Abstract
Paraduodenal hernia is a rare congenital anomaly; however, it is the most common cause of internal herniation. Clinical findings are often indeterminate. Computerized tomography is usually diagnostic; however, the diagnosis is often made intra-operatively. Paraduodenal hernia carries a risk of incarceration leading to bowel obstruction and strangulation; therefore, it should be repaired surgically when diagnosed. Here we present a case of left PDH that was diagnosed preoperatively and repaired laparoscopically.
Keywords: Laparoscopy, paraduodenal, hernia
INTRODUCTION
Internal hernias result from the extension of the intestine through a defect within the peritoneum or mesentery (1). They may be either congenital or acquired. Paraduodenal hernia (PDH) is a rare congenital anomaly that results from an error of rotation of the midgut (2). PDHs are the most common form of internal hernias, accounting for 53% of all internal hernias (1, 3). PDHs are difficult to diagnose because the clinical symptoms are variable (4). PDH can begin with symptoms of acute obstruction or recurring abdominal pain (43%) or can be asymptomatic throughout the patient’s life. Between 10% and 50% of internal hernias are discovered during unrelated abdominal surgeries or imaging exams and autopsy (5). Preoperative computerized tomography scan of the abdomen is usually diagnostic; however, the diagnosis is often made intra-operatively. Surgical treatment can be performed with traditional open methods or minimally invasive laparoscopic techniques. We describe herein the preoperative radiological diagnosis and successful laparoscopic repair of a left PDH in an adult man.
CASE PRESENTATION
A 39-year-old man was admitted to the emergency department with complaints of epigastric cramps and nausea and vomiting that persisted for almost one day. It was known that he had been suffering from similar problems for a long time, and he had applied to 3 different hospitals in the last 10 days. There was no specific finding except for upper left quadrant tenderness. He had no history of abdominal surgery. His vital signs were normal. On his plain abdominal film, vague and limited air-fluid levels and a mass-like lesion were found in the left quadrants. Laboratory results were normal, except his leukocyte count was 11600. He was hospitalized for follow-up. It was noticed that he was comfortable while resting on his left side; however, his pain worsened in the supine position. Encapsulated and moderately dilated small bowel loops were detected in the upper left quadrant between the stomach and pancreas by CT (Figure 1). He was preoperatively diagnosed with left PDH. Four ports were inserted; one 10 mm supraumblical port for the camera, another port 10 mm from the upper left quadrant, and two 5 mm ports in the upper right quadrant. During exploration, left PDH was observed on the left side of Treitz’s ligament behind the inferior mesenteric vein. An entrapped jejunum loop of approximately 80 cm was then reduced from the hernia sac into the abdominal cavity with an atraumatic tool. The loop was easily released by gentle traction. There was no ischemic or necrotic intestinal loop. The hernia sac was not resected, and the orifice was then closed intracorporeally with interrupted sutures using non-absorbable multifilament 3-0 material from the tissue around the inferior mesenteric vein to the tissue on the posterior abdominal wall and the serosa of the jejunum, avoiding injury to the inferior mesenteric vessels (Figure 2). Surgery time was 25 minutes. Loss of blood was approximately 30 ml. The patient’s postoperative course was uneventful. The patient was given oral nutrition 8 hours after the surgery and was discharged 36 hours after operation. No recurrence was observed at one-year follow-up.
Figure 1.
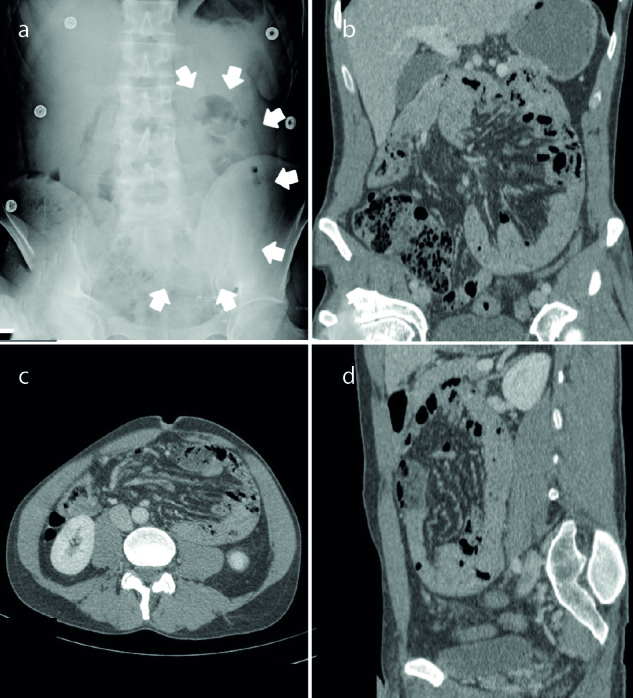
a-d. Radiologic findings in this case (a) A plain radiograph of the abdomen shows a mass-like lesion (arrows). Computerized tomography scan of the abdomen in coronal (b), axial (c) and sagittal (d) cuts
Figure 2.
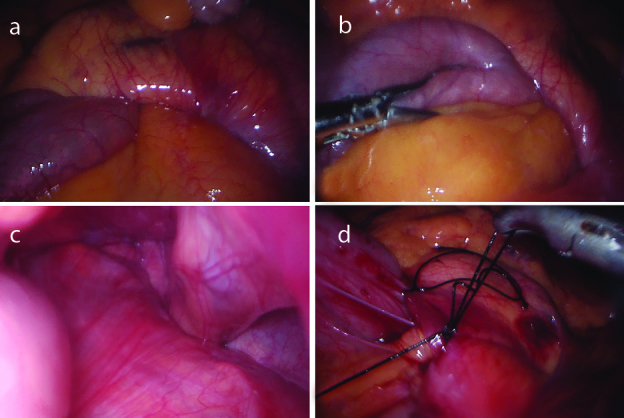
a-d. Laparoscopic view of the left PDH (a) Hernia orifice and distal part of entrapped jejunum, (b) Reduction of the entrapped jejunal loop (c) Hernia sac and cavity (d) Closure of the hernia orifice with intracorporeal sutures
DISCUSSION
Paraduodenal hernia is a rare condition; however, it is the most common cause of internal hernia (2). The first PDH was evidently described during an autopsy by Neubauer in 1786. In 1857, Treitz defined PDHs as “retroperitoneal hernias”; he believed that they were caused by herniation of the intestine into the duodenojejunal fossa. Jonnesco, in 1889 and 1890, divided these hernias into two distinct types: left and right. In 1923, Andrews first described the basis of the embryogenic origin of right PDH as a result of defective or incomplete midgut rotation. A clear description of the mechanism of left PDH as a fusion defect between the left mesocolon and the mesentery of the duodenum was provided by Callander in 1935 (6). In the present case, the bowels were observed to have completed their rotation; therefore, it was thought that the left PDH was due to a fusion defect. 25% of PDHs develop on the right side of Treitz’s ligament and involve the mesentericoparietal fossa (Waldeyer’s fossa). Approximately 75% occur on the left and involve the paraduodenal fossa (Landzert’s fossa). The Landzert’s fossa is situated immediately lateral to the ascending duodenum, posterior to the inferior mesenteric vein (IMV) and the ascending branch of the left colic artery, directly beneath the posterior parietal peritoneum. Left PDH extends in a retrocolic fashion into the left portion of the transverse mesocolon and the descending mesocolon (7) (Figure 3). PDH can present at any age but is usually seen between the 4th and 6th decades of life (mean age 38.5 years). Males are affected three times more than females (4, 6).
Figure 3.
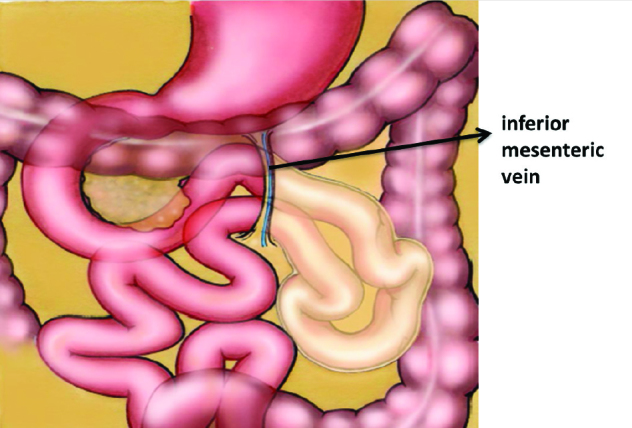
Graphic illustration of a left PDH depicts jejunal loop prolapsing through posterior of left mesocolon, lateral to Treiz’s ligament, behind inferior mesenteric vein
Paraduodenal hernias can be asymptomatic and can be found by laparotomy or autopsy (8). Symptomatic presentation can range from intermittent and mild digestive complaints to acute intestinal obstruction. Complaints are usually relieved by changes in position. Symptoms are often postprandial (especially after a large meal), and pain may be relieved when the patient lies supine (4, 8). In this case, the patient had colic and postprandial growing pain for a long time; however, it is notable that the pain was relieved in the left lateral supine position. Symptoms such as postprandial abdominal pain, nausea, and vomiting can lead the physician to misdiagnose PDH as biliary disease and peptic ulcer (4). Due to its nonspecific symptoms, PDH can even be misinterpreted as FMF in countries such as Turkey, which contains a large proportion of patients who suffer from FMF (9).
There is no specific physical examination finding for left PDH. However, it can be felt as a palpable mass in the left upper quadrant. Correct preoperative diagnosis of PDH is difficult and can only be made radiologically. In abdominal plain radiographs or gastrointestinal contrast studies, left PDH presents as an encapsulated circumscribed mass of a few intestinal loops in the left upper quadrant, lateral to the fourth part of the duodenum. The first diagnosis of an internal hernia by CT was presented by Harbin in 1982 (10). Abdominal CT is the gold standard to provide a correct diagnosis; the CT findings for a left PDH may show entrapped intestinal loops with the appearance of a smooth encapsulated border, called Donnelly’s border, between the stomach and pancreas (5, 11). In this case, CT was ordered after vague air-fluid levels and a mass-like lesion were detected in the left quadrants on plain x-ray. As classic CT findings were observed, a definitive diagnosis was made preoperatively.
Paraduodenal hernia carries an approximately 50% lifetime risk of incarceration, leading to bowel obstruction and strangulation; therefore, it should be repaired surgically when diagnosed (4, 8). Surgical treatment can be performed with conventional open methods or minimally invasive laparoscopic techniques. The standard surgical approach for PDHs involves reduction of the entrapped intestinal loops, with resection if necessary in the case of nonviable segments, and repair of the defect by either closure or wide opening of the hernia orifice so the hernia sac becomes a part of the general peritoneal cavity (2, 7). Left PDH can usually be reduced easily. The closure of the hernia orifice with sutures is sufficient. If reduction is difficult, widening of the hernia orifice by an incision along an avascular plane of the descending mesocolon or division of the IMV is performed (2). Excision of the hernia sac is generally not mandatory. Recurrent cases can be repaired with a mesh (3). In this case, because the left PDH was easily reduced, expansion of the hernia sac and IMV scarification were not necessary. Primary closure of the hernia orifice was sufficient.
There are many reports in the literature of left PDH, although the total number of reported cases is less than 500 (12). The approach of minimally invasive techniques for hernia is relatively new; the first successful laparoscopic repair of PDH was reported by Uematsu in 1998 (7). Since then, several successful laparoscopic PDH repairs have been reported in various countries. After searching the national and international literature, we found 22 cases related to adult PDH in Turkey (9, 13–30). This is summarized in the Table 1. This is the first case report of laparoscopically repaired PDH from Turkey. Öztaş et al. (29) preoperatively diagnosed a case by CT and began laparoscopic surgery; however, the operation was converted to open surgery.
Table 1.
Published cases from Turkey in the national and international literature
| Author | Published date | Age | Sex | Previously abdominal surgery | Preoperative examination | Side of hernia | Surgical technique | Hernia repair technique | Discharge time |
|---|---|---|---|---|---|---|---|---|---|
| Cebeci et al. (13) | 1976 | 70 | F | None | x-ray, PE | Right | Laparotomy | Primary closure | P.O.-1 exitus |
| Tireli et al. (14) | 1982 | 18 | M | None | x-ray, PE | Left | Laparotomy | Primary closure | UD |
| Kebudi et al. (15) | 1989 | 43 | M | None | x-ray, PE | Right | Laparotomy | Primary closure | 10 days |
| Yüceyar et al. (16) | 1993 | 49 | M | None | x-ray, PE | Left | Laparotomy | Wide opening | 13 days |
| Özçelik et al. (17) | 1993 | 21 | M | None | x-ray, PE | Left | Laparotomy | Primary closure | UD |
| Şahin et al. (18) | 1998 | 44 | M | None | x-ray, PE | Left | Laparotomy | Primary closure | 10 days |
| Şahin et al. (18) | 1998 | 63 | M | None | x-ray, PE | Left | Laparotomy | Primary closure | 7 days |
| Ovalı et al. (19) | 2005 | 52 | F | None | CT | Left | Refused surgery | ||
| Cingi et al. (9) | 2006 | 30 | M | None | CT | Left | Laparotomy | Resection of the hernia sac | 4 days |
| Şen et al. (20) | 2007 | 24 | F | None | x-ray, PE | Left | Laparotomy | Primary closure | 5 days |
| Şen et al. (20) | 2007 | 20 | M | None | CT | Right | Laparotomy | Primary closure | 6 days |
| Tekin et al. (21) | 2007 | 53 | M | None | x-ray, PE | Right | Laparotomy | Primary closure | 4 days |
| Tekin et al. (21) | 2007 | 48 | M | None | x-ray, PE | Right | Laparotomy | Primary closure | 11 days |
| Akın et al (22) | 2009 | 23 | M | None | x-ray, PE | Left | Laparotomy | Resection of the hernia sac | 3 days |
| Okan et al. (23) | 2010 | 43 | M | None | CT | Left | Laparotomy | Primary closure | 8 day |
| Polat et al. (24) | 2010 | 25 | M | None | x-ray, PE | Left | Laparotomy | Primary closure | 4 days |
| Acu et al. (25) | 2010 | 29 | M | Appendectomy | CT | Left | Laparotomy | Primary closure | UD |
| Arslan et al. (26) | 2012 | 49 | M | None | CT | Left | Laparotomy | Primary closure | 3 days |
| Akbulut et al. (27) | 2012 | 42 | M | None | x-ray, PE | Left | Laparotomy | Primary closure | 5 days |
| Öztaş et al. (28) | 2013 | 42 | M | Appendectomy | CT | Left | Laparoscopy convertion laparotomy | Primary closure | 4 day |
| Cengiz et al. (29) | 2013 | 43 | M | Appendectomy | CT | Left | Laparotomy | Primary closure | UD |
| Gemici et al. (30) | 2014 | 45 | F | None | CT | Left | Laparotomy | Primary closure | 4 days |
M: male; F: female; CT: computed tomography; PE: physical examination; UD: undeclared
Early and correct preoperative diagnosis may play an important role in determining the surgical strategy. In the present case, preoperative diagnosis and no ischemic sign in the CT findings enabled us to decide on a laparoscopic surgery approach. The major benefits of laparoscopic surgery can be cited as less postoperative pain, short hospital stay, and early return to normal activity.
CONCLUSION
Paraduodenal hernia is very rare, and preoperative diagnosis is difficult because there are no specific symptoms or physical examination findings. CT is the gold standard for preoperative diagnosis. Laparoscopic surgery is technically easy and may be the best surgical method for left PDHs without bowel necrosis.
Acknowledgements
The authors thank to Elif Gökçal and Emine Deniz Gözen for their contributions.
Footnotes
Informed Consent: Written informed consent was obtained from patient who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - F.G., Y.Ç., Z.A.; Design - F.G., F.A.; Supervision - Y.Ç., F.A.; Data Collection and/or Processing - F.G., F.A., Z.A.; Analysis and/or Interpretation -F.G., Z.A.; Literature Search - F.G., Y.Ç.; Writing Manuscript F.G., Y.Ç.; Critical Reviews - F.G., Y.Ç.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Coakley BA, Froylich D, Wong R, Khaitov S. Repair of primary bowel obstruction resulting from a left paraduodenal hernia. Am Surg. 2012;78:E422–424. [PubMed] [Google Scholar]
- 2.Bartlett MK, Wang C, Williams WH. The surgical management of paraduodenal hernia. Ann Surg. 1968;168:249–254. doi: 10.1097/00000658-196808000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Palanivelu C, Rangarajan M, Jategaonkar PA, Anand NV, Senthilkumar K. Laparoscopic management of paraduodenal hernias: mesh and mesh-less repairs. A report of four cases. Hernia. 2008;12:649–653. doi: 10.1007/s10029-008-0376-y. [DOI] [PubMed] [Google Scholar]
- 4.Yun MY, Choi YM, Choi SK, Kim SJ, Ahn SI, Kim KR. Left paraduodenal hernia presenting with atypical symptoms. Yonsei Med J. 2010;51:787–789. doi: 10.3349/ymj.2010.51.5.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Assenza M, Rossi D, Rossi G, Reale C, Simonelli L, Romeo V, et al. Laparoscopic management of left paraduodenal hernia. Case report and review of literature. G Chir. 2014;35:185–189. https://doi.org/10.11138/gchir/2014.35.7.185. [PMC free article] [PubMed] [Google Scholar]
- 6.Khan MA, Lo AY, Vande Maele DM. Paraduodenal hernia. Am Surg. 1998;64:1218–1222. [PubMed] [Google Scholar]
- 7.Uematsu T, Kitamura H, Iwase M, Yamashita K, Ogura H, Nakamuka T, et al. Laparoscopic repair of a paraduodenal hernia. Surg Endosc. 1998;12:50–52. doi: 10.1007/s004649900591. [DOI] [PubMed] [Google Scholar]
- 8.Manji R, Warnock GL. Left paraduodenal hernia: an unusual cause of small-bowel obstruction. Can J Surg. 2001;44:455–457. [PMC free article] [PubMed] [Google Scholar]
- 9.Cingi A, Demirkalem P, Manukyan MN, Tuney D, Yegen C. Left-sided paraduodenal hernia: report of a case. Surg Today. 2006;36:651–654. doi: 10.1007/s00595-006-3205-x. [DOI] [PubMed] [Google Scholar]
- 10.Olazabal A, Guasch I, Casas D. Case report: CT diagnosis of nonobstructive left paraduodenal hernia. Clin Radiol. 1992;46:288–289. doi: 10.1016/S0009-9260(05)80175-8. [DOI] [PubMed] [Google Scholar]
- 11.Martin LC, Merkle EM, Thompson WM. Review of internal hernias: radiographic and clinical findings. AJR Am J Roentgenol. 2006;186:703–717. doi: 10.2214/AJR.05.0644. [DOI] [PubMed] [Google Scholar]
- 12.Downes R, Cawich SO. A case of a paraduodenal hernia. Int J Surg Case Rep. 2010;1:19–21. doi: 10.1016/j.ijscr.2010.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cebeci H, Alver O. Ender görülen boğulmuş bir paraduodenal fıtık olgusu. Cerrahpaşa Tıp Fakültesi Dergisi. 1976;7:114–122. [Google Scholar]
- 14.Tireli M. Left paraduodenal hernia. Br J Surg. 1982;69:114. doi: 10.1002/bjs.1800690219. [DOI] [PubMed] [Google Scholar]
- 15.Kebudi A, Canik A, Şermet G. İntestinal obstrüksiyona yol açmış bir paraduodenal herni vakası. Ulus Cerrahi Derg. 1989;5:75–76. [Google Scholar]
- 16.Yüceyar S, Er M, Kaya A. Sol paraduodenal herni. Cerrahpaşa Tıp Fakültesi Dergisi. 1993;24:523–527. [Google Scholar]
- 17.Özçelik MF. Sol paraduodenal herniye bağlı ileus. Klinik ve Deneysel Cerrahi Dergisi. 1993;1:261–262. [Google Scholar]
- 18.Şahin M, Tekin Ş, Çiftçi E, Gürocak B. Paraduodenal herniler: Olgu sunumu. Cerrahi Tıp Arşivi. 1998;3:38–39. [Google Scholar]
- 19.Ovali GY, Orguc S, Unlu M, Pabuscu Y. Transient left paraduodenal hernia. Comput Med Imaging Graph. 2005;29:459–461. doi: 10.1016/j.compmedimag.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 20.Sen M, Inan A, Dener C, Bozer M. Paraduodenal internal hernias: clinical analysis of two cases. Ulus Travma Acil Cerrahi Derg. 2007;13:232–236. [PubMed] [Google Scholar]
- 21.Tekin A, Şahin M, Küçükkartallar T, Kaynak A. Nadir bir ileus nedeni: Paraduodenal herni. Genel Tıp Dergisi. 2007;17:111–114. [Google Scholar]
- 22.Akın M, Kurukahvecioğlu O, Bostancı H, Anadol AZ, Taneri F. Left Paraduodenal Hernia Caused by a Peritoneal Membrane: Report of a Case. Erciyes Med J. 2009;1:29–32. [Google Scholar]
- 23.Okan I, Ozkan OV, Sahin M, Bas G, Alimoglu O. Left paraduodenal hernia diagnosed preoperatively. ANZ J Surg. 2010;80:116. doi: 10.1111/j.1445-2197.2009.05191.x. [DOI] [PubMed] [Google Scholar]
- 24.Polat FR, Dinelek H. Left paraduodenal hernia: Report of a case. Sakarya Medical Journal. 2012;2:56–58. doi: 10.5505/sakaryamj.2012.46338. [DOI] [Google Scholar]
- 25.Acu R, Ökten S, Küçükay F, Tunç B, Kalkan İH, Ölçer T. Sol paraduodenal herni: Çok kesitli bilgisayarlı tomografi bulguları. Akademik Gastroenteroloji Dergisi. 2010;9:38–40. [Google Scholar]
- 26.Arslan K, Doğru O, Köksal H, Atay A. A rare cause of intestinal obstructions: left paraduodenal hernia. Case Study and Case Report. 2012;2:137–142. [Google Scholar]
- 27.Akbulut S. Unusual cause of intestinal obstruction: left paraduodenal hernia. Case Rep Med. 2012;2012 doi: 10.1155/2012/529246. 529246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Öztaş M, Can MF, Öztürk E, Yağcı G. A rare pathology that caused high-level intestinal obstruction: Left paraduodenal hernia. Ulus Cerrahi Derg. 2013;29:92–95. doi: 10.5152/UCD.2013.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cengiz MB, Hasbahceci M, Cipe G, Karatepe O, Muslumanoglu M. Acute intestinal obstruction secondary to left paraduodenal hernia: a case report. Ulus Travma Acil Cerrahi Derg. 2013;19:573–575. doi: 10.5505/tjtes.2013.30776. [DOI] [PubMed] [Google Scholar]
- 30.Gemici K, Okuş A, Arık B, Acar T, Efe D. Sol paraduodenal herni. Türkiye Klinikleri Journal of Case Reports. 23:393–396. [Google Scholar]


