Abstract
While there have been gains in the overall quality of health care, racial and ethnic disparities in health outcomes continue to persist in the United States. The Learning Health System (LHS) has the potential to significantly improve health care quality using patient‐centered design, data analytics, and continuous improvement. To ensure that health disparities are also being addressed, targeted approaches must be used. This document sets forth a practical framework to incorporate health equity into a developing LHS. Using a case study approach, the framework is applied to 2 projects focused on the reduction of health disparities to highlight its application.
Keywords: health equity, health information technology, social determinants of health
1. BACKGROUND
Despite improvements in overall health care quality, inequities in health outcomes persist.1 The World Health Organization (WHO) defines health inequities as “avoidable” differences in health between population groups caused by differences such as social and economic conditions.2 Health disparities have been associated with individual‐level factors such as race, ethnicity, gender and gender identity, sexual orientation, disability, and socioeconomic status.
In addition to being morally unacceptable, health inequities are costly, both financially and in terms of mortality and quality of life.3, 4 Life expectancy varies as much as 30 years between the richest and poorest US counties.5 Between 2003 and 2006, the elimination of racial and ethnic health disparities is estimated to have saved $230 billion in direct medical expenditures and over $1 trillion in indirect costs.6 Elimination of the black‐white mortality gap would have prevented approximately 83 570 excess deaths in 2002.7 And while health disparities continue to be prevalent, they can be eliminated. From 1990 to 2000, 10 US counties either sustained or moved toward equitable breast cancer mortality rates between black and white women.8 In addition, significant improvements in black‐white infant mortality rates were made in the last decade, with 30 states demonstrating a reduction of the gap.9
The mechanisms required to move towards equity are multifaceted and often unique to a given community due to differing resources, cultures, and priorities.10 Many of these factors can be described using the umbrella term “social determinants of health” (SDH), which involve the conditions in which people are born, grow, work, live, and age.11 The SDH include factors like the built environment and access to health care, education, healthy foods, and jobs.12Efforts to reduce health disparities have traditionally focused on the health care system, despite evidence that health care services impact only 10% of the risk for premature death.13 In fact, social, environmental factors, and individual behavior, which contribute a combined 60% to premature death and are heavily intertwined with the SDH, go underfunded and often unaddressed nationally and specifically in health care settings.14
Quality improvement (QI) initiatives dominate the literature, clinical settings, and policy discourse. However, improving overall quality does not directly translate to reducing health disparities.15 Moreover, QI interventions focused on the general population may exacerbate existing disparities if the population with higher quality outcomes at baseline also have higher uptake and/or effectiveness of the intervention.16 Targeted approaches focused on meeting the needs of diverse populations and on addressing the SDH have been proven to be effective.17, 18 For example, racial and ethnic disparities in childhood vaccine rates were significant in the 1980s, but dual strategies to reach both the general population and additional approaches focused on reaching minority and underserved children were effective in eliminating the disparity by the mid‐1990s.19
The evolution and expansion of learning health systems (LHS) provide significant opportunities for the advancement of health equity. The purpose of this paper is to demonstrate the overlap of the LHS model with health equity, set forth a practical framework for integrating health equity into LHS, and to demonstrate how this framework applies using two case studies.
2. HEALTH EQUITY IS EMBEDDED IN THE LEARNING HEALTH SYSTEM VALUES
The mission of LHS is a truly integrated health system “in which progress in science, informatics, and care culture align to generate new knowledge as an ongoing, natural by‐product of the care experience, and seamlessly refine and deliver best practices for continuous improvement in health and health care.”20 To accomplish this mission, 10 core values have been developed that present a gold standard approach for the adoption of a national, patient‐centered LHS.21 The alignment of LHS with health equity becomes clear through the application of a health equity lens to the 10 core LHS values (Table 1).
Table 1.
Alignment of the LHS core values with health equity
| LHS Core Value | LHS Core Value Description | Alignment with Health Equity |
|---|---|---|
| Person‐focused care | The LHS will protect and improve the health of individuals by informing choices about health and health care. The LHS will do this by enabling strategies that engage individuals, families, groups, communities, and the general population, as well as the United States health care system as a whole. | To ensure person‐focused care that includes individuals, families and communities from diverse backgrounds, culturally competent strategies that address SDH, health literacy, and other unique factors may be needed. The role of these factors, especially the role SDH play within a community, should not be underestimated, as interventions effective within one community or patient population may not work in others. |
| Privacy | The LHS will protect the privacy, confidentiality, and security of all data to enable responsible sharing of data, information, and knowledge, as well as to build trust among all stakeholders. | Data privacy and security is important to populations experiencing health disparities and to build trust among these stakeholders; they should be involved in decisions around privacy and security to the extent possible. |
| Inclusiveness | Every individual and organization committed to improving the health of individuals, communities, and diverse populations, who abides by the governance of the LHS, is invited and encouraged to participate. | Community and individual participation is critical to eliminating health disparities. In the context of LHS, active participation may necessitate going beyond invitation and encouragement, to overcoming the SDH, which can pose barriers to participation. Receiving buy‐in from well‐respected community leaders can facilitate the building of trust needed to engage the community. |
| Transparency | With a commitment to integrity, all aspects of LHS operations will be open and transparent to safeguard and deepen the trust of all stakeholders in the system, as well as to foster accountability. | Due to historical abuses of minorities and vulnerable populations, mistrust of health care and research institutions may require intentional strategies to engage these communities and demonstrate the integrity and transparency embedded in this core value. |
| Accessibility | All should benefit from the public good derived from the LHS. Therefore, the LHS should be available and should deliver value to all, while encouraging and incentivizing broad and sustained participation. | Accessibility to advancing health equity should be executed in different ways to reach different audiences, understanding that diverse communities have different needs. The SDH and community engagement also play a significant role in operationalizing this value, as accessibility cannot be determined by those providing access, but must be measured by those attempting to access. |
| Adaptability | The LHS will be designed to enable iterative, rapid adaptation, and incremental evolution to meet current and future needs of stakeholders. | Continuous data collection, including stratification by racial and ethnic subgroups, the SDH, and other disparity variables is the best way to monitor disparities and to adapt strategies to address them. Demographic and social factors should be routinely and systematically integrated into all analytics and decision‐making processes. |
| Governance | The LHS will have that governance, which is necessary to support its sustainable operation, to set required standards, to build and maintain trust on the part of all stakeholders, and to stimulate ongoing innovation. | Governance structures should ensure that sustainability measures and standards are inclusive of the needs of minority and underserved populations and targeted to reduce health disparities. Sustainability will require buy‐in from the community, which is achieved through inclusion of the community in governance structures. |
| Cooperative and participatory leadership | The leadership of the LHS will be a multistakeholder collaboration across the public and private sectors including patients, consumers, caregivers, and families, in addition to other stakeholders. Diverse communities and populations will be represented. Bold leadership and strong user participation are essential keys to unlocking the potential of the LHS. | Intentional inclusion of minority patients, consumers, caregivers, and families is essential to a participatory structure that will reduce health disparities. In addition, ensuring that SDH do not pose a barrier to participation. Examples may include evening and/or weekend meetings so participants do not have to take time off work, compensation and child care, holding meetings in locations convenient to public transportation. |
| Scientific integrity | The LHS and its participants will share a commitment to the most rigorous application of science to ensure the validity and credibility of findings, and the open sharing and integration of new knowledge in a timely and responsible manner. | The existence of health disparities associated with many different health outcomes is demonstrated by a strong evidence base. However, the science on the elimination of health disparities is less clear, constantly evolving and unique to individual patient populations and communities. Therefore, it is even more critical that LHS prioritize the identification of best practices and to continuously evaluate effectiveness of targeted health disparity interventions. |
| Value | The LHS will support learning activities that can serve to optimize both the quality and affordability of health care. The LHS will be efficient and seek to minimize financial, logistical, and other burdens associated with participation. | The costs of health disparities are significant, with regard to financial burden on individuals and the health care system, loss of productivity, and early death. LHS that address health inequities will provide value to individuals and the system. |
3. INTEGRATING HEALTH EQUITY INTO THE LHS: THE PETAL FRAMEWORK
Despite the clear alignment of the core LHS values with health equity, a gap remains between theory and practice. To not only recognize health equity but also to achieve it, clear and practical methods for integrating health equity into existing and developing LHS are needed. We have undertaken the first step towards this goal by developing a practical framework that is grounded in community partnership and incorporates supportive technology, SDH, and sustainability. The PETAL framework was developed to work in parallel with LHS core values and provide practical and actionable steps that all potential stakeholders in a LHS can effectively implement to improve health equity (Figure 1). We envision this framework to be applicable to any level of the LHS, from the individual clinician to programs spanning single organizations to multi‐institutional systems.
Figure 1.
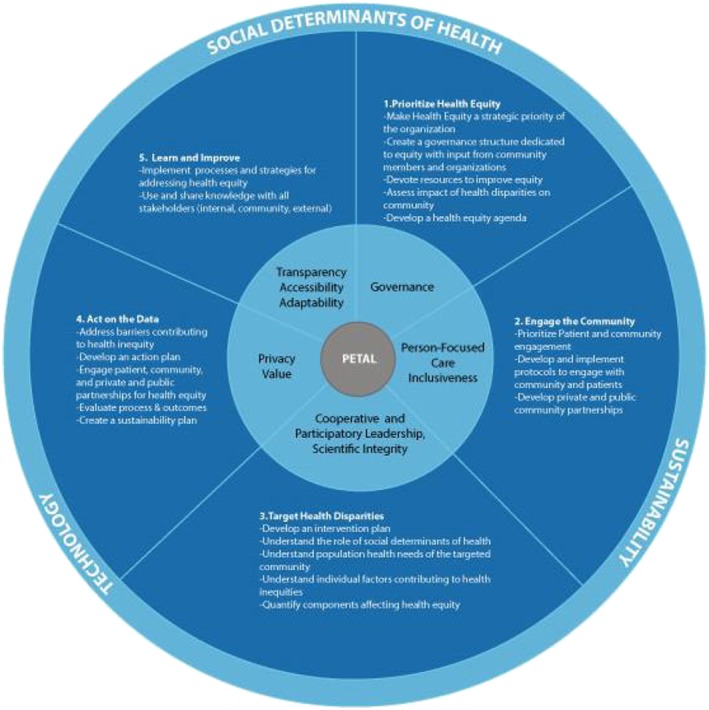
The PETAL Framework for integrating health equity into Learning Health Systems.
In developing the PETAL framework, we closely reviewed and synthesized several existing health equity frameworks and aligned them with the LHS core values to establish the PETAL key components.22, 23, 24, 25, 26 The core components of the proposed framework include the following: Prioritize health equity; Engage the community; Target health disparities; Act on the data; and Learn and improve (PETAL). Two factors set the PETAL framework apart from other health equity frameworks: (1) alignment with LHS core values and (2) the community‐driven approach that provides the foundation and runs throughout all core components.
4. OVERARCHING ELEMENTS OF THE PETAL FRAMEWORK
Three overarching elements are embedded in each of the PETAL core components: SDH, sustainability, and technology. Common examples of the negative impact of SDH include a diabetic's desire to eat healthier that is restricted by distance to a grocery store, which may be exacerbated by lack of transportation; a parent's work shift and lack of paid leave, which hinders his daughter's regular asthma checkups; or a senior on a fixed income deciding to purchase food instead of medication. These examples demonstrate the impact of SDH yet also highlight mechanisms to address them. However, clinicians remain unaware of the role of SDH in their patients' lives unless they specifically ask questions about them. Effective interventions to reduce the impact of SDH on poor health outcomes depend on systematic collection and analysis of this data. Using community‐level data on SDH, health care providers may decide to locate close to public transportation or provide extended or weekend clinic hours or Medicaid programs may provide transportation services for enrollees.
Technology and data analytics are rapidly advancing and play a major role in LHS and the elimination of health disparities.27, 28 Real‐time clinical, community, and patient‐reported data are the foundation for continuous improvement in LHS. Electronic health records (EHR), health information exchanges, mobile health applications, telemedicine, home monitoring, and clinical data registries are providing an abundance of data that is being leveraged to develop actionable and timely interventions. Although in some cases, health information technology (HIT) is still in its infancy, it is rapidly evolving and the potential for HIT to transform health care is evident. Technology enables the flow of data from multiple sources, including clinical settings, public health departments, and insurance claims to identify “hot spots” and high‐disparity communities, enabling targeted interventions.29 Due to federal policy changes, by 2018, certified EHR technology will have the capacity to collect eight domains of social, psychological, and behavioral health data, and some vendors are already going beyond this requirement. This capacity will allow physicians to proactively identify the SDH and link patients with needed community and social services. As is demonstrated in the framework core components and the two case studies below, technology supports each component of the PETAL framework and is becoming ubiquitous in the health care system.
Sustainability of effective interventions is a challenge for health care and research in general, but especially for addressing health disparities.30 In most cases, financial and human resources are needed to implement interventions that will reduce health disparities. When these interventions are initially supported by external funding, the sustainability beyond the initial investment may be fragile. For this reason, sustainability should be targeted from the beginning. Inclusion of community members and leaders, partner organizations, and policymakers lends to increased likelihood of sustainability. This ties into the first core component, because when health equity is prioritized by leadership and integrated into all facets of an organization, sustainability is built in and attainable.
5. CORE COMPONENTS OF THE PETAL FRAMEWORK
5.1. Prioritize health equity
The first component of the PETAL framework is the prioritization of health equity. Health equity cannot simply exist as a concept; it must be embedded into the core mission and supported through purposeful, tangible, and measureable actions. To accomplish this, health equity must be a strategic priority based on community need with recognition of SDH, supported with technology, and directed by a governance structure dedicated to equity that includes community members and leaders. Commitment to health equity as a strategic priority should be reflected and integrated throughout all initiatives and reinforced through allocation of resources.31 Through community engagement and preliminary data analysis, a health equity agenda can be developed to prioritize and strategize on how interventions should be deployed.32
5.2. Engage the community
It is impossible to address and eliminate the health inequities of populations without engaging the very people affected: the community. Overcoming historical distrust of institutions requires buy‐in from and ownership of initiatives by the community.33 Deliberate and strategic actions are necessary to engage patients, families, community organizations, and health professionals across the system.34 Community members should be included in decision making, and governance capacities and their feedback sought to inform all initiatives. Community leaders (elected and lay) should be involved early in the process to understand the concerns of their constituents and to facilitate gaining the trust of the community. Additionally, structured mechanisms for incorporating their feedback should be in place. Strong partnerships with public officials and private organizations are essential, including service organizations that address SDH. Public partnerships may include public safety and/or transportation officials, Medicaid programs, school board members, and city council members. Private and/or service organizations may include faith‐based entities, local convenience stores and bodegas, schools, food pantries, and grocery stores. Leveraging these relationships will also contribute to the visibility and, in turn, the sustainability of the initiative. Innovative technology designed to support and engage under‐resourced communities is important for gathering data and measuring the effectiveness and perceptions of existing interventions.
5.3. Target health disparities
The intervention must be evidence‐based, driven by the data, and targeted to address disparities. Data collection may include both qualitative and quantitative methods. Causes of health disparities and solutions can be gained from the community, including individual factors and beliefs contributing to health inequities and the role that SDH play. Quantitative data may come from a variety of sources, including EHR, insurance claims, public health departments, census surveys, patient surveys, and other sources. Individual‐level data must be collected with informed patient consent, and abide by relevant privacy and security regulations. Individuals from underserved communities may prefer more in‐depth explanations of how their data will be used, who will see it, and how it will be protected. The necessary level of disclosure, appropriate communication mechanisms, and transparency should be guided by individuals serving in governance and leadership capacities but will ultimately be determined by the individuals providing the data. The scientific literature should be reviewed to identify effective strategies, keeping in mind that by nature, health disparities manifest differently in different communities. Thus, community input will be needed to fine tune and execute an effective strategy or intervention.
5.4. Act on the data
Once the data are gathered and analyzed, strategies and interventions can be developed to address specific barriers to health equity. It is essential to develop an action plan that is targeted, prioritized, and initiated strategically.35 Patients, community members, and private and public organizations should be included to address immediate concerns, develop impactful actions, and determine thresholds for goal achievement. Throughout execution, data should be continuously collected and evaluated to monitor successes and/or barriers to effectiveness. In turn, the strategy should be updated and adjusted accordingly to account for any challenges or gaps in services. Interested organizations will need to establish a sustainability plan to continue to work with their patient, community, private, and public partnerships; create specific leadership roles and resource allocations; and develop policies and procedures to modify strategies when necessary.36
5.5. Learn and improve
The final component of the PETAL framework is to learn from the challenges and successes of the interventions and to improve health disparities. This is the culmination of all the preceding components and also the starting point in the feedback loop of continuous improvement. At this point, all processes and outcomes should be analyzed to understand the factors that contributed to success and to identify the barriers that will require adjustment moving forward. Dissemination of findings should be broad and transparent, including to the community. Sustainability is critical to the execution of this component and will determine whether and how the findings are embedded in the long term.
6. CASE STUDIES
Many organizations and programs have recognized the importance of reducing health inequities. The following case studies provide practical examples of how the PETAL framework can be leveraged to prioritize health care equity in a LHS. Please note, while the case studies referenced concern predominately African American communities, this should not be viewed as the only populations affected or otherwise limit the application of the PETAL framework. Applicability of the framework is far reaching, across many domains of health inequities as demonstrated in the table below (Table 2).
Table 2.
Additional case studies: PETAL framework
| Program | Target Population | Summary of Program |
|---|---|---|
| Camden Coalition of Healthcare Providers: Care Management Initiatives, Healthcare HotSpotting | Frequent users/patients with high admission rates | Health care Hotspotting (HH) uses health care data driven to better serve the needs of patients with high readmission rates, or “Super Users.” The HH technique applies a multidisciplinary and coordinated approach that not only treats the patient's health needs but also addresses SDH.a |
| Bithlo Transformation Effort | Semirural, impoverished, environmental health hazards | The “Bithlo transformation Effort,” focuses on improving the health of the community using the following core components: education, environment, transportation, health care, housing, basic needs, and building community. The Florida Hospital along with 65 community, health, and political partners work together to improve the health of the region. The effort uses health data gathered from Florida Hospital/Adventist Health System's EHR records to measure the impact of their engagements.b |
| Dignity Health | Impoverished and disenfranchised | Dignity Health partners with their community members to improve the quality of life of their patients through health programs, grants, investments, and sustainability initiatives. Hospitals affiliated with Dignity Health participate in an annual report on the measurable impacts of their community health programs to adjust for gaps and improvements. Dignity Health, along with Truven Health, jointly developed a Community Need Index (“CNI”). The CNI uses data to analyze demographic metrics and SDH (for example, income, culture/language, education, insurance, and housing) to inform investment strategies addressing the drivers of health inequities.b , c |
| New Hampshire Health and Equity Partnerships | Racial, ethnic, and linguistic minorities | Comprehensive public/private program that focuses on addressing SDH. Periodic report cards are released that report a “disparity score” that includes information pertaining to race, ethnicity, and language (REaL). REaL data are then used to compare outcomes across populations to better address health inequities.d , e |
Camden Coalition of Health Providers. https://www.camdenhealth.org/. Last visited April 20, 2017.
Stakeholder Health. https://stakeholderhealth.org/about/. Last visited April 17, 2017.
Community Need Index Methodology and Source Notes. Truven Health Analytics. http://cni.chw‐interactive.org/Truven%20Health_2015%20Source%20Notes_Community%20Need%20Index.pdf .
Pooler, Jennifer. Holly Korda, Plan to Address Health Disparities and Promote Health Equity in New Hampshire. New Hampshire Health and Equity Partnership. Altarum Institute. March 2011.
Building a Nation of Neighbors. Stories of Impact: Pursuing Health Equity through Welcoming Work. Welcoming America. http://www.welcomingamerica.org/sites/default/files/Health%20Equity%20Stories%20of%20Impact%20FINAL.pdf. Last visited April 17, 2017.
6.1. Case study: Community engagement for early recognition and immediate action in stroke (CEERIAS)
The CEERIAS study is a Patient‐Centered Outcomes Research Institute (PCORI) funded, multi‐institutional and academic‐community partnered program designed to address disparities in stroke awareness, barriers to acute stroke care, and treatments and outcomes in Chicago's minority communities. CEERIAS addresses racial and ethnic disparities in stroke early identification and treatment through community engagement and education. It is currently lead by coprincipal investigators Drs Neelum Aggarwal and Shyam Prabhakaran.
6.1.1. Prioritize health equity
Health equity was prioritized by the funder, PCORI, and the principal investigators. PCORI funds robust patient, family, caregiver, and community‐centered projects that engage these stakeholders in every phase of research. Based on historical knowledge and experience working with the community, the principal investigators knew that the burden of stroke fell disproportionately on minority communities in ways that, for the most part, had little to do with underlying biological or genetic predisposition. Rather, these disparities were reflected in historical and modern day inequalities in access to resources in these communities. Armed with this knowledge, the principal investigators prioritized understanding factors contributing to SDH as best practices for the health care teams and the institutions that were participants in this project.
6.1.2. Engage the community
The project was divided into 2 phases. Phase 1 of the project involved interviews with community members from the neighborhoods impacted by high stroke rates and mortality. Despite ongoing public messaging about stroke, many members of the community were unaware of the signs of stroke that medication could reverse stroke complications and of the existence of primary stroke centers right in their own neighborhoods. There was also a significant amount of bias and fear of discrimination associated with some of the local hospitals, resulting in reluctance to call Emergency Medical Services (EMS). Assessing SDH and openly discussing barriers with community members revealed that financial considerations such as perceived ambulance charges and lack of health insurance also posed major barriers to activating EMS. Based on this feedback, Phase 2 involved the recruitment of “stroke promoters,” respected community leaders, including city council members, school officials, faith‐based organizations, local business owners, and health care providers. The promoters were given tours of the stroke centers and training on stroke identification. They signed the “Pact to Act F.A.S.T.,” an agreement to proactively identify stroke and call EMS immediately. Over 200 stroke promoters were trained over 9 months, and hundreds of thousands of PACT to Act F.A.S.T. cards were distributed throughout the community.
6.1.3. Target health disparities
Literature clearly establishes racial and ethnic disparities in stroke outcomes, exacerbated by gaps in stroke awareness, recognition, appropriate action, and treatment. Data from the local hospital EHR and intake systems and EMS supplemented the literature, indicating that black patients were not receiving the time sensitive medication—tPA—as often as white patients and identified high‐risk areas of the city. However, using more detailed data and analysis methods, the team combined mode of transportation to the emergency department (ED) from the community (calling 911, walk in, or had someone drive to ED) with time to symptom onset and found that significant delay in ED arrival for black compared to white patients impacted whether tPA could be administered. They also used geographic information system (GIS) techniques to determine the community “hot spots” with the most significant disparities in outcomes. These analyses, along with the feedback from the community, provided the compelling case for targeting racial and ethnic minorities in the study.
6.1.4. Act on the data
Despite numerous initiatives to improve stroke outcomes in the community, including establishment of community stroke centers, policy changes, marketing campaigns, and dissemination of educational materials, outcomes in these communities remained poor. The community feedback in Phase 1 was the foundation for the recruitment of stroke promoters who were recognized and respected members of the community and therefore had the influence to expand stroke identification and immediate treatment. These factors led the research team to provide education on identifying stroke symptoms and select the Pact to Act F.A.S.T. online tool, to provide accurate information on ED costs and to demonstrate the benefits of primary stroke centers within the community.
6.1.5. Learn and improve
Ongoing evaluation and measurement were at the core of the study as it evolved from anecdotal understanding of the problem to evidence‐based. Technology was supportive of each phase of the project, including extraction of data from EHRs, the hospital intake system, and the local health department; problem identification and data analysis; and development of an online Pact to Act F.A.S.T. tool that collected geographic information, which would tie back to the community “hot spots” that were initially targeted by the intervention. Each layer of data was used to determine the next steps, and changes were made along the way in response to new data. Sustainability of the “stroke promoter” model is currently being pursued.
6.2. Case study: Toward health recovery and integrated vital engagement (Project THRIVE)
Project THRIVE is a community‐based research project at the Morehouse School of Medicine (MSM) that seeks to reduce mental health disparities through the development, implementation, and evaluation of a culturally centered integrative health care model targeted to predominantly African American population at risk for co‐occurring depression, cardiovascular disease, and/or diabetes. Three community health clinics (CHCs) within the Grady Health System in Atlanta, Georgia, serve as clinical sites for this initiative.
6.2.1. Prioritize health equity
The MSM mission is “leading the creation and advancement of health equity,” and the institution is very engaged with the local community. Project THRIVE is one of the 4 subprojects within the National Institute on Minority Health and Health Disparities (NIMHD)‐funded Transdisciplinary Collaborative Center for Health Disparities Research (TCC) at MSM. The founding Principal Investigator was Dr David Satcher and is currently led by Dr Kisha Holden and Dr Elizabeth Ofili. Extensive literature on mental health disparities in the black community and experience of the project team within the local community drove the decision to prioritize African American mental health disparities for this project.
6.2.2. Engage the community
Project THRIVE consisted of 2 phases, which included mixed methods (qualitative and quantitative) approaches and robust engagement of individual patients, providers, and community members. Phase 1 of the project involved patient focus groups and provider/administrator key informant interviews within primary care centers. The investigative team used data generated from these focus groups and key informant interviews, as well as selected components of 4 different models and some therapeutic approaches. This data is used to inform the development of a culturally competent provider training and a feasible, culturally competent integrated care model in Phase 2 of the project. Engagement of the patients from the CHC sites in Phase 1 contributed to their participation in Phase 2.
6.2.3. Target health disparities
Extensive literature on the significant mental health disparities in African American communities supported the targeted approach used in Project THRIVE. Despite lower incidence and prevalence of depression among African Americans, they experience higher depression chronicity and are less likely to seek, have less access to, and receive poorer quality mental health care than whites. In addition, data from the CHCs demonstrated the need for mental health services, yet no specialists were located within the CHC itself. Lack of colocated mental and physical health services was exacerbated by the SDH since it required transportation, missing another day of work and potentially another copay to receive mental health services. For these reasons, the team decided to focus on developing an intervention that would increase access to high quality mental health care in a location and form conducive to utilization by African American patients of the CHC sites.
6.2.4. Act on the data
A major finding from the focus group discussions was the belief that depression in the community was mainly caused by racial, social and economic stressors, illicit drug use, and caregiver stress. The feedback received was that the culturally tailored educational program should focus on stressors related to race and social disadvantage. Access to healthy food, education, transportation, and employment, which are common issues in disadvantaged communities, were prevalent within the focus group participants. Patients also indicated they would be more likely to seek mental health services within the same setting as physical health services, so a screening kiosk was placed in a waiting area in an inconspicuous location to ensure privacy and minimize stigma. Patients exhibiting symptoms of depression were referred to a behavioral health consultant (BHC), located on‐site 1 day/week at each of the CHCs. The BHC was also a licensed professional counselor (LPC), selected for having experience in both therapy and social work to address the SDH. The BHC used a technology platform that identified social services in their community to which she could refer the patient. Approximately 330 patients were referred for consultation and 174 are in ongoing treatment with the BHC.
6.2.5. Learn and improve
Project THRIVE leveraged technology, data, and feedback from patients and providers to develop the culturally centered integrated care model, which brought services to the clinical sites and to a population that did not otherwise have access. Development of the kiosks was an innovative spin on telemedicine technology to colocate the mental health screenings within a primary care setting. In order to maintain culturally tailored and patient‐centeredness throughout the project, the feedback loop was critical. The project team expects that the findings from the project will support the case for sustainability of the mental health kiosks and a BHC within the CHCs; furthermore, expecting that this will be a model that can be adopted in similarly situated organizations.
7. CONCLUSION
The LHS offers a strong model to help confront health care disparities; however, it requires more strategic alignment with health equity principles to truly achieve health equity. The PETAL framework offers a foundation for LHS to begin to integrate health equity into the LHS core values. As with all LHS principles, it is the intention of this framework to be analyzed, built upon, and adjusted to meet each community, program, and organizational need.
ACKNOWLEDGEMENTS
The authors would like to thank the program staff from Project THRIVE and the CEERIAS study who provided information for the case studies. The authors would also like to thank Mr Devon Douglas for his graphic design work.
Brooks D, Douglas M, Aggarwal N, Prabhakaran S, Holden K, Mack D. Developing a framework for integrating health equity into the learning health system. Learn Health Sys. 2017;1:e10029 10.1002/lrh2.10029
REFERENCES
- 1. 2015 National Healthcare Quality and Disparities Report and 5th Anniversary Update on the National Quality Strategy. Rockville, MD: Agency for Healthcare Research and Quality; April 2016. AHRQ Pub. No. 16‐0015. [Google Scholar]
- 2. World Health Organization . Social Determinants of Health, Key concepts. http://www.who.int/social_determinants/thecommission/finalreport/key_concepts/en/. Last visited Jan. 25, 2017.
- 3. Institute of Medicine . Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care (full printed version). Washington, DC: The National Academies Press; 2003. doi: https://doi.org/10.17226/10260. [PubMed] [Google Scholar]
- 4. Ayania, John Z . The costs of racial disparities in health care. Institute for Healthcare Policy and Innovation, University of Michigan NEJM Catalyst. http://catalyst.nejm.org/the‐costs‐of‐racial‐disparities‐in‐health‐care/. February 15, 2016. Last accessed January 17, 2017.
- 5. Powell, Alvin . The costs of inequality: money = quality health care = longer life. Harvard Gazette. February 22, 2016.
- 6. LaVeist TA, Gaskin D, Richard P. Estimating the economic burden of racial health inequalities in the United States. Int J Health Serv. 2011;41(2):231‐238. [DOI] [PubMed] [Google Scholar]
- 7. Satcher D, Fryer GE Jr, McCann J, Troutman A, Woolf SH, Rust G. What if we were equal? A comparison of the black‐white mortality gap in 1960 and 2000. Health Aff (Millwood). 2005. Mar‐Apr;24(2):459‐464. [DOI] [PubMed] [Google Scholar]
- 8. Rust G, Zhang S, Malhotra K, et al. Paths to health equity: local area variation in progress toward eliminating breast cancer mortality disparities, 1990‐2009. Cancer. 2015;121(16):2765‐2774. 10.1002/cncr.29405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brown Speights JS, Goldfarb SS, Wells BA, Beitsch L, Levine RS, Rust G. State‐level progress in reducing the black‐white infant mortality gap, United States, 1999‐2013. Am J Public Health. 2017;107(5):775‐782. 10.2105/AJPH.2017.303689. Epub 2017 Mar 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rust G, Zhang S, Yu Z, et al. Counties eliminating racial disparities in colorectal cancer mortality. Cancer. 2016;122(11):1735‐1748. 10.1002/cncr.29958. [DOI] [PubMed] [Google Scholar]
- 11. Social determinants of health . World Health Organization. Available at http://www.who.int/social_determinants/en/.
- 12. Promoting Health and Reducing Health Inequities by Addressing the Social Determinants of Health. Europe: http://www.euro.who.int/__data/assets/pdf_file/0016/141226/Brochure_promoting_health.pdf. The World Health Organization; 2017. Last visited January 10, 2017. [Google Scholar]
- 13. Schroeder SA. Shattuck lecture. We can do better—improving the health of the American people. N Engl J Med. 2007;357(12):1221‐1228. [DOI] [PubMed] [Google Scholar]
- 14. Heiman H, Artiga S. Beyond health care: the role of social determinants in promoting health and health equity. Issue Brief. The Kaiser Commission on Medicaid and the Uninsured at the Kaiser Family Foundation, Satcher Health Leadership Institute at Morehouse School of Medicine. 2015.
- 15. 2015 National healthcare quality and disparities report and 5th anniversary update on the National Quality Strategy. Content last reviewed 2016. Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/research/findings/nhqrdr/nhqdr15/index.html
- 16. Lion KC, Raphael JL. Partnering health disparities research with quality improvement science in pediatrics. Pediatrics. 2015;135(2):354‐361. 10.1542/peds.2014-2982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Herbst LWJH, Coury‐Doniger P, Painter TM, et al. Efficacy of an HIV/STI prevention intervention for black men who have sex with men: findings from the Many Men, Many Voices (3MV) project. AIDS Behav. 2009;13(3):532‐544. [DOI] [PubMed] [Google Scholar]
- 18. Woods ER, Bhaumik U, Sommer SJ, et al. Community asthma initiative to improve health outcomes and reduce disparities among children with asthma. MMWR Suppl. 2016;65:11–20. [DOI] [PubMed] [Google Scholar]
- 19. Hutchins SS, Jiles R, Bernier R. Elimination of measles and of disparities in measles childhood vaccine coverage among racial and ethnic minority populations in the United States. J Infect Dis. 2004;189(Suppl 1):S146‐S152. [DOI] [PubMed] [Google Scholar]
- 20. Friedman C, Rubin J, Brown J, et al. Toward a science of learning systems: a research agenda for the high‐functioning Learning Health System. J Am Med Inform Assoc. 2014;22(1):43‐50. 10.1136/amiajnl-2014-002977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Core Values Underlying a National‐Scale Person‐Centered Continuous Learning Health System (LHS) . 2012. Learning Health System summit. Available at http://www.learninghealth.org/corevalues/.
- 22. Equity Framework for Health . USAID. Health policy initiative. Available at http://www.healthpolicyinitiative.com/index.cfm?id=topicEquity. Last accessed January 17, 2017.
- 23. National Academies of Sciences, Engineering, and Medicine . Communities in Action: Pathways to Health Equity. Washington, DC: The National Academies Press; 2017. https://doi.org/10.17226/24624. [PubMed] [Google Scholar]
- 24. The Victorian Health Promotion Foundation (VicHealth) framework for health equity. https://www.vichealth.vic.gov.au/media‐and‐resources/publications/the‐vichealth‐framework‐for‐health‐equity.
- 25. Murray CJL, Frenk J. A WHO framework for health system performance assessment. Evidence and information for policy. World Health Organization. http://www.who.int/healthinfo/paper06.pdf [Google Scholar]
- 26. Wyatt R, Laderman M, Botwinick L, Mate K, Whittington J. Achieving Health Equity: A Guide for Health Care Organizations. IHI White Paper. Institute for Healthcare Improvement: Cambridge, MA; 2016. http://www.ihi.org/resources/Pages/IHIWhitePapers/Achieving-Health-Equity.aspx. [Google Scholar]
- 27. Charles D, Gabriel M, Furukawa MF. “Adoption of Electronic Health Record Systems among U.S. Non‐federal Acute Care Hospitals: 2008‐2013,” ONC Data Brief, no. 16. Washington, DC: Office of the National Coordinator for Health Information Technology; 2014. [Google Scholar]
- 28. Lee J. The impact of health information technology on disparity of process of care. Int J Equity Health. 2015;14:34 10.1186/s12939-015-0161-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Using Geographic Information to Target Health Disparities: State Experience . Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality; 2016. www.hcup‐us.ahrq.gov/reports/race/GeographicInfoIB.jsp. [Google Scholar]
- 30. Wallerstein N, Duran B. Community‐based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. 2010. Apr 1;100(Suppl 1):S40‐S46. 10.2105/AJPH.2009.184036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. 14 Inside and outside strategies to advance health equity within local public health practice. Human Impact Partners. 2016. http://www.humanimpact.org/wp‐content/uploads/HE_Practice_InsideOutsideStrategies_Descriptions.pdf. Last accessed January 15, 2017.
- 32. Urban HEART: Urban Health Equity Assessment and Response Tool . World Health Organization. http://www.who.int/kobe_centre/publications/urban_heart_manual.pdf. 2010; Last accessed January 10, 2017 [Google Scholar]
- 33. Cuevas AG. "Exploring four barriers experienced by African Americans in healthcare: perceived discrimination, medical mistrust, race discordance, and poor communication." 2013. Dissertations and Theses. Paper 615.
- 34. Patient And Family Engagement . A framework for understanding the elements and developing interventions and policies. Health Aff. 2013;32(2):223‐231. 10.1377/hlthaff.2012.1133 [DOI] [PubMed] [Google Scholar]
- 35. Urban HEART . Urban health equity assessment and response tool. World Health Organization. http://www.who.int/kobe_centre/publications/urban_heart_manual.pdf. 2010; Last accessed January 10, 2017 [Google Scholar]
- 36. Batan, Marilyn , MPH . Sustainability planning guide. CDC's healthy communities program https://www.cdc.gov/nccdphp/dch/programs/healthycommunitiesprogram/pdf/sustainability_guide.pdf. Last accessed January 17, 2017.


