected against weight loss and decreased the colon weight per length ratio. EC extract administration also decreased pro-inflammatory cytokine expression, increased IL-10 levels, and reduced colonic damage. Therefore, a dietary polysaccharide-rich extract from E. cottonii reduced DSS-induced bowel inflammation, thereby becoming a promising candidate for the treatment of colitis.
Introduction
Inflammatory bowel disease (IBD), a designation that includes Crohn’s disease (CD) and ulcerative colitis (UC), is a known medical burden in most developed countries [1, 2]. UC is characterized by intestinal inflammation and often results in diarrhea, bloody mucus, weight loss, and colon shortening [1, 3]. Since the mid-twentieth century, IBD incidence has increased in the Western world (e.g., North America, Europe, New Zealand, and Australia) [4], but only recently have newly industrialized countries in Asia, the Middle East, and South America documented the emergence of IBD [5]. Furthermore, increasing IBD prevalence has also been observed in newly industrialized countries with large populations and rapid urbanization and westernization such as India and China. As such, IBD can be categorized as a global disease [4, 5].
Currently, pharmacological and surgical intervention are the two main treatment approaches for IBD [6]. Traditional therapeutic agents such as azathioprine, 6-mercaptopurine, and antibiotics are becoming more important in steroid-resistant and steroid-dependent patients [7]. Drugs such as corticosteroids, aminosalicylates, and immunosuppressants aim to decrease inflammation, but show limited efficacy for long-term remission and present significant side effects [8]. As such, natural products, including those with marine origins, have been investigated in order to identify potential candidates for the improvement of IBD clinical symptoms [9].
Seaweeds, also known as marine algae, are now considered as potential sources for new IBD treatments. Some seaweeds can be used for the management or treatment of IBD, including Caulerpa mexicana [1], a sulfated polysaccharide from Hypnea musciformis [10], and fucoidan extract from Fucus vesicolosus [6]. These seaweeds have many bioactive compounds, such as polysaccharides, terpenes, and flavonoids, which have been documented to possess pharmacological activities including antitumor, antiprotozoal, antiviral, antioxidant, anti-nociceptive, anti-inflammatory, and anticoagulant effects [1, 11–13]. Seaweeds contain large amounts of polysaccharides, but the majority of them are not digested by humans due to the absence of the required enzymes in the gastrointestinal tract. Therefore, these can be regarded as dietary fibers, resulting in seaweed being classified as having high levels of dietary fibers (33–75%) [14, 15]. The proportion of dietary fiber is particularly rich in the soluble fraction (50–85% of the total dietary fraction), which in red seaweeds is mostly composed of sulfated galactans such as carrageenan and agar [15]. Dietary fiber has been used to treat colitis [16, 17] and modulate the gut microbiota [18, 19].
Eucheuma cottonii is a red seaweed previously reported to demonstrate antioxidant, anticoagulant, anti-tumor, and anti-inflammation properties [20–24]. Eucheuma cottonii is also known as Kappaphycus alvarezii (KA) or the “sea-bird nest” [25, 26]. In addition, studies have reported that extracts produced from this seaweed can slow tumor cell growth rate [27], promote wound healing [28], and upregulate cancer cell apoptosis [29]. Moreover, KA extracts have been shown to improve cardiovascular, liver, and metabolic parameters in obese rat models [30] and present anti-diabetic effects in streptozotocin-induced type 2 diabetic mice [31]. However, the effects of a dietary polysaccharide-rich extract from Eucheuma cottonii in a murine model of colitis has not been reported.
Various chemical agents can be used to induce colitis in rodent models, including dextran sodium sulfate (DSS), trinitrobenzene sulfonic acid (TNBS), oxazolone, acetic acid, carrageenan, indomethacin (a non-steroidal anti-inflammatory drug [NSAID]), and peptidoglycan-polysaccharides [32]. Acute or chronic colonic inflammation can be induced by DSS administration via drinking water, with its effects depending on dosage and duration [33]. The DSS colitis model is popular owing to its controllability, reproducibility, simplicity, and rapidity [34] and it has been confirmed to represent colitis both biochemically and morphologically [35]. This study therefore aimed to examine the suppressive effects of a dietary polysaccharide-rich extract from Euchuema cottonii against DSS-induced colitis in mice.
Materials and methods
Materials
Eucheuma cottonii (EC) was provided by a seaweed farm in Sabah (Famous Alpine Sdn. Bhd, Sabah, Malaysia). Curcumin was purchased from Nacalai Tesque, Inc. (Kyoto, Japan). Dextran sulfate sodium (DSS, MW ~40.000 Da) was purchased from Tokyo Chemical Industry (Tokyo, Japan). Tumor necrosis factor (TNF)-α (Cat. No. ARG80206), interleukin (IL)-6 (Cat. No. ARG80199), IL-1β (Cat. No. ARG80196), and IL-10 (Cat. No. ARG80200) ELISA kits were purchased from Arigo Biolaboratories Corporation (Hsinchu, Taiwan). Formaldehyde solution (4%) was purchased from Avantor Performance Materials, Inc. (Pennsylvania, U.S.A.). Dulbecco’s modified Eagle’s medium-low glucose (DMEM-L) and Dulbecco’s phosphate buffered saline (PBS) powders were purchased from Sigma Aldrich (Missouri, U.S.A). Antibiotic-Antimycotic (15240–062) was purchased from Gibco Life Technologies (Massachusetts, U.S.A.).
Seaweed extraction and characterization
Seaweed extraction
Seaweed extraction was performed according to previously used methods [36]. Briefly, 40 g of Eucheuma cottonii dried powder was placed in an Erlenmeyer flask and macerated with 200 mL of 70% ethanol. Extraction was performed at 50 °C for 3 h with stirring by a magnetic stirrer. The solution was filtered to separate the liquid ethanol extract from residue, with residue taken for repeated extraction by adding fresh solvent under the same conditions as the first extraction. Three extractions were performed in total. The ethanol extracts were then combined with the solvent then evaporated using a vacuum evaporator at 40 °C, resulting in a concentrated ethanol extract. Concentrated extract was transferred into fresh bottles and dried using a freeze dryer in order to obtain the final E. cottonii ethanol (EC) extract. The extraction yield (%) was calculated as extract weight (g) divided by dried seaweed powder weight (g) x 100%. The extraction yield was 17.79 ± 0.09%.
Seaweed extract characterization
EC extract proximate analysis was performed by following AOAC (2000) methods. Extract moisture content was determined in triplicate by drying at 105 °C in a hot-air oven to obtain a constant dry weight. Total nitrogen content was determined by Kjeldahl nitrogen analysis. The percentage of crude protein was estimated by multiplying total nitrogen content by a factor of 6.25 (AOAC method 981.10). Crude fat content was determined by extracting a dry ground sample for 6 h in a Soxhlet extractor with ethyl ether (AOAC method 991.36). Ash content was determined by complete incineration of the sample in a muffle furnace at 550 °C (AOAC method 930.05). Carbohydrate content was determined by the difference method.
Previously used methods were used to analyze 3,6-anhydro-galactose levels [37]. Briefly, resorcinol reagent was mixed with standards or samples in ice water for 3 min. Mixtures were then moved into a water bath and incubated at 80 °C for 10 min to allow for color development. After this, they were immediately transferred to a 96-well microplate to read absorbance at 520 nm. D-fructose (250 μmol/L) was used as a standard, with 55% of the solution an equimolar amount of 3,6-anhydro-α-D-galactopyranoside [38].
Cell viability assay
RAW 264.7 macrophages (RAW 264.7) were purchased from Bioresearch Collection and Research Center (BCRC), Taiwan and cultured in DMEM-L containing 1 g/L of glucose and L-glutamine and supplemented with 1% of antibiotic/antimycotic and 10% fetal bovine serum (FBS). Cells were maintained at 37 °C in a humidified atmosphere (5% CO2).
Cellular viability was performed by using a 3-[4,5-dimethylthiazol-2-yl]-2,5 diphenyl tetrazolium bromide (MTT)-based colorimetric assay [39]. Briefly, RAW 264.7 cells (1x105 cells/well) were cultured in 96-well microplates with different concentrations of EC extract (125, 250, 500, or 1000 μg/mL) or in the absence of EC extract (control) for 24 h. Culture supernatant was then removed and cells were washed with phosphate buffer saline (PBS). After this, 100 μL of MTT solution (1 mg/mL) was added to each well and cells were incubated for 4 h at 37 °C. After incubation, cells were dissolved with 100 μL of dimethyl sulfoxide (DMSO) and shaken at room temperature in the dark for 15 min, after which absorbance was recorded at 570 nm.
Animal models
Six-week-old male BALB/c mice were purchased from the National Laboratory Animal Center (Yilan, Taiwan). All mice were fed a standard chow-fed diet and water ad libitum. Mice were acclimatized for 1 week. Mice were housed 4 mice per cage in a room maintained at 25 ± 2 °C under a 12 h day/night cycle throughout experimentation. All procedures were carried out according to the Animal Protection Act (Act/APC) and the Experimental Animal Ethics Committee of the Council of Agriculture (CoA) of the Executive Yuan, Taiwan. The Institutional Animal Care and Use Committee (IACUC Approval No. 107003) of the National Taiwan Ocean University reviewed and approved all protocols.
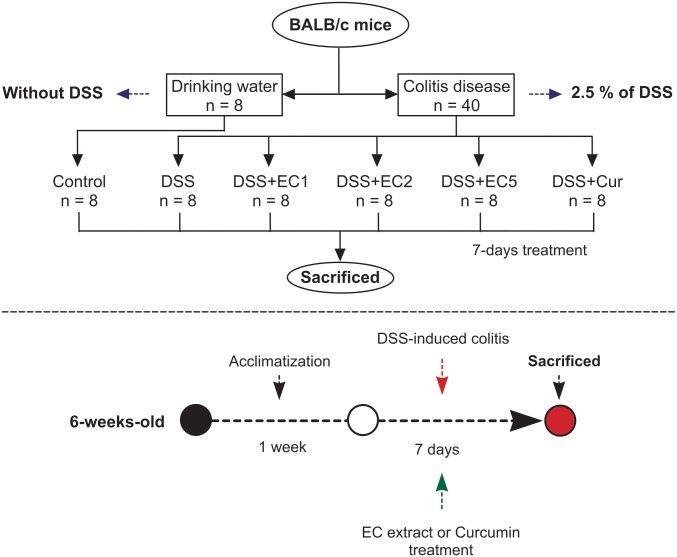
Acute colitis was established using a previously established method [35]. Briefly, mice were administered 2.5% (w/v) DSS in drinking water for 7 days [34]. Forty-eight mice were weighed prior to experimentation and then divided into six groups (8 mice per group), one which received no DSS administration (control) and five which did (DSS groups). DSS groups were then administered either varying dosages of EC extract by oral gavage (0.35 g/kg body weight, DSS+EC1; 0.70 g/kg, DSS+EC2; or 1.75 g/kg, DSS+EC5), curcumin (0.10 g/kg, DSS+Cur), or water (DSS) (Fig 1). Mice were examined daily for body weight, stool consistency, and the presence of fecal blood. EC extract and curcumin were orally delivered once per day of DSS treatment for 7 days. The mice were sacrificed on the 8th day and fasted for 12 h prior to sacrifice. Mice were euthanized by CO2 exposure in an empty chamber. The colon weight and length were measured on the day of sacrifice. Serum and colon tissue were stored at -20 °C until further analysis.
Fig 1. Flowchart of dextran sulfate sodium (DSS) induction of colitis in mice.
Disease activity index
Disease activity index (DAI) was measured by previous methods [35, 40, 41] and calculated based on the presence of fecal blood, stool consistency, and weight loss percentage. DAI values were calculated as [(weight loss score) + (stool consistency) + (rectal bleeding score)]/4 and scored on a 0–4 scale (Table 1).
Table 1. Disease activity index (DAI) scoring of DSS-induced colitis.
| Score | Occult/gross bleeding | Weight loss (% of initial weight) | Stool consistency |
|---|---|---|---|
| 0 | None | < 1 | Normal stools |
| 1 | Small spots of blood stool; dry anal region | 1–5 | Soft pellets not adhering to the anus |
| 2 | Large spots of blood in stool; blood appears through the anal orifice | 5–10 | Very soft pellets adhering to the anus |
| 3 | Deep red stool; blood spreads largely around the anus | 10–15 | Liquid stool in long streams; wet anus |
| 4 | Gross bleeding | > 15 | Diarrhea |
Inflammatory cytokine level analysis
Blood serum was collected using a syringe and centrifuged for 15 min at 3,000 rpm and stored at -20 °C. The supernatant of homogenized colon tissue was prepared by weighing 100 mg of colon tissue, suspending it in 900 μL of cold PBS, and then homogenizing using a micro-tube homogenizer. Preparations were stored at -20°C, then thawed at room temperature prior to use. Homogenized tissue was centrifuged at 5,000 rpm for 15 min and the supernatant was collected for the cytokine analysis [42, 43]. Pro-inflammatory cytokines (TNF-α, IL-1β, and IL-6) and anti-inflammatory (IL-10) cytokines were detected using enzyme-linked immunosorbent assay (ELISA) kits via manufacturer’s protocols.
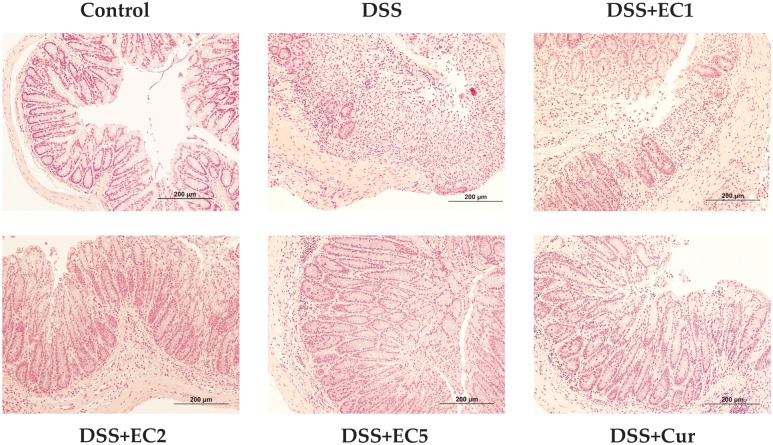
Histopathology analysis
Upon sacrifice, mouse colons were collected and the distal colon was fixed in 4% neutral-buffered formaldehyde solution. Specimens were then embedded in paraffin after fixation and 5 μm-thick sections were cut and stained with hematoxylin and eosin (H&E) as described by previous methods [44] by Lie Pei Co., Ltd. Colonic histology was scored according to previous methods [45, 46]: Scores were defined as: 0, normal colonic mucosa; 1, loss of one-third of the crypts; 2, loss of two-thirds of the crypts; 3, lamina propria covered with a single layer of epithelial cells with mild inflammatory cell infiltration; and 4, erosions and marked inflammatory cell infiltration.
Statistical analysis
All data were expressed as mean ± standard deviation (S.D.). The data were analyzed using Duncan’s multiple range test (P<0.05) using SPSS 22.0.
Results
EC extract chemical composition
Proximate analysis revealed that EC extract possessed high levels of carbohydrates (74.77 ± 1.15%) and ash (19.66 ± 0.16%), followed by proteins (2.88 ± 0.05%), moisture (1.44 ± 0.48%), and fat (1.26 ± 0.18%). The level of 3,6-anhydro-D-galacose was roughly 43.74 ± 6.30 μmol/L.
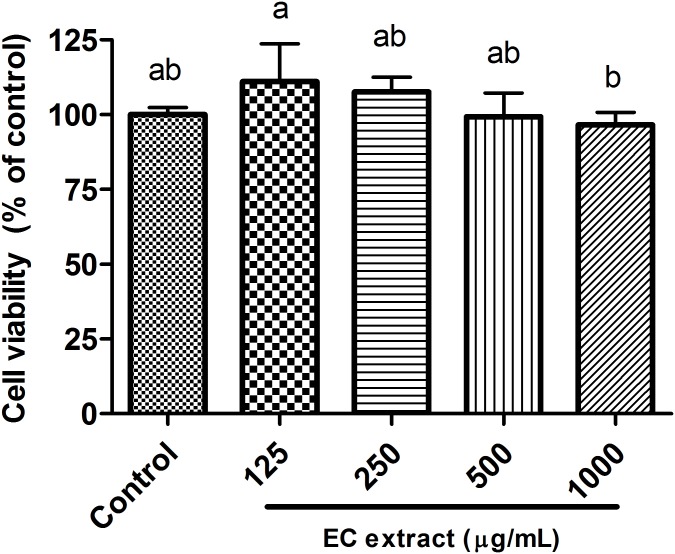
Effect of EC extract on cell viability
EC extract was not toxic to RAW 264.7 macrophage cells (Fig 2) or normal cells. Cell viability between EC extract- and control-treated cells did not differ significantly. Seaweed extracts have been previously reported to be non-toxic to normal cells [47] and human keratinocyte (HaCaT) cells [26].
Fig 2. Cell viability of RAW 264.7 macrophage after treatment with EC extract for 24 h.
Data are shown as the mean ± S.D. (n = 5). Different letters (a-b) indicate statistical significance (P<0.05) as determined by Duncan’s multiple range test.
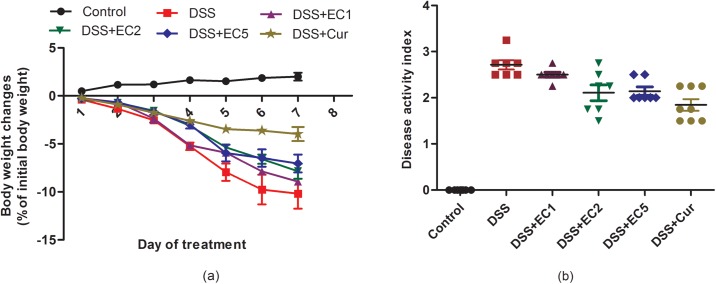
Weight loss and disease activity index scores
Body weight loss was increased in DSS-treated mice, with EC extract or Curcumin administration attenuating body weight loss extent (Fig 3a). Disease activity index scores were higher in untreated DSS-treated mice versus EC- and Curcumin-treated counterparts (Fig 3b).
Fig 3. Effect of EC extract on (a) weight loss and (b) disease activity index in DSS-treated mice during and after 7 days of treatment.
Data are shown as the mean ± S.D. (n = 8). Letters indicate statistical significance (P<0.05) as analyzed by Duncan’s multiple range test.
Colon weight and length
Colon length was decreased in DSS-treated mice after 7 days of treatment. Administration of a high dosage of EC extract or Curcumin significantly (P<0.05) attenuated colon shortening (Fig 4a). In addition, both treatments also resulted in decreased colon weight per length ratio (Fig 4b) and reduced splenic weight (Fig 4c). Fig 4d shows a representative colon for each group.
Fig 4. Effects of EC extract treatment on colon health after 7 days of treatment: (a) colon length, (b) colon weight/length ratio, (c) splenic weight, (d) representative colons for each group.
Data are shown as the mean ± S.D. (n = 8). Letters indicate statistical significance (P<0.05) as analyzed by Duncan’s multiple range test.
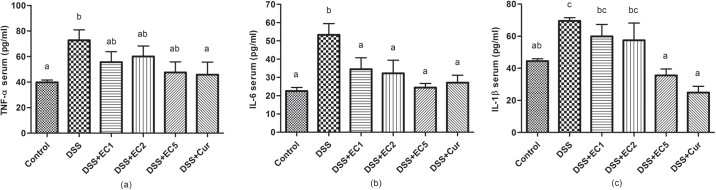
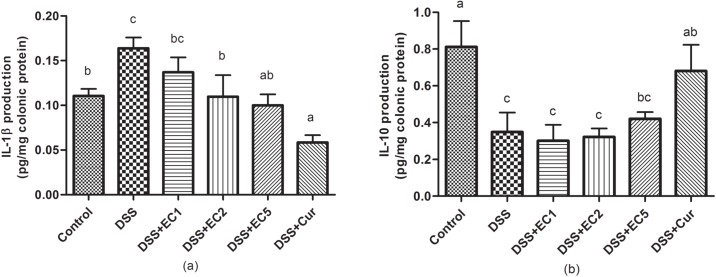
Inflammatory cytokines
After DSS treatment, pro-inflammatory cytokine levels (e.g., TNF-α, IL-1β, and IL-6) were significantly (P<0.05) increased relative to control mice (Fig 5a and 5b). Treatment with EC extract or Curcumin reduced TNF-α, IL-1β, and IL-6 levels in serum. In addition, EC extracts also significantly (P<0.05) reduced IL-1β expression in colon tissues (Fig 6a). IL-10 expression was high in healthy mice and decreased in DSS-treated mice. Treatment with EC extract or Curcumin both regulated IL-10 expression in colon tissue (Fig 6b).
Fig 5. Effects of EC extract on inflammatory cytokine expression in serum after 7 days of treatment: (a) TNF-α, (b) IL-6, and (c) IL-1β.
Data are shown as the mean ± S.D. (n = 8). Letters indicate statistical significance (P<0.05) as analyzed by Duncan’s multiple range test.
Fig 6. Effects of EC extract on inflammatory cytokine expression in colon tissue after 7 days of treatment: (a) IL-1β and (b) IL-10.
Data are shown as the mean ± S.D. (n = 8). Letters indicate statistical significance (P<0.05) as analyzed by Duncan’s multiple range test.
Colonic histopathology
Under hematoxylin and eosin (H&E) observation, the normal colon shows good wall layer architecture and no loss of crypt cells (Score 0). However, DSS-treated mice presented thicker mucosal layers accompanied by erosion (Score 4, Fig 7). After treatment with EC extract (especially high doses) or Curcumin, crypt cell loss was ameliorated (Score 1).
Fig 7. Representative colonic tissue histopathology for each group after 7 days of treatment.
Discussion
Inflammatory bowel diseases, including Crohn’s disease and ulcerative colitis, can be recognized by intestinal inflammation [34]. Various animal models have been developed for studying IBD pathogenesis, including dextran sodium sulfate (DSS), trinitrobenzene sulfonic acid (TNBS), oxazolone, acetic acid, carrageenan, indomethacin (a non-steroidal anti-inflammatory drug [NSAID]), and peptidoglycan-polysaccharide induced models [32]. DSS administration in the drinking water is a commonly used method for inducing colitis in mice owing to its simplicity, reproducibility, controllability, and rapidity. DSS dosages given to BALB/c mice have ranged between 2.5–5.0% [34].
Body weight decreased in mice with DSS-induced colitis, with EC extract or Curcumin administration both helping to attenuate this body weight loss (Fig 3a). In addition, the disease activity index scores were also increased in mice with colitis (Fig 3b). These results are in accordance with previous studies [34, 35, 45]. Colitis induced by DSS was associated with acute histological changes such as weight loss, diarrhea, and rectal bleeding, resulting in increased disease activity index scores. The oral administration of either EC extract or Curcumin alleviated disease activity index scores in DSS-treated mice. Colitis was also characterized by colon shortening (Fig 4a and 4c) and increased colon weight/length ratios (Fig 4b), with EC extract or Curcumin treatment preventing this increase in colon weight. Overall, treatment with EC extract or Curcumin ameliorated the clinical signs and symptoms of colitis induced in mice by DSS.
Molecular observations supported the beneficial effects of EC extract and Curcumin, as treatment with either reduced the levels of pro-inflammatory cytokines such as TNF-α, IL-1β, and IL-6 in DSS-treated mouse sera. In contrast, untreated DSS-mice showed increased expression levels of these cytokines (Fig 5). TNF-α, IL-6, and IFN-γ are the main inflammatory mediators in murine colitis models [35, 48]. TNF signaling has been found to induce the pleiotropic pro-inflammatory effects of colitis, including the activation of effector T cells and macrophages. TNF signaling also directed intestine epithelial cell (ICE) damage via myosin light chain kinase (MLCK) activation [49, 50]. Increased IL-6 production by the lamina propria and CD4+ T cells has been reported in experimental colitis models [51]. A recent study reported that the administration of anti-TNF-α may be a strategy for managing colitis [52]. Colitis can also be prevented by regulating IL-10 expression [49, 53]. The present study showed that in DSS-treated mice, IL-10 expression in colon tissues was lower than in animals treated with EC extract or Curcumin (Fig 6b). A previous study has also reported that untreated IL-10 gene-deficient mice showed progressive histopathological injury, increased colon weight/length ratios, and elevated IFN-γ and IL-17 expression [54]. Colitis severity is related to colonic damage severity. Here, untreated mice presented thicker mucosal layers and erosion. EC extract or Curcumin treatment both reduced histopathological score severity and resulted in a high number of crypt cells in the mucosal layer (Fig 7). A previous study has reported that mice treated with 5% DSS presented mucosal thickness and epithelial injury as well as increased microscopic damage scores [45].
Red seaweeds are mostly composed of sulfated galactans such as carrageenan and agar [15], which are made up of repeating disaccharide units of alternating 3-linked β-D-galactopyranose and 4-linked α-D-galactopyranose or 4-linked 3,6-anhydro-α-D-galactopyranose. These can be extracted from red seaweeds (Rhodophyta) such as Eucheuma, Hypnea, Gigartina, and Chondrus crispus [55, 56]. Dietary fibers include polysaccharides, oligosaccharides, lignins, and other compounds associated with plant substances. Dietary fiber, as edible parts of plants or analogous carbohydrates, are resistant to digestion and absorption in the human small intestine, resulting in complete or partial fermentation in the large intestine [57]. A recent review reported that dietary fermented oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAP) possessed beneficial effects for IBD patients by reducing levels of the pro-inflammatory markers C-reactive protein and fecal calprotein [58].
The EC extract has shown antioxidant, anti-inflammation, and anti-cancer properties [26, 27, 59, 60], and has previously been demonstrated to slow tumor cell growth rate [27], promote wound healing [28], and upregulate cancer cell apoptosis [29]. Moreover, extracts of this seaweed improved cardiovascular, liver, and metabolic parameters in obese rat models [30] and presented anti-diabetic effects in streptozotocin-induced type 2 diabetic mice [31].
Used in this study as a positive control, Curcumin has been demonstrated to prevent colitis by suppressing NF-κB [61] and inhibiting STAT3 signaling [62]. In addition, Curcumin can also modulate certain inflammatory mediators such as TNF-α and nitric oxide [63]. Future work should focus on microbiota variation in murine intestines, as previous studies have reported that the gut microbiota is altered in cases of IBD [64, 65].
Conclusions
Here, a Eucheuma cottonii ethanol (EC) extract has demonstrated suppressive effects on colonic disease induced by DSS in mice. EC extract treatment reduced weight loss and disease activity index scores, as well as regulating the levels of pro-inflammatory cytokines such as TNF-α, IL-6, and IL-1β. EC extract administration also reduced colon injury in DSS-treated mice. As such, the dietary polysaccharides found in the E. cottonii extract may be used for the future treatment of colitis.
Acknowledgments
The sponsor had no role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript and the decision to submit the manuscript for publication.
Data Availability
All relevant data are within the manuscript.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Bitencourt MAO, Silva HMD, Abílio GMF, Miranda GEC, Moura AMA, de Araújo-Júnior JX, et al. Anti-inflammatory Effects of Methanolic Extract of Green Algae Caulerpa mexicana in a Murine Model of Ulcerative Colitis. Revista Brasileira de Farmacognosia. 2015;25(6):677–82. 10.1016/j.bjp.2015.10.001 [DOI] [Google Scholar]
- 2.Cosnes J, Gower–Rousseau C, Seksik P, Cortot A. Epidemiology and Natural History of Inflammatory Bowel Diseases. Gastroenterology. 2011;140(6):1785–94. 10.1053/j.gastro.2011.01.055 [DOI] [PubMed] [Google Scholar]
- 3.Hendrickson BA, Gokhale R, Cho JH. Clinical Aspects and Pathophysiology of Inflammatory Bowel Disease. Clinical Microbiology Reviews. 2002;15(1):79–94. 10.1128/CMR.15.1.79-94.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, et al. Increasing Incidence and Prevalence of the Inflammatory Bowel Diseases With Time, Based on Systematic Review. Gastroenterology. 2012;142(1):46–54.e42. 10.1053/j.gastro.2011.10.001 [DOI] [PubMed] [Google Scholar]
- 5.Kaplan GG. The Global Burden of IBD: from 2015 to 2025. Nature Reviews Gastroenterology & Hepatology. 2015;12(12):720–7. 10.1038/nrgastro.2015.150 [DOI] [PubMed] [Google Scholar]
- 6.Lean QY, Eri RD, Fitton JH, Patel RP, Gueven N. Fucoidan Extracts Ameliorate Acute Colitis. Plos One. 2015;10(6):e0128453 10.1371/journal.pone.0128453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cho E-j, Shin J-S, Noh Y-S, Cho Y-W, Hong S-J, Park J-H, et al. Anti-inflammatory Effects of Methanol Extract of Patrinia scabiosaefolia in Mice with Ulcerative Colitis. Journal of Ethnopharmacology. 2011;136(3):428–35. 10.1016/j.jep.2010.04.047 [DOI] [PubMed] [Google Scholar]
- 8.Triantafillidis J, Merikas E, Georgopoulos F. Current and Emerging Drugs for The Treatment of Inflammatory Bowel Disease. Drug Design, Development and Therapy. 2011;5:185–210. 10.2147/DDDT.S11290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.D’Orazio N, Gammone MA, Gemello E, De Girolamo M, Cusenza S, Riccioni G. Marine Bioactives: Pharmacological Properties and Potential Applications against Inflammatory Diseases. Marine Drugs. 2012;10(12):812–33. 10.3390/md10040812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brito TV, Barros FCN, Silva RO, Dias GJ Júnior, C. JS Júnior, Franco ÁX, et al. Sulfated Polysaccharide from the Marine Algae Hypnea musciformis inhibits TNBS-induced Intestinal Damage in Rats. Carbohydrate Polymers. 2016;151:957–64. 10.1016/j.carbpol.2016.06.047 [DOI] [PubMed] [Google Scholar]
- 11.De Souza ÉT, Pereira de Lira D, Cavalcanti de Queiroz A, Costa da Silva DJ, Bezerra de Aquino A, Campessato Mella E, et al. The Antinociceptive and Anti-Inflammatory Activities of Caulerpin, a Bisindole Alkaloid Isolated from Seaweeds of the Genus Caulerpa. Marine Drugs. 2009;7(4):689–704. 10.3390/md7040689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.da Matta CBB, De Souza ÉT, De Queiroz AC, De Lira DP, De Araújo MV, Cavalcante-Silva LHA, et al. Antinociceptive and Anti-Inflammatory Activity from Algae of the Genus Caulerpa. Marine Drugs. 2011;9(12):307–18. 10.3390/md9030307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Torres FAE, Passalacqua TG, Velásquez AMA, de Souza RA, Colepicolo P, Graminha MAS. New Drugs with Antiprotozoal Activity from Marine Algae: A Review. Revista Brasileira de Farmacognosia. 2014;24(3):265–76. 10.1016/j.bjp.2014.07.001 [DOI] [Google Scholar]
- 14.Gómez-Ordóñez E, Jiménez-Escrig A, Rupérez P. Dietary fibre and physicochemical properties of several edible seaweeds from the northwestern Spanish coast. Food Research International. 2010;43(9):2289–94. 10.1016/j.foodres.2010.08.005 [DOI] [Google Scholar]
- 15.Jiménez-Escrig A, Sánchez-Muniz FJ. Dietary fibre from edible seaweeds: Chemical structure, physicochemical properties and effects on cholesterol metabolism. Nutrition Research. 2000;20(4):585–98. 10.1016/s0271-5317(00)00149-4 [DOI] [Google Scholar]
- 16.Galvez J, Rodríguez-Cabezas ME, Zarzuelo A. Effects of dietary fiber on inflammatory bowel disease. Molecular Nutrition & Food Research. 2005;49(6):601–8. 10.1002/mnfr.200500013 [DOI] [PubMed] [Google Scholar]
- 17.Rodríguez-Cabezas ME, Gálvez J, Lorente MD, Concha A, Camuesco De, Azzouz S, et al. Dietary Fiber Down-Regulates Colonic Tumor Necrosis Factor α and Nitric Oxide Production in Trinitrobenzenesulfonic Acid-Induced Colitic Rats. The Journal of Nutrition. 2002;132(11):3263–71. 10.1093/jn/132.11.3263 [DOI] [PubMed] [Google Scholar]
- 18.Koh A, De Vadder F, Kovatcheva-Datchary P, Bäckhed F. From Dietary Fiber to Host Physiology: Short-Chain Fatty Acids as Key Bacterial Metabolites. Cell. 2016;165(6):1332–45. 10.1016/j.cell.2016.05.041 [DOI] [PubMed] [Google Scholar]
- 19.Makki K, Deehan EC, Walter J, Bäckhed F. The Impact of Dietary Fiber on Gut Microbiota in Host Health and Disease. Cell Host & Microbe. 2018;23(6):705–15. 10.1016/j.chom.2018.05.012 [DOI] [PubMed] [Google Scholar]
- 20.Kumar KS, Ganesan K, Rao PVS. Antioxidant potential of solvent extracts of Kappaphycus alvarezii (Doty) Doty—An edible seaweed. Food Chem. 2008;107(1):289–95. 10.1016/j.foodchem.2007.08.016 [DOI] [Google Scholar]
- 21.Liang W, Mao X, Peng X, Tang S. Effects of sulfate group in red seaweed polysaccharides on anticoagulant activity and cytotoxicity. Carbohydrate Polymers. 2014;101:776–85. 10.1016/j.carbpol.2013.10.010 [DOI] [PubMed] [Google Scholar]
- 22.Abu-Bakar NA, Anyanji VU, Mustapha NM, Lim S-L, Mohamed S. Seaweed (Eucheuma cottonii) reduced inflammation, mucin synthesis, eosinophil infiltration and MMP-9 expressions in asthma-induced rats compared to Loratadine. Journal of Functional Foods. 2015;19:710–22. 10.1016/j.jff.2015.10.011 [DOI] [Google Scholar]
- 23.Matanjun P, Mohamed S, Mustapha NM, Muhammad K, Ming CH. Antioxidant activities and phenolics content of eight species of seaweeds from North Borneo. Journal of Applied Phycology. 2008;20(4):367–73. 10.1007/s10811-007-9264-6 [DOI] [Google Scholar]
- 24.Namvar F, Mohamed S, Fard SG, Behravan J, Mustapha NM, Alitheen NBM, et al. Polyphenol-rich seaweed (Eucheuma cottonii) extract suppresses breast tumour via hormone modulation and apoptosis induction. Food Chem. 2012;130(2):376–82. 10.1016/j.foodchem.2011.07.054 [DOI] [Google Scholar]
- 25.Fayaz M, Namitha KK, Murthy KNC, Swamy MM, Sarada R, Khanam S, et al. Chemical Composition, Iron Bioavailability, and Antioxidant Activity ofKappaphycus alvarezzi(Doty). Journal of Agricultural and Food Chemistry. 2005;53(3):792–7. 10.1021/jf0493627 [DOI] [PubMed] [Google Scholar]
- 26.Lim CL, Koh RY, Haw TY, Boudville LA, Boudville LA, Boudville LA. Antioxidant Activity of the Sea Bird Nest (Eucheuma cottonii) and Its Radical Scavenging Effect on Human Keratinocytes. Journal of Medical and Bioengineering. 2015;4(6):461–5. doi: 10.12720/jomb.4.6.461-465 [Google Scholar]
- 27.Chang V-S, Okechukwu PN, Teo S-S. The properties of red seaweed (Kappaphycus alvarezii) and its effect on mammary carcinogenesis. Biomedicine & Pharmacotherapy. 2017;87:296–301. 10.1016/j.biopha.2016.12.092 [DOI] [PubMed] [Google Scholar]
- 28.Fard SG, Shamsabadi FT, Emadi M, Meng GY, Muhammad K, Mohamed S. Ethanolic Extract of Eucheuma cottonii Promotes in vivo Hair Growth and Wound Healing. Jownal of Animal and Veterinary Advances. 2011;10(5):601–5. [Google Scholar]
- 29.Abu-Bakar NA, Mohamed S, Ibrahim TAT, Shalan NAM. Changes in rats’ breast tumor ultrastructure and immune and messenger RNA responses caused by dietary Seaweed (Kappaphycus alvarezii) extract. Journal of Microscopy and Ultrastructure. 2017;5(2):70–81. 10.1016/j.jmau.2016.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wanyonyi S, du Preez R, Brown L, Paul N, Panchal S. Kappaphycus alvarezii as a Food Supplement Prevents Diet-Induced Metabolic Syndrome in Rats. Nutrients. 2017;9(11):1261 10.3390/nu9111261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee J, Wang J, Sen TS. Antidiabetic effect of Kappaphycus alvarezii extracts on streptozotocin-induced Type II Diabetic ICR Mice. Annals of Pharmacology and Pharmaceutics. 2017;2(10):1056. [Google Scholar]
- 32.Randhawa PK, Singh K, Singh N, Jaggi AS. A Review on Chemical-Induced Inflammatory Bowel Disease Models in Rodents. The Korean Journal of Physiology & Pharmacology. 2014;18(4):279–88. 10.4196/kjpp.2014.18.4.279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Park YH, Kim N, Shim YK, Choi YJ, Nam RH, Choi YJ, et al. Adequate Dextran Sodium Sulfate-induced Colitis Model in Mice and Effective Outcome Measurement Method. Journal of Cancer Prevention. 2015;20(4):260–7. doi: 10.15430/JCP.2015.20.4.260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chassaing B, Aitken JD, Malleshappa M, Vijay-Kumar M. Dextran Sulfate Sodium (DSS)-Induced Colitis in Mice. Current Protocols in Immunology. 2015;104:15.25.1–15.25.14. 10.1002/0471142735.im1525s104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jeon Y-D, Kang S-H, Bang K-S, Chang Y-N, Lee J-H, Jin J-S. Glycyrrhetic Acid Ameliorates Dextran Sulfate Sodium-Induced Ulcerative Colitis in Vivo. Molecules. 2016;21(4):523 10.3390/molecules21040523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hwang E-S, Nhuan DT. Effects of Extraction and Processing Methods on Antioxidant Compound Contents and Radical Scavenging Activities of Laver (Porphyra tenera). Preventive Nutrition and Food Science. 2014;19(1):40–8. 10.3746/pnf.2014.19.1.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yaphe W. Colorimetric Determination of 3,6-Anhydrogalactose and Galactose in Marine Algal Polysaccharides. Analytical Chemistry. 1960;32(10):1327–30. 10.1021/ac60166a030 [DOI] [Google Scholar]
- 38.Matsuhiro B, Zanlungo AB. Colorimetric Determination of 3,6-anhydrogalactose in Polysaccharides from Red Seaweeds. Carbohydrate Research. 1983;118:276–9. 10.1016/0008-6215(83)88056-2 [DOI] [Google Scholar]
- 39.van de Loosdrecht AA, Beelen RHJ, Ossenkoppele GJ, Broekhoven MG, Langenhuijsen MMAC. A tetrazolium-based colorimetric MTT assay to quantitate human monocyte mediated cytotoxicity against leukemic cells from cell lines and patients with acute myeloid leukemia. Journal of Immunological Methods. 1994;174(1–2):311–20. 10.1016/0022-1759(94)90034-5 [DOI] [PubMed] [Google Scholar]
- 40.Soriano A, Salas A, Salas A, Sans M, Gironella M, Elena M, et al. VCAM-1, but Not ICAM-1 or MAdCAM-1, Immunoblockade Ameliorates DSS-Induced Colitis in Mice. Laboratory Investigation. 2000;80(10):1541–51. 10.1038/labinvest.3780164 [DOI] [PubMed] [Google Scholar]
- 41.Gommeaux J, Cano C, Garcia S, Gironella M, Pietri S, Culcasi M, et al. Colitis and Colitis-Associated Cancer Are Exacerbated in Mice Deficient for Tumor Protein 53-Induced Nuclear Protein 1. Molecular and Cellular Biology. 2007;27(6):2215–28. 10.1128/MCB.01454-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kim S-J, Kim M-C, Um J-Y, Hong S-H. The Beneficial Effect of Vanillic Acid on Ulcerative Colitis. Molecules. 2010;15(10):7208–17. 10.3390/molecules15107208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abdelali A, Al-Bader M, Kilarkaje N. Effects of Trans-Resveratrol on hyperglycemia-induced abnormal spermatogenesis, DNA damage and alterations in poly (ADP-ribose) polymerase signaling in rat testis. Toxicology and Applied Pharmacology. 2016;311:61–73. 10.1016/j.taap.2016.09.023 [DOI] [PubMed] [Google Scholar]
- 44.Kitajima S, Takuma S, Morimoto M. Histological Analysis of Murine Colitis Induced by Dextran Sulfate Sodium of Different Molecular Weights. Experimental Animals. 2000;49(1):9–15. 10.1538/expanim.49.9 [DOI] [PubMed] [Google Scholar]
- 45.Kim D-S, Ko J-H, Jeon Y-D, Han Y-H, Kim H-J, Poudel A, et al. Ixeris dentata NAKAI Reduces Clinical Score and HIF-1 Expression in Experimental Colitis in Mice. Evidence-Based Complementary and Alternative Medicine. 2013;2013:1–9. 10.1155/2013/671281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hamamoto Maemura, Hirata Murano, Sasaki Katsu. Inhibition of dextran sulphate sodium (DSS)-induced colitis in mice by intracolonically administered antibodies against adhesion molecules (endothelial leucocyte adhesion molecule-1 (ELAM-1) or intercellular adhesion molecule-1 (ICAM-1)). Clinical and Experimental Immunology. 1999;117(3):462–8. 10.1046/j.1365-2249.1999.00985.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Namvar F, Baharara J, Mahdi AA. Antioxidant and Anticancer Activities of Selected Persian Gulf Algae. Indian Journal of Clinical Biochemistry. 2013;29(1):13–20. 10.1007/s12291-013-0313-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Myers KJ, Murthy S, Flanigan A, Witchell DR, Butler M, Murray S, et al. Antisense Oligonucleotide Blockade of Tumor Necrosis Factor-alpha in Two Murine Models of Colitis. Journal of Pharmacology and Experimental Therapeutics. 2003;304(1):411–24. 10.1124/jpet.102.040329 [DOI] [PubMed] [Google Scholar]
- 49.Neurath MF. Cytokines in Inflammatory Bowel Disease. Nature Reviews Immunology. 2014;14(5):329–42. 10.1038/nri3661 [DOI] [PubMed] [Google Scholar]
- 50.Su L, Nalle SC, Shen L, Turner ES, Singh G, Breskin LA, et al. TNFR2 Activates MLCK-Dependent Tight Junction Dysregulation to Cause Apoptosis-Mediated Barrier Loss and Experimental Colitis. Gastroenterology. 2013;145(2):407–15. 10.1053/j.gastro.2013.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kai Y, Takahashi I, Ishikawa H, Hiroi T, Mizushima T, Matsuda C, et al. Colitis in mice lacking the common cytokine receptor γ chain is mediated by IL-6-producing CD4+ T cells. Gastroenterology. 2005;128(4):922–34. 10.1053/j.gastro.2005.01.013 [DOI] [PubMed] [Google Scholar]
- 52.Pugliese D, Felice C, Papa A, Gasbarrini A, Rapaccini GL, Guidi L, et al. Anti TNF-α therapy for ulcerative colitis: current status and prospects for the future. Expert Review of Clinical Immunology. 2016;13(3):223–33. 10.1080/1744666X.2017.1243468 [DOI] [PubMed] [Google Scholar]
- 53.Li M-C, He S-H. IL-10 and its related cytokines for treatment of inflammatory bowel disease. World Journal of Gastroenterology. 2004;10(5):620–5. 10.3748/wjg.v10.i5.620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ung VYL, Foshaug RR, MacFarlane SM, Churchill TA, Doyle JSG, Sydora BC, et al. Oral Administration of Curcumin Emulsified in Carboxymethyl Cellulose Has a Potent Anti-inflammatory Effect in the IL-10 Gene-Deficient Mouse Model of IBD. Digestive Diseases and Sciences. 2009;55(5):1272–7. 10.1007/s10620-009-0843-z [DOI] [PubMed] [Google Scholar]
- 55.Campo VL, Kawano DF, Silva DBd, Carvalho I. Carrageenans: Biological properties, chemical modifications and structural analysis—A review. Carbohydrate Polymers. 2009;77(2):167–80. 10.1016/j.carbpol.2009.01.020 [DOI] [Google Scholar]
- 56.Ghani NAA, Othaman R, Ahmad A, Anuar FH, Hassan NH. Impact of purification on iota carrageenan as solid polymer electrolyte. Arabian Journal of Chemistry. 2018. 10.1016/j.arabjc.2018.06.008 [DOI] [Google Scholar]
- 57.Dhingra D, Michael M, Rajput H, Patil RT. Dietary fibre in foods: a review. Journal of Food Science and Technology. 2011;49(3):255–66. 10.1007/s13197-011-0365-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Barbalho SM, Goulart RdA, Aranão ALdC, de Oliveira PGC. Inflammatory Bowel Diseases and Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols: An Overview. Journal of Medicinal Food. 2018;21(7):633–40. 10.1089/jmf.2017.0120 [DOI] [PubMed] [Google Scholar]
- 59.Raman M, Doble M. κ-Carrageenan from Marine Red Algae, Kappaphycus alvarezii—A Functional Food to Prevent Colon Carcinogenesis. Journal of Functional Foods. 2015;15:354–64. 10.1016/j.jff.2015.03.037 [DOI] [Google Scholar]
- 60.Shamsabadi FT, Khoddami A, Fard SG, Abdullah R, Othman HH, Mohamed S. Comparison of Tamoxifen with Edible Seaweed (Eucheuma cottonii L.) Extract in Suppressing Breast Tumor. Nutrition and Cancer. 2013;65(2):255–62. 10.1080/01635581.2013.756528 [DOI] [PubMed] [Google Scholar]
- 61.Brumatti LV, Marcuzzi A, Tricarico P, Zanin V, Girardelli M, Bianco A. Curcumin and Inflammatory Bowel Disease: Potential and Limits of Innovative Treatments. Molecules. 2014;19(12):21127–53. 10.3390/molecules191221127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yang J-Y, Zhong X, Yum H-W, Lee H-J, Kundu JK, Na H-K, et al. Curcumin Inhibits STAT3 Signaling in the Colon of Dextran Sulfate Sodium-treated Mice. Journal of Cancer Prevention. 2013;18(2):186–91. doi: 10.15430/JCP.2013.18.2.186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Arafa HMM, Hemeida RA, El-Bahrawy AIM, Hamada FMA. Prophylactic role of curcumin in dextran sulfate sodium (DSS)-induced ulcerative colitis murine model. Food and Chemical Toxicology. 2009;47(6):1311–7. 10.1016/j.fct.2009.03.003 [DOI] [PubMed] [Google Scholar]
- 64.Ilott NE, Bollrath J, Danne C, Schiering C, Shale M, Adelmann K, et al. Defining the microbial transcriptional response to colitis through integrated host and microbiome profiling. The ISME Journal. 2016;10(10):2389–404. 10.1038/ismej.2016.40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rooks MG, Veiga P, Wardwell-Scott LH, Tickle T, Segata N, Michaud M, et al. Gut microbiome composition and function in experimental colitis during active disease and treatment-induced remission. The ISME Journal. 2014;8(7):1403–17. 10.1038/ismej.2014.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the manuscript.