Abstract
Background
Sexual behaviors in HIV-infected pregnant women in South Africa are not well understood.
Methods
HIV-infected pregnant women were recruited into a prospective cohort at first antenatal care visit. Sociodemographic information and self-collected vulvovaginal swab samples were collected from participants. Vulvovaginal swab samples were tested for Chlamydia trachomatis (CT), Neisseria gonorrhoea (NG) and Trichomonas vaginalis (TV) using GeneXpert®. We investigated sexual behaviors, alcohol use and factors associated with condomless sex during pregnancy and prevalent sexually transmitted infection (STI) among our cohort. We report descriptive, univariate and multivariable logistic regression results of sexual behaviors and alcohol use, factors associated with condomless sex at last sex, and having any STI during pregnancy adjusting for a priori confounders.
Results
We recruited and enrolled 430 HIV-infected pregnant women. Median age was 30-years; median gestational age was 20-weeks. 89% of women reported sex during pregnancy. At last sex, 68% reported condomless sex; 18% reported having >1 sex partner in the past 12-months. Adjusting for age, income and relationship status, condom use at last sex was associated with prior knowledge of HIV status (aOR=2.46; 95% CI=1.54–3.92) and being in a concordant HIV-positive (aOR=3.17; 95% CI=1.84–5.50), or serodiscordant relationship (aOR=6.50; 95% CI=3.59–11.80). The prevalence of any STI was 41% (95% CI=36%–45%). Adjusting for mothers’ age and employment, odds of having a STI increased if the woman reported alcohol use during pregnancy (aOR=1.96; 95% CI=1.06–3.64) or if the father of the child was a non-cohabiting or casual partner (aOR=1.42; 95% CI=0.97–2.03).
Conclusion
Almost all HIV-infected pregnant women were sexually active during pregnancy and most women reported condomless sex at last sex. Condom use was associated with knowledge of serostatus and/or partner’s serostatus before first ANC visit. Factors associated with having a STIs included: alcohol use during pregnancy and father of child being a non-cohabiting partner.
Keywords: STD, pregnant women, behaviors, HIV-infected, South Africa
Introduction
There are an estimated 351 million new cases of Trichomonas vaginalis (TV), Chlamydia trachomatis (CT), and Neisseria gonorrhea (NG), annually.1 Those sexually transmitted infections (STIs) are associated with adverse pregnancy, pregnancy and birth outcomes such as increased risk of ectopic pregnancy, pre-term labor, growth retardation, and intrauterine death.1–6 Furthermore, STIs can be vertically transmitted to newborns during passage through the birth canal.7 Prior studies reported that 30% to 50% of infants born to mothers with untreated CT and NG infections develop clinical conjunctivitis and 10% to 20% develop pneumonia.8–10
In addition to adverse birth and pregnancy outcomes, STIs also increases the risk of HIV transmission to sex partners during intercourse due to increased inflammation and lesions that facilitate HIV shedding and acquisition.11–14 Moreover, studies reported that pregnant women with STIs may have an increased risk of mother-to-child-transmission (MTCT) of HIV.15,16 Given the World Health Organization (WHO)’s new 2016–2021 prevention and treatment strategy on HIV, viral hepatitis, and STIs, it is important to understand and reduce risk factors associated with STIs in HIV-infected pregnant women to reduce MTCT of STIs and HIV.17 The South African Government has rolled out an ambitious PMTCT program that includes reaching women before and during pregnancy to provide HIV counseling and testing (at each visit if HIV-uninfected at prior visit) though the postnatal period up to 18-months. If HIV-infected, the mother starts on life-long ART and receives viral load monitoring, including a viral load at the same time of confirmed pregnancy. If the viral load is >1000 copies/ml she will receive comprehensive adherence counseling and repeated viral load testing 1-month later to evaluate the need to switch to second line regiment as per adult ART guidelines.18
Sexual behavior in HIV-infected pregnant women in South Africa are not well understood. While there are numerous studies on the physiological changes during pregnancy and postpartum periods which increase HIV risk, behaviors that increase risky sex during pregnancy, thus increasing the risk of HIV and STI acquisition and transmission are not well described.19 A recent study in Zambia showed that heavy alcohol use in serodiscordant couples was associated with reporting one or more outside sex partners, increased risk of HIV acquisition, and lower odds of initiating ART in HIV-infected female heavy drinkers.20 A study from KwaZulu-Natal, South Africa, demonstrated that alcohol use by HIV-infected women was associated with prior STI treatment and increased number of sex partners,21 while a study conducted in pregnant women in Mpumalanga, South Africa, showed that HIV-infection, physical partner violence in the past 6-months, and psychological distress was associated with having an STI.22 Given the increased risk of horizontal and vertical transmission of HIV associated with STIs, understanding sexual and behavioral risk factors associated with STIs during pregnancy is urgently needed.
We conducted a study among a prospective cohort of HIV-infected pregnant women in Tshwane District, South Africa. We previously demonstrated a high prevalence of 47.8% of women testing positive for either CT, NG, or TV infection in this cohort.23 This study describes sexual behaviors during pregnancy and evaluates behavioral factors associated with risky sex, defined as condomless sex at last sex, and STIs to inform interventions to address the burden of STIs in HIV-infected pregnant women.
Methods
Study Design
We conducted a study amongst HIV-infected pregnant women attending their first antenatal care (ANC) visit at one of three public sector clinics in Tshwane District, South Africa. This study was embedded within a prospective cohort study evaluating the impact of STI screening among HIV-infected pregnant women.23 Data collection for sexual history and risk behavior was collected via interview and was previously described.23 To improve the internal validity of the questions asked, we asked the questions in different ways and the interviewers were peers who were trained to be sensitive around asking questions about sexual activity. Evaluation of recent alcohol use was collected using previously validated, standardized AUDIT questionnaires.24 For this study, we evaluated: (1) sexual behaviors and alcohol use in HIV-infected pregnant women, (2) factors associated with condomless sex at last sex during pregnancy, and (3) factors associated with prevalent STI at participant’s first ANC visit. To be eligible for the study, women had to be aged ≥18 years, HIV-infected, and currently pregnant (<34-weeks pregnant) with the stated intention to reside in Tshwane District (Gauteng Province) for the duration of the pregnancy.
Specimen Collection and Testing
As previously described,23 women self-collected vulvovaginal swab specimens using Xpert® CT/NG Vaginal/Endocervical Specimen Collection kits [Cepheid, Sunnyvale, CA], and were tested for CT, NG and TV using the Xpert® CT/NG assay and the Xpert® TV assay [Cepheid, Sunnyvale, CA]. Self-collected vaginal swabs have been shown to have a high sensitivity and specificity.25
Treatment
Women with a positive STI test result were provided targeted, same-day treatment in accordance with South Africa National guidelines.26 For their sex partner(s), women were given the option to either take a pill packet of targeted antibiotics to her partner(s) or present her partner(s) with a referral letter to attend clinic for STI testing and treatment. All women were provided condoms and counseling around condom use.
Definitions and data analysis
Gestational age was determined by date of last menstrual period. Proportions were used to summarize categorical variables and chi-squared tests were used for comparisons between groups. Mean, median, range, and interquartile range were used to summarize continuous variables.
Initially, we conducted a descriptive analysis of socio-demographics, clinical characteristics and sexual behaviors in study participants. Then, we conducted logistic regression analyses to evaluate: (1) demographic, relationship and behavioral factors associated with condomless sex at last sex during pregnancy and (2) associations between demographic, relationship, clinical and behavioral variables and any STI infection. In multivariable analyses we included any variable that had p<0.10 in univariate analyses. In addition, the following variables were considered for inclusion in the model based on the value of the estimated odds ratio or considering they were a priori variables including: age, relationship with father of the child, income or employment status. We tested for collinearity using a variance inflation factor and excluded any variables that were collinear in a model and kept the variable that had the strongest association with the outcome. Each model adjusted for potential confounders: age, partnership status and income. For the factors associated with having any STI, we ran separate models for each of the significant covariates (p<0.10), adjusting for age and employment status. Data analyses were performed using STATA v14 (StataCorp, College Station, Texas).
Ethics
Ethical approval and oversight was provided by the Institutional Review Board at the University of Pretoria, Faculty of Health Sciences, Research Ethics Committee under reference number 401/2015 and the University of California Los Angeles under reference number 15-001351. We received additional permission from the Tshwane District Health Department, as well as each primary health care facility and tertiary care facility for the abstraction of pregnancy outcomes data from clinical records. Informed consent was obtained from all participants prior to enrollment.
Results
We enrolled 430 HIV-infected pregnant women attending their first ANC visit. The median age of study participants was 30 years old (interquartile range [IQR]=26–34) and the median gestational age was 20 weeks [IQR=14–25]. Fifty-five percent of women did not complete secondary school (n=236), 59% of were not currently employed (n=251), and 40% received a social grant to meet their basic monthly needs (n=184). Overall, 91% of women were from South Africa (n=391) whereas 9% reported being from other countries (e.g. Zimbabwe [n=21], Lesotho [n=12], Mozambique [n=6] and Swaziland [n=1]). Fifty-four percent of women reported that the father of the child was either non-cohabiting, a casual partner, or that they had no relationship (n=230); 46% of women were living with the father of the child or were married (n=199) and 5 women were widowed or divorced (1%). Although 62% of women (n=236) knew their HIV status before their first ANC visit, only 29% were virally suppressed (<400 copies/mL) at their first ANC visit. In addition, of women who knew their HIV status at first ANC, 12% had a CD4-cell count of <200 cells/mL. (Table 1).
Table 1.
Socio-demographic, clinical and behavioral characteristics of human immunodeficiency virus (HIV)-infected pregnant women, Tshwane, South Africa (n=430)
| Total (n, %) | ||
|---|---|---|
| Total | 430 | |
| Socio-demographic characteristics | ||
| Age (median, IQR) | 30 (26–34) | |
| Gestational age (median, IQR) | 20 (14, 25) | |
| Education | ||
| Less than secondary | 236 (55%) | |
| Secondary or greater | 194 (45%) | |
| Relationship with father of child | ||
| Married or cohabiting | 225 (53%) | |
| Non-cohabiting, casual partner or no relationship | 199 (46%) | |
| Widow or divorced | 5 (1%) | |
| Employment status (mother) | ||
| Full-time, part-time or self-employed | 178 (41%) | |
| Unemployed | 251 (59%) | |
| Clinical characteristics | ||
| Ever treated for a STI | 48 (11%) | |
| Knew HIV status before first ANC | 236 (62%) | |
| Ever treated for a STI | 48 (11%) | |
| Virally suppressed at last viral load done (<400 copies) | 124 (29%) | |
| Last known CD4 cell count (cells/mL) (median, IQR) | 397 (256–591) | |
| Sexual behaviour during pregnancy | ||
| Vaginal sex during pregnancy | 382 (89%) | |
| Fellatio sex during pregnancy | 12 (8%) | |
| Anal sex during pregnancy | 4 (3%) | |
| How long ago was last sex: | ||
| 0–7 days ago | 247 (58%) | |
| 8–30 days ago | 102 (23%) | |
| 31–60 days ago | 36 (9%) | |
| >60 days ago | 41 (10%) | |
| Male condom used at last sex among women reporting sex during pregnancy | ||
| Yes | 123 (32%) | |
| No | 259 (68%) | |
| Frequency of condom use since pregnant | ||
| All the time | 37 (15%) | |
| Sometimes | 80 (33%) | |
| Never | 127 (52%) | |
| Ever forced to have sex | 29 (7%) | |
| More than 1 sex partner in past 12-months | 77 (18%) | |
| Suspect partner has other partners | 153 (36%) | |
| Partner’s serostatus (reported) | ||
| Concordant HIV-positive | 103 (28%) | |
| Discordant | 74 (20%) | |
| Don’t know | 198 (53%) | |
| Alcohol consumption during pregnancy | ||
| Frequency of alcohol use since pregnant | ||
| Never | 365 (85%) | |
| Monthly or less | 47 (11%) | |
| 2+ times/month | 16 (4%) | |
| Among drinkers, quantity consumed when drinking alcohol since pregnant | ||
| 1–2 drinks | 28 (44%) | |
| 3–4 drinks | 19 (30%) | |
| 5+ drinks | 17 (26%) | |
| Frequency of 6+ drinks per session during pregnancy | 28 (44%) | |
| Among drinkers, reported uncontrollable drinking during pregnancy | 7 (11%) | |
Sexual behaviors and alcohol use during pregnancy
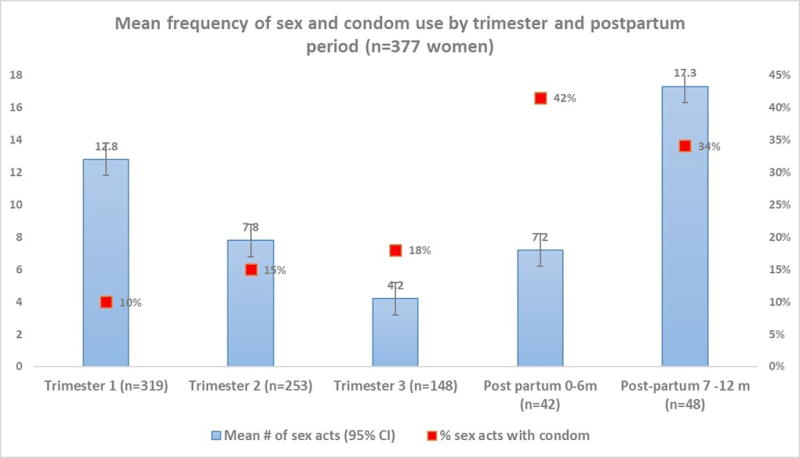
Overall, 89% (95% CI=86, 92%) of study participants reported having sex during pregnancy of whom 7.8% reported giving oral sex (95% CI=5.5, 11%) and 2.4% anal sex (95% CI=1.2, 4.8%) during pregnancy. Fifty-eight percent of sexually active women reported having sex within the 7-days prior to study enrolment, and 24% reported having sex in the past 8 and 30-days. Over 18% of women reported having more than one sexual partner in the past year (n=77). Of those, 63 (81%) reported having 1 additional partner, while 14 (18%) reported 2 or more partners. One-fifth of women reported that they were in a serodiscordant relationship, and 28% reported that their partner’s status was the same, i.e., concordant HIV-infected; the remaining 53% did not know their partner’s serostatus. Alcohol use during pregnancy, defined as consuming alcohol monthly or more frequently, was reported among 15% of women (95% CI=12, 19%) of whom 4% (n=16 women) reported drinking alcohol 2 or more times per month. Among drinkers, 44% (n=28 women) reported drinking 1–2 drinks when drinking alcohol since pregnant and 56% (n=36 women) said they drank 3 or more drinks when drinking during pregnancy. (Table 1).
Condom use during pregnancy
Of the pregnant women who reported having sex during pregnancy (n=382 women), 32% reported using a condom at last sex act (95% CI=28, 37%) and15% of women reported always using condoms during pregnancy. Adjusted for age, partnership status and income, condom use at last sex was associated with prior knowledge of HIV status (aOR=2.46, 95% CI=1.54, 3.92); having sex within the last 8–30 days vs. 0–7 days (aOR=1.71, 95% CI=1.04, 2.81); and being in a concordant (aOR=3.17, 95% CI=1.84, 5.50) or discordant relationship (aOR=6.50, 95% CI=3.59, 11.80) vs. not knowing partner’s serostatus. Age, education, relationship with father of the child and employment status were not associated with condom use at last sex (Table 2).
Table 2.
Factors associated with condomless sex at last sex during pregnancy in pregnant human immunodeficiency virus (HIV)-infected women in Tshwane, South Africa (n=382 sexually active pregnant women)
| Total (n, %)* | Condom used at last sex | Condomless sex at last sex | OR (95% CI) | Adjusted OR (95% CI)* | ||
|---|---|---|---|---|---|---|
| Total | 382 | 123 (32%) | 259 (68%) | |||
| Demographic characteristics | ||||||
| Age (median, IQR) | 30 (26–34) | 30 (26–34) | 30 (26–34) | 1.00 (0.96, 1.04) | 1.01 (0.94, 1.06) | |
| Education | ||||||
| Less than secondary | 208 (55%) | 66 (54%) | 142 (54%) | ref | ||
| Secondary or greater | 174 (45%) | 57 (46%) | 117 (45%) | 1.05 (0.68, 1.61) | ||
| Relationship with father of child | ||||||
| Steady partner (married, cohabiting) | 213 (56%) | 72 (58%) | 141 (54%) | 0.90 (0.59, 1.37) | 0.97 (0.65, 1.54) | |
| Occasional partner (no relationship, not cohabiting, casual partner) | 166 (43%) | 49 (40%) | 117 (45%) | ref | ref | |
| Divorced | 3 (1%) | 2 (2%) | 1 (1%) | |||
| Knew HIV status before this visit | ||||||
| Yes | 236 (62%) | 92 (75%) | 144 (56%) | 2.37 (1.47, 3.81) | 2.46 (1.54, 3.92) | |
| No | 146 (38%) | 31 (25%) | 115 (44%) | ref | ref | |
| Employment status (mother) | ||||||
| Full-time, part-time or self-employed | 160 (42%) | 55 (45%) | 105 (40%) | 1.19 (0.77, 1.83) | 1.06 (0.87, 1.94) | |
| Unemployed | 222 (58%) | 68 (55%) | 154 (60%) | ref | ref | |
| Father of child employed | 150 (67%) | |||||
| Full-time, part-time or self-employed | 210 (93%) | 75 (94%) | 135 (93%) | 1.22 (0.41, 3.65) | ||
| Unemployed | 16 (7%) | 5 (6%) | 11 (7%) | ref | ||
| Income per month | ||||||
| None | 37 (9%) | 8 (6%) | 29 (10%) | ref | ||
| <$80 per month | 132 (31%) | 40 (29%) | 92 (32%) | 1.58 (0.66, 3.74) | ||
| $81–$400 per month | 213 (50%) | 78 (57%) | 135 (46%) | 2.09 (0.91, 4.81) | ||
| $400–$800 per month | 38 (9%) | 10 (7%) | 28 (10%) | 1.29 (0.45, 3.76) | ||
| >$800 per month | 8 (2%) | 1 (1%) | 7 (2%) | 0.52 (0.04, 4.84) | ||
| Ever treated with STI | 48 (11%) | 16 (12%) | 32 (11%) | 1.06 (0.89, 1.28) | ||
| Sexual history | ||||||
| How long ago was last sex: | ||||||
| 0–7 days ago | 247 (65%) | 71 (58%) | 176 (68%) | ref | ref | |
| 8–30 days ago | 97 (25%) | 39 (32%) | 58 (22%) | 1.67 (1.02, 2.72) | 1.71 (1.04, 2.81) | |
| 31–60 days ago | 29 (7%) | 9 (7%) | 19 (7%) | 1.17 (0.51, 2.72) | 1.25 (0.59, 2.66) | |
| >60 days ago | 10 (3%) | 4 (3%) | 6 (2%) | 1.65 (0.45, 6.03) | 1.55 (0.74, 3.26) | |
| More than 1 sex partner during pregnancy | 69 (18%) | 22 (18%) | 48 (18%) | 0.99 (0.57, 1.74) | ||
| Suspect partner has other partners | 132 (35%) | 33 (27%) | 99 (38%) | 1.01 (0.94, 1.08) | ||
| Frequency of condom use since pregnant | ||||||
| All the time | 34 (15%) | 34 (41%) | 3 (2%) | ref | ref | |
| Sometimes | 78 (32%) | 41 (49%) | 37 (24%) | 0.10 (0.03, 0.35) | 0.10 (0.03, 0.34) | |
| Never | 125 (52%) | 8 (10%) | 117 (74%) | 0.01 (0.01, 0.02) | 0.01 (0.01, 0.02) | |
| Partner’s serostatus | ||||||
| Same (e.g. concordant HIV-positive) | 90 (27%) | 38 (36%) | 52 (23%) | 3.38 (1.92, 5.96) | 3.17 (1.84, 5.50) | |
| Different (e.g. discordant) | 67 (20%) | 37 (35%) | 30 (13%) | 5.70 (3.58, 10.55) | 6.50 (3.59, 11.80) | |
| Don’t know | 180 (53%) | 32 (30%) | 148 (64%) | ref | ref | |
| Alcohol consumption during pregnancy | ||||||
| Frequency of alcohol use since pregnant | ||||||
| Never | 320 (84%) | 104 (85%) | 216 (83%) | ref | ||
| Monthly or less | 46 (12%) | 16 (13%) | 30 (12%) | 1.11 (0.58, 2.12) | ||
| 2+ times/month | 16 (4%) | 3 (2%) | 13 (5%) | 0.50 (0.13, 1.72) | ||
| Among drinkers, quantity consumed when drinking alcohol | ||||||
| 1–2 drinks | 27 (44%) | 8 (42%) | 19 (44%) | ref | ||
| 3–4 drinks | 19 (31%) | 8 (42%) | 11 (26%) | 1.73 (0.51, 5.91) | ||
| 5+ drinks | 16 (26%) | 3 (16%) | 13 (30%) | 0.55 (0.12, 2.46) | ||
2 women were missing condom reporting
each variable was run independently adjusting for age, partnership status and income
bold: p<0.10
Prevalence of STIs in pregnancy
The prevalence of any STI was 41% (n=174). Overall, 17% of women had CT, 0.9% had NG, 10% had TV, 2.6% had CT and NG, 8.6% had CT and TV, 0.7% had NG and TV, and 1.4% had all three STIs at baseline (Figure 1). Of those women who reported not having sex during pregnancy, 42% tested positive for a STI (n=19 of 45).
Factors associated with STI prevalence during pregnancy
Odds of having a prevalent STI at first ANC visit decreased as age increased (OR/year=0.96; 95% CI= 0.93, 1.00, p=0.03). Young women age 18–24 years had the highest STI positivity (57%) compared to women age 25–35 years (37%) or those age >35 years (39%; OR comparing <25 to ≥25 years old=2.10, 95% CI=1.07, 4.09). Being employed decreased the odds of having any STI (OR=0.62, 95% CI=0.42, 0.92). If the father of the child was a non-cohabitating or casual partner, the odds of having a STI were 85% higher (OR=1.85, 95% CI=1.25, 2.74) though this associate was slightly attenuated after controlling for age and employment (aOR=1.42, 95% CI=0.97, 2.03, p=0.07). Reporting having sex five or more times during pregnancy by first ANC visit was also associated with having any STI after adjusting for age and employment (aOR=1.88, 95% CI=1.01, 3.49).
Of women who reported alcohol use during pregnancy (n=63 women), 44% reported six or more drinks per drinking session (n=28) and 11% reported that they were unable to stop drinking once they had started drinking during pregnancy (n=7). After adjusting for mothers’ age and employment, monthly or more frequent alcohol use during pregnancy was associated with being diagnosed with any STI (aOR=1.96, 95% CI=1.06, 3.64; Table 3).
Table 3.
Factors associated with any sexually transmitted infection (CT, NG and/or TV) in pregnant HIV-infected women in Tshwane, South Africa (n=430 women)
| Total (n, %) | No STI (n, %) | Any STI (n, %)* | OR (95% CI) | Adjusted OR (95% CI)** | ||
|---|---|---|---|---|---|---|
| Total | 430 | 256 (59%) | 174 (41%) | |||
| Socio-demographic characteristics | ||||||
| Age (median, IQR) | 30 (26–34) | 31 (27–35) | 29 (25–33) | 0.96 (0.93, 1.00) | 0.95 (0.90, 1.01) | |
| Gestational age (median, IQR) | 20 (14, 25) | 20 (14–24) | 21 (14–25) | 1.01 (0.98, 1.05) | ||
| Education | ||||||
| Less than secondary | 236 (55%) | 132 (52%) | 104 (60%) | ref | ||
| Secondary or greater | 194 (45%) | 124 (48%) | 70 (40%) | 0.72 (0.49, 1.06) | ||
| Relationship with father of child | ||||||
| Occassional partner (no relationship, not cohabiting or casual partner) | 199 (46%) | 103 (40%) | 96 (55%) | 1.52 (1.05, 2.20) | 1.42 (0.97, 2.03) | |
| Steady partner (married, cohabiting) | 225 (53%) | 148 (58%) | 77 (45%) | ref | ref | |
| Divorced or widowed | 5 (1%) | 5 (2%) | 0 (0%) | -- | -- | |
| Knew HIV status before this visit | ||||||
| Yes | 271 (63%) | 162 (63%) | 109 (63%) | 0.97 (0.65, 1.45) | ||
| No | 159 (37%) | 94 (37%) | 65 (37%) | |||
| Mother employed | ||||||
| Full-time, part-time or self-employed | 178 (41%) | 118 (46%) | 60 (35%) | 0.62 (0.42, 0.92) | 0.82 (0.44, 1.55) | |
| Unemployed | 251 (59%) | 138 (54%) | 113 (65%) | ref | ||
| Clinical characteristics | ||||||
| Virally suppressed at last viral load done (<400 copies) (n=234 missing) | 124 (63%) | 77 (69%) | 47 (55%) | 0.55 (0.04, 0.30) | 0.58 (0.32, 1.07) | |
| Last known CD4 <200 vs. =>200 cells/mL (n=114 missing) | 53 (17%) | 38 (20%) | 15 (12%) | 1.12 (0.76, 1.65) | ||
| Ever diagnosed with STI | 48 (11%) | 34 (13%) | 14 (8%) | 0.89 (0.71, 1.10) | ||
| Sexual history | ||||||
| Sex during pregnancy (yes vs. no) | 382 (89%) | 228 (89%) | 154 (89%) | 1.00 (0.54, 1.85) | ||
| Fellatio during pregnancy | 30 (8%) | 18 (8%) | 12 (8%) | 0.99 (0.47, 2.11) | ||
| Anal sex during pregnancy | 9 (2%) | 5 (2%) | 4 (3%) | 1.19 (0.31, 4.50) | ||
| How long ago was last sex: | ||||||
| 0–7 days ago | 247 (58%) | 150 (59%) | 97 (57%) | 0.62 (0.32, 1.20) | 0.82 (0.31, 1.21) | |
| 8–30 days ago | 102 (23%) | 59 (23%) | 43 (25%) | 0.69 (0.34, 1.44) | 0.67 (0.32, 1.40) | |
| 31–60 days ago | 36 (9%) | 26 (10%) | 10 (6%) | 0.37 (0.14, 0.95) | 0.35 (0.13, 0.92) | |
| >60 days ago | 41 (10%) | 20 (8%) | 21 (12%) | ref | ref | |
| Sex frequency during pregnancy | ||||||
| >5 times vs. ≤5 times | 95 (51%) | 54 (46%) | 41 (60%) | 1.80 (0.98, 3.30) | 1.88 (1.01, 3.49) | |
| More than 1 sex partner during pregnancy | 77 (18%) | 46 (18%) | 31 (18%) | 0.99 (0.60, 1.64) | ||
| Suspect partner has other partners | 153 (36%) | 89 (35%) | 64 (37%) | 1.00 (0.94, 1.06) | ||
| Condom use at last sex | 137 (32%) | 82 (32%) | 55 (32%) | 0.98 (0.65, 1.49) | ||
| Frequency of condom use since pregnant | ||||||
| All the time | 37 (15%) | 25 (17%) | 12 (13%) | ref | ||
| Sometimes | 80 (33%) | 42 (28%) | 38 (40%) | 1.88 (0.83, 4.26) | ||
| Never | 127 (52%) | 81 (55%) | 46 (48%) | 1.18 (0.54, 2.57) | ||
| Partner’s serostatus | ||||||
| Same (e.g. concordant HIV-positive) | 103 (28%) | 59 (27%) | 44 (29%) | 1.10 (0.68, 1.78) | ||
| Different (e.g. discordant) | 74 (20%) | 44 (20%) | 30 (20%) | 1.01 (0.58, 1.73) | ||
| Don’t know | 198 (53%) | 118 (53%) | 80 (51%) | ref | ||
| Alcohol consumption during pregnancy | ||||||
| Frequency of alcohol use since pregnant | ||||||
| Never | 365 (85%) | 224 (88%) | 141 (81%) | ref | ||
| Monthly or more frequently | 65 (15%) | 33 (13%) | 33 (19%) | 1.97 (1.07, 3.63) | 1.48 (0.67, 3.27) | |
| Among drinkers, quantity consumed when drinking alcohol during pregnancy | ||||||
| 1–2 drinks | 28 (44%) | 15 (50%) | 12 (38%) | ref | ||
| 3–4 drinks | 19 (30%) | 6 (19%) | 13 (41%) | 2.89 (0.85, 9.82) | ||
| 5+ drinks | 17 (27%) | 10 (31%) | 7 (22%) | 0.93 (0.28, 3.17) | ||
missing values if does not equal total n
each variable was run independently adjusting for age and employment
bold: p<0.10
Discussion
Our research investigated sexual behaviors, alcohol use and factors associated with condomless sex during pregnancy and prevalent STI among HIV-infected pregnant women in Tshwane District, South Africa. By their first ANC visit, almost all women reported having vaginal sex during pregnancy, with the majority having sex within the week prior to study enrollment. Over one-quarter of participants reported being in a seroconcordant relationship with a seropositive male partner, one-fifth reported they were in a serodisconcordant relationship with a seronegative male partner, and more than half did not know their partner’s serostatus. Our study identified significant behavioral risks for HIV and STI transmission during pregnancy including frequent condomless vaginal sex with a serodiscordant partner or partners of unknown serostatus and heavy alcohol use during pregnancy. We found that two-thirds of the participants did not use a condom at their last sexual encounter during pregnancy. Overall, 73% of women were in serodiscordant relationships or did not know the serostatus of their sexual partner(s), and most of those women did not use a condom at last sex. Only 15% of HIV-infected pregnant women reported always using condoms during pregnancy and 18% of women reported having one or more partner in the past 12-months. Adjusting for age, income and relationship status, prior knowledge of HIV-positive serostatus and knowledge of partner’s serostatus (being discordant or concordant positive) at first ANC visit were associated with condom use at last sex during pregnancy. Finally, our study found that alcohol consumption during pregnancy, not in a casual or non-cohabiting relationship with the father of the child, and sexual frequency (≥5 sex acts during pregnancy by first ANC visit) were associated with increased odds of prevalence of any STI.
To the best of our knowledge, our study is one of the first to report factors associated with condomless sex and STIs in HIV-infected pregnant women in South Africa. Condom use during pregnancy in South Africa is important in a context of high secondary HIV transmission and STI acquisition during pregnancy. Of concern, we found that women who did not know their partner’s serostatus had increased odds of not using a condom at last sex. Prior research found that women have difficulty talking about condom use and HIV with their partners, especially with occasional partners, which increases their vulnerability to HIV and STI acquisition.27 Our analysis demonstrated that pregnant women with non-cohabitating or casual partners were likely to report having condomless sex at last sex act. We also found that among women who reported condomless sex at last sex, many also reported that they “always” used condom use during pregnancy, highlighting the potential social desirability bias, and potential for over-reporting of condom use in our study.
Though relationship status was not associated with condom use, it was an important predictor of having a STI in pregnancy. In multivariable analyses, if the father of the child was a casual or non-cohabiting partner, the odds of having a STI were 42% higher than a regular, cohabiting partner. That result is similar to prior studies conducted among HIV-uninfected persons, which found that relationship status plays an important role in the transmission of STIs.21 Research among HIV-infected and uninfected pregnant women in Mpumalanga, South Africa, revealed that HIV-infection, physical violence by a partner in the past 6-months, and psychological distress were associated with having an STI.21 Further, given that participants in our study had a high viral load at first ANC visit (only 29% of pregnant women were virally suppressed at first ANC), they may be at increased risk of vertical HIV transmission because of viremia and active, untreated STIs.13, 15
Overall 16% of pregnant women reported alcohol consumption during pregnancy. Alcohol consumption in pregnant and postpartum women was evaluated in recent study in South Africa which identified that 26% of women reported alcohol use prior to pregnancy, though most women had reduced alcohol intake during pregnancy.28 In our study, alcohol consumption in pregnancy was also associated with having a STI at first ANC visit. Similarly, a study among HIV-positive pregnant women in KwaZulu-Natal, South Africa, reported that prior STI treatment and increased number of sexual partners were associated with alcohol use.22 Heavy alcohol use in serodiscordant couples was associated with increased risk of HIV acquisition and lower odds of initiating ART in HIV-infected female heavy drinkers in Zambia.20 In addition to being associated with odds of having a STI, heavy alcohol use is detrimental to fetal development during pregnancy. As a result, we recommend that women receive targeted counseling on the risks associated with alcohol use during ANC.
Our study findings support the need for targeted interventions to prevent, diagnose and treat STIs in pregnant women, especially in HIV-infected pregnant women. However, lack of healthcare resources in South Africa29 could make it difficult to implement standardized rapid molecular screening for CT, NG, and TV among all HIV-infected pregnant women. Tools could be developed to assess STI risk to improve targeted delivery of STI diagnostic tests. Our study demonstrates the important role that partner dynamics and alcohol use play in determining condom use during pregnancy and STI acquisition.
This was a cross-sectional study and may be subject to recall bias with past behaviors or symptoms. Survey questions on sexual behavior, sexual history, and alcohol use could be influenced by social desirability or reporting biases especially in pregnant women interviewed by healthcare staff. Our study used standardized instruments when available (e.g. AUDIT for alcohol measures) but in sexual behavior questions they were not available which may affect the external validity of the findings to other African populations.
HIV-infected pregnant women are at high risk for prevalent STIs, and for transmitting both HIV and STIs to their partners and newborns. We identified high rates of condomless sex, multiple partners and alcohol use during pregnancy in our study population. Lack of knowledge of HIV status, and/or the father of the child’s serostatus actors was associated with condomless sex during pregnancy. Factors associated with prevalent STI in pregnancy included: younger age, unemployment, casual or non-cohabiting partner and alcohol use during pregnancy. Those findings may help inform the design of targeted interventions that address the burden of STIs during pregnancy and reduce vertical and horizontal HIV and STI transmission.
Summary.
Our study of HIV-infected pregnant women in South Africa describes sexual behaviors during pregnancy and factors associated with having a sexually transmitted infection including alcohol use during pregnancy and relationship status.
Acknowledgments
We wish to thank all the clinicians who worked on the study and all of the women who participated in the study. We received funding from NIH-NICHD- R21HD084274-01. Dvora Joseph Davey received support from a T32 post-doctoral fellowship with University of California, Los Angeles (NIH-NIAID-T32MH080634-11). Noah Kojima is supported by the Fogarty International Center of the National Institutes of Health (NIH) under award number D43TW009343 and the University of California Global Health Institute (UCGHI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or UCGHI.
References
- 1.World Health Organization. GLOBAL HEALTH SECTOR STRATEGY ON SEXUALLY TRANSMITTED INFECTIONS, 2016–2021. Geneva, Switzerland: WHO Document Production Services; 2016. [Google Scholar]
- 2.Silver BJ, Guy RJ, Kaldor JM, et al. Trichomonas vaginalis as a cause of perinatal morbidity: a systematic review and meta-analysis. Sex Transm Dis. 2014;41(6):369–76. doi: 10.1097/OLQ.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 3.Adachi K, Klausner JD, Xu J, et al. Chlamydia trachomatis and Neisseria gonorrhoeae in HIV-infected Pregnant Women and Adverse Infant Outcomes. Pediatr Infect Dis J. 2016;35(8):894–900. doi: 10.1097/INF.0000000000001199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adachi K, Nielsen-Saines K, Klausner JD. Chlamydia trachomatis Infection in Pregnancy: The Global Challenge of Preventing Adverse Pregnancy and Infant Outcomes in Sub-Saharan Africa and Asia. Biomed Res Int. 2016;2016:9315757. doi: 10.1155/2016/9315757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cotch MF, Pastorek JG, 2nd, Nugent RP, et al. Trichomonas vaginalis associated with low birth weight and preterm delivery. The Vaginal Infections and Prematurity Study Group. Sex Transm Dis. 1997;24(6):353–60. doi: 10.1097/00007435-199707000-00008. [DOI] [PubMed] [Google Scholar]
- 6.McClelland RS, Sangare L, Hassan WM, et al. Infection with Trichomonas vaginalis increases the risk of HIV-1 acquisition. The Journal of infectious diseases. 2007;195(5):698–702. doi: 10.1086/511278. [DOI] [PubMed] [Google Scholar]
- 7.Workowski KA, Bolan GA, et al. Centers for Disease C. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(RR-03):1–137. [PMC free article] [PubMed] [Google Scholar]
- 8.Hammerschlag MR. Chlamydial and gonococcal infections in infants and children. Clin Infect Dis. 2011;53(Suppl 3):S99–102. doi: 10.1093/cid/cir699. [DOI] [PubMed] [Google Scholar]
- 9.Schachter J, Grossman M, Holt J, et al. Prospective study of chlamydial infection in neonates. Lancet. 1979;2(8139):377–80. doi: 10.1016/s0140-6736(79)90400-8. [DOI] [PubMed] [Google Scholar]
- 10.Schachter J, Grossman M, Sweet RL, et al. Prospective study of perinatal transmission of Chlamydia trachomatis. JAMA. 1986;255(24):3374–7. [PubMed] [Google Scholar]
- 11.Wasserheit JN. Epidemiological synergy. Interrelationships between human immunodeficiency virus infection and other sexually transmitted diseases. Sex Transm Dis. 1992;19(2):61–77. [PubMed] [Google Scholar]
- 12.Masson L, Mlisana K, Little F, et al. Defining genital tract cytokine signatures of sexually transmitted infections and bacterial vaginosis in women at high risk of HIV infection: a cross-sectional study. Sex Transm Infect. 2014;90(8):580–7. doi: 10.1136/sextrans-2014-051601. [DOI] [PubMed] [Google Scholar]
- 13.Cohen MS. Sexually transmitted diseases enhance HIV transmission: no longer a hypothesis. Lancet. 1998;351(Suppl 3):5–7. doi: 10.1016/s0140-6736(98)90002-2. [DOI] [PubMed] [Google Scholar]
- 14.Levine WC, Pope V, Bhoomkar A, et al. Increase in endocervical CD4 lymphocytes among women with nonulcerative sexually transmitted diseases. J Infect Dis. 1998;177(1):167–74. doi: 10.1086/513820. [DOI] [PubMed] [Google Scholar]
- 15.Adachi K, Klausner JD, Bristow CC, et al. Chlamydia and Gonorrhea in HIV-Infected Pregnant Women and Infant HIV Transmission. Sex Transm Dis. 2015;42(10):554–65. doi: 10.1097/OLQ.0000000000000340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fawzi W, Msamanga G, Renjifo B, et al. Predictors of intrauterine and intrapartum transmission of HIV-1 among Tanzanian women. AIDS. 2001;15(9):1157–65. doi: 10.1097/00002030-200106150-00011. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. Briefing Note 16.09.2015. World Health Organization; 2015. Proposing 2016–2021 Global Health Sector Strategies for HIV, viral hepatitis and Sexually Transmitted Infections (STIs). Global Health Sector Strategies 2016–2021. [Google Scholar]
- 18.South African National Department of Health. [accessed on February 20, 2018];National Consolidated Guidelines for the Prevention of Mother-to-Child Transmission of HIV (PMTCT) and the Management of HIV in Children, Adolescents and Adults. 2015 Apr; http://www.sahivsoc.org/Files/ART%20Guidelines%2015052015.pdf.
- 19.Drake AL, Wagner A, Richardson B, John-Stewart G. Incident HIV during Pregnancy and Postpartum and Risk of Mother-to-Child HIV Transmission: A Systematic Review and Meta-Analysis. PLoS Med. 2014;11(2) doi: 10.1371/journal.pmed.1001608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joseph Davey D, Kilembe W, Wall KM, Khu NH, Brill I, Vwalika B, Chomba E, Mulenga J, Tichacek A, Javanbakht M, Comulada WS, Allen S, Gorbach PM. Risky Sex and HIV Acquisition Among HIV Serodiscordant Couples in Zambia, 2002–2012: What Does Alcohol Have To Do With It? AIDS Behav. 2017 Jul;21(7):1892–1903. doi: 10.1007/s10461-017-1733-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peltzer K, Mlambo G. Sexual HIV risk behaviour and associated factors among pregnant women in Mpumalanga, South Africa. BMC Pregnancy Childbirth. 2013;13:57. doi: 10.1186/1471-2393-13-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Desmond K, Milburn N, Richter L, et al. Alcohol consumption among HIV-positive pregnant women in KwaZulu-Natal, South Africa: prevalence and correlates. Drug Alcohol Depend. 2012;120(1–3):113–8. doi: 10.1016/j.drugalcdep.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mudau M, Peters RP, De Vos L, et al. High prevalence of asymptomatic sexually transmitted infections among human immunodeficiency virus-infected pregnant women in a low-income South African community. Int J STD AIDS. 2017 doi: 10.1177/0956462417724908. 956462417724908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test, Guidelines for Use in Primary Care. 2. Geneva, Switzerland: Department of Mental Health and Substance Dependence, World Health Organization; 2001. [Google Scholar]
- 25.Lunny C, Taylor D, Hoang L, et al. Self-Collected versus Clinician-Collected Sampling for Chlamydia and Gonorrhea Screening: A Systemic Review and Meta-Analysis. PLoS One. 2015;10(7):e0132776. doi: 10.1371/journal.pone.0132776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.South African National Department of Health. [Accessed October 28, 2017];Sexually Transmitted Infections Management Guidelines. 2015 Jun; Available from: https://www.idealclinic.org.za/docs/National-Priority-Health-conditions/Sexually%20Transmitted%20Infections_%20Management%20Guidelines%202015.pdf.
- 27.Maman S, Moodley D, McNaughton-Reyes HL, Groves AK, Kagee A, Moodley P. Efficacy of enhanced HIV counseling for risk reduction during pregnancy and in the postpartum period: a randomized controlled trial. PLoS One. 2014 May 13;9(5):e97092. doi: 10.1371/journal.pone.0097092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Davis EC, Rotheram-Borus MJ, Weichle TW, Rezai R, Tomlinson M. Patterns of Alcohol Abuse, Depression, and Intimate Partner Violence Among Township Mothers in South Africa Over 5 Years. AIDS Behav. 2017 Nov;21(Suppl 2):174–182. doi: 10.1007/s10461-017-1927-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mayosi BM, Benatar SR. Health and health care in South Africa-20 years after Mandela. The New England journal of medicine. 2014;371(14):1344–53. doi: 10.1056/NEJMsr1405012. [DOI] [PubMed] [Google Scholar]


