Abstract
Context
Secondhand smoke exposure (SHSe) affects up to half of all children in the United States. Many studies have identified factors associated with in-home SHSe, but few have contrasted these factors between households with and without residential smokers. In the latter case, exposure occurs from only external sources that enter the home, such as visitors or environmental incursion.
Objective
Among children with SHSe at home, to examine demographic and psychosocial differences between households with and without residential smokers.
Design
Baseline analysis of an observational cohort.
Setting
Baltimore City, Maryland.
Participants
157 children with asthma, ages 5–12.
Measures
At-home airborne nicotine; caregiver-reported depression, asthma-related quality of life, functional social support, and demographics. Univariable comparisons were performed between SHS-exposed households with and without residential smokers. Multivariable logistic regression models were fit to examine associations between measured factors and absence of residential smokers.
Results
78.3% of children had at-home SHSe. Of these, 40.7% lived in households without residential smokers. Compared to households with residential smokers, these caregivers endorsed stronger beliefs in SHS harms, but also worse functional social support and asthma-related stress, despite no differences in asthma morbidity. In adjusted models, SHS-exposed children with caregivers in the lowest tertile of functional social support (aOR 3.50; 95% CI 1.12–10.99), asthma-related quality of life (2.90; 1.06–7.95), and those living alone (5.28; 1.26–22.15), had at least twice higher odds of having exclusively external SHSe compared to the highest tertile (P-trends<0.05).
Conclusions
In-home SHS exposure remains alarmingly high in urban environments. However, a substantial proportion of this exposure appears to be occurring only from external sources that enter the home. Caregivers in these homes had higher desire but lower agency to avoid SHSe, driven by lack of functional support and physical isolation. Public policies targeting these factors may help remediate exposure in this especially vulnerable population.
Keywords: secondhand smoke exposure, asthma, smoking bans, epidemiology, health behavior
INTRODUCTION
Secondhand smoke (SHS) is a common indoor air pollutant. Despite comprehensive knowledge of its harmful effects, approximately half of all children, and as high as seventy percent of African American children, remain exposed in the United States1,2. SHS exposure is particularly detrimental to those who have asthma, where its occurrence is associated with worsened disease control, diminished pulmonary function, and increased rates of hospitalization3,4.
The majority of children are exposed to SHS at home, and the most common source of in-home SHS are household members, such as smoking parents5,6. However, children can also be exposed at home from external sources: smoking visitors6, incursion of SHS from the outside environment7,8, and attendant “thirdhand” smoke from these elements9.
Although many studies have examined factors that predict in-home SHS exposure in children10, these have largely treated exposure as a unitary outcome. Importantly, we recognize that a distinct subset of exposed children are living in households without residential smokers, being exposed from exclusively external sources that enter the home. We hypothesize that there will be differences in demographic, psychosocial, and medical factors between these households and households with residential smokers, where children are being exposed from a mix of familial and external sources. For instance, poor parental health-related quality of life11, social status12,13, and residence in single-parent households12,14, which have all been associated with a higher likelihood of in-home SHS exposure in general, may be unevenly distributed between these two types of homes.
Identification of factors associated with the absence of residential smokers among households with SHS, representing families who are able to maintain partial SHS remediation, may be informative of potential barriers for full SHS removal in these homes. Additionally, identified factors may also guide discussion on legislation and public policies on smoking bans.
To explore possible differences between SHS-exposed children living in households with and without residential smokers, we examined baseline data from the Discover study, an environmental observational cohort of inner-city children with asthma.
METHODS
Study Design and Participant Recruitment
The Discover study is an environmental cohort study of 162 children with asthma recruited from Baltimore City, Maryland. Participants were (1) aged 5–12, (2) had a physician diagnosis of intermittent or persistent asthma, and (3) had rescue inhaler use in the preceding six months. Participants were excluded if they were primary smokers or had another major pulmonary condition.
Participants and their principal caregivers were recruited from outpatient pulmonary clinics in the Johns Hopkins Pediatric Outpatient Clinics, the Johns Hopkins Pediatric Emergency Department, and from participant lists from prior asthma studies performed by local investigators. Enrolled participants and their primary caregivers presented for a baseline clinic visit, where sociodemographic information and health and psychosocial questionnaires were recorded with assistance of research staff. Participants then underwent home environmental monitoring, including assessment of airborne nicotine, over a week-long period. Written informed consent was obtained from all primary caregivers and assent was obtained from all participants. This study was approved by the Institutional Review Board of the Johns Hopkins School of Medicine.
Secondhand Smoke Exposure
Presence of household residential smokers was assessed by questionnaire. During the baseline clinic visit, caregivers were asked if any individuals who lived in the home smoked in the past month and to identify if these individuals were the mother, father, or others. Answers to these questions were summed to represent the total number of smokers living in the home.
During the environmental monitoring period, in-home airborne nicotine was measured. A passive monitor, containing a sodium bisulfite treated filter in a cassette, was placed in the room where the participant reported spending the most time (most often the bedroom)15. Filters were subsequently extracted, and the amount of nicotine was measured by gas chromatography-mass spectroscopy with a nitrogen phosphorus detector. Time weighted average concentrations of nicotine were calculated by dividing the amount of nicotine collected by the volume of air sampled16. The limit of detection was 0.034 μg/m3.
Participant and Caregiver Characteristics
Demographic, socioeconomic, and household characteristics were provided by the caregiver. Asthma morbidity was assessed by participant symptoms and healthcare utilization, using questions derived from other studies of inner-city asthma. Asthma symptomatology was described using the “maximum asthma symptom-day” as defined in the National Cooperative Inner-City Asthma Study17. This is the largest value among the number of days in the prior two weeks the participant had (1) wheezing, coughing, or tightness in the chest, (2) slowed activity due to asthma, and (3) nocturnal awakening. For example, a participant with three days of wheezing, five days of slowed activity, and two days of nocturnal awakening in the prior two weeks would have a maximum symptom-day value of five. Participants were considered to have had healthcare utilization if they needed emergency department services, experienced a hospitalization, or had an unscheduled physician visit due to their asthma in the previous three months.
Caregiver belief in the harms of SHS was assessed by asking their agreement with the statement that their child’s asthma will be better controlled by avoiding cigarette smoke, with responses scored on a 5-point Likert scale ranging from strongly disagree to strongly agree.
Asthma health-related quality of life was assessed by the Children’s Health Survey for Asthma (CHSA)18. This instrument measures five asthma-related domains: emotional health of child, emotional health of family, activity limitation on child, activity limitation on family, and physical health of child. The physical health domain was not assessed by the CHSA in this study. The emotional health of family, assessed by a 17-item subscale, ascertained a caregiver’s distress over their child’s asthma with questions such as “My child’s asthma caused stress in the family,” “Sometimes I lose hope that my child will get better,” and “I am bothered by getting my child to take asthma medications.” Responses were on a 5-point Likert scale, which were grouped according to domain and transformed to a scale of 0–100, with higher numbers indicating improved functioning within that domain. The internal consistency of the subscales in our sample was high (Cronbach’s α = 0.86–0.93).
Caregiver depression was ascertained through the Center for Epidemiological Studies Depression scale (CES-D). This instrument, validated in a representative population19, was presented in the shortened 11-question form20. A score of ≥9 was considered to reflect clinically significant depressive symptoms. The internal consistency in our sample was high (Cronbach’s α = 0.82).
Caregiver social support was assessed by a modified form of the Duke-UNC Functional Social Support Questionnaire (FSSQ)21. This 14-item instrument measures four domains of functional support: quantity of support, variety of confidants, amount of affection, and availability of instrumental support (e.g. assistance when ill or help with transportation). In the modified version, two questions relating to opportunities to speak about problems at work and in personal life were combined, and an additional question of availability of babysitter support was added. Caregivers answered questions on a simplified Likert-type scale, from 1 (never) to 3 (most of the time). Scores were averaged across all domains, with a higher score indicating better social support. The internal consistency in our sample was high (Cronbach’s α = 0.88).
Statistical Analysis
Because our primary objective was to explore differences among homes with SHS exposure, we examined cases with detectable airborne nicotine during the environmental monitoring period. A household was considered to be exclusively externally exposed to SHS if there was detectable airborne nicotine but no disclosed residential smokers living in the home.
Data were initially analyzed descriptively and distributions were assessed graphically. Differences between SHS-exposed households with and without residential smokers were statistically compared with χ2 tests, in the case of categorical variables, and Wilcoxon rank-sum tests, in the case of continuous variables. Validity of caregiver-reported presence of residential smokers was assessed by a Cuzick’s test for trend for increasing airborne nicotine levels with higher numbers of reported smokers living in the home.
Multivariable logistic regression models were constructed to examine the association between caregiver reported factors and the odds of an in-home SHS-exposed child living in a household without residential smokers. The base model included demographic variables: participant age, sex, self-identified race (black/other), sibling status (0–1, 2, 3, 4 or more), insurance status (public/other); caregiver age, relationship (birth mother/other), education level (less than high school/completed high school/postsecondary education), unemployment status (considered unemployed if answered laid off, seeking work, disabled, or other); and number of adults in home (1, 2, 3 or more). One caregiver’s age was not disclosed and was imputed as the mean age of all birth mothers in this cohort; removal of this observation did not substantively modify any results. Family income was not included due to high levels of non-response. Of the households who reported income status, there was moderate correlation with education level (Spearman’s ρ = 0.47).
Additional models then added each psychosocial measure separately to these base variables. Measure scores were divided into tertiles or dichotomized, depending on distribution. Tests for linear trend across quantiles were performed in separate regression models where each participant was assigned the midpoint score in their quantile. All statistical analyses were performed in Stata 13 (StataCorp; College Station, TX).
RESULTS
Environmental Measurements
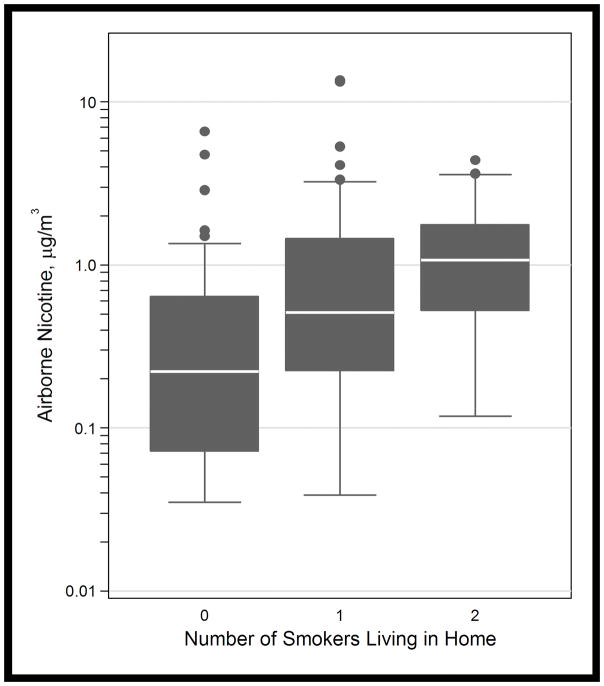
Of the 162 participants, 157 had available environmental monitoring data at the baseline visit. Airborne nicotine was detected in the majority of homes (123, 78%). Of the homes with detectable air nicotine, nearly half did not have residential smokers (50, 41%). These households had a median (interquartile range) air nicotine concentration of 0.22 (0.07–0.64) μg/m3 compared to 0.78 (0.30–1.68) μg/m3 in households with residential smokers (p-value <0.001, Wilcoxon rank-sum). The average concentration of airborne nicotine increased with higher numbers of reported smokers (p-value <0.001, Cuzick’s test for trend) (Figure 1).
FIGURE 1.
In-home airborne nicotine concentrations by self-reported number of smokers living in the home. A Cuzick’s test for trend across number of smoker categories was significant (p<0.001).
Homes were classified as row homes (85, 69%), apartments (21, 17%), and detached or semi-detached properties (17, 14%). A Kruskal-Wallis test indicated no statistically significant differences in median concentrations of airborne nicotine by home type.
Participant and Caregiver Characteristics
The majority of participants with in-home SHS exposure were African American (112, 91.1%), received public insurance (111, 90.2%), and had two or more siblings (95, 60.5%). Their caregivers were most often the birth mother (105, 85.4%) and lived with at least another adult in the household (95, 77.2%). Although the majority of caregivers reported attaining at least a high school education (86, 70.0%), approximately one-third were unemployed (46, 37.4%). Of the 72 caregivers who disclosed annual income (accounting for 58.5% of dyads), the majority were below $25,000 (53, 73.6%). Almost all caregivers endorsed some agreement with the importance of avoiding cigarette smoke (104/122, 85.3%). These characteristics were statistically similar to households without detectable nicotine (results not shown).
On average, nearly half of participants experienced an unanticipated health care contact due to asthma in the preceding three months (49, 40%), and participants reported asthma symptoms for an average of three days in the previous two weeks. However, approximately half of caregivers reported no limitation in their family’s activities (62, 50.4%) or their child’s activities (61, 49.6%) due to asthma, scoring the scale maximum in the activity limitation on family and child domains of the CHSA. Approximately one-third of caregivers in our study had clinically significant depressive symptoms during the baseline interview, scoring ≥9 on the CES-D scale (38, 30.7%).
Bivariable Analysis
Compared to households with residential smokers, SHS-exposed children living in households without residential smokers were more likely to have caregivers who strongly agree that avoidance of cigarette smoke is important for their child’s asthma health (42.9% vs. 24.7%, Fisher’s exact p-value <0.05) (Table 1). Participants in SHS-exposed households without residential smokers were also more likely to be male. Although SHS-exposed households without residential smokers had lower concentrations of airborne nicotine than households with residential smokers, participants did not have statistically significant differences in asthma symptom burden and rates of healthcare utilization over the recall period.
TABLE 1.
Participant and Caregiver Characteristics in Homes with SHS Exposure
| Characteristic, no (%) | Smoker Living in Home | P-value | |
|---|---|---|---|
|
| |||
| Yes (n=73) | No (n=50) | ||
| Child | |||
| Age (years), mean±SD | 8.6±2.3 | 9.1±2.3 | 0.20 |
| Male | 32 (43.8) | 31 (62.0) | <0.05 |
| African American | 67 (91.8) | 45 (90.0) | 0.73 |
| Public Insurance | 69 (94.5) | 42 (84.0) | 0.05 |
| Number of Siblings | 0.09 | ||
| None or one | 16 (21.9) | 12 (24.0) | |
| Two | 13 (17.8) | 18 (36.0) | |
| Three | 17 (23.3) | 9 (18.0) | |
| Four or more | 27 (37.0) | 11 (22.0) | |
| Asthma Morbidity | |||
| Maximum symptom-days*, mean±SD | 3.6±4.7 | 3.0±3.8 | 0.76 |
| Unscheduled healthcare need†, no (%) | 32 (43.8) | 17 (34.0) | 0.27 |
|
| |||
| Caregiver | |||
| Age (years), mean±SD | 36.1±10.0 | 35.4±9.6 | 0.87 |
| Relationship to Child | 0.49 | ||
| Birth mother | 61 (83.6) | 44 (88.0) | |
| Other | 12 (16.4) | 6 (12.0) | |
| Education Level | 0.22 | ||
| Not high school graduate | 25 (34.3) | 12 (24.0) | |
| High school graduate | 35 (48.0) | 23 (46.0) | |
| Some postsecondary education | 13 (17.8) | 15 (13.0) | |
| Annual Household Income | 0.15 | ||
| Less than $25,000 | 36 (49.3) | 17 (34.0) | |
| $25,000 – $50,000 | 8 (11.0) | 6 (12.0) | |
| More than $50,000 | 1 (1.4) | 4 (8.0) | |
| Declined to provide | 28 (38.4) | 23 (46.0) | |
| Unemployed | 29 (39.7) | 17 (34.0) | 0.52 |
| Number of Adults in Home | 0.22 | ||
| One | 14 (19.2) | 14 (28.0) | |
| Two | 42 (57.5) | 30 (60.0) | |
| Three or more | 17 (23.3) | 6 (12.0) | |
| Cigarette Smoke Harmful‡, no (%) | <0.05 | ||
| Strongly agree | 18 (24.7) | 21 (42.9) | |
| Agree | 46 (63.0) | 19 (38.8) | |
| Neutral or disagree | 9 (12.3) | 9 (18.4) | |
Maximum of days of (1) cough, wheezing, chest tightness, (2) limited activity due to cough, wheezing, chest tightness, and (3) nocturnal awakening trouble breathing, in the prior 2 weeks
Needed oral steroids, emergency department care, or unscheduled physician visit for asthma, in the prior 3 months
Answer to “my child’s asthma will be better controlled by avoiding cigarette smoke,” n=122, Fisher’s exact
With respect to the psychosocial scales, caregivers living in SHS-exposed households without residential smokers had lower family emotional health scores, indicating poorer emotional health, and lower social support scores, indicating worse social support. There were no differences in the proportion of caregivers disclosing depressive symptoms between groups (Table 2).
TABLE 2.
Psychosocial Scales of Caregivers in Homes with SHS Exposure
| Survey Score, mean±SD | Smoker Living in Home | P-value | |
|---|---|---|---|
|
| |||
| Yes (n=73) | No (n=50) | ||
| Health-Related Quality of Life (CHSA)* | |||
| Child’s Activities | 87.0±18.6 | 80.2±24.3 | 0.11 |
| Family’s Activities | 90.9±14.8 | 88.8±17.8 | 0.21 |
| Child’s Emotional Health | 75.2±30.7 | 66.4±31.5 | 0.11 |
| Family’s Emotional Health | 80.3±15.3 | 72.4±16.3 | <0.01 |
| Social Support (FSSQ)† | 2.54±0.40 | 2.39±0.39 | <0.05 |
| Depressive Symptoms, no (%) (CES-D)‡ | 24 (32.9) | 14 (28.0) | 0.57 |
Children’s Health Survey for Asthma, on a scale of 1–100, with higher indicating better quality of life
Duke-UNC Functional Social Support Questionnaire, on a scale of 1–3, with higher indicating more support
Center for Epidemiological Studies Depression Scale, proportion of those with clinically significant depression
Multivariable Analysis
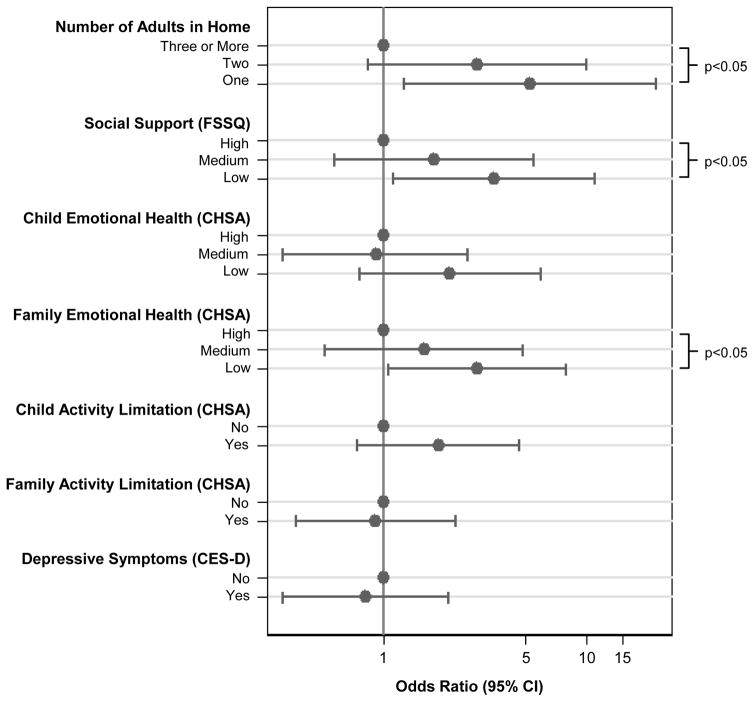
All relevant model results are plotted in Figure 2. In the base multivariable model, decreasing numbers of adults living in the household was associated with increased odds of the SHS-exposed child living in a household without residential smokers (p-value for linear trend 0.024). Compared to a household with three or more adults, a SHS-exposed child living in a household with a single adult had approximately five times the odds of the household having no residential smokers (aOR 5.28; 95% CI 1.26–22.15).
FIGURE 2.
Association of each factor with odds of the SHS-exposed household having no residential smokers. Scales are divided into tertiles or dichotomized. With respect to child emotional health, the highest tertile represents 34% of participants with a score of 100 (the scale maximum). With respect to child and family activity limitation, “No” indicates a score of 100 (the scale maximum). P-values indicate a test for linear trend across tertiles. The base model controlled for participant age, gender, race, insurance status, sibling status; caregiver age, relationship to participant, education level, unemployment status; and number of adults in the home. Psychosocial scale estimates are from separate models that include that scale in addition to base model predictors. CHSA = Children’s Health Survey for Asthma. FSSQ = Duke-UNC Functional Social Support Scale. CES-D = Center for Epidemiological Studies Depression Scale.
In full models, each with a different psychosocial scale in addition to the variables in the base model, SHS-exposed children with caregivers in the lowest tertile of asthma-related emotional health had almost three times higher odds of being from a household without residential smokers compared to the highest tertile (aOR 2.90; 95% CI 1.06–7.95) (p-value for linear trend 0.035). Additionally, SHS-exposed children with caregivers in the lowest tertile of functional social support had more than three times higher odds of being from a household without residential smokers compared to the highest tertile (aOR 3.50; 95% CI 1.12–10.99) (p-value for linear trend 0.040).
No associations were identified with the child’s asthma-related emotional health, the child’s and family’s asthma-related activity limitations, and the presence of clinically significant caregiver depressive symptoms and the odds of a SHS-exposed child being from a household without residential smokers.
DISCUSSION
Because no amount of exposure to tobacco smoke is considered safe, identification of barriers to complete SHS remediation is critical. Our findings highlight multiple sources of SHS in households and thereby underscore the necessity of a multifaceted approach to in-home SHS exposure remediation. In a cohort of children with asthma who are exposed to SHS at home, those living in households without residential smokers, and therefore exposed from exclusively external sources, had caregivers with stronger beliefs in the harms of SHS. However, despite comparatively improved environmental circumstances, these caregivers were also more likely to experience low functional social support and worse child-specific asthma-related emotional health, findings which persisted after adjustment for relevant confounders. To our knowledge, this is the first study to quantitatively contrast characteristics between SHS-exposed households with and without residential smokers, identifying factors that may represent differential barriers to SHS remediation.
Considering the at-risk caregiver identified in our study, with heightened psychosocial distress over their child’s asthma and without robust social support to process their concerns, an overall pattern emerges that these individuals likely have lower agency to exert control over their environment and circumstances. Importantly, nearly twice the proportion of these caregivers strongly agreed that SHS should be avoided to improve their child’s asthma, supporting the possibility that they may not have had capability to fully prevent their child from being exposed or may not have recognized the exposure.
The identification of these factors is helpful in informing approaches to remediation of in-home SHS exposure in this population. The institution of a home smoking ban (HSB) is protective for pediatric SHS exposure, and HSBs are generally recognized as a valid counseling strategy for children who experience SHS exposure at home. However, our findings suggest that this approach may be less effective in our at-risk households, where caregivers may not be sufficiently empowered or able to restrict external sources of SHS exposure. Within urban environments in general and our local community in particular, studies have demonstrated generally low rates of HSB adoption5,22,23. Indeed, interviews of caregivers in our community have shown that non-adoption of HSBs are associated with restricted social networks and lack of caregiver confidence in directing who may smoke in their home24.
A prominent challenge in efforts to reduce SHS exposure in children is its association with predictors that are either unalterable or infeasible to change. However, the factors identified in this study represent elements that are potentially modifiable on an individual level. These findings suggest that efforts to decrease general isolation through referrals to community or neighborhood organizations and initiatives to provide instrumental support, including assistance with transportation and childcare, may be helpful in achieving complete SHS remediation in these homes. These interventions may be initiated and coordinated by a variety of individuals in the care spectrum, from physicians (both the caregiver’s and the child’s) to community health workers, and if effective would represent valuable public health levers to limit SHS exposure for these children.
Further, large components of the caregiver’s asthma-related emotional health centered on doubts, worry, frustration, and stress over their ability to manage their child’s asthma. Despite this, there was strikingly no difference in objective markers of asthma severity between the two groups. Clinician efforts to improve caregiver knowledge of his or her child’s asthma, focusing on normalization of concerns and anticipatory guidance of disease trajectories, may be an effective and simple intervention to empower caregivers.
It is noteworthy that SHS-exposed children living in households without residential smokers accounted for nearly half of the total children exposed to in-home SHS in this study. By showing contrasting caregiver beliefs toward the harms of SHS exposure between these groups, this study adds to the evidence base for overall efforts to expand the scope of smoking bans, which have been effective in improving asthma health. These interventions are expected to be especially relevant for SHS incursion from the outside environment, which has been well-characterized, especially in public housing7,8. Government-initiated policies remove some of the onus of preventing SHS exposure from the caregivers, who as further characterized by this study may not be well-positioned to do so themselves. A national prohibition on public smoking in Scotland, for example, was associated with decreased rates of asthma admissions among children25. In the United States, this effort is continuing to develop, and a smoking ban in federally-subsidized public housing is scheduled to be fully implemented by 201826.
Finally, these findings offer some nuance to the wealth of literature examining connections between caregiver distress, both disease-specific and globally, with worsened asthma outcomes in their children27–30. Smoking and secondhand smoke are associated with both stressful states and respiratory morbidity and are often treated as a potential confounders in analytic constructs31. The results of this study suggest that ascertaining SHS exposure by identifying a smoker living in the home, which is often used, presents a source of differential confounding that may bias estimates. The impact of such an effect can only be speculated and should be considered hypothesis generating only, but this possibility supports the use of more comprehensive questionnaire- or biomarker-based methods to assign SHS exposure.
A strength of this study is the objective measurement of airborne nicotine, permitting unequivocal site-specific detection of SHS exposure and improving inferential validity. These results underscore the high prevalence of SHS exposure that is occurring in urban environments, even among households without residential smokers. The SHS exposure borne by children in these environments, which are higher than national averages, has been consistently associated increased healthcare utilization and additional adverse outcomes3,4, highlighting manifold downstream effects on the child, household, and health system. The results add further urgency to public health efforts to mitigate and prevent SHS exposure among children.
However, there are a number of limitations. Our findings rely on caregiver report on whether or not there are smokers residing within the home. A recognized social desirability bias may be expected to underestimate the proportion of smoking households. However, within pediatric populations overall, caregiver reports of their children’s SHS exposure compared against objective markers of SHS exposure have shown adequate reliability32,33.
Additionally, because we did not expressly query about the presence of smoking visitors or residence in public housing, we are unable to describe in more detail the individual contributors to SHS exposure among our households without residential smokers. Based on studies performed in our community and elsewhere, we anticipate substantial overlap of sources within this group34, highlighting the value of our parsimonious approach.
Familial emotional health, as assessed by the CHSA, is asthma-specific. It is unknown what other stressors may be associated with SHS exposure in households without residential smokers, and our results should not be interpreted to extend to stress in general. However, it is possible that other stressors not measured in this study may be predictive; in a population of inner-city adults with asthma, there was modest correlation between asthma-related quality of life as measured by the Asthma Quality of Life Questionnaire (AQLQ) and with the Perceived Stress Scale (PSS), a global measure of individual stress35.
The CHSA scales used to assess asthma-related activity limitation did not have strong discriminant ability in our population, and therefore conclusions about the null findings in those domains should be made cautiously. Approximately half of households scored the scale maximum in both familial and child-specific asthma-related activity limitation. Additionally, the emotional health of the child was indirectly assessed by the caregiver and may also be prone to inaccuracy.
Because of the low number of children in our population without SHS exposure, this study is not adequately powered to describe differences between these households and our SHS-exposed households that have no residential smokers, which is a complementary approach that may identify additional opportunities for intervention. However, because of the wealth of existent literature correlating factors associated with in-home SHS exposure in general, our study is a necessary step in this line of investigation.
Finally, there are limitations of generalizability, as this study was focused on children with asthma recruited from urban environments. Further research in other settings is necessary to better characterize sources of familial and caregiver stress and to confirm whether this effect may be identified in other populations susceptible to SHS exposure.
In a cohort of inner-city children with asthma who are exposed to SHS at home, those exposed from exclusively external sources (living in households without residential smokers) had caregivers with stronger beliefs in the harms of SHS. However, these caregivers also endorsed worse social support, physical isolation, and increased distress over their child’s asthma, without objective differences in asthma morbidity. Targeting these identified factors may be an effective opportunity to remediate SHS exposure in this highly prevalent and especially vulnerable population.
IMPLICATIONS FOR POLICY AND PRACTICE.
Secondhand smoke exposure (SHSe) is a prevalent public health issue and affects up to half of all children in the United States.
In an urban cohort of children with asthma, an alarming three-fourths have SHSe at home. Importantly, however, nearly half of these homes did not have residential smokers. Caregivers in these homes felt more strongly about avoiding SHSe, but were more physically isolated, endorsed less functional social support, and felt higher distress over their child’s asthma, despite no differences in asthma symptoms.
These findings suggest that the lack of caregiver agency, contributed by the absence of functional support and physical isolation, is a significant driver of SHSe in these children.
Public health initiatives designed to provide functional support to at-risk caregivers may be important levers to SHSe prevention in urban populations representative of this cohort.
These findings are also supportive of more comprehensive policies toward public smoking bans and bans for smoking in public housing.
As an additional methodological implication, studies associating stress with SHSe-related outcomes should ascertain SHSe through methods other than asking about the presence of a smoker in the home, as this would represent a source of differential misclassification.
Acknowledgments
FUNDING
This work was supported by grants from the National Institute for Environmental Health Sciences of the National Institutes of Health (NIH) (grant number F32ES028578 to TDW, P50ES018176 to NNH, and P01ES018176, P50ES015903, and K24ES021098 to GBD); the National Center for Advancing Translational Sciences of the NIH (grant number KL2TR001077 to EPB); and the United States Environmental Protection Agency (EPA) (agreement number 83615201 and 83451001 to NNH). This manuscript has not been formally reviewed by EPA or NIH, and the views expressed in this document are solely those of the authors and do not necessarily reflect those of EPA or NIH.
References
- 1.Quinto K, Kit B, Lukacs S, Akinbami L. Environmental tobacco smoke exposure in children aged 3–19 years with and without asthma in the United States, 1999–2010. National Center for Health Statistics; 2013. [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. U.S. Department of Health and Human Services, Center for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. [Google Scholar]
- 3.Wang Z, May SM, Charoenlap S, et al. Effects of secondhand smoke exposure on asthma morbidity and health care utilization in children: a systematic review and meta-analysis. Ann Allergy Asthma Immunol. 2015;115(5):396–401. e392. doi: 10.1016/j.anai.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 4.Jin Y, Seiber EE, Ferketich AK. Secondhand smoke and asthma: what are the effects on healthcare utilization among children? Prev Med. 2013;57(2):125–128. doi: 10.1016/j.ypmed.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 5.Hopper JA, Craig KA. Environmental tobacco smoke exposure among urban children. Pediatrics. 2000;106(4):E47. doi: 10.1542/peds.106.4.e47. [DOI] [PubMed] [Google Scholar]
- 6.Schuster MA, Franke T, Pham CB. Smoking patterns of household members and visitors in homes with children in the united states. Arch Pediatr Adolesc Med. 2002;156(11):1094–1100. doi: 10.1001/archpedi.156.11.1094. [DOI] [PubMed] [Google Scholar]
- 7.Klassen AC, Lee NL, Pankiewicz A. Secondhand Smoke Exposure and Smoke-free Policy in Philadelphia Public Housing. Tob Regul Sci. 2017;3(2):192–203. doi: 10.18001/TRS.3.2.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kraev TA, Adamkiewicz G, Hammond SK, Spengler JD. Indoor concentrations of nicotine in low-income, multi-unit housing: associations with smoking behaviours and housing characteristics. Tob Control. 2009;18(6):438–444. doi: 10.1136/tc.2009.029728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matt GE, Quintana PJE, Destaillats H, et al. Thirdhand Tobacco Smoke: Emerging Evidence and Arguments for a Multidisciplinary Research Agenda. Environ Health Perspect. 2011;119(9):1218–1226. doi: 10.1289/ehp.1103500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Orton S, Jones LL, Cooper S, Lewis S, Coleman T. Predictors of Children’s Secondhand Smoke Exposure at Home: A Systematic Review and Narrative Synthesis of the Evidence. PLoS One. 2014;9(11):e112690. doi: 10.1371/journal.pone.0112690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Halterman JS, Yoos HL, Conn KM, et al. The impact of childhood asthma on parental quality of life. J Asthma. 2004;41(6):645–653. doi: 10.1081/jas-200026410. [DOI] [PubMed] [Google Scholar]
- 12.Chen X, Stanton B, Hopper J, Khankari N. Sources, locations, and predictors of environmental tobacco smoke exposure among young children from inner-city families. Journal of pediatric health care : official publication of National Association of Pediatric Nurse Associates & Practitioners. 2011;25(6):365–372. doi: 10.1016/j.pedhc.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Delpisheh A, Kelly Y, Brabin B. Passive cigarette smoke exposure in primary school children in Liverpool. Public health. 2006;120(1):65–69. doi: 10.1016/j.puhe.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 14.Longman JM, Passey ME. Children, smoking households and exposure to second-hand smoke in the home in rural Australia: analysis of a national cross-sectional survey. BMJ open. 2013;3(7):e003128. doi: 10.1136/bmjopen-2013-003128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hammond SK, Leaderer BP. A diffusion monitor to measure exposure to passive smoking. Environ Sci Technol. 1987;21(5):494–497. doi: 10.1021/es00159a012. [DOI] [PubMed] [Google Scholar]
- 16.Apelberg BJ, Hepp LM, Avila-Tang E, et al. Environmental monitoring of secondhand smoke exposure. Tob Control. 2013;22(3):147–155. doi: 10.1136/tobaccocontrol-2011-050301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Evans R, 3rd, Gergen PJ, Mitchell H, et al. A randomized clinical trial to reduce asthma morbidity among inner-city children: results of the National Cooperative Inner-City Asthma Study. J Pediatr. 1999;135(3):332–338. doi: 10.1016/s0022-3476(99)70130-7. [DOI] [PubMed] [Google Scholar]
- 18.Asmussen L, Olson LM, Grant EN, Fagan J, Weiss KB. Reliability and Validity of the Children’s Health Survey for Asthma. Pediatrics. 1999;104(6):e71. doi: 10.1542/peds.104.6.e71. [DOI] [PubMed] [Google Scholar]
- 19.Thomas JL, Jones GN, Scarinci IC, Mehan DJ, Brantley PJ. The utility of the CES-D as a depression screening measure among low-income women attending primary care clinics. The Center for Epidemiologic Studies-Depression. Int J Psychiatry Med. 2001;31(1):25–40. doi: 10.2190/FUFR-PK9F-6U10-JXRK. [DOI] [PubMed] [Google Scholar]
- 20.Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J Aging Health. 1993;5(2):179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 21.Broadhead WE, Gehlbach SH, de Gruy FV, Kaplan BH. The Duke-UNC Functional Social Support Questionnaire. Measurement of social support in family medicine patients. Med Care. 1988;26(7):709–723. doi: 10.1097/00005650-198807000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Okah FA, Choi WS, Okuyemi KS, Ahluwalia JS. Effect of Children on Home Smoking Restriction by Inner-City Smokers. Pediatrics. 2002;109(2):244. doi: 10.1542/peds.109.2.244. [DOI] [PubMed] [Google Scholar]
- 23.Mills AL, White MM, Pierce JP, Messer K. Home Smoking Bans Among U.S. Households with Children and Smokers: Opportunities for Intervention. Am J Prev Med. 2011;41(6):559–565. doi: 10.1016/j.amepre.2011.08.016. [DOI] [PubMed] [Google Scholar]
- 24.Hoehn JL, Riekert KA, Borrelli B, Rand CS, Eakin MN. Barriers and motivators to reducing secondhand smoke exposure in African American families of head start children: a qualitative study. Health Educ Res. 2016;31(4):450–464. doi: 10.1093/her/cyw028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mackay D, Haw S, Ayres JG, Fischbacher C, Pell JP. Smoke-free Legislation and Hospitalizations for Childhood Asthma. N Engl J Med. 2010;363(12):1139–1145. doi: 10.1056/NEJMoa1002861. [DOI] [PubMed] [Google Scholar]
- 26.Office of the Assistant Secretary for Public and Indian Housing. Instituting Smoke-Free Public Housing. Department of Housing and Urban Development: Federal Register. 2016;81 FR 87430. [Google Scholar]
- 27.Nagano J, Kakuta C, Motomura C, et al. The parenting attitudes and the stress of mothers predict the asthmatic severity of their children: a prospective study. Biopsychosoc Med. 2010;4:12. doi: 10.1186/1751-0759-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mrazek DA, Klinnert M, Mrazek PJ, et al. Prediction of early-onset asthma in genetically at-risk children. Pediatr Pulmonol. 1999;27(2):85–94. doi: 10.1002/(sici)1099-0496(199902)27:2<85::aid-ppul4>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 29.Wood BL, Miller BD, Lehman HK. Review of Family Relational Stress and Pediatric Asthma: The Value of Biopsychosocial Systemic Models. Fam Proc. 2015;54(2):376–389. doi: 10.1111/famp.12139. [DOI] [PubMed] [Google Scholar]
- 30.Milam J, McConnell R, Yao L, Berhane K, Jerrett M, Richardson J. Parental Stress and Childhood Wheeze in a Prospective Cohort Study. J Asthma. 2008;45(4):319–323. doi: 10.1080/02770900801930277. [DOI] [PubMed] [Google Scholar]
- 31.Halterman JS, Fagnano M, Conn KM, Lynch KA, DelBalso MA, Chin NP. Barriers to Reducing ETS in the Homes of Inner-City Children with Asthma. J Asthma. 2007;44(2):83–88. doi: 10.1080/02770900601180545. [DOI] [PubMed] [Google Scholar]
- 32.Gehring U, Leaderer BP, Heinrich J, et al. Comparison of parental reports of smoking and residential air nicotine concentrations in children. Occup Environ Med. 2006;63(11):766. doi: 10.1136/oem.2006.027151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wong GC, Bernaards CA, Berman BA, Jones C, Bernert JT. Do children with asthma and their parents agree on household ETS exposure? Implications for asthma management. Patient Educ Couns. 2004;53(1):19–25. doi: 10.1016/S0738-3991(03)00123-X. [DOI] [PubMed] [Google Scholar]
- 34.Jones LL, Atkinson O, Longman J, Coleman T, McNeill A, Lewis SA. The motivators and barriers to a smoke-free home among disadvantaged caregivers: identifying the positive levers for change. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2011;13(6):479–486. doi: 10.1093/ntr/ntr030. [DOI] [PubMed] [Google Scholar]
- 35.Wisnivesky JP, Lorenzo J, Feldman JM, Leventhal H, Halm EA. The Relationship between Perceived Stress and Morbidity among Adult Inner-City Asthmatics. J Asthma. 2010;47(1):100–104. doi: 10.3109/02770900903426989. [DOI] [PubMed] [Google Scholar]